Back to Journals » Cancer Management and Research » Volume 14
Real-World Outcomes and Prognostic Factors Among Patients with Advanced Non-Small Cell Lung Cancer and High PD-L1 Expression Treated with Immune Checkpoint Inhibitors as First-Line Therapy
Authors Ge W, Wu N, Jalbert JJ, Quek RGW, Liu J, Rietschel P, Pouliot JF, Harnett J, Hsu ML, Feliciano JL
Received 23 June 2022
Accepted for publication 21 October 2022
Published 16 November 2022 Volume 2022:14 Pages 3191—3202
DOI https://doi.org/10.2147/CMAR.S376510
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Harikrishna Nakshatri
Wenzhen Ge,1 Ning Wu,1 Jessica J Jalbert,1 Ruben GW Quek,1 Jinjie Liu,2 Petra Rietschel,1 Jean-Francois Pouliot,1 James Harnett,1 Melinda Laine Hsu,3 Josephine L Feliciano4
1Regeneron Pharmaceuticals, Inc., Tarrytown, NY, USA; 2Genesis Research, LLC, Hoboken, NJ, USA; 3University Hospitals, Cleveland Medical Center, Cleveland, OH, USA; 4Department of Oncology, Johns Hopkins University School of Medicine, Baltimore, MD, USA
Correspondence: Josephine L Feliciano, Department of Oncology, Johns Hopkins University School of Medicine, Baltimore, MD, USA, Tel +1 410 550 1711, Email [email protected]
Background: Immune checkpoint inhibitors (ICIs) are standard-of-care for patients with advanced non-small cell lung cancer (aNSCLC) and programmed cell death-ligand 1 (PD-L1) expression ≥ 50%.
Methods: A retrospective cohort study was conducted using the US de-identified electronic health record-derived Flatiron Health aNSCLC database (January 1, 2018, to July 31, 2021) among patients with PD-L1 ≥ 50% initiating first-line ICIs with or without chemotherapy. A clinical trial-like sub-cohort was also identified with Eastern Cooperative Oncology Group performance status 0– 1, adequate organ function, and no brain metastases or other primary cancers. Kaplan–Meier methods were used to estimate time to treatment discontinuation, time to next treatment, progression-free survival and overall survival (OS) by ICI regimen (ICI+chemotherapy, ICI monotherapy) and PD-L1 expression (50– 69%, 70– 89%, 90– 100%). Cox proportional hazard models were used to examine associations between ICI regimen, PD-L1 level, and OS, adjusting for baseline demographic and clinical variables.
Results: A total of 2631 patients with aNSCLC initiating ICI+chemotherapy (n = 992) or ICI monotherapy (n = 1639) were included; median (Q1, Q3) age was 71 (63– 78) years and 51.6% were male. The trial-like sub-cohort (n = 1029) generally had better outcomes vs. the overall cohort. Patients receiving ICI+chemotherapy generally had longer median OS vs. ICI monotherapy. Multivariable analyses showed no association between ICI regimen and OS among patients with PD-L1 70– 89% (hazard ratio [HR]: 0.90, 95% confidence interval [CI]: 0.73– 1.09) or 90– 100% (HR: 0.91, 95% CI: 0.77– 1.08), but patients with PD-L1 50– 69% receiving ICI+chemotherapy had longer OS (HR: 0.80, 95% CI: 0.64– 0.99).
Conclusion: Outcomes in real-world clinical trial-like patients with aNSCLC approached those reported in pivotal ICI trials in high PD-L1 expressers. ICI monotherapy offers a potential alternative in patients with PD-L1 ≥ 70% while avoiding potential chemotherapy toxicity exposure; the benefits are less clear in patients with PD-L1 50– 69%. Future studies should confirm these findings.
Keywords: immune checkpoint inhibitors, non-small cell lung cancer, PD-L1 expression, real-world data, overall survival, progression-free survival
Introduction
Immune checkpoint inhibitors (ICIs) are recommended for first-line treatment of patients with advanced non-small cell lung cancer (aNSCLC) and high programmed cell death-ligand 1 (PD-L1) expression levels (i.e., PD-L1 ≥50%) without genomic aberrations.1,2 In clinical trials, several ICI therapies resulted in significant improvements vs. chemotherapy in overall survival (OS) (median OS ≥18 months or not reached in the ICI arm; Supplementary Table 1) and progression-free survival (PFS) (median PFS approximately 7–8 months in the ICI arm; Supplementary Table 1) and with lower rates of toxicities, supporting US Food and Drug Administration (FDA) and European Medicines Agency (EMA) approval.3–5 ICIs have become the standard of care for treatment of patients with aNSCLC without actionable genomic aberrations. More recently, the FDA approved the first ICI for adjuvant treatment following resection and platinum-based chemotherapy in patients with stage II to IIIA NSCLC with PD-L1 ≥1%.6 Potential neoadjuvant use of ICIs in patients with resectable NSCLC are currently under investigation.7
In addition to clinical trials, understanding the real-world effectiveness of these immunotherapies in patients with aNSCLC can help guide treatment decisions.8,9 Several real-world evidence studies reported shorter OS than what was observed in clinical trials,10–13 limiting the generalizability of clinical trial data to clinical practice.9 Moreover, some ICIs are recommended as first-line treatment alone (ICI monotherapy) or in combination with chemotherapy (ICI+chemotherapy).1,2 However, results from randomized controlled trials that compared different ICI regimens are not currently available. Results from a real-world observational study among patients with high PD-L1 expression suggested median PFS and OS did not differ between ICI monotherapy and ICI+chemotherapy.14
To better understand the effectiveness of different ICI regimens, the main objectives of this study were to describe real-world outcomes among patients with aNSCLC and high PD-L1 expression treated with first-line ICI and to describe clinical outcomes among a sub-cohort who met commonly implemented ICI clinical trial criteria. A secondary objective was to explore the associations between ICI regimen (ICI+chemotherapy or ICI monotherapy) and PD-L1 expression level and OS, for which data are lacking.
Patients and Methods
Study Design and Data Source
This was a retrospective cohort study of patients with aNSCLC initiating ICI monotherapy or ICI+chemotherapy as first-line treatment in the US nationwide Flatiron Health electronic health record (EHR)-derived database. This longitudinal database comprises de-identified patient-level structured and unstructured data curated via technology-enabled abstraction.15 During the study period (2018–2021), the Flatiron Health data originated from ~280 US cancer clinics representing ~800 sites of care. The data are de-identified and subject to obligations to prevent re-identification and protect patient confidentiality. Institutional Review Board approval of the study protocol for creating the aNSCLC research database was obtained by Flatiron Health before the current study was conducted and included a waiver of informed consent.
Study Population
The study included adults newly diagnosed with aNSCLC, confirmed by review of pathology reports, between January 1, 2018, and July 31, 2021, who initiated first-line treatment with ICI monotherapy or ICI+chemotherapy within 90 days of the aNSCLC diagnosis. The date of first-line therapy initiation was defined as the index date. Lines of therapies were identified using Flatiron Heath oncologist-defined algorithms.16 Patients were also required to have received at least one PD-L1 testing result ≥50% before or within 28 days of first-line treatment initiation, and the initial diagnosis of aNSCLC had to be documented in the oncologist record within the Flatiron Health network no earlier than 30 days before the first EHR activity to ensure capture of full aNSCLC treatment history. Patients with known epidermal growth factor receptor (EGFR), anaplastic lymphoma kinase (ALK), or C-ROS oncogene 1 (ROS1) alterations were excluded.
A clinical trial-like sub-cohort was identified of patients who met key inclusion and exclusion criteria commonly implemented in pivotal PD-1 and PD-L1 clinical trials. The inclusion criteria were at least one Eastern Cooperative Oncology Group (ECOG) performance status measurement within 30 days before the index date with the highest ECOG performance status ≤1. The exclusion criteria were any diagnosis of other primary malignancies (other than non-squamous skin cancer or carcinoma in situ) before the index date; any diagnosis of central nervous system metastases (ICD-10-CM codes, C79.3X or C79.4X) on or before the index date; and any abnormal organ or bone marrow function within 30 days on or before the index date, defined as meeting any of the following: hemoglobin <9.0 g/dL, absolute neutrophil count <1.5 × 109/L, platelet count <100,000/mm3, glomerular filtration rate ≤30 mL/min/1.73 m2, total bilirubin ≥1.5×upper limit of normal (ULN) or >3 × ULN if liver metastases, aspartate aminotransferase and alanine aminotransferase >3× ULN or >5 × ULN if liver metastases, alkaline phosphatase >2.5× ULN or >5.0× ULN if liver or bone metastases, or met criteria for Hy’s law (alanine aminotransferase >3 × ULN and bilirubin >2× ULN).
Outcomes
Patients were followed from the index date to the event of interest, death, or October 31, 2021, the date of most recent data cut or end of follow-up. Outcomes following initiation of first-line treatment (index date) were defined as follows: time to treatment discontinuation (TTD) was time until initiation of second-line therapy or having a gap >120 days with no systemic therapy following the last administration of first-line treatment or death; time to next treatment (TTNT) was time to the date of initiation of second-line therapy or death; PFS was time to the first real-world progression event or death; and OS was time to date of death. Real-world progression was based on information abstracted by Flatiron Health from the medical charts and was defined as distinct episodes in the patient journey at which the treating physician determined there was spread or worsening of the disease. Flatiron Health uses a clinician-anchored approach supported by radiology report data, which was found to be the optimal and most practical method for assessing real-world progression.17 Patient-level structured data (EHRs, obituaries, and Social Security Death Index) and unstructured EHR data (abstracted) were linked by Flatiron to generate a composite mortality variable, which showed high sensitivity and specificity compared with the National Death Index.18
Baseline Variables
Baseline demographic and clinical characteristics included age at aNSCLC diagnosis, sex, race or ethnicity, treatment setting (academic, community), payer type (commercial, Medicare, Medicaid, other or unknown), histology (non-squamous cell carcinoma, squamous cell carcinoma, NSCLC not otherwise specified), ECOG performance status, smoking history, stage at initial NSCLC diagnosis, metastases (bone, liver or bile duct, brain), and PD-L1 expression level (50–69%, 70–89%, 90–100%). ECOG performance status was assessed within 30 days pre-index, and the closest value to the index date was used when multiple scores were available. Metastasis was defined as having any diagnosis code (ICD-10-CM) of secondary malignancy neoplasm of the corresponding site on or any time before the index date. The PD-L1 thresholds were selected based on the distribution of PD-L1 expression level.
Statistical Analysis
Baseline characteristics on the index date were described by first-line treatment (ICI+chemotherapy, ICI monotherapy) for both the main cohort and the clinical trial-like sub-cohort. Median TTD, TTNT, PFS, and OS with 95% confidence intervals (CIs) were estimated using the Kaplan-Meier method by first-line treatment in both the main cohort and sub-cohort for all patients with PD-L1 ≥50% and stratified by PD-L1 expression (50–69%, 70–89%, 90–100%).
The potential associations between ICI regimen (ICI+chemotherapy, ICI monotherapy) and PD-L1 expression level (50–69%, 70–89%, 90–100%) and OS in the main cohort were assessed using multivariate Cox proportional hazard models adjusting for baseline demographic and clinical characteristics, with estimates reported as hazard ratios (HRs) and 95% CIs. Considering the potential variation in the association between ICI regimen and outcomes across different PD-L1 levels, we included an interaction measure to reflect all six combinations of ICI regimens and PD-L1 expression levels. Pairwise comparison between selected pairs of regimens and PD-L1 subgroups was conducted to examine: 1) associations between PD-L1 expression levels and OS within the same ICI regimen; and 2) associations between ICI regimen and OS within the same PD-L1 expression level.
Results
Patient Population
Of the 25,144 adults newly diagnosed with aNSCLC between January 1, 2018, and July 31, 2021, in the Flatiron Health database, 16,542 initiated first-line systemic treatment within 90 days of their aNSCLC diagnosis, and 2631 met all other study criteria and were included in the main cohort (Supplementary Figure 1). The sub-cohort consisted of 1029 patients from the main cohort who met the additional clinical trial-like criteria (Supplementary Figure 1).
Patients in the main cohort were 51.6% male, 68.1% White, with a mean (SD) age of 70.0 (9.7) years (Table 1). The South had the greatest representation (45.0%), and 51.0% of the patients were commercially insured. The initial diagnosis of NSCLC was Stage IIIB or above in 79.7% of patients, with most patients having non-squamous cell carcinoma histology (72.0%), and 55.8% of patients had ECOG performance status 0 or 1 (Table 1). The distribution of patients across PD-L1 levels was 24.0%, 29.2%, and 46.9% for PD-L1 50–69%, 70–89%, and 90–100%, respectively. Patients who received ICI monotherapy were generally older than those who received ICI+chemotherapy, with a higher proportion of female patients, and were characterized by differences in clinical characteristics including higher proportions with recurrent disease (25.8% vs. 11.1%) and ECOG performance status 2–4 (23.8% vs. 14.8%).
 |
Table 1 Baseline Demographic and Clinical Characteristics of the Study Populations |
Demographic and clinical characteristics of the trial-like sub-cohort were similar to those of the main cohort overall and for each ICI regimen (i.e., ICI+chemotherapy, ICI monotherapy) except that all trial-like patients had ECOG performance status 0 or 1 and no central nervous system metastasis, and a lower proportion of patients treated in the academic setting (1.8% in the trial-like sub-cohort vs. 7.8% in the main cohort; Table 1). Characteristics by PD-L1 expression level for each treatment regimen are shown in Supplementary Table 2.
Time-to-Event Analysis
Median (Q1, Q3) duration of follow-up in the main cohort was 7.8 (2.4–18.7) months, which was slightly shorter vs. 9.4 (3.7–20.1) months in the trial-like sub-cohort. Similarly, median (Q1, Q3) duration of follow-up was shorter with ICI monotherapy than ICI+chemotherapy, 7.4 (2.1–18.6) months and 8.5 (3.3–19.0) months, respectively. Median PFS and OS were generally longer with ICI+chemotherapy than with ICI monotherapy, generally increased across both ICI regimens at higher PD-L1 expression levels, and were generally longer in the trial-like sub-cohort than the overall cohort (Table 2). In particular, the median OS was 16.8 months (95% CI: 13.7–19.0) and 13.2 months (95% CI: 11.7–15.3) with ICI+chemotherapy and ICI monotherapy, respectively, among the overall high PD-L1 expresser population. This difference was primarily driven by patients with PD-L1 50–69% (medians of 14.9 [95% CI: 11.3–19.8] and 10.5 [95% CI: 8.1–13.2] months with ICI+chemotherapy and ICI monotherapy, respectively), as the difference between treatment groups was small for both the PD-L1 70–89% (12.6 [95% CI: 9.9–19.0] vs. 12.5 [95% CI: 10.5–14.8] months) and PD-L1 90–100% (18.9 [95% CI: 15.9–22.8] vs. 17.6 [95% CI: 13.4–21.3] months) expression levels (Table 2). A higher proportion of patients receiving ICI monotherapy had ECOG performance status ≥1 than those receiving ICI+chemotherapy, with the largest difference between treatment regimens observed among those with PD-L1 50–69% (59.3% vs. 43.5%), followed by PD-L1 90–100% (59.7% vs. 51.7%), and PD-L1 70–89% (58.8% vs. 55.1%), which might partially explain the shorter median OS in those receiving ICI monotherapy. Median (95% CI) TTD and TTNT are shown in Supplementary Table 3, with generally longer median time to events in ICI+chemotherapy than ICI monotherapy.
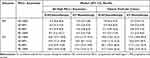 |
Table 2 Unadjusted Median Progression-Free Survival and Overal Survival |
Patients in the clinical trial-like sub-cohort generally had better outcomes relative to those in the overall cohort across all PD-L1 levels (Table 2, Supplementary Table 3). Differences in OS between the main cohort and trial-like cohort varied across PD-L1 levels in patients receiving ICI+chemotherapy, with the largest difference seen in those with PD-L1 70–89%. For ICI monotherapy, differences in median OS between the two cohorts were observed across PD-L1 expression levels. For each ICI regimen, median PFS was similar between the main cohort and the trial-like sub-cohort (difference in median PFS was ≤1 month; Table 2) and was also close to what was reported in ICI pivotal clinical trials (Supplementary Table 1).
Associations Between ICI Regimen, PD-L1 Expression Level, and OS
Comparisons between ICI regimens by PD-L1 levels showed that among patients with PD-L1 50–69%, those receiving ICI+chemotherapy had a lower risk of death than those receiving ICI monotherapy (HR: 0.80, 95% CI: 0.64–0.99). A similar risk of death was observed between ICI regimens among patients with PD-L1 expression levels of 70–89% and 90–100% (Figure 1). Among patients treated with ICI+chemotherapy, the risk of death was similar for those with PD-L1 50–69% and those with PD-L1 70–89%, with the HR approaching 1 (HR: 0.98, 95% CI: 0.78–1.24). In contrast, patients with PD-L1 50–69% or 70–89% had an approximately 20% higher risk of death than those with PD-L1 90–100% (HRs of 1.19 [95% CI: 0.96–1.49] and 1.21 [95% CI: 0.99–1.49], respectively) (Figure 1). Similarly, within the ICI monotherapy group, there was no difference in risk of death between patients with PD-L1 50–69% and 70–89%. However, compared with patients with PD-L1 90–100%, those with PD-L1 50–69% and 70–89% had higher risks of death, by 37% (HR: 1.37, 95% CI: 1.16–1.60) and 24% (HR: 1.24, 95% CI: 1.06–1.45), respectively.
Other Variables Associated with OS
Several other variables were found to be associated with OS. Patients treated in the academic setting had a 58% lower risk of death than those in a community setting (HR: 0.42, 95% CI: 0.28–0.63). In contrast, several patient characteristics were associated with poorer OS, including male sex, age ≥75 years, squamous cell carcinoma histology, ECOG performance status, stage IV disease, and metastasis in either the liver/bile duct or bone/bone marrow (Figure 1). For ECOG performance status, a higher risk of death was observed at higher scores relative to a score of 0, with HRs that ranged from 1.32 (95% CI: 1.13–1.54) with ECOG performance status 1, to 2.85 (95% CI: 2.19–3.71) with ECOG performance status ≥3.
Discussion
The survival benefits of several ICI therapies compared with chemotherapy among patients with aNSCLC and PD-L1 ≥50% were demonstrated in clinical trials. Our results showed that in real-world patients who met several ICI trial inclusion and exclusion criteria, the median OS and PFS approached those reported in the pivotal trials of ICIs in patients with aNSCLC and PD-L1 ≥50% (Supplementary Table 1). Consistent with prior real-world studies,13,19,20 survival estimates in the broader high PD-L1 expresser cohort were generally lower than those in the clinical trial-like sub-cohort and compared with clinical trials, but differences were minimized in patients with PD-L1 ≥90%. To our knowledge, our study is the first real-world study reporting survival outcomes by ICI regimen and by granular PD-L1 expression levels among high expressers. Our results suggest ICI+chemotherapy may have a greater benefit in patients with PD-L1 50–69% while ICI monotherapy may offer a potential alternative to the ICI+chemotherapy combination in those with PD-L1 ≥70%.
Real-world outcomes differ from clinical trials as trial participants tend to be healthier and younger due to more restrictive selection criteria than in the real-world setting. The presence of an ECOG performance status ≥2, active brain metastasis, and inadequate organ function are often reasons for exclusion of patients from clinical trials, yet these clinical variables are important prognostic factors for survival in patients with aNSCLC. When we selected real-world patients meeting such key trial eligibility criteria, we observed outcomes closer to those reported in trials despite the fact that these real-world patients were older with a percentage of patients ≥75 years old (34%) that was higher than typically seen in clinical trials. Furthermore, there were very small differences overall in PFS between the clinical trial-like sub-cohort and the main cohort when stratified by ICI regimen, which may be related to the lack of potential confounders associated with post-progression antineoplastic treatment. The median PFS in this real-world patient population also approached that reported in clinical trials (Supplementary Table 1).
While the use of select ICI monotherapy or ICI+chemotherapy has been recommended for patients with PD-L1 ≥50% in the absence of contraindicated genomic aberrations,1 there are no randomized controlled trial data to further guide regimen selection between ICI monotherapy and ICI+chemotherapy in this population. A recent network meta-analysis of clinical trials evaluating the efficacy of ICIs in aNSCLC showed that ICI+chemotherapy appeared to improve OS and overall response rate compared with ICI monotherapy only among PD-L1 high expressers, defined as PD-L1 ≥50%; no benefits were conferred by ICI+chemotherapy relative to ICI monotherapy or dual-agent ICI for negative (PD-L1 <1%) or low expressers (PD-L1 1–49%).21 On other hand, three real-world studies reported survival outcomes among patients with aNSCLC and high PD-L1 expression by ICI regimen. One study among patients with PD-L1 ≥50%, ECOG performance status 0 or 1, non-squamous histology, and normal laboratory values in the Flatiron Health database found similar PFS and OS outcomes between ICI+chemotherapy and ICI monotherapy after multivariate adjustment.12 Another study, which also used the Flatiron Health database, reported similar median OS between ICI+chemotherapy and ICI monotherapy among patients with squamous histology (median OS 12.3 [95% CI: 9.3–not estimable] vs. 11.9 [95% CI: 10.0–14.1] months), while numerically longer median OS was observed in ICI+chemotherapy among patients with non-squamous histology (median OS 19.1 [95% CI: 15.5–22.1] vs. 15.3 [95% CI: 13.4–17.5] months).20 A third study among high PD-L1 expressers using the ConcertAI Oncology database reported a median OS of 22.4 months (95% CI: 15.7–not estimable) with ICI+chemotherapy vs. 18.3 months (95% CI: 14.8–22.0) with ICI monotherapy.22 No adjusted comparison between ICI+chemotherapy and ICI monotherapy was performed in the latter two studies. Population heterogeneity may also contribute to different findings across studies and none of these studies reported outcomes by further granular strata of PD-L1 ≥50%. Additionally, it should be noted that in these studies, patients in the ICI monotherapy group tended to be older with poorer ECOG performance status (≥2) compared with those receiving ICI+chemotherapy, which was also observed in our study population.
Few studies have reported outcomes further stratified by PD-L1 expression levels among those with PD-L1 ≥50%. In the exploratory analysis of the Phase 3 clinical trial of cemiplimab among high PD-L1 expressers (EMPOWER-Lung 1), PD-L1 expression levels (≥90%, >60% to <90%, ≥50% to ≤60%) correlated with depth of changes in tumor measurements as well as with incremental improvements in OS, PFS, and overall response rate.5 Additional real-world studies among patients treated with first-line pembrolizumab monotherapy have evaluated other strata for optimal grouping of PD-L1 expression levels using recursive partitioning.23,24 In those studies, very high PD-L1 expressers, defined as PD-L1 ≥90%, were compared with PD-L1 50–89%,23–25 and had both higher overall response rate and longer OS. However, these studies did not evaluate ICI+chemotherapy vs. ICI monotherapy.
In the current study, we found that among patients with PD-L1 expression ≥70%, ICI monotherapy and ICI+chemotherapy resulted in similar benefits in OS, despite that patients receiving ICI monotherapy were older and had poorer ECOG performance status, while ICI+chemotherapy seemed to provide greater survival benefits than ICI monotherapy in those with PD-L1 50–69%. Approximately 39% of patients received ICI+chemotherapy in the PD-L1 50–69% group, highlighting a potential opportunity for therapy that warrants further evaluation. Furthermore, 37% of those with PD-L1 ≥70% received concomitant chemotherapy even though our findings suggested a benefit similar to ICI monotherapy, which avoids the toxicity of chemotherapy. The reasons behind such treatment choices were unavailable in this database, but may relate to several clinical factors. Some studies suggested the possibility of acquired resistance to ICIs when used over long periods of time, or more important, the fact that chemotherapy may increase the tumor’s response to ICIs and provide better short-term disease control.26 More granular stratification among patient with high PD-L1 expression should be included in future clinical trials and real-world studies to help better evaluate how the addition of chemotherapy to ICIs may impact outcomes in patients with aNSCLC.
A few strengths and limitations of this study should be noted. First, the study used the nationwide EHR-derived database comprising patients treated primarily in the community setting, reflecting a more general clinical practice. Even though we attempted to generate a clinical trial-like cohort, these patients might not resemble such patients in clinical trials due to limited data availability and achievable operationalization of trial-like eligibility criteria in real-world databases, e.g., patients without laboratory measurements were assumed to have adequate organ function. The distribution of demographic or clinical characteristics, such as age, sex, or histology may also differ in real-world vs. clinical trial populations. We were also not able to identify whether patients received ICIs as adjuvant or neoadjuvant treatments for earlier stages of disease. Therefore, differences in outcomes observed between the trial-like cohort and ICI pivotal clinical trials may be attributable to the differences in baseline characteristics and should be interpreted with caution. Indication bias was possible as patients receiving ICI monotherapy appeared to be older with poorer ECOG performance status than those receiving ICI+chemotherapy. Residual confounding in this study is likely; confounding by severity of detrimental prognostic factors might not be well captured in this database. However, if healthier patients were more likely to receive concomitant chemotherapy, such treatment choice may bias towards better outcomes in patients receiving ICI+chemotherapy, further supporting our finding of no survival benefits with concomitant chemotherapy in those with high PD-L1 expression. PD-L1 expression misclassification was possible as different commercial and laboratory-based assays were used among patients and the reliability of these assays might vary. Future studies should explore the benefit of adding chemotherapy to ICIs among patients with aNSCLC and high PD-L1 expression. The study period overlapped with occurrence of the COVID-19 pandemic, which may have impacted treatment patterns and clinical outcomes.
Conclusions
In this large real-world study of patients with aNSCLC and high PD-L1 expression who initiated first-line ICI regimens, outcomes in the clinical trial-like patients approached those reported in the key pivotal ICI trials conducted in high PD-L1 expressers. ICI monotherapy may offer a chemotherapy-sparing option in those with PD-L1 levels ≥70%; the benefits are less clear in patients with PD-L1 expression levels 50–69%. Future studies are warranted to better understand the benefits of adding chemotherapy in patients with high PD-L1 expression.
Abbreviations
ALK, anaplastic lymphoma kinase; aNSCLC, advanced non-small cell lung cancer; CI, confidence interval; ECOG, Eastern Cooperative Oncology Group; EGFR, epidermal growth factor receptor; EHR, electronic health record; HR, hazard ratio; ICI, immune checkpoint inhibitor; IQR, interquartile range; ITT, intent-to-treat; NE, not evaluable; NOS, not otherwise specified; NR, not reached; NSCLC, non-small cell lung cancer; OS, overall survival; PD-L1, programmed cell death-ligand 1; PFS, progression-free survival; ROS1, C-ROS oncogene 1; SD, standard deviation; TTD, time to treatment discontinuation; TTNT, time to next treatment; ULN, upper limit of normal.
Data Sharing Statement
The data that support the findings of this study have been originated by Flatiron Health, Inc. and are not publicly available, in order to safeguard the terms that ensure that the data remain deidentified. These de-identified data may be made available upon request and are subject to a license agreement with Flatiron Health; interested researchers should contact [email protected] to determine licensing terms.
Ethics Approval and Informed Consent
Institutional Review Board (WCG IRB, Puyallup, WA) approval of the study protocol was obtained before study conduct and included a waiver of informed consent.
Acknowledgments
Medical writing support in the preparation of this publication was provided by E. Jay Bienen, PhD, an independent medical writer, and funded by Regeneron Pharmaceuticals, Inc.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was funded by Regeneron Pharmaceuticals, Inc.
Disclosure
Wenzhen Ge, Ning Wu, Jessica J Jalbert, Ruben G W Quek, Petra Rietschel, Jean-Francois Pouliot, and James Harnett are employees and shareholders of Regeneron Pharmaceuticals, Inc. Jinjie Liu is an employee of Genesis Research, which provides consulting services to Regeneron Pharmaceuticals, Inc. Josephine L Feliciano reports receiving grants from Bristol Myers, AstraZeneca, and Pfizer; consulting fees from Merck, Takeda, Genentech, Coherus, AstraZeneca, Eli Lilly, and Regeneron; and payment or honoraria from Jansen. Melinda Laine Hsu reports personal fees from Regeneron, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. National Comprehensive Cancer Network (NCCN). Non-small cell lung cancer. Version 3.2020; 2020. Available from: https://www.nccn.org/professionals/physician_gls/pdf/nscl.pdf.
2. Planchard D, Popat S, Kerr K, et al. Metastatic non-small cell lung cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Updated version published 15 September 2020 by the ESMO guidelines committee; 2018. Available from: https://www.esmo.org/content/download/347819/6934778/1/ESMO-CPG-mNSCLC-15SEPT2020.pdf.
3. Reck M, Rodriguez-Abreu D, Robinson AG, et al. Pembrolizumab versus chemotherapy for PD-L1-positive non-small-cell lung cancer. N Engl J Med. 2016;375(19):1823–1833. doi:10.1056/NEJMoa1606774
4. Herbst RS, Giaccone G, de Marinis F, et al. Atezolizumab for first-line treatment of PD-L1-selected patients with NSCLC. N Engl J Med. 2020;383(14):1328–1339. doi:10.1056/NEJMoa1917346
5. Sezer A, Kilickap S, Gumus M, et al. Cemiplimab monotherapy for first-line treatment of advanced non-small-cell lung cancer with PD-L1 of at least 50%: a multicentre, open-label, global, phase 3, randomised, controlled trial. Lancet. 2021;397(10274):592–604. doi:10.1016/S0140-6736(21)00228-2
6. U.S. Food and Drug Administration. FDA approves atezolizumab as adjuvant treatment for non-small cell lung cancer; 2021. Available from: https://www.fda.gov/drugs/resources-information-approved-drugs/fda-approves-atezolizumab-adjuvant-treatment-non-small-cell-lung-cancer.
7. Friedlaender A, Naidoo J, Banna GL, Metro G, Forde P, Addeo A. Role and impact of immune checkpoint inhibitors in neoadjuvant treatment for NSCLC. Cancer Treat Rev. 2022;104:102350. doi:10.1016/j.ctrv.2022.102350
8. Juarez-Garcia A, Sharma R, Hunger M, Kayaniyil S, Penrod JR, Chouaid C. Real-world effectiveness of immunotherapies in pre-treated, advanced non-small cell lung cancer patients: a systematic literature review. Lung Cancer. 2022;166:205–220. doi:10.1016/j.lungcan.2022.03.008
9. Tang M, Lee CK, Lewis CR, et al. Generalizability of immune checkpoint inhibitor trials to real-world patients with advanced non-small cell lung cancer. Lung Cancer. 2022;166:40–48. doi:10.1016/j.lungcan.2022.01.024
10. Khozin S, Abernethy AP, Nussbaum NC, et al. Characteristics of real-world metastatic non-small cell lung cancer patients treated with nivolumab and pembrolizumab during the year following approval. Oncologist. 2018;23(3):328–336. doi:10.1634/theoncologist.2017-0353
11. Nadler E, Arondekar B, Aguilar KM, et al. Treatment patterns and clinical outcomes in patients with advanced non-small cell lung cancer initiating first-line treatment in the US community oncology setting: a real-world retrospective observational study. J Cancer Res Clin Oncol. 2021;147(3):671–690. doi:10.1007/s00432-020-03414-4
12. Lester J, Escriu C, Khan S, et al. Retrospective analysis of real-world treatment patterns and clinical outcomes in patients with advanced non-small cell lung cancer starting first-line systemic therapy in the United Kingdom. BMC Cancer. 2021;21(1):515. doi:10.1186/s12885-021-08096-w
13. Kehl KL, Greenwald S, Chamoun NG, Manberg PJ, Schrag D. Association between first-line immune checkpoint inhibition and survival for medicare-insured patients with advanced non–small cell lung cancer. JAMA Netw Open. 2021;4(5):e2111113. doi:10.1001/jamanetworkopen.2021.11113
14. Peters S, Dafni U, Perol M, et al. Effectiveness of PD-(L)1 inhibitors alone or in combination with platinum-doublet chemotherapy in first-line (1L) non-squamous non-small cell lung cancer (Nsq-NSCLC) with high PD-L1 expression using real-world data.
15. Ma X, Long L, Moon S, Adamson BJS, Baxi SS. Comparison of population characteristics in real-world clinical oncology databases in the US: flatiron health, SEER, and NPCR. medRxiv. 2020. doi:10.1101/2020.03.16.20037143
16. Khozin S, Carson KR, Zhi J, et al. Real-world outcomes of patients with metastatic non-small cell lung cancer treated with programmed cell death protein 1 inhibitors in the year following U.S. regulatory approval. Oncologist. 2019;24(5):648–656. doi:10.1634/theoncologist.2018-0307
17. Griffith SD, Tucker M, Bowser B, et al. Generating real-world tumor burden endpoints from electronic health record data: comparison of RECIST, Radiology-anchored, and clinician-anchored approaches for abstracting real-world progression in non-small cell lung cancer. Adv Ther. 2019;36(8):2122–2136. doi:10.1007/s12325-019-00970-1
18. Zhang Q, Gossai A, Monroe S, Nussbaum NC, Parrinello CM. Validation analysis of a composite real-world mortality endpoint for patients with cancer in the United States. Health Serv Res. 2021;56(6):1281–1287. doi:10.1111/1475-6773.13669
19. Velcheti V, Hu X, Piperdi B, Burke T. Real-world outcomes of first-line pembrolizumab plus pemetrexed-carboplatin for metastatic nonsquamous NSCLC at US oncology practices. Sci Rep. 2021;11(1):9222. doi:10.1038/s41598-021-88453-8
20. Waterhouse D, Lam J, Betts KA, et al. Real-world outcomes of immunotherapy-based regimens in first-line advanced non-small cell lung cancer. Lung Cancer. 2021;156:41–49. doi:10.1016/j.lungcan.2021.04.007
21. Pathak R, De Lima Lopes G, Yu H, et al. Comparative efficacy of chemoimmunotherapy versus immunotherapy for advanced non-small cell lung cancer: a network meta-analysis of randomized trials. Cancer. 2021;127(5):709–719. doi:10.1002/cncr.33269
22. Zhang X, DeClue RW, Herms L, et al. Real-world treatment patterns and outcomes in PD-L1-positive non-small cell lung cancer. Immunotherapy. 2021;13(18):1521–1533. doi:10.2217/imt-2021-0145
23. Aguilar EJ, Ricciuti B, Gainor JF, et al. Outcomes to first-line pembrolizumab in patients with non-small-cell lung cancer and very high PD-L1 expression. Ann Oncol. 2019;30(10):1653–1659. doi:10.1093/annonc/mdz288
24. Cortellini A, Tiseo M, Banna GL, et al. Clinicopathologic correlates of first-line pembrolizumab effectiveness in patients with advanced NSCLC and a PD-L1 expression of ≥ 50. Cancer Immunol Immunother. 2020;69(11):2209–2221. doi:10.1007/s00262-020-02613-9
25. Cortellini A, Cannita K, Tiseo M, et al. Post-progression outcomes of NSCLC patients with PD-L1 expression >/= 50% receiving first-line single-agent pembrolizumab in a large multicentre real-world study. Eur J Cancer. 2021;148:24–35. doi:10.1016/j.ejca.2021.02.005
26. Zouein J, Haddad FG, Eid R, Kourie HR. The combination of immune checkpoint inhibitors and chemotherapy in advanced non-small-cell lung cancer: the rational choice. Immunotherapy. 2022;14(2):155–167. doi:10.2217/imt-2021-0014
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

