Back to Journals » Patient Related Outcome Measures » Volume 13
Exploring Disease Remission and Bowel Urgency Severity Among Adults with Moderate to Severe Ulcerative Colitis: A Qualitative Study
Authors Dubinsky MC, Newton L, Delbecque L, Hunter T, Guobyte A, Naegeli AN, McFadden S, Donaldson J, Symonds T , Lewis JD
Received 24 June 2022
Accepted for publication 10 December 2022
Published 22 December 2022 Volume 2022:13 Pages 287—300
DOI https://doi.org/10.2147/PROM.S378759
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Robert Howland
Marla C Dubinsky,1 Louise Newton,2 Laure Delbecque,3 Theresa Hunter,4 Aiste Guobyte,5 April N Naegeli,4 Shehan McFadden,5 Jill Donaldson,6 Tara Symonds,2 James D Lewis7
1Icahn School of Medicine, Mount Sinai, NY, USA; 2Clinical Outcomes Solutions, Folkestone, UK; 3Eli Lilly and Company, Brussels, Belgium; 4Eli Lilly and Company, Indianapolis, IN, USA; 5Clinical Outcomes Solutions, Chicago, IL, USA; 6Crohn’s and Colitis Foundation, New York, NY, USA; 7Perelman School of Medicine, Division of Gastroenterology and Hepatology, University of Pennsylvania, Philadelphia, PA, USA
Correspondence: Laure Delbecque, Principal Research Scientist, Eli Lilly and Company, Brussels, Belgium, Tel +32 (0)499 72 31 37, Email [email protected]
Purpose: Achieving and maintaining symptom control is a key treatment goal in ulcerative colitis (UC). Bowel urgency is an important symptom of UC, thus measurement of urgency is critical. This research explored the patient experience of UC and “remission” in UC, with a focus on urgency, and cognitively debriefed the Urgency Numeric Rating Scale (NRS), including score interpretation and examination of meaningful improvement.
Patients and Methods: Semi-structured hybrid concept elicitation and cognitive debriefing interviews with adults with moderately-severely active UC were conducted to explore experiences of UC and urgency, as well as examine meaningful improvement and score interpretation of the Urgency NRS. Purposive sampling was used to identify 20 eligible adult participants with UC. Concept elicitation data were analyzed using thematic analysis, and a deductive approach was used to analyze cognitive debriefing data. Thematic analysis was also applied to meaningful change-related data.
Results: Twenty participants were interviewed (average age = 42.6 years old, 50% male); 14 with moderately active (70.0%) and 6 with severely active UC (30.0%). Disease remission was not consistently defined by participants and description varied in terms of definition (absence vs not complete absence of symptoms), duration (months vs days) and key symptoms to consider. Urgency was a prominent symptom for all participants, with 8 (40.0%) identifying it as the most bothersome aspect of UC. No issues were identified with the Urgency NRS. Participants were able to define different levels of urgency severity, describe how they relate to daily life impacts, and score them differently on the Urgency NRS. Participants were also able to reflect urgency improvement on the NRS and discuss how small changes in numeric ratings of urgency can reflect meaningful change in the symptom burden of their UC.
Conclusion: The Urgency NRS is a content valid and interpretable measure to assess bowel urgency severity.
Keywords: ulcerative colitis, qualitative, bowel urgency, content validity
Introduction
Patients with ulcerative colitis (UC) experience multiple bowel and gastrointestinal (GI) symptoms as part of this chronic inflammatory bowel disease.1,2 Alongside other symptoms, bowel urgency is recognized by the leading GI societies as an important symptom for UC diagnosis, a critical target for treatment success, and a key component of disease remission.1 Bowel urgency has been defined as the sudden need to have a bowel movement.1 The American College of Gastroenterology (ACG) clinical guidelines for the management of UC include absence of bowel urgency in their definition of UC disease remission.1 Despite this, assessment of bowel urgency is not incorporated in the Mayo score, which is the most commonly used disease activity measure for UC clinical trials. Assessment of bowel urgency is captured by the European Crohn’s and Colitis Organisation (ECCO)’s Simple Clinical Colitis Activity Index;3 a single “urgency of defecation” item uses a 4-point verbal response scale (VRS) with descriptors of “no urgency”, “hurry”, “immediately”, and “incontinence”. A potential limitation is that the interpretation between “hurry” and “immediately” may be difficult for respondents. Furthermore, its ability to detect meaningful changes is likely to be limited since it captures only 4 levels of urgency severity.
Given the importance of achieving disease remission as a treatment target, as well as the importance of reduction in bowel urgency as a clinical outcome, there is a growing need to have patient-friendly, sensitive, and reliable measures of bowel urgency for use in clinical practice and to incorporate in drug registration trials.
The Urgency Numeric Rating Scale (NRS) was designed to evaluate the self-reported severity of urgency to have a bowel movement.4 The Urgency NRS is an 11-point (0 “No Urgency” – 10 “Worst Possible Urgency”) patient-reported outcome (PRO) measure, which uses a 24-hour recall period and asks respondents: “How severe was your urgency (sudden or immediate need) to have a bowel movement in the past 24 hours?” The original qualitative research demonstrated the Urgency NRS is valid within patients with UC.5
Following on from the original research, this study was designed to explore the patient experience of UC and “remission” in UC, with a focus on bowel urgency, and cognitively debrief the Urgency NRS including score interpretation and examination of meaningful improvement in urgency and UC.
Methods
To address the study objectives, semi-structured hybrid concept elicitation and cognitive debriefing qualitative interviews were conducted with adults with clinically confirmed UC which was at least moderately active based on a clinician-completed severity rating scale at the time of recruitment. Patients with active disease were selected to match the population that would be most relevant in future clinical trials of UC and to ensure that participants were able to discuss recent symptomatic experiences and impacts on their health-related quality of life during the interview.
All interviews were conducted in US-English via telephone and lasted approximately 90 minutes. Study documents were submitted and given exempt status by the WCG Independent Review Board®. The study was conducted in compliance with Good Clinical Practice Guidelines,6 including the International Conference on Harmonization Guidelines7 and the study adhered to all local laws and regulatory requirements. Informed consent was obtained for all patients who participated in the study, including consent for publication of anonymized responses. Feedback from patients on their interpretation of response labels used in other bowel urgency assessment tools was also collected. Debriefing of a study-specific Patient Global Impression of UC Severity (PGIS) scale and a Patient Global Impression of Change in UC (PGIC) scale was also conducted to collect qualitative evidence that participants understood the scales as intended and explore which symptoms participants considered when selecting their response on the PGIS and PGIC. This is important because these scales could be used as anchors to inform the threshold that would constitute a clinically meaningful, within-patient change (MWPC) in the Urgency NRS score.
Recruitment and Sampling
Purposive sampling8 was used to identify 20 eligible adult participants from the US (≥18 years of age) with UC (confirmed by documentation of previous sigmoidoscopy or colonoscopy). A sample of 20 was chosen based on a general acceptance that this sample size is typically sufficient to reach a point of “informational redundancy”9 or “thematic saturation”10 in qualitative research where there is a fairly specific research question being explored. In addition, while purposive sampling can suffer from selection bias, which can limit the external validity of the study, the approach used here was appropriate because participants needed to be experienced in the topics of interest and be willing/able to participate in order for the study to address the desired research objectives.
As noted above, only individuals rated by clinicians as having moderately or severely active UC “at this time” were enrolled. Demographic criteria were targeted to ensure the sample was sufficiently diverse including at least 5 participants over the age of 45, at least 10 male participants, at least 2 participants of Hispanic or Latino ethnicity, and at least 2 Black or African American participants. In addition, participants that had lower education, defined as having no more than a high school diploma, were sought to ensure that assessment tools were acceptable to individuals with different education levels.
Individuals were excluded if they had a previous diagnosis of Crohn’s disease, indeterminate colitis, radiation colitis or diverticular associated colitis. Previous surgical resection and any other medical or psychiatric condition that might interfere with participant’s ability to evaluate their UC experience were also exclusion criteria.
Recruitment was carried out by two clinical sites and a patient advocacy group (PAG). For clinical sites, clinicians reviewed their patient database to identify individuals who met the study eligibility criteria. The PAG advertised the study to their network of UC patients through a newsletter, posted on a social media site, and posted on the PAG website. The advertisement introduced the study and provided instructions for contacting study staff.
Interview Discussion
A semi-structured discussion guide was used to conduct patient interviews. The discussion guide utilized two methodologies to address the study objectives: concept elicitation (CE) and cognitive interviews (CI).11 In the CE discussion, participants were asked to describe their experiences of UC symptoms and upon spontaneous mention of bowel urgency, were asked in-depth questions to explore the symptom in more detail. If a participant did not report bowel urgency spontaneously, they were asked if they had ever experienced this symptom and answered more specific questions thereafter. Participants then discussed disease remission; as well as talking about their personal experience of disease remission, they were also asked how they interpreted the term “remission” and how they felt the concept was best defined. In the subsequent CI discussion, participants completed a “think-aloud” exercise using the Urgency NRS (Figure 1A) which involved them reading the contents aloud while completing the measure and explaining their interpretation and response to the NRS at the same time. Participants were also asked to indicate which scores on the Urgency NRS response options would constitute “none”, “mild”, “moderate”, and “severe” labels. Additionally, some participants were asked to place the ACG Clinical Guideline response labels (“Hurry”, “Immediately”, and “None”) along the NRS response options in the same manner. To explore meaningful improvement of the Urgency NRS, participants were asked to identify the amount of score change that would be meaningful and explain the types of improvements that they associate with that level of change. A similar exercise was conducted using the study-specific PGIS and the PGIC scales to collect insights around meaningful change in UC, as well as feedback on comprehension of the global measures (Figure 1B and C). Asking participants to define an individual level for meaningful change in this way is an acceptable approach to help identify a clinically MWPC on the PRO measures of interest.12 Interviews were conducted by two experienced researchers who participated in several practice interviews prior to the start of the study.
Data Analysis
Transcribed data were entered into NVivo v1.3 where qualitative coding and analysis were undertaken by trained researchers. Prior to analysis, all data were deidentified. To address the CE-related research objectives, data were analyzed using a thematic analysis approach9 whereby the researcher familiarized themselves with each transcript, noted initial ideas, and then coded relevant text systematically according to themes related to research objectives. This process aims to be flexible and reflective in order to generate a broad picture of what it is like to live with bowel urgency and how participants understand the concept of remission as related to bowel urgency and UC broadly. Qualitative differences in bowel urgency and UC experiences were examined between participants with moderately active UC and those with severely active UC. A deductive approach was used to analyze CI data. Thematic analysis was also applied to meaningful change-related data to enable triangulation of qualitative data and responses on the PRO measures of interest.
To ensure a high level of coding and agreement among the researchers, both analysts coded the first 2 transcripts and regularly reviewed how codes and themes were being applied to the transcripts. The lead researcher [LN] also reviewed all themes for consistency in analysis.
Results
Study Population
In all, 21 participants from the US were recruited in the study. One participant dropped out due to hospitalization (reason unreported); therefore, a total of 20 participants were interviewed, with a 50:50 ratio of male to female. At screening, clinicians rated participants’ disease activity according to how their UC was “at this time”. In total, 14 participants were rated as having moderately active UC (70.0%) and 6 were rated as having severely active UC (30.0%). Participants with moderately active UC were on average (mean) slightly younger than those with severely active UC; however, the age range was similarly distributed (39.9 [SD: 13.13] vs 49.0 [SD: 14.52], respectively) (Table 1). In the total sample, 10 participants were over 45 years old. There were 3 participants (15.0%) who reported their ethnicity as Hispanic/Latino and 4 (20.0%) who reported their race as Black/African American, while 16 (80.0%) reported their race as White/Caucasian. In total, there were 7 participants (35.0%) who’s highest-level of education was a high school diploma or less, including 1 participant (5.0%) who did not graduate high school.
 |
Table 1 Summary of Demographic Characteristics of Participants (N = 20) |
From point of study enrollment, the mean (SD) time since diagnosis was 110 (139). The most recent diagnosis was 4 months previously and the longest was 506 months. The mean (SD) time since last colonoscopy was 18 (29) months. The most common current treatment for UC was aminosalicylates (5-ASA) (n = 11, 55.0%), followed by biologics (n = 6, 30.0%).
Bowel Urgency
Analysis of CE data by disease activity indicated that no substantive differences were observed between those with moderately active versus severely active UC. Qualitative descriptions of bowel urgency, including its severity and frequency, as well as experiences of UC remission, were generally consistent across the two severity groups.
Bowel urgency was a prominent symptom of UC for participants. When asked at the start of the interview to describe what UC is like in general, 40% (n=8/20; n = 6 with moderately active UC and n = 2 with severely active UC) spontaneously mentioned it as a symptom of their UC and the remaining participants (n=12/20, 60.0%) confirmed that they experience this symptom when asked directly by the interviewer. Furthermore, when asked to identify the most bothersome symptom of UC, bowel urgency (n=8/20, 40.0%) was most often cited, followed by abdominal pain (n=6/20, 30.0%), and frequent bowel movement (n=4/20, 20.0%). Bowel urgency was seen as the most bothersome symptom for participants with moderately active UC (n=6/14, 42.9%) and for participants with severely active UC (n=2/6, 33.3%).
Bowel urgency was described as a feeling of not being able to hold on to a bowel movement (n=14/20, 70.0%), with participants talking about bowel movements occurring “all of a sudden”, “right now”, or were “uncontrollable”. One participant spoke about how her bowel urgency comes on “suddenly” rather than being due to delaying a bowel movement. Many reported that bowel urgency may lead to “accidents” (n=11/20, 55.0%) which was associated with fear of not making it to the restroom in time,
What happens when I get that feeling of urgency? If I don’t get to a bathroom in time, I will, I will go on myself. I mean, it, that’s the reason why I have to wear diapers. (Male, aged 50 with severely active UC)
As a result of bowel urgency, participants (n=6/20, 30.0%) spoke about feeling “frantic”, “panicked”, or “worried”.
Bowel urgency occurred at different rates for participants. Some reported high frequencies, for example between 6 and 8 urgent bowel movements every day (n=5/20, 25.0%), or 10 or more times a day (n=7/20, 35.0%). Five participants (25.0%) discussed frequency as “bad days” and explained how they typically have 4 to 5 bad bowel urgency days each week. Participants were able to describe several levels of urgency severity, and severity of bowel urgency was more consistent day to day for the majority of participants (n=13/20, 65.0%), except during a flare when severity can be worse than usual. Severity of bowel urgency was described in terms of an increase in the number of times urgency occurs, or in terms of a decrease in the amount of time one can hold in a bowel movement. For instance, one participant described normal urgency as being “able to hold it, in a considerable time, you know? 15, 20 minutes, or maybe even longer than that”, whereas during a flare “within minutes, my body started to release, and that’s when I really had to just drop everything I had to do and, uh, and rush to the restroom” (Male, aged 35 with moderately active UC). When bowel urgency is severe, participants explained how their lives “revolved around the bathroom” (n=18/20, 90.0%). During these times, participants talked about having to run to the bathroom and trying their best to avoid having an accident. The notion of preparation and pre-planning was a clear theme in participants’ narratives; when bowel urgency is severe, they must know where the closest bathroom is and plan in case of emergencies, with some even carrying a change of clothes and adult diapers.
As well as discussing severe bowel urgency, participants were also asked about times when they had been in remission in relation to bowel urgency. Some participants were able to describe a time in their life since being diagnosed with UC where their bowel urgency went away completely (n=9/20, 45.0%) but they did not use the term “bowel urgency remission” to describe this state; rather they talked about how their urgency had “gone away”, or they were experiencing no symptoms. For instance, one participant described remission as follows: “…There’s a time when urgency has been better like, there’ll be like. There’s been like a few months where like I don’t have any symptoms” (Male, aged 25 with severely active UC). Other participants (n=9/20, 45.0%) described times where their bowel urgency had “reduced”, “improved”, or “is normal”. Only 2 participants (10.0%) reported never having experienced an improvement in their bowel urgency. Participants who experienced improvement in urgency talked about feeling normal (n=7/20, 35.0%) and happy (n=5/20, 25.0%) during these periods of improvement. As a result of improvements in bowel urgency, participants spoke about bathroom trips being easier and feeling less worried about needing to find a bathroom (n=9/20, 45.0%). The ability to attend or function better in work/school (n=5/20, 25.0%) was also noted when bowel urgency was less impactful, as remarked upon by this 52-year-old male participant (with moderately active UC),
I don’t have to run out. meaning I can eat lunch here at work this afternoon and I won’t have to jump out of a meeting or jump off a phone call, run to the toilet.
Being able to socialize more (n=5/20, 25.5%) and “go out” (n=4/20, 20.0%) were also highlighted when bowel urgency improved. As a result, participants are able to go back to their usual activities outside the home.
Bowel urgency was not experienced in isolation. Frequent bowel movements were the most commonly reported co-occurring symptom with severe bowel urgency (n=18/20, 90.0%). Incontinence was also commonly reported during periods of severe bowel urgency (n=14/20, 70.0%). When asked how severe their urgency has to be for it to result in having an “accident”, participants typically described the worst level of urgency, “How severe? Well, as severe as it could get because it’s like they’re ready to come out” (Female, aged 48 with moderately active UC). Abdominal pain (n=13/20, 65.0%), blood in stool (n=9/20, 45.0%), and fatigue (n=6/20, 30.0%) were also mentioned as occurring when urgency is present.
Disease Remission
The concept of “UC remission” resonated with participants during the interviews. Sixteen of the 20 participants who were asked to describe remission in UC talked about “normalcy” (n = 4, 20.0%) and “stability” (n = 8, 40.0%). Participants defined remission as times when their UC is “dormant”, in a “holding pattern”, or “solid”. Three participants (15.0%) referred to having “freedom”, while two (10.0%) used language relating to a religious experience, such as “heaven” and “hallelujah”. Others (n = 5, 25.0%) saw remission as a temporary experience, stating that it was “fragile”, “for the moment”, and a “pause” on symptoms. Despite this fragility, UC remission was strongly associated with better quality of life, with participants referring to being able to lead a normal life (n=7/20, 35.0%), as well as having less worry or anxiety, less concern about being near a bathroom, greater ability to socialize, and less concern about their diet (all n=4/20, 20.0%). Thirteen participants talked about how UC remission should be defined; 8 of these defined UC remission as the total absence of symptoms, whereas the remaining 5 defined remission as a time of having fewer or less severe symptoms but not necessarily complete symptom absence. Some symptoms appeared to be more important when thinking about remission. For example, participants remarked that frequent bowel movements (n=7/20, 35.0%), bowel urgency (n=5/20, 25.0%), nausea (n=3/20, 15.0%), abdominal pain (n=2/20, 10.0%), and blood in stool (n=2/20, 10.0%) would need to be eradicated or reduced for them to consider the period as remission. Some also talked about how long improvements should last for to consider the period of time as remission. For example, several (n=8/20, 40.0%) suggested that reduced or absent symptoms must occur for months or years – with 2 indicating that symptoms must be absent “forever” – while others (n=4/20, 20.0%) felt that remission could be defined by a shorter period of time, such as a few weeks or even a few days. Among those who suggested longer, more sustained change in symptoms, they noted that this was important due to previously experiencing “good days” that did not last.
Debriefing and Exploration of Meaningful Change on the Bowel Urgency NRS
The Urgency NRS evaluates the severity of bowel urgency based on patient self-report. A full summary of the results of the CI interviews are presented in Table 2. Content validity of the Urgency NRS was well-demonstrated in the CI interviews; for example, the concept of bowel urgency was relevant to all participants (n = 20, 100.0%) and almost all demonstrated a good understanding of the item wording (n = 19, 95.0%). All participants were able to recall the severity of their bowel urgency over the past 24 hours in order to select a response to the Urgency NRS (n=20/20, 100.0%).
 |
Table 2 Frequency Table for Urgency NRS |
Participants demonstrated they understood the Urgency NRS response options and scale (n = 20, 100.0%) and were able to articulate the meaning of different responses:
And that’s why I kind of put it in the middle. So immediate need is you got to solve this now, you’re in trouble, and that’s a 10, to zero being you can just decide in the afternoon, I’m going to hold it and just continue doing what I’m doing and then go later. (Male, aged 47 with moderately active UC)
Overall, the 0–10 scale was considered suitable for ratings of bowel urgency (n=17/20, 85.0%). The 3 participants who felt the NRS response scale could be improved indicated that an 11-point scale was too broad to reflect their experience of the different levels of urgency severity and it would be easier to select from fewer response options.
When asked where they would place the categories of mild, moderate, and severe bowel urgency on the scale, most participants (n = 17, 85.0%) commented a score of 1 to 3 would indicate “mild” bowel urgency, although 2 participants also included “0”. Mild urgency was described as “almost normal” to “normal urgency” (n = 6, 30.0%) and was also associated with being able to make it to the bathroom with ease (n = 6, 30.0%), being less worried about experiencing urgency when away from a bathroom (n = 4, 20.0%), being able to go more places (n = 2, 10.0%), or being able to eat the food they desired (n = 2, 10.0%). A score of 4 to 6 was associated with “moderate” bowel urgency by most participants (n = 16, 80%), stating that at this level they would need to ensure they are close to a bathroom (n = 8, 40.0%) and there would be an increase in bowel frequency (n = 4, 20%). “Severe” bowel urgency was associated with scores of 6 to 8 (n = 7, 35.0%) or 8 to 10 (n = 13, 65.0%); severe bowel urgency was described as an immediate or uncontrollable need (n = 8, 40.0%) which impacted individual’s ability to leave the home (n = 8, 40.0%) (Figure 2).
 |
Figure 2 Participants’ description of severity bands. A measure showing roughly three severity bands on the response option scale. The more saturated the red color, the more severe the band. |
Some participants were asked to place the ACG Clinical Guideline response labels (“Hurry”, “Immediately”, and “None”) along the NRS response scale. Of the 8 asked about “None”, 6 placed it at 0 on the NRS, 1 placed it at 1 and 1 felt it could be a 0 or 1. Of the 17 asked about “Hurry”, 8 placed it between 8 and 10 on the scale, while another 8 felt it reflected a score between 5 and 7. There were a few participants who overlapped, for example 1 participant allocated “hurry” to 5 to 8 while another placed it at 5 to 10. Finally, 2 allocated “hurry” between 3 and 4. For the label “Immediately”, most placed it between 9 and 10 on the NRS and 2 suggested between 8 and 10.
To examine participants’ perspectives on what constitutes a meaningful change on the Urgency NRS, participants were asked to consider if a 1-point improvement in their initial NRS response was meaningful. Half of all participants reported that this amount of change would be meaningful to them (n=10/20, 50.0%), stating that “any amount” of improvement in bowel urgency was important (Figure 3). With a 1-point change, participants described that they would expect to have less bowel urgency, resulting in better emotional well-being and greater ability to leave their home or go to work. Of those that endorsed a 1-point change as meaningful, their initial score on the Urgency NRS ranged from 2 to 9 suggesting that this small amount of change may not be driven by their baseline score only. Five participants (25.0%) reported that they would want to experience at least a 2-point improvement on the NRS to consider the change in bowel urgency to be meaningful. Participants who wanted at least a 2-point improvement reported that this amount of change would mean “having less frequent urges” which would lead to improvements in their mental health and ability to engage in social and leisure activities. Again, these participants scored from 2 to 7 suggesting that this amount of change may not be driven by their baseline score only. All the participants who indicated that a larger score change was needed to consider the change meaningful (including a 3-point change: n = 2; 4-point change: n = 1, >5-point change: n = 2) scored at least a 7 on the 0–10 scale initially. Participants talked about the greater score change would result in less frequent bowel movements (BMs) and being able to travel, go out more often, and plan less.
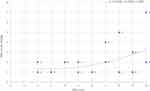 |
Figure 3 Level of change as meaningful on Urgency NRS by Urgency NRS score. Upward trending line shows that any level of change on the Urgency NRS is meaningful, regardless of severity level of UC. |
Of note, out of the participants who had a low score on the scale (<3) (n = 5), only 1 participant thought that a meaningful improvement would require a score of 0 (no urgency), while the other participants thought a score of 1 or 2 on the Urgency NRS was sufficient for meaningful improvement. One participant with a baseline score of 2 still considered a 1-point reduction meaningful, suggesting that a score of 1 on the urgency NRS may be a meaningful treatment target. For example, this participant indicated that a 1-point reduction “[.] would mean that my symptoms are pretty much remission” (Male, aged 41 with moderately active UC). Out of the participants who reported a higher score on the scale (>3) (n = 15), none targeted an Urgency NRS score below 3 as a score of meaningful improvement.
Debriefing and Exploration of Meaningful Change on the PGIS and PGIC
The PGIS captures overall severity of UC symptoms asking, “How would you rate your overall Ulcerative Colitis symptoms over the past 24 hours?” It uses a response scale containing 6 possible ratings: “No symptoms”, “Very mild”, “Mild”, “Moderate”, “Severe”, “Very severe”. A comprehensive summary of the results of the CI interviews on the PGIS are presented in Table 3. Participants demonstrated a good understanding of the wording of the PGIS (n=19/20, 95.0%) interpreting “overall ulcerative colitis symptoms” as referring to UC symptoms they experience in totality. Participants reported thinking about various UC symptoms, predominately bowel urgency (n=9/19, 47.4%), abdominal pain (n=7/19, 36.8%), blood in stool (n=6/19, 31.6%), and frequent BMs (n=5/19, 26.3%) when answering the PGIS.
 |
Table 3 Frequency Table for the PGIS |
To examine participants’ perspectives on what constitutes a meaningful change on the PGIS, participants were asked to consider if a 1-point improvement in their PGIS response was meaningful. Almost all (n=19/20, 95.0%) endorsed this amount of change as meaningful, stating that such improvement would allow them to better engage in daily activities and result in more opportunities to leave the home. Participants also felt a 1-point change would lead to reduced symptoms including improved urgency, abdominal pain, blood in stool, and frequent bowel movements. In contrast, 1 participant (5.0%) with severely active UC reported that they would need to improve by 4-points on the PGIS to consider the improvement meaningful, which they commented would allow them to leave the home more easily.
The PGIC captures overall change in UC symptoms, instructing respondents to, “Mark the box that best describes how your Ulcerative Colitis symptoms are now, compared to how they were before you started taking this medicine”. It uses a categorical response scale with 7 options: “Very much improved”, “Much improved”, “Minimally improved”, “No change”, “Minimally worse”, “Much worse”, “Very much worse”.
The PGIC was also well understood by participants and appropriate responses were selected when asked about a hypothetical change scenario. Nine participants (45.0%) spontaneously mentioned specific symptoms they considered when answering the PGIC, most often frequent BMs (n=4/9, 44.4%) and bowel urgency (n=3/9, 33.3%). All participants understood the PGIC response options and thought that they were suitable for capturing change. A full summary of the results is presented in Table 4.
 |
Table 4 Frequency Table for the PGIC |
Participants were asked to select a response to the PGIC which best reflected the amount of “meaningful change” that they reported using the PGIS. As noted above, almost all participants (n=19/20, 95.0%) endorsed a 1-point change on the PGIS as meaningful and of these, participants most often selected either “Minimally improved” (n=8/20, 40.0%) or “Much improved” (n=8/20, 40.0%) on the PGIC to reflect this 1-point change. The results of this analysis are presented in Supplemental Materials Tables 1 and 2. Those who reported a 1-point PGIS score change as minimally improved described having positive changes in UC symptoms including bowel urgency. Those who reported a 1-point PGIS score change as much improved associated this with better UC symptoms including bowel urgency, blood in stools, frequent bowel movements, and abdominal pain.
Discussion
This qualitative study provides important insights into the patients’ perspective of disease remission and bowel urgency as a meaningful symptom of UC. Indeed, this was one of the first qualitative studies to explore the concept of bowel urgency in-depth. Qualitative differences between those with moderately active UC compared with severely active UC in terms of their bowel urgency experiences were not found, although most participants talked about good days and bad days with bowel urgency suggesting that fluctuations in this symptom are a very real component of living with UC. This burdensome nature of bowel urgency was well-documented in these interviews with participants describing a range of other UC symptoms which occur alongside bowel urgency including frequent bowel movements and abdominal pain. On the other hand, participants also talked about the amelioration of bowel urgency which can lead to a “normal” life, further supporting the importance of this symptom as a target for treatment. Disease remission was a meaningful premise despite not being consistently defined. While previous studies have examined patient-defined remission based on clinical guidelines and assessment tools,10–12 this study was the first to use qualitative research methods to explore the concept of remission with patients themselves. In this study, some participants described remission as the total absence of symptoms while others felt it could be reflected in times of fewer or less severe symptoms, albeit not complete absence. Similarly, some noted that remission is a state of health that lasts months or years, while others would define a period as remission even if it only lasted a few weeks or even a few days. One possible interpretation of these data is that remission is not clear terminology to patients, and therefore, it is important that the concept of remission is well defined for patients so that they understand the intention of this concept consistently. Notably, participants did not emphasize resolution of inflammation in their definition of remission, again highlighting the importance of distinguishing these concepts.
The Urgency NRS was employed in these interviews to understand how participants use the 0–10 scale and reflect meaningful improvement in their bowel urgency severity. Participants were able to define different levels of urgency severity, describe how they relate to daily life impacts, and score them differently on the Urgency NRS. Participants were also able to discuss urgency improvement as it relates to the NRS and how small changes in numeric ratings of urgency could reflect meaningful change in the symptom burden of their UC. For at least half of the study sample, any improvement was considered important and for 75% as little as a 2-point change was considered meaningful. Descriptions of bowel urgency by those endorsing a 1-point change were consistent with descriptions by those endorsing a 2-point change as clinically meaningful. Improvements of this magnitude on the NRS and were associated with improvements in symptom burden, emotional well-being, and confidence to leave the home. Twenty-five percent of the participants indicated a larger score change would be needed for them to consider the change meaningful, all of these had baseline scores of “7” or higher on the NRS (range: 7–10). In contrast, baseline scores for those who endorsed a 1 or 2-point score change were well-spread across the scale (range: 2–9) suggesting that the smaller threshold was not only a function of skewness towards the lower severity end of the scale. However, findings regarding what would constitute a meaningful improvement should be interpreted with caution given the small sample size and artificial nature of the interview, as participants discussed the meaningfulness of a hypothetical treatment-related improvement. Urgency NRS score interpretation and any MWPC threshold should be calculated based on anchor-based analyses using data from interventional studies, complemented by these qualitative data.
Participants also largely agreed on the rating range for mild (scores of 1–3 on the NRS) and moderate (scores of 4–6 on the NRS) bowel urgency, while severe bowel urgency was split (scores of 6–8 and 8–10 on the NRS), suggesting that a “very severe” bowel urgency category may also be relevant. Of note, when debriefing the ACG Clinical Guideline response label of “Hurry”, there was confusion among participants; some rated the label as an 8 to 10 on a 0–10 scale, while others rated it as a 5 to 7; a few even scored “Hurry” between a 3 and 4. In contrast, the label “Immediately” was generally scored more severely as a 9 or 10. Thus, the term “hurry” may not be suitable as a response label due to differences in the level of severity that is associated with the concept of “hurry”. The Urgency NRS which uses a numeric scale may be a viable alternative, or supplementary approach, to these VRS assessments of bowel urgency used in the ACG Guideline and ECCO’s Simple Clinical Colitis Activity Index.
Meaningful change of the PGIS was also examined and again, participants endorsed a 1-point score change as a meaningful change across the 6 response categories. When asked to reflect this meaningful change in UC severity on the PGIC, half rated the change as “minimally improved” and half as “much improved” suggesting that these are the most relevant change categories to reflect meaningful improvement in UC from the patient’s perspective. These qualitative insights into meaningful change on the Urgency NRS and PGIS are important first steps in establishing how to interpret these measures.
It is critical for data integrity that the PRO measure is understood and relevant across the demography of the target population. In this study, all measures tested were well-understood by participants including those whose highest level of education was high school or less. There was no indication based on the interviews that patients from diverse backgrounds would have difficulty using the tested PRO measures and as such, are considered suitable for use in the patient segments tested to date. That said, collection of biomarker data (such as C-reactive protein or fecal calprotectin) or endoscopic information would have augmented the validity of the interview results and provided greater confidence in the clinical suitability of the study population. As well as this clinical limitation, there was also the lack of geographic diversity within the study population. In recruitment, focus was placed on ensuring that participants with a range of disease activity levels and educational attainments were enrolled and as a result, almost three-quarters of the sample were recruited from the southeast region of the US and only a quarter from other regions of the US. Although this limits the potential geographic representativeness of the findings, the need for clinical representativeness of the sample was considered more pressing and, therefore, prioritized. To build on this work, further research may wish to address this limitation if relevant for future use of the three PRO measures. In addition, psychometric validation of the measures in an interventional study to explore their validity, reliability, and further examine interpretations of meaningful change are important next steps.
Conclusion
In summary, this work helps to define how patients experience UC. Urgency was endorsed by all participants with moderate or severely active UC. Patients highly value urgency as a core symptom of the UC experience, yet little work has been done to determine how best to measure urgency.13 The new NRS is easy to use and interpret and demonstrated content validity. Similarly, the PGIS and PGIC described in this research are potentially useful tools for categorizing overall patient reported disease activity and change. Additional longitudinal studies in larger populations are needed to further define the psychometric properties of these new PRO tools.
Abbreviations
ACG, American College of Gastroenterology; BM, bowel movement; CE, concept elicitation; CI, cognitive interviews; ECCO, European Crohn’s and Colitis Organisation; GI, gastrointestinal; MWPC, meaningful within-patient change; NRS, numeric rating scale; PAG, patient advocacy group; PRO, patient reported outcome; PGIC, Patient Global Impression of Change; PGIS, Patient Global Impression of Severity; SD, standard deviation; UC, ulcerative colitis; US, United States; VRS, verbal rating scale; Y, years.
Data Sharing Statement
The datasets generated and/or analyzed during the current study are not publicly available due to the sensitive nature of the questions asked in this study; however, they are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
All study procedures were in accordance with ethical standards of the 1964 Helsinki Declaration and its later amendments, relevant laws, institutional guidelines, and granted an exemption under 45 CFR § 46.104(d)(2) by Western Institutional Review Board. Participant informed consent (written or verbal) was obtained as approved by the institutional review board.
Consent for Publication
Informed consent, including consent for publication of anonymized responses, was obtained from all individuals who participated in the study.
Acknowledgments
The authors received editorial support in the preparation of this manuscript from Clinical Outcomes Solutions. The authors, however, guided and are fully responsible for all content and editorial decisions for this manuscript.
Author Contributions
All authors made a significant contribution to the work reported, whether that is the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The authors acknowledge the financial support for this study from Eli Lilly and Company.
Disclosure
Laure Delbecque, Theresa Hunter, and April N. Naegeli are employees and shareholders of Eli Lilly and Company. Louise Newton, Aiste Guobyte, Shehan McFadden, and Tara Symonds are employees of Clinical Outcomes Solutions. Jill Donaldson received consulting fees from Eli Lilly and Company. Marla Dubinsky received consulting fees and served on advisory boards for AbbVie, Arena, Bristol-Myers Squibb, Eli Lilly, Gilead, Janssen Pharmaceuticals, Pfizer, Prometheus Labs, and Takeda. James Lewis received consulting fees from Johnson & Johnson Consumer Inc., Takeda, Eli Lilly and Company, Samsung Bioepis, UCB (DSMB), Bristol-Myers Squibb, Nestle Health Science, Dark Canyon Laboratories, Merck, Celgene/BMS, Janssen Pharmaceuticals, Bridge Biotherapeutics, Inc., Entasis Therapeutics, AbbVie, Pfizer (DSMB), Gilead (DSMB), Arena Pharmaceuticals (DSMB), Protagonist Therapeutics (DSMB), Amgen (DSMB), Sanofi (DSMB) and Scipher Medicine. James Lewis provided research support for Nestle Health Science, Takeda, Janssen, and AbbVie. The authors report no other conflicts of interest in this work.
References
1. Rubin DT, Ananthakrishnan AN, Siegel CA, Sauer BG, Long MD. ACG clinical guideline: ulcerative colitis in adults. Am J Gastroenterol. 2019;114(3):384–413. doi:10.14309/ajg.0000000000000152
2. Gajendran M, Loganathan P, Jimenez G, et al. A comprehensive review and update on ulcerative colitis. Dis Month. 2019;65(12):100851. doi:10.1016/j.disamonth.2019.02.004
3. Walmsley R, Ayres R, Pounder R, Allan R. A simple clinical colitis activity index. Gut. 1998;43(1):29–32. doi:10.1136/gut.43.1.29
4. Dubinsky M, Naegeli AN, Dong Y, et al. SA1820 The Urgency Numeric Rating Scale (NRS): a Novel Patient-Reported Outcome Measure to Assess Bowel Urgency in Adult Patients with Ulcerative Colitis. Gastroenterology. 2020;158(6):S–439. doi:10.1016/S0016-5085(20)31780-7
5. Dubinsky MC, Naegeli A, Dong Y, Lissoos T, Arora V, Irving P The Urgency Numeric Rating Scale (NRS): a novel patient-reported outcome measure to assess bowel urgency in adult patients with ulcerative colitis.
6. Food and Drug Administration. E6(R2) Good Clinical Practice: integrated Addendum to ICH E6(R1) Guidance for Industry; 2018. Available from: https://www.fda.gov/downloads/Drugs/Guidances/UCM464506.pdf.
7. World Medicial Association. Declaration of Helsinki; 2013. Available from: https://www.wma.net/what-we-do/medical-ethics/declaration-of-helsinki/.
8. Patton MQ. Two decades of developments in qualitative inquiry: a personal, experiential perspective. Qualitative Social Work. 2002;1(3):261–283. doi:10.1177/1473325002001003636
9. Lincoln YS, Guba EG. Naturalistic Inquiry. sage; 1985.
10. Charmaz K. Constructing Grounded Theory: A Practical Guide Through Qualitative Analysis. sage; 2006.
11. Patrick DL, Burke LB, Gwaltney CJ, et al. Content validity—establishing and reporting the evidence in newly developed patient-reported outcomes (PRO) instruments for medical product evaluation: ISPOR PRO Good Research Practices Task Force report: part 2—assessing respondent understanding. Value in Health. 2011;14(8):978–988. doi:10.1016/j.jval.2011.06.013
12. U.S. Department of Health and Human Services FDA Center for Drug Evaluation and Research; U.S. Department of Health and Human Services FDA Center for Biologics Evaluation and Research; U.S. Department of Health and Human Services FDA Center for Devices and Radiological Health; Guidance for Industry: Patient-Reported Outcome Measures: Use in Medical Product Development to Support Labeling Claims: Draft Guidance. Vol. 4: Health Qual Life Outcomes; 2006. 79. doi:10.1186/1477-7525-4-79
13. Dawwas GK, Jajeh H, Shan M, Naegeli AN, Hunter T, Lewis JD Prevalence and Factors Associated with Fecal Urgency Among Patients with Ulcerative Colitis and Crohn’s Disease in the Study of a Prospective Adult Research Cohort with Inflammatory Bowel Disease. Crohn's & Colitis. 2021;360:3.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

