Back to Journals » International Journal of General Medicine » Volume 15
SARS-CoV-2 Seroepidemiological Investigation in Jordan: Seroprevalence, Herd Immunity, and Vaccination Coverage. A Population-Based National Study
Authors Sheikh Ali S, Kheirallah KA , Sharkas G, Al-Nusair M , Al-Mistarehi AH , Ghazo M, Zeitawi A, Bellizzi S, Ramadan M, Alsulaiman JW, Alzoubi H, Belbesi A, Allouh MZ
Received 21 April 2022
Accepted for publication 1 July 2022
Published 5 September 2022 Volume 2022:15 Pages 7053—7062
DOI https://doi.org/10.2147/IJGM.S371711
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Sami Sheikh Ali,1 Khalid A Kheirallah,2 Ghazi Sharkas,1 Mohammed Al-Nusair,2 Abdel-Hameed Al-Mistarehi,2 Mahmoud Ghazo,1 Ali Zeitawi,1 Saverio Bellizzi,3 Mohannad Ramadan,3 Jomana W Alsulaiman,4 Hamed Alzoubi,5 Adel Belbesi,1 Mohammed Z Allouh6,7
1Epidemics Management, Jordan Ministry of Health, Amman, Jordan; 2Department of Public Health and Community Medicine, Faculty of Medicine, Jordan University of Science and Technology, Irbid, Jordan; 3Emergency Program, World Health Organization, Jordan Country Office, Amman, Jordan; 4Department of Pediatrics, Faculty of Medicine, Yarmouk University, Irbid, Jordan; 5Department of Microbiology and Immunology, Faculty of Medicine, Mutah University, Mutah, Jordan; 6Department of Anatomy, Faculty of Medicine, Jordan University of Science and Technology, Irbid, Jordan; 7Department of Anatomy, College of Medicine and Health Sciences, United Arab Emirates University, Al Ain, United Arab Emirates
Correspondence: Khalid A Kheirallah, Department of Public Health and Community Medicine, Faculty of Medicine, Jordan University of Science and Technology, P. O. Box: 3030, Irbid, 22110, Jordan, Tel +962 7 9611 9094, Email [email protected] Mohammed Z Allouh, Department of Anatomy, College of Medicine and Health Sciences, United Arab Emirates University, P. O. Box: 15551, Al Ain, United Arab Emirates, Tel +971 3 713 7551, Email [email protected]
Background: Population-based serosurveillance is a cornerstone to furthering our understanding of the COVID-19 pandemic at the community levels. In Jordan, four waves (phases) of seroprevalence epidemiological investigations were conducted using representative population-based national samples. This study aims to estimate the population-based seropositivity, herd immunity, and vaccination coverage at the fourth wave.
Methods: Multistage sampling technique was implemented to recruit a nationally representative sample for the fourth wave of the seroprevalence investigation (June to August 2021). Electronically collected data utilized a questionnaire on background demographics, chronic diseases, and COVID-19 vaccination history. Also, blood samples were collected to detect the presence of total Anti-SARS-CoV-2 IgM and IgG using Wantai/ELISA assays. Prevalence estimates were presented using percentage and 95% Confidence Intervals (C.I.).
Results: There were 8821 participants included in this study, with a mean age of 31.3 years, and 61.7% were females. COVID-19 national seroprevalence and vaccination coverage estimates were 74.1% (95% C.I.: 73.1– 74.9%) and 38.4% (95% C.I.: 37.1– 39.6%), respectively. Among children, seroprevalence estimates were similar to unvaccinated adults. Among COVID-19 adults, 57.2% were vaccinated. Among vaccinated participants, 91.5% were seropositive, while among unvaccinated, 63.2% were seropositive. By age group, seroprevalence ranged between 53.0% and 86.9%. Seroprevalence estimates were significantly different by gender, vaccination status and dose, and residence.
Conclusion: The reported interplay between seropositivity and vaccination coverage estimate seems insufficient to provide herd immunity levels to combat new variants of SARS-CoV-2. Children and healthcare workers seem to be an epidemiologically influential group in spreading COVID-19. As the globe is still grappling with SARS-CoV-2 infection, national seroepidemiological evidence from Jordan calls for more focus on vaccination coverage, especially among epidemiologically vulnerable groups, to optimize herd immunity.
Keywords: SARS-CoV-2, COVID-19, seropositivity, seroprevalence, herd immunity, vaccination, Middle East, Jordan
Introduction
Despite the rapid spread of COVID-19,1 the number of reported cases, especially in developing countries, is just a proportion of the SARS-CoV-2 infection. This is mainly attributed to incomplete reporting due to insufficient funds and resources. A comprehensive testing plan for the detection and isolation of SARS-CoV-2 infected patients is considered vital to reducing the spread of the disease.2,3 Detecting serum antibodies against SARS-CoV-2 can provide a precise assessment of the infected individuals within a specific population irrespective of the appearance of the clinical symptoms since many of these individuals may be asymptomatic.4–7 If new epidemic waves emerge, seropositivity investigations can help identify high-risk populations who could benefit from special preventive measures. The precise assessment of SARS-CoV-2 seroprevalence in the population is important in spite of the availability of vaccines recently.8,9 This is because seropositivity investigations can reveal the high-risk groups within the population on whom the vaccination efforts should be focused on.
On the other hand, population-based seroprevalence estimates of SARS-CoV-2 antibodies are crucial for evaluating population immunity against SARS-CoV-2. Still, seroepidemiological investigations have been limited.2,10–17 Population-based studies are the best feasible way to assess COVID-19 prevalence and the acquired immunity level. This is important from a public health viewpoint since COVID-19 patients usually do not show the classical symptoms of the infection. Add to that, some of these patients could be asymptomatic during the entire infection period.7 Therefore, seropositivity investigations are very important for tracking the infection chain that includes the asymptomatic patients who could further contribute to the spreading of the infection.18 Additionally, these investigations provide precise information about the spread and distribution of the infection in the population.19,20
With over one million confirmed cases and greater than 12,000 deaths by late mid-December 2021, Jordanians contributed approximately 5% to the total COVID-19 cases and 4% to overall deaths in the World Health Organization’s Eastern Mediterranean Region (WHO-EMR). This comprised 7% of all COVID-19 cases reported worldwide at the time. During the same period, Jordan was classified fifth among the most hit countries in the EMR.21 The COVID-19 epidemiological curve in Jordan during the first 19 months of the pandemic showed four distinct phases that reflect the complex interrelation between the natural evolution of the outbreak, the implementation of Non-Pharmaceutical Intervention (NPI) measures, the introduction of COVID-19 variants of concern (VoC), and the COVID-19 vaccination campaign (Figure 1). The first phase, which started in March 2020, witnessed the implementation of strict NPI measures that flattened the epidemiologic curvature and prolonged the “sporadic transmission”.22–24 The second phase featured a rapid increase in the number of infected cases due to toning down on preventive measures. During the second phase, Jordan was classified among the top countries with COVID-19 infection.15 In third phase, there was a new steady and progressive upsurge of cases with a peak of almost 10,000 daily cases over the last quarter of March 2021 (most likely due to the introduction of the Delta VOC). The final stage witnessed a steady decline of the epidemiological curve with a long plateau of around 900 daily cases during the June–September 2021 period.25 Recently, an upsurge of cases was witnessed due to the Omicron variant.
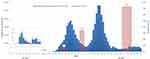 |
Figure 1 Epidemiologic curve of COVID-19 in Jordan: number of weekly reported cases and seropositivity. |
While the phases mentioned above are based on the national surveillance reporting system, the true effect of the pandemic on the Jordanian population was explored through serological nationwide representative surveys. The seroprevalence was reported to dramatically increase between August 2020 (0.3%) and October 2020 (7.0%). By the end of 2020, about one-third of the overall population was found to be COVID-19 seropositive (34.2%). This estimate would equal around 3.5 million of the total 10.2 million Jordanian population.15 Such seroprevalence estimation quantifies the extent of SARS-CoV-2 circulation with the third wave of the epidemic in Jordan (March 2021) as well as to the ongoing COVID-19 vaccination program. Four COVID-19 vaccines have been administered in Jordan; Pfizer/BioNTech and Sinopharm/Beijing starting mid-January 2021, then Oxford/AstraZeneca in mid-March 2021, and Sputnik V around April 2021. The majority of administered vaccines are Pfizer/BioNTech and Sinopharm/Beijing. Today, around 10 million vaccine doses have been administered for COVID-19, and about 5 million Jordanians are being totally vaccinated. This is comprised about 43.9% of the total population of Jordan. Additionally, There are half a million Jordanians being administered the booster dose (https://corona.moh.gov.jo/en).
The fourth phase of the nationwide, population-based serosurveillance was launched at the end of June 2021 with an aim to provide a better picture of the continuum of the pandemic in Jordan following the introduction of the COVID-19 vaccination campaign. This study utilized the fourth phase of seroprevalence investigations to provide national estimates for SARS-CoV-2 seroprevalence, herd immunity, and vaccination coverage.
Materials and Methods
Data was used from the fourth phase of the cross-sectional, population-based, COVID-19 serosurveillance data. Detailed methods and procedures are reported elsewhere.15 In short, a multistage sampling technique generated a population proportionate to size (PPS) national sample covering all governorates (N=12) and urban/rural settings. Considering a 10% of vaccination coverage at the time of the survey, there was a need to increase the sample size to ensure that the sample size for those non-vaccinated is similar to the previous study phases. The sample size was calculated based on an estimated disease prevalence of 35% and an acceptable margin of error of 5% (95% confidence level). Thus, the required sample size was estimated at 8732 participants within 1746 households (5 participants per household). A household was defined as a group of 2 or more individuals living in the same residence. A convenient household sample was selected from each governorate as defined by the Jordan Department of Statistics census blocks. Field home visits were used to identify households and invite members to participate. All persons living in the household (a maximum of six from one household) were invited to participate in the study. A line list of household residents was developed, and a sample of individuals was selected accordingly when potential participants’ number exceeded six.
The electronic data collection method was utilized to gather data regarding participants’ characteristics, including socio-demographics, chronic diseases (mainly diabetes mellitus and hypertension), and vaccination history. Blood samples were collected from the participants, then centrifuged, serum aliquoted, and properly shipped to the Jordanian Public Health Laboratory site for testing. The standardized laboratory procedures were previously presented.15
Fifteen teams of the Jordan Ministry of Health (MOH) healthcare workers were trained on the study protocol, interview-based data collection, and blood sampling. The teams’ work was facilitated by governorate supervisors. Each team included a data collector, a lab technician for specimen collection, and one local guide from the respective area. Electronic data was completed in 20 working days between June 27 and August 5, 2021. Blood samples were collected by a trained laboratory technician or nurse in a plain tube with gel before being transferred to the National Public Health Laboratory Directorate to detect the presence of Total Anti-SARS-CoV-2 IgM and IgG using the WANTAI SARS-CoV-2 Ab ELISA. WANTAI, a commercial microplate ELISA based on the receptor binding domain of the SARS-CoV-2 spike protein, is widely used around the world for qualitative detection of total antibodies to SARS-CoV-2.26 The test was carried out following manufacturer’s instructions (https://www.fda.gov/media/140929/download).
Overall national estimates were presented using numbers and percentages with the 95% confidence interval (95% C.I.). The chi-square test compared seroprevalence and vaccination coverage estimates by population background characteristics, including COVID-19 vaccination history. Epi Info statistical software application (version 7.1.5.0) was used to calculate the 95% CIs and conduct the chi-square test.
Research activities complied with the Code of Ethics of the World Medical Association, Declaration of Helsinki, for experiments involving humans. The study protocol was approved by the Jordanian Ministry of Health (MOH) Institutional Review Board (IRB). Written informed consent was signed by each participant or by the legal guardian for participants below 16 years of age. Individuals who refused to give informed consent or had a contraindication to venipuncture, households with less than two members, and residential institutions, such as boarding schools, dormitories, hostels, and prisons were excluded from the study.
Results
Out of the total number of study participants (N=8821), 61.7% were females, and more than half were 20 to 59 (54.0%) years old. The mean (SD) age was 31.3 (20.3) years. The proportions of subjects under five years old, five to nine, or 10 to 14 years old were about 3%, 10%, and 13%, respectively.
Overall, COVID-19 seroprevalence was 74.1% (95% C.I.: 73.1–74.9%). The percentage of COVID-19 vaccination was 38.4% (95% C.I.: 37.1–39.6%). Among COVID-19 age-eligible participants at the time of the study, 18 years or older (n=5877), 57.2% received the vaccine. Among vaccinated participants, 91.5% (95% C.I.: 90.6–92.4%) were found to be SARS-CoV-2 seropositive, while among unvaccinated, seropositivity was 63.2% (95% C.I.: 61.4–64.9%). By age group, seropositivity ranged between 53.0% and 86.9%, as presented in Figure 2. Significant differences in the seroprevalence estimates were detected by vaccination status and gender. Study participants who were COVID-19 vaccine eligible were more likely (80.8%) than their younger age counterparts (60.8%) to be seropositive (p<0.001). Female participants were more likely (76.1%) than males (70.8%) to be seropositive (p<0.001). The majority of vaccinated females (92.2%) and males (90.6%) were seropositive. Seropositivity showed slight differences by administrative geographical boundaries (governorates), ranging between 61.4% and 79.7%. Major urban areas also showed higher seroprevalence compared to rural areas.
 |
Figure 2 Distribution of seropositivity by age group (A), and its distribution by age group with COVID-19 vaccination status (B). |
To increase the accuracy of seroprevalence estimates related to vaccinated participants, we estimated the seroprevalence among vaccinated eligible adult participants who had no history of illness or contact with COVID-19 at the time of the study by excluding all vaccinated participants who had a fever or respiratory symptoms in the last 30 days, or who reported being in contact with a confirmed COVID-19 case within the last seven days. The total number of vaccinated participants used to estimate the seroprevalence estimate was 2469. Accordingly, among those who reported receiving a single dose of the COVID-19 vaccine (n=702), the estimated seroprevalence was 83.4% (586/702), while among participants who reported receiving the two doses (n=1767), the estimated seroprevalence was 94.2% (1665/1767) (p<0.001). The total seroprevalence estimate for the same group, regardless of the vaccine dose, was 91.2% (2251/2469). Similarly, when seroprevalence estimates are compared by vaccine type, statistically significant differences (p<0.001) between vaccine type and the seropositivity estimates (range 87–100%) were detected. The highest seroprevalence estimates were related to participants who reported receiving AstraZeneca (96.9% 282/291), followed by Pfizer (94.4%, 952/1008) and Sinopharm (86.8%, 1004/1157).
Seroprevalence by vaccine dose, single vs double, showed that participants who received a single dose of AstraZeneca or Pfizer were 90.0% seropositive, for each vaccine type, compared to 72.0% among those who received Sinopharm. Seroprevalence estimates for those who received the two doses were 100%, 97%, and 91% for AstraZeneca, Pfizer, and Sinopharm, respectively. Seroprevalence among unvaccinated according to their contact with a confirmed COVID-19 positive case was 77.7% compared to 60.8% among those who did not report contact with a case (p<0.001).
Out of the total adult participants (n=5877), 13.4% had chronic diseases (mainly diabetes mellitus and hypertension). Among participants who had chronic diseases, 61.0% were vaccinated and 82.1% were seropositive, while among those who did not report chronic diseases, 56.6% were vaccinated and 80.6% were seropositive (p=0.0216 and p=0.3097, respectively). Among study participants, 3.5% (n=305) were healthcare workers. Among those, the overall seroprevalence was 89.5%. Among vaccinated healthcare workers (n=252, 82.6%) the seroprevalence was 95.2% compared to 62.3% among their non-vaccinated counterparts (p<0.001).
Discussion
The emergence of COVID-19 seems to have changed the dynamics of vaccines, infection, and population immunity, especially with the effect of SARS-CoV-2 variants on the ever-changing threshold for herd immunity. Understanding this interplay is critical to evaluating the pandemic conditions and creating more tailored national and global responses. This study estimated the SARS-CoV-2 seroprevalence and vaccination coverage utilizing a nationally representative sample from Jordan. Among every ten individuals living in Jordan, more than seven were found to have the COVID-19 antibodies, and about four were vaccinated against COVID-19. The results also suggested a good immunization coverage among adults (57.2%) and a high seroprevalence among those who reported being vaccinated (91.5%). The study results provide public health officials and policymakers with the current immunization situation to develop appropriate vaccination strategies, effective immunization approaches, and action plans, such as utilizing a multi-sectoral One Health approach and non-state actors in combating pandemics.27,28
This study’s findings call for tailored, fine-tuned public health interventions to optimize community immunity levels by focusing on vulnerable groups and ensuring full vaccination dosage is administered. Recent literature has shown that achieving herd-immunity is more difficult than expected. For example, Los Angeles County in the United States reported a high level (72%) of population immunity in April 2021; however, there was a significant increase in COVID-19 infections three months later in the same county.29 Additionally, in China, researchers investigated the possibility of achieving herd-immunity against the “Delta” variant of the SARS-CoV-2 virus by utilizing a transmission compartmental vaccination approach.30 However, they did not succeed since herd-immunity required the vaccination of 93% of the population when considering vaccine effectiveness of 90% against the “Delta” variant.30
Addressing the issue of vaccine prioritization to reach herd-immunity has been considered. For example, the reduced protective immunity in Afro-American ethnicity and among individuals with lower-income in the United States was an indicator to tailor vaccination efforts for such vulnerable groups.29 A recent study investigated vaccine prioritization by using an age-structured vaccination modeling technique. It was suggested that, with a shortage of vaccine availability, an immunization protocol established on minimizing the basic reproduction number (R0) could be performed by providing more protection to age groups that are more vulnerable to infection.31 Another vulnerable group identified in some studies was healthcare workers, especially those working in intensive care units and emergency medical services, who are exposed to a higher-risk of being seropositive.32 On the other hand, tailored vaccination programs should also consider the pivotal role of “good governance” in facilitating vaccination, especially in developing countries. Effective and politically stable governments were suggested to be more influential in leading good immunization program and in better herd immunity levels through a prompt and an effective vaccine distribution.33 Within this context, our results support the notion that tailored vaccination programs are crucial particularly among vulnerable groups. This includes not only those living within geographically and economically vulnerable areas, but also healthcare workers. Accordingly, based on the available evidence, reaching herd immunity may be a challenging target. Still, effective immunization should consider vulnerable groups to dramatically reduce COVID-19 burden.
Gender differences in seropositivity may be attributed to the higher rates of the workforce among men, leaving women within households providing medical attention to the sick and potential COVID-19 cases. Similarly, observed age differences in seroprevalence estimates may be attributed to vaccine eligibility and vaccination priority for older age groups before allowing younger age groups to receive the vaccines. Still, the seroprevalence estimate among participants who were less than 18 years old is close to that among the unvaccinated persons in the community. This finding may be attributed to the fact that all age groups were affected in the same proportion, and the risk of COVID-19 spread among schoolchildren was high, as recently announced by the Jordanian government following a lengthy period of school closure and adoption of online education. Accordingly, the surge in COVID-19 cases following school re-opening could be justified by the recent risk of disease transmission among children.34–36 Differences in seroprevalence estimates by type and dose of the COVID-19 vaccine highlight the need to call for receiving the full vaccine dosages, especially for Sinopharm.
Our results regarding vaccination coverage harmonize with the coverage levels announced by the COVID-19 national vaccination program (31% of the general population and 56% in the targeted population at the time of the study). The overall seropositivity in the vaccine-eligible population (91%) also varied by vaccine type. The seroprevalence among non-vaccinated participants was also high (63%). Throughout the four serosurveillance phases, the seroprevalence estimates were in compliance with the national epidemiological situation in Jordan. The first phase was implemented before the community transmission and reflected a very low seroprevalence (0.28%). The second phase was implemented during the first COVID-19 wave and reflected about 7% seroprevalence, while the third phase was implemented after the peak of the first wave and estimated the seroprevalence at about 35%. In the current fourth phase, which was implemented after the end of the second wave, seroprevalence reflected about 75% seropositivity (Figure 1). The seroprevalence estimates also indicate that COVID-19 has spread on a large scale and has covered all ages and regions of the country. The evident sharp increase of seropositivity in the fourth phase reflects community transmission on a large scale in the second wave of the disease. Such serial surveillance activities are essential to further our understanding of the COVID-19 epidemiological curve, evaluate the actual national needs to combat the spread of COVID-19, and compare nationally reported COVID-19 statistics with seroprevalence estimates. Our results then deepen our understanding of the pandemic and ensure proper epidemiological tools are available to evaluate the community spread of the epidemic.
Further, connecting seroprevalence estimates to nationally reporting statistics strengthens the public health evidence of COVID-19 estimates in Jordan and provide grounds for proper risk communication and more reliance on surveillance activities at the national levels. Estimating seropositivity using population-based national studies provides a clear picture of the herd immunity levels needed to control the spread of the epidemic. On the other hand, the study results identify the importance of COVID-19 vaccination in increasing the seropositivity in the community, where about 17% of seropositivity is related to vaccines.
Considering that our results are based on a population-based study, it presents an unsettling example of what transient herd immunity might look like. The concept of herd immunity,10,37 when it comes to COVID-19, is still dynamic and depends on the interplay between vaccines, infections, and variants of SARS-CoV-2, as well as the mounting levels of uncertainties associated with the immunogenicity of the pathogen. While the initial threshold of herd immunity ranged between 60% and 67%,36 it was then argued that if COVID-19 vaccination does not generate protective immunity in vaccinated individuals, then the proportion of people requiring vaccination to achieve herd immunity will be higher than 67%. With the introduction of Delta and Omicron variants, the herd immunity levels were then raised to around 90%.38–41 Waning vaccine-induced immunity also adds to the interplay stated earlier and adds to the complex uncertainties associated with SARS-CoV-2 infection. To this end, Jordan’s reported seroprevalence may be disturbing as the country is still seeing a surge in numbers of cases, hospitalizations, and deaths that may have been associated with the Omicron variant. Also, the sub-optimal vaccination coverage reported in the current study is of concern. Without optimal vaccination, the risk of COVID-19 will be a significant concern to public health and socio-economic life in Jordan. This is especially true considering that herd immunity is driven by both contagiousness of the variant and the effectiveness of the vaccine. Our results, then, call to focus more on the role of vaccine protection and an ever-evolving virus, which keeps moving the goalposts, than merely focusing on a slippery concept like herd immunity. This is especially true as different countries have experienced different vaccine types at different coverage levels but still can reduce the effect of the infection by implementing more social distancing and mask-wearing. On the other hand, greater genomic surveillance can further our understanding of how much waning immunity, a highly contagious new variant, or other factors might have contributed to the resurgence of COVID-19 statistics.
Estimates of vaccination coverage and seroprevalence among specific population subgroups might be an indicator of a successful vaccination program and disease risk communication at the community level. Coverage and seroprevalence estimates among epidemiologically influential subgroups are essential for securing herd immunity levels. For example, vaccination coverage among healthcare workers (82.6%) seems not in compliance with the actual risk perceived among front-liners of the pandemic. While vaccinated healthcare workers may have high seroprevalence (95.2%), their unvaccinated counterparts had only 62.3%. Targeting such epidemiologically influential subgroups at an early pandemic stage should have been a cornerstone to ensure their relative immunity is optimized. Previous studies from Jordan reported the low willingness of healthcare workers to be vaccinated against COVID-19 and exaggeration of emotional distress and psychological challenges among healthcare providers and medical students.42–45 Another epidemiologically influential group in the current study was those with chronic diseases (13.4% of adult participants). Of which, about two-thirds were vaccinated, and 82.1% were seropositive. These numbers were significantly higher than that reported for participants without chronic diseases (56.6% and 80.6%, respectively). Jordan may have successfully communicated the message of high COVID-19 risk associated with chronic diseases and ensured such participants have a higher priority in vaccination.
Similarly, children were recently reported to be more influential in transmitting the SARS-CoV-2 than initially assumed.34,35 This report is evident in our findings, as more than half of the children were seropositive (Figure 1). Considering that COVID-19 vaccines are now (after study completion) approved for 12–18 years old in Jordan, such influential groups are then a potential target to increase herd immunity levels and play a role in the dynamics of the pandemic in Jordan. Prioritizing healthcare workers, children, and those with chronic diseases is then a necessity that needs to be further investigated in line with vaccine hesitancy reported in the region.46 Of importance for Jordan are refugees living within camp and host community settings, which represent more than 10% of the total population and could be the most influential groups for achieving optimal levels of herd immunity and vaccination coverage,47 given refugees’ sub-optimal living conditions that include crowdedness and shortage of essential services within the camp or host-community settings. Such groups need further investigation to understand their vaccination coverage and seroprevalence levels better.
Strengths and Limitations of the Study
This study’s strengths included the large sample size and its approach to figuring out seropositivity and vaccination coverage estimates and examining multiple factors to predict seropositivity. Our results are based on a nationally representative sample from different areas throughout the country and standardized laboratory testing procedures and protocols. Training on data collection and specimen collection and testing improved the validity and reliability of our results. Also, the study timeliness is one of its strengths. Most vitally, this is one of the first population-based seroprevalence investigation studies that obtained insights into COVID-19 herd immunity, seropositivity, and vaccination coverage in an Eastern Mediterranean developing country. Thus, we tried to fill the literature gap regarding such issues outside Western countries.
However, several limitations should be mentioned. Some study data was based on participants’ self-reporting, and thus, we could not check the accuracy of participants’ responses, and the results may be subjected to recall bias. However, the electronic data collection approach provides a private and safe environment for the respondents to answer questions honestly and accurately compared with face-to-face interviews and is a cost-effective method. Thus, the extent of such bias in the results is believed to be minimal with the large representative sample. The lack of available data on non-respondents and the cross-sectional design of the study are other limitations that could affect the results’ interpretation. ELISA was targeting the receptor-binding domain of spike protein which was validated against Wuhan strain. This might represent a limitation for future studies as new variants appeared since then with S gene mutations that could partially affect the antigenicity of the S protein. Lastly, our study estimated COVID-19 vaccine coverage rates under the condition that the vaccine was free; thus, vaccination coverage and seropositivity results might be affected if there would be out-of-pocket costs associated with the vaccine.
Conclusion
This study sheds light on the interplay between seropositivity and vaccination coverage to achieve herd immunity levels to combat new variants of SARS-CoV-2, such as Omicron. Among every ten individuals living in Jordan, more than seven were found to have the COVID-19 antibodies, and about four were vaccinated against COVID-19. Children and healthcare workers seem to be epidemiologically high-vulnerable groups in spreading COVID-19. The study findings call for tailored, fine-tuned public health interventions to optimize community immunity levels by focusing on vulnerable groups and ensuring full vaccination dosage is administered.
Ethics Approval and Informed Consent
All procedures performed in this study involving participants were reviewed and ethically approved by the Institutional Review Board (IRB) of the Jordanian Ministry of Health (MOH), Amman, Jordan. A written informed consent was obtained from all subjects involved in the study or from the legal guardian for participants below 16 years of age.
Acknowledgments
The authors would like to thank all participants of the study, along with the Ministry of Health staff who supported the implementation of the research activities and the WHO country office for providing support to the conduct of the research activities.
Funding
The article publishing charges were provided by a grant to M. Z. Allouh from the College of Medicine and Health Sciences at the United Arab Emirates University, Al Ain, UAE (Grant # G00003632).
Disclosure
The authors report no conflicts of interest in this work.
References
1. WHO coronavirus (COVID-19) dashboard. Available from: https://covid19.who.int.
2. Royo-Cebrecos C, Vilanova D, López J, et al. Mass SARS-CoV-2 serological screening, a population-based study in the Principality of Andorra. Lancet Reg Health Eur. 2021;5:100119. doi:10.1016/j.lanepe.2021.100119
3. Samrah SM, Al-Mistarehi AHW, Ibnian AM, et al. COVID-19 outbreak in Jordan: epidemiological features, clinical characteristics, and laboratory findings. Ann Med Surg. 2020;57:103–108. doi:10.1016/j.amsu.2020.07.020
4. Hellewell J, Abbott S, Gimma A, et al. Feasibility of controlling COVID-19 outbreaks by isolation of cases and contacts. Lancet Glob Health. 2020;8(4):e488–e496. doi:10.1016/S2214-109X(20)30074-7
5. Pan A, Liu L, Wang C, et al. Association of public health interventions with the epidemiology of the COVID-19 Outbreak in Wuhan, China. JAMA. 2020;323(19):1915–1923. doi:10.1001/jama.2020.6130
6. Okba NMA, Müller MA, Li W, et al. Severe acute respiratory syndrome coronavirus 2-specific antibody responses in coronavirus disease patients. Emerg Infect Dis. 2020;26(7):1478–1488. doi:10.3201/eid2607.200841
7. Khraise WN, Khraise TW, Starling EB, Allouh MZ. Epidemiologic and clinical characteristics of COVID-19 patients from a quarantine center in a developing community: a retrospective study. Int J Gen Med. 2020;13:937–944. doi:10.2147/IJGM.S276742
8. Lancet Respiratory Medicine T. Realising the potential of SARS-CoV-2 vaccines-a long shot? Lancet Respir Med. 2021;9(2):117. doi:10.1016/S2213-2600(21)00045-X
9. Wood S, Schulman K, Malina D. Beyond politics - promoting Covid-19 vaccination in the United States. N Engl J Med. 2021;384(7):e23. doi:10.1056/NEJMms2033790
10. Fontanet A, Cauchemez S. COVID-19 herd immunity: where are we? Nat Rev Immunol. 2020;20(10):583–584. doi:10.1038/s41577-020-00451-5
11. Thompson CP, Grayson NE, Paton RS, et al. Detection of neutralising antibodies to SARS-CoV-2 to determine population exposure in Scottish blood donors between March and May 2020. Euro Surveill. 2020;25:42. doi:10.2807/1560-7917.ES.2020.25.42.2000685
12. Ng DL, Goldgof GM, Shy BR, et al. SARS-CoV-2 seroprevalence and neutralizing activity in donor and patient blood. Nat Commun. 2020;11(1):4698. doi:10.1038/s41467-020-18468-8
13. Busch MP, Stone M. Serosurveillance for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) incidence using global blood donor populations. Clin Infect Dis. 2021;72(2):254–256. doi:10.1093/cid/ciaa1116
14. Pollán M, Pérez-Gómez B, Pastor-Barriuso R, et al. Prevalence of SARS-CoV-2 in Spain (ENE-COVID): a nationwide, population-based seroepidemiological study. Lancet. 2020;396(10250):535–544. doi:10.1016/S0140-6736(20)31483-5
15. Bellizzi S, Alsawalha L, Sheikh Ali S, et al. A three-phase population based sero-epidemiological study: assessing the trend in prevalence of SARS-CoV-2 during COVID-19 pandemic in Jordan. One Health. 2021;13:100292. doi:10.1016/j.onehlt.2021.100292
16. Carrat F, De Lamballerie X, Rahib D, et al. Antibody status and cumulative incidence of SARS-CoV-2 infection among adults in three regions of France following the first lockdown and associated risk factors: a multicohort study. Int J Epidemiol. 2021;50(5):1458–1472. doi:10.1093/ije/dyab110
17. Hallal PC, Hartwig FP, Horta BL, et al. SARS-CoV-2 antibody prevalence in Brazil: results from two successive nationwide serological household surveys. Lancet Glob Health. 2020;8(11):e1390–e1398. doi:10.1016/S2214-109X(20)30387-9
18. Oran DP, Topol EJ. Prevalence of asymptomatic SARS-CoV-2 infection: a narrative review. Ann Intern Med. 2020;173(5):362–367. doi:10.7326/M20-3012
19. Koopmans M, Haagmans B. Assessing the extent of SARS-CoV-2 circulation through serological studies. Nat Med. 2020;26(8):1171–1172. doi:10.1038/s41591-020-1018-x
20. Sughayer MA, Mansour A, Al Nuirat A, Souan L, Ghanem M, Siag M. Dramatic rise in seroprevalence rates of SARS-CoV-2 antibodies among healthy blood donors: the evolution of a pandemic. Int J Infect Dis. 2021;107:116–120. doi:10.1016/j.ijid.2021.04.059
21. COVID-19: WHO EMRO biweekly situation report #23. Available from: http://www.emro.who.int/images/stories/coronavirus/covid_sitrep_23.pdf?ua=1.
22. Kheirallah KA, Alsinglawi B, Alzoubi A, et al. The effect of strict state measures on the epidemiologic curve of covid-19 infection in the context of a developing country: a simulation from Jordan. Int J Environ Res Public Health. 2020;17(18):E6530. doi:10.3390/ijerph17186530
23. Ramadan M, Hasan Z, Saleh T, et al. Beyond knowledge: evaluating the practices and precautionary measures towards COVID-19 amongst medical doctors in Jordan. Int J Clin Pract. 2021;75(6):e14122. doi:10.1111/ijcp.14122
24. Samrah SM, Al-Mistarehi AH, Kewan T, et al. Viral clearance course of COVID-19 outbreaks. J Multidiscip Healthc. 2021;14:555–565. doi:10.2147/JMDH.S302891
25. Ministry of Health, the official website of the Jordanian Ministry of Health. Coronavirus disease. Available from: https://corona.moh.gov.jo/en.
26. GeurtsvanKessel CH, Okba NMA, Igloi Z, et al. An evaluation of COVID-19 serological assays informs future diagnostics and exposure assessment. Nat Commun. 2020;11(1):3436. doi:10.1038/s41467-020-17317-y
27. Kheirallah KA, Al-Mistarehi AH, Alsawalha L, et al. Prioritizing zoonotic diseases utilizing the one health approach: Jordan’s experience. One Health. 2021;13:100262. doi:10.1016/j.onehlt.2021.100262
28. Khassawneh AH, Alrabadi N, Al-Mistarehi AH, Obeidat N, Kheirallah KA. The role of non-state actors in combating COVID-19 spread in Northern Jordan. Ann Med Surg. 2020;60:484–486. doi:10.1016/j.amsu.2020.11.005
29. Sood N, Pernet O, Lam CN, et al. Seroprevalence of antibodies specific to receptor binding domain of SARS-CoV-2 and vaccination coverage among adults in Los Angeles County, April 2021: the LA pandemic surveillance cohort study. JAMA Netw Open. 2022;5(1):e2144258. doi:10.1001/jamanetworkopen.2021.44258
30. Liu H, Zhang J, Cai J, et al. Investigating vaccine-induced immunity and its effect in mitigating SARS-CoV-2 epidemics in China. BMC Med. 2022;20(1):37. doi:10.1186/s12916-022-02243-1
31. Saldaña J, Scoglio C. Influence of heterogeneous age-group contact patterns on critical vaccination rates for herd immunity to SARS-CoV-2. Sci Rep. 2022;12(1):2640. doi:10.1038/s41598-022-06477-0
32. Wiggen TD, Bohn B, Ulrich AK, et al. SARS-CoV-2 seroprevalence among healthcare workers. PLoS One. 2022;17(4):e0266410. doi:10.1371/journal.pone.0266410
33. Aida T, Shoji M. Cross-country evidence on the role of national governance in boosting COVID-19 vaccination. BMC Public Health. 2022;22(1):576. doi:10.1186/s12889-022-12985-5
34. Auger KA, Shah SS, Richardson T, et al. Association between statewide school closure and COVID-19 incidence and mortality in the US. JAMA. 2020;324(9):859–870. doi:10.1001/jama.2020.14348
35. Calvani M, Cantiello G, Cavani M, et al. Reasons for SARS-CoV-2 infection in children and their role in the transmission of infection according to age: a case-control study. Ital J Pediatr. 2021;47(1):193. doi:10.1186/s13052-021-01141-1
36. Piraveenan M, Sawleshwarkar S, Walsh M, et al. Optimal governance and implementation of vaccination programmes to contain the COVID-19 pandemic. R Soc Open Sci. 2021;8(6):210429. doi:10.1098/rsos.210429
37. Desai AN, Majumder MS. What is herd immunity? JAMA. 2020;324(20):2113. doi:10.1001/jama.2020.20895
38. Coronavirus disease (COVID-19): vaccines. Avialable from. https://www.who.int/news-room/questions-and-answers/item/coronavirus-disease-(covid-19)-vaccines.
39. Episode #45 - delta variant. Avialable from: https://www.who.int/emergencies/diseases/novel-coronavirus-2019/media-resources/science-in-5/episode-45—delta-variant.
40. Coronavirus disease (COVID-19): herd immunity, lockdowns and COVID-19. Avaialable from: https://www.who.int/news-room/questions-and-answers/item/herd-immunity-lockdowns-and-covid-19.
41. McDermott A. Core Concept: herd immunity is an important-and often misunderstood-public health phenomenon. Proc Natl Acad Sci U S A. 2021;118(21):e2107692118. doi:10.1073/pnas.2107692118
42. Al-Mistarehi AH, Kheirallah KA, Yassin A, et al. Determinants of the willingness of the general population to get vaccinated against COVID-19 in a developing country. Clin Exp Vaccine Res. 2021;10(2):171–182. doi:10.7774/cevr.2021.10.2.171
43. Yassin A, Al-Mistarehi AH, El-Salem K, et al. Prevalence estimates and risk factors of anxiety among healthcare workers in Jordan over one year of the COVID-19 pandemic: a cross-sectional study. Int J Environ Res Public Health. 2022;19(5):2615. doi:10.3390/ijerph19052615
44. Al-Shatanawi TN, Sakka SA, Kheirallah KA, et al. Self-reported obsession toward COVID-19 preventive measures among undergraduate medical students during the early phase of pandemic in Jordan. Front Public Health. 2021;9:719668. doi:10.3389/fpubh.2021.719668
45. Kheirallah K, Bloukh S, Khasawneh W, et al. Medical students’ relative immunity, or lack thereof, against COVID-19 emotional distress and psychological challenges; a descriptive study from Jordan. F1000Res. 2021;10:297. doi:10.12688/f1000research.52051.2
46. Abdou MS, Kheirallah KA, Aly MO, et al. The coronavirus disease 2019 (COVID-19) vaccination psychological antecedent assessment using the Arabic 5c validated tool: an online survey in 13 Arab countries. PLoS One. 2021;16(11):e0260321. doi:10.1371/journal.pone.0260321
47. Kheirallah KA, Ababneh BF, Bendak H, Alsuwaidi AR, Elbarazi I. Exploring the mental, social and lifestyle effects of COVID-19 infection on Syrian refugees in Jordan: a qualitative study. Review. 2021. doi:10.21203/rs.3.rs-1101153/v1
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
