Back to Journals » Clinical Interventions in Aging » Volume 17
Risk Factors Analysis and the Establishment of Nomogram Prediction Model of Hidden Blood Loss After Total Hip Arthroplasty for Femoral Neck Fracture in Elderly Women
Authors Hong WS, Zhang YX, Lin Q, Sun Y
Received 23 February 2022
Accepted for publication 20 April 2022
Published 4 May 2022 Volume 2022:17 Pages 707—715
DOI https://doi.org/10.2147/CIA.S363682
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Nandu Goswami
Wei-Shi Hong,1,* Ya-Xin Zhang,1,* Qun Lin,1 Yu Sun2
1The Graduate School, Dalian Medical University, Dalian, Liaoning, People’s Republic of China; 2Department of Orthopedics, Northern Jiangsu People’s Hospital Affiliated to Yangzhou University, Yangzhou, Jiangsu, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yu Sun, Email [email protected]
Purpose: To investigate the risk factors of increased hidden blood loss (HBL) after total hip arthroplasty (THA) for femoral neck fracture in elderly women and establish the nomogram prediction model for the guidance to reduce HBL in clinic.
Patients and Methods: A total of 206 elderly female patients with femoral neck fracture who underwent THA in Northern Jiangsu People’s Hospital from January 2019 to November 2021 were included. The demographic and relevant clinical information of the patients were collected. Pearson, independent sample t-test, multiple linear regression and other statistical methods were used for correlation analysis by SPSS 22.0 statistical software. Moreover, the risk factors of postoperative HBL increase in THA patients were obtained and the nomogram prediction model for the guidance to reduce HBL in clinic was established.
Results: HBL was 626 ± 400 mL, accounting for 72.8% ± 18.4% of the perioperative total blood loss (TBL) (799 ± 411 mL), while blood loss of HGB was 15.1± 10.4 g/L. Multiple linear regression analysis showed that HBL was associated with lower age (regression coefficient = − 9.271, P = 0.010), operative time (regression coefficient = 2.653, P = 0.004), preoperative blood calcium (< 2.25 mmol/L) (regression coefficient = 232.492, P < 0.001), hypertension (regression coefficient = 150.352, P = 0.002) and osteoporosis (regression coefficient = 276.072, P < 0.001). R software was used to construct the nomogram prediction model and draw the ROC curve and calibration curve. The area under the curve (AUC) is 0.92 and the slope of calibration curve is close to 1.
Conclusion: Based on the five independent risk factors including age, operative time, preoperative blood calcium, hypertension and osteoporosis, the nomogram can predict the risk of HBL after THA for femoral neck fracture in elderly women with favorable differentiation and accuracy.
Keywords: total hip arthroplasty, hidden blood loss, risk factors, nomogram prediction model, femoral neck fracture
Introduction
Femoral neck fracture in elderly women is steadily increasing due to the related complications such as osteoporosis, obesity, diabetes and degenerative muscle tone reduction. Total hip arthroplasty (THA) is one of the effective methods for the treatment of displaced femoral neck fracture, because it can promote early postoperative ambulation and achieve better functional outcomes after operation compared with internal fixation. However, the procedure of THA frequently leads to massive blood loss and 30–69% of patients need blood transfusion, which is a risk factor for postoperative complications, such as allergy, hemolysis and infection.
A multicenter European observational study by Lasocki et al showed that the average perioperative blood loss during primary unilateral THA was 1944 mL.1 In fact, the total blood loss (TBL) after surgery for hip fractures is much greater than actually observed during surgery.2,3 More and more studies have shown that hidden blood loss (HBL) of THA for femoral neck fracture significantly affect the TBL. This phenomenon of HBL was first described by Pattison et al in 1973 and formally defined in 2000.4,5 Currently, there is evidence that blood penetration into the tissues, blood accumulation around the joint, as well as hemolysis result in the formation of HBL.
The influential factors of HBL after THA for femoral neck fracture in elderly women have not been determined. Therefore, this study aims to find out the risk factors that may lead to the increase of HBL after THA by retrospective analysis. Moreover, the nomogram prediction model of massive blood loss and blood transfusion after THA for femoral neck fracture is established using R software, and the ROC curve is drawn to evaluate the differentiation of the nomogram model. The predictors of HBL in these patients can provide guidance for reducing the postoperative HBL of elderly women with femoral neck fracture.
Patients and Methods
Patients
A total of 206 elderly women with femoral neck fracture and an average age of (60–91 y) were recruited in this study. All the patients underwent primary THA surgery, which was performed by one same group of orthopedic surgeons in Northern Jiangsu People’s Hospital from January 2019 to November 2021. The study was conducted in accordance with the Declaration of Helsinki, and approved by the Ethics Committee of Northern Jiangsu People’s Hospital (protocol code 2021ky298). The need for informed consent from patients was waived by the board, since it was a retrospective cross-sectional study, and all the data were collected and analyzed anonymously without any potential harm to the patients. The inclusion criteria were aged >60 years, female, unilateral femoral neck fracture, no previous ipsilateral proximal femoral fracture or surgery and completed medical data. The exclusion criteria were preoperative blood transfusion, pathological fractures, any other traumatic fracture, neoplastic diseases, severe hematologic disorders and severe perioperative contraindications who cannot tolerate surgery normally.
Intra-Operative Treatment
All the patients received THA through the Moore posterolateral approach by the same surgeon and his team. Prophylactic intravenous cefazolin (2 g) was administered 30 minutes before the operation. General anesthesia or intraspinal anesthesia were performed according to the consultation advice of anesthesiologists. The length of incision was within a range of 10 to 15 cm, and uncemented prostheses were used in all cases. After the surgical field was rinsed, the hemostasis was performed by electrocoagulation. The tranexamic acid was also injected locally to stop the bleeding, and there was no drainage tube placed during operation. Postoperative intravenous cefazolin (2 g, bid) was administered to prevent infection within the first 24 hours. Low-molecular-weight heparin sodium (4000 AXaIU IH QD) was used to prevent deep venous thrombosis from preoperative to discharge.
Post-Operative Treatment (Transfusion Management + Data Acquisition)
Due to the policy for restrictive transfusion after THA, transfusions in patients in our hospital were performed when Hb<70 g/L and Hb<80 g/L with serious anemia symptoms (extreme weakness, chest pain, extreme paleness, or major bleeding) or with destabilizing vital signs (heart rate>100 or systolic blood pressure<90 mmHg).
The data were collected for all the patients including age, body mass index (BMI), hypertension, osteoporosis, preoperative Hematocrit (HCT), preoperative hemoglobin (HGB), preoperative red blood cell (RBC), preoperative platelet (PLT), preoperative prothrombin time (PT), preoperative activated partial thrombin time (APTT), preoperative international normalized ratio (INR), preoperative thrombin time (TT), preoperative fibrinogen (FIB), preoperative blood calcium, preoperative C-reactive protein (CRP), preoperative erythrocyte sedimentation rate (ESR), preoperative DD polymers, American Society of Anesthesiologists score (ASA), intraoperative blood loss, operative time, three days postoperatively HGB and three days postoperatively HCT. The preoperative medication control of hypertension patients was <140/90 mmHg. T score <-2.5 was defined as osteoporosis according to the results of bone mineral density examination.
Calculation of HBL
The estimated blood volume (EBV) was calculated according to Gross formula: EBV = K1 × height (m)3+ K2 × weight (kg)+ K3. When the patient is male, K1 =0.3669, K2 =0.03219, K3=0.6041, while when the patient is female, K1 =0.3561, K2 =0.03308, K3 =0.1833.6 Then, TBL was also calculated according to Gross’s formula: TBL=EBV× (preoperative HCT- postoperative HCT)/average value of HCT.7
The HBL was calculated according to the formula: HBL=calculated TBL + transfusion volume - visible blood loss (intraoperative blood loss+ postoperative drainage).3 Intraoperative blood loss was measured as the total amount of blood in the suction bottle (after subtracting the lavage fluid used during surgery) and gauze weighed during surgery.
Statistical Method
Data were collected for analysis using SPSS 22.0 statistical software. The descriptive statistics were shown as mean ± standard deviation or number of cases and percentage. The independent sample t-test was used to calculate the significant differences in HBL between different count data, while Pearson was used for univariate analysis between measurement data. Variables with the value of P<0.05 were accepted as candidates for multiple linear regression analysis to identify independent risk factors associated with HBL. The positive coefficient represents the positive influence on the dependent variable (HBL), while the negative coefficient represents the negative influence. All independent variables were included in the model. P<0.05 was considered statistically significant.
Result
Perioperative Parameters
We retrospectively analyzed the data of 206 consecutive female patients who underwent THA by the same senior surgeon in North Jiangsu People’s Hospital from January 2019 to November 2021. The mean age was 73.64±6.79 years (range from 60 to 91 years), and the mean BMI was 22.73±3.58 (range from 15.1 to 40.0). Data of HCT level loss, HGB loss, number of patients with preoperative and postoperative HGB <100 g/L,7 calculated TBL, visible blood loss, HBL and percentage of HBL are shown in Table1–3. The average TBL was 799±411 mL, and the average HBL was 626±400 mL, accounting for 72.8%±18.4% of TBL. There were 26 patients with Hb<100g/L before surgery (12.6%), while this number increased to 76 (36.9%) after surgery.
 |
Table 1 Perioperative Parameters of Patients |
Univariate Analysis
According to univariate analysis, there were no significant correlation of HBL with BMI, preoperative RBC, preoperative PLT, preoperative PT, preoperative INR, preoperative TT, preoperative FIB, preoperative DD polymer, preoperative ESR, intraoperative blood loss and ASA score. However, there were statistically significant differences in age, operative time, preoperative HGB, preoperative HCT, preoperative APTT, preoperative CRP, hypertension, osteoporosis, and preoperative blood calcium levels (P<0.05). The analysis results of measurement data and count data were shown in Tables 2 and 3 respectively.
 |
Table 2 Perioperative Hidden Blood Loss Parameters and Pearson Correlation Analysis Results |
 |
Table 3 Correlation Analysis Results of Perioperative Hidden Blood Loss Parameters and Independent Sample t-Test |
Multiple Linear Regression Analysis
Multiple linear regression analysis with nine statistically significant variables as independent variables and postoperative HBL as dependent variables showed that HBL was associated with lower age (regression coefficient =−9.271, P=0.010), operative time (regression coefficient =2.653, P=0.004), preoperative blood calcium (<2.25) (regression coefficient=232.492, P<0.001), hypertension (regression coefficient=150.352, P=0.002) and osteoporosis (regression coefficient =276.072, P < 0.001), as shown in Table 4.
 |
Table 4 Multiple Linear Regression Analysis of HBL Risk Factors After THA |
Prediction Model Construction
According to the results of multifactor analysis, R software (4.1.1) was used to construct the nomogram model of blood transfusion in elderly female patients after THA (Figure 1). The ROC curve of blood transfusion after THA in elderly women was drawn by the nomogram model using R language software, and the area under the curve (AUC) was calculated to be 0.92 (Figure 2), indicating that the prediction model had a favorable degree of differentiation. The calibration curve of the nomogram model was made, and the results showed that the slope of the calibration curve was close to 1 (Figure 3), which showed that the predicted risk of the prediction model was consistent with the actual risk, and the calibration degree of the prediction model was favorable.
 |
Figure 1 Nomogram of blood transfusions after THA in elderly women. |
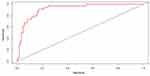 |
Figure 2 ROC curve of blood transfusion in elderly female patients after THA. |
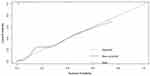 |
Figure 3 Calibration curves for the prediction of blood transfusions after THA in elderly female patients. |
Discussion
With the progress of social economy and medical technology, THA has become the first choice for more and more patients with displaced femoral neck fracture. In order to further improve the postoperative quality of life and satisfaction of patients, it becomes increasingly important to solve the problem of high allogeneic transfusion rate after THA. At present, relatively complete conclusions have been obtained in related studies on reducing intraoperative dominant blood loss in patients with THA. However, the risk factors for HBL after THA for femoral neck fracture in elderly women remain inconclusive.8–11 Therefore, this study carried out a detailed investigation on 206 consecutive elderly women with THA with relatively complete clinical data. The Gross formula widely used in the calculation of HBL in orthopedics was used to obtain a relatively reliable HBL.12–15 In this study, the mean HBL of the patients was 626±400 mL, accounting for 72.8%±18.4% of the total perioperative blood loss (799±411 mL). However, the HBL in our study was more than that in previous research (the HBL of THA was 429 ± 223 mL, with a percentage of 35.4% ± 11.0% in TBL).16 The reasons might be that we did not place drainage tube during the operation, resulting in partial dominant blood loss being included in HBL. Therefore, HBL plays a more important role in increasing the probability of postoperative allogeneic transfusion compared to readily observable dominant blood loss. In previous studies, it has been found that when blood loss exceeds 20% of total blood volume (1000 mL), appropriate replenishment of concentrated red blood cells is required to increase oxygen carrying capacity. Therefore, HBL=1000 mL was set as the outcome of the nomogram, so as to predict the probability of postoperative blood transfusion in present study.
The influence of age on postoperative HBL is still controversial.16,17,18 The result of our study showed that age is inversely correlated with HBL, and a 60-year-old female patient will gain approximately 44 points of weight in the nomogram compared to a 95-year-old female patient. There are two possible reasons for this result. Firstly, compared with younger patients with strong bodies and abundant blood vessels, the purpose of THA surgery for femoral neck fracture is more to relieve pain and improve postoperative function, while elderly patients mainly focused on relieving pain, which affected the surgical method and operative time. Therefore, perioperative blood loss in elderly female patients may be less due to less damage to soft tissue. Pearson analysis showed that patient age was negatively correlated with duration of surgery (P=0.002) and duration of surgery was positively correlated with HBL (P<0.001), which to some extent confirmed our study. Moreover, given that elderly patients tend to appear more emaciated, we suspected that lower occult blood volume in elderly female patients may be related to their own blood volume. Pearson analysis received supportive results that patient age was negatively correlated with EBV (P<0.001).
Furthermore, we found that operative time was also an important risk factor in HBL, which is similar to the results of previous studies.19,20 The reason may be that longer operative time usually means greater surgical damage, resulting in increased residual blood loss in the postoperative dead space. At the same time, a longer operative time will lead to a more severe postoperative inflammatory response, which will further aggravate hemolysis.21 Each additional 100 minutes of operative time will add approximately 38 points of weight to the nomogram.
Previous studies have indicated that reduced blood calcium activates the perivascular nerves where calcium ion receptors reside, resulting in changes in hemodynamics around the incision with more blood loss.22 Moreover, calcium ions play an important role in both endogenous and exogenous coagulation mechanism enzyme linked reactions. Therefore, the decrease of blood calcium implied the decrease of coagulation function, resulting in more blood loss. Our study showed that preoperative decrease in serum calcium ion concentration was an independent risk factor for postoperative HBL in elderly female patients undergoing THA. Compared with elderly female patients with normal serum calcium before surgery, elderly female patients with reduced serum calcium after THA would have an increased weight of about 100 points in the nomogram. Therefore, reasonable increase of blood calcium could effectively reduce postoperative HBL for elderly female patients with reduced preoperative blood calcium level.
It has been reported that hypertension is a risk factor for postoperative blood loss,23,24 which is consistent with the results of this study. In our study, elderly female patients with hypertension were given an additional weight of about 23 points in the nomogram compared with patients with normal blood pressure. Although tranexamic acid and other hemostatic drugs are routinely used during surgery, anticoagulant therapy was also used to prevent the formation of postoperative complications such as deep vein thrombosis of lower limbs, which potentially increased the occurrence of HBL after surgery. The tiny hemorrhagic spots formed by soft tissue release, acetabular grinding and intraoperative medullary expansion continued to ooze blood and remained in the tissue space under the effect of increased blood pressure and increased capillary brittleness, resulting in a significant increase in HBL of patients.25 Furthermore, the cardiovascular regulatory ability is mostly related to the active substances released by vascular endothelial cells, but the compensatory capacity in elderly women with hypertension was weakened and unable to effectively secrete vasoactive substances. Therefore, vascular elastic function decreases and vascular wall sclerosis, resulting in the capillary bed tension could not be timely regulated and body fluid was difficult to enter the systemic circulation to supple the lost blood volume. In addition, the reduction of vascular elasticity made the damaged blood vessels during surgery unable to retract normally, and the local HBL in the joint cavity was more likely to increase after surgery. Therefore, controlled hypotensive therapy in the perioperative period is of great significance to reduce postoperative HBL for elderly female patients with preoperative hypertension.
It has been previously reported that low bone density is a significant risk factor for HBL after hip fracture.26 Considering that the bone density of osteoporosis in elderly women was reduced, and the bone trabecula was narrowed or even broken, thus increasing the bone marrow space. Therefore, after proximal femur osteotomy, blood flowed into the enlarged bone marrow space, resulting in an increase of HBL. The increased level of oxygen-free radicals in the body of osteoporosis female patients could produce peroxidation reactions with the phospholipid membrane of red blood cells, further resulting in hemolysis reaction and exacerbating the loss of hemoglobin.27 Moreover, osteoporosis patients tend to be older, have less ability to regulate themselves, and their blood vessel elasticity is poor, which also increased the risk of HBL. Estrogen levels dropped after menopause in elderly women also affected the body’s absorption of calcium and increased the risk of osteoporosis. The results of our study were consistent with previous reports, showing HBL was associated with osteoporosis in elderly women. Our study also showed that elderly female patients with osteoporosis had an increased weight of about 58 points in the nomogram compared with patients with normal bone mass. Therefore, preoperative intervention measures, such as preoperative blood dilution or autologous blood transfusion, could be taken to prevent postoperative blood transfusion for elderly female patients with osteoporosis.
The shortcomings of this study were as follows: (1) retrospective study was adopted, and the data included in the study were all from the hospital medical record system, which was prone to selection bias and recall bias. The discriminant ability of prediction needed to be confirmed by external tests. Prospective studies are needed in the future to better confirm this conclusion. (2) Due to the limitations of research conditions, this study was a single-center clinical study, so there may be bias in surgical technology, hardware facilities and surgical medication.
Conclusion
In conclusion, HBL was an important component of TBL after THA in elderly women with femoral neck fracture. The patient age, operative time, preoperative blood calcium level, hypertension and osteoporosis were independent risk factors for increased hidden blood loss after THA in elderly women with femoral neck fractures. The differentiation and accuracy of the prediction model of postoperative blood transfusion line diagram constructed by R language software were favorable. Patients at high risk of postoperative transfusion could be screened out in advance according to the prediction model of the nomogram. Moreover, active measures can be taken, such as preoperative reasonable control of patients’ blood pressure and blood calcium level, preoperative application of erythropoietin, perioperative blood dilution and autologous blood transfusion, to reduce the occurrence of postoperative blood transfusion in elderly women with THA.
Funding
This study was supported by the Nature Science Foundation of Jiangsu Province (Grant No: BK20201221), Cross cooperation project of North Jiangsu People’s Hospital (No: SBJC21013) and Jiangsu Province Medical Youth Talent (Grant No: QNRC2016344).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Lasocki S, Krauspe R, von Heymann C, et al. PREPARE: the prevalence of perioperative anaemia and need for patient blood management in elective orthopaedic surgery: a multicentre, observational study. Eur J Anaesthesiol. 2015;32(3):160–167. doi:10.1097/EJA.0000000000000202
2. Liu X, Zhang X, Chen Y, et al. Hidden blood loss after total hip arthroplasty. J Arthroplasty. 2011;26(7):1100–1105.e1101. doi:10.1016/j.arth.2010.11.013
3. Sehat KR, Evans RL, Newman JH. Hidden blood loss following hip and knee arthroplasty. Correct management of blood loss should take hidden loss into account. J Bone Joint Surg Br. 2004;86(4):561–565. doi:10.1302/0301-620X.86B4.14508
4. Pattison E, Protheroe K, Pringle RM, et al. Reduction in haemoglobin after knee joint surgery. Ann Rheum Dis. 1973;32(6):582–584. doi:10.1136/ard.32.6.582
5. Sehat KR, Evans R, Newman JH. How much blood is really lost in total knee arthroplasty? Correct blood loss management should take hidden loss into account. Knee. 2000;7(3):151–155. doi:10.1016/S0968-0160(00)00047-8
6. Nadler SB, Hidalgo JH, Bloch T. Prediction of blood volume in normal human adults. Surgery. 1962;51(2):224–232.
7. Gross JB. Estimating allowable blood loss: corrected for dilution. Anesthesiology. 1983;58(3):277–280. doi:10.1097/00000542-198303000-00016
8. Sizer SC, Cherian JJ, Elmallah RD, et al. Predicting blood loss in total knee and hip arthroplasty. Orthop Clin North Am. 2015;46(4):445–459. doi:10.1016/j.ocl.2015.06.002
9. Liu X, Liu J, Sun G. A comparison of combined intravenous and topical administration of tranexamic acid with intravenous tranexamic acid alone for blood loss reduction after total hip arthroplasty: a meta-analysis. Int J Surg. 2017;41:34–43. doi:10.1016/j.ijsu.2017.03.031
10. Sershon RA, Fillingham YA, Malkani AL, et al. Independent risk factors for transfusion in contemporary revision total hip arthroplasty. J Arthroplasty. 2021;36(8):2921–2926. doi:10.1016/j.arth.2021.03.032
11. Browne JA, Adib F, Brown TE, et al. Transfusion rates are increasing following total hip arthroplasty: risk factors and outcomes. J Arthroplasty. 2013;28(8 Suppl):34–37. doi:10.1016/j.arth.2013.03.035
12. Schwab PE, Lavand’homme P, Yombi JC, et al. Lower blood loss after unicompartmental than total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2015;23(12):3494–3500. doi:10.1007/s00167-014-3188-x
13. Wen L, Jin D, Xie W, et al. Hidden blood loss in anterior cervical fusion surgery: an analysis of risk factors. World Neurosurg. 2018;109:e625–e629. doi:10.1016/j.wneu.2017.10.050
14. Tian S, Li H, Liu M, et al. Dynamic analysis of perioperative hidden blood loss in intertrochanteric fractures. Clin Appl Thromb Hemost. 2019;25:1076029618823279. doi:10.1177/1076029618823279
15. Xu K, Anwaier D, He R, et al. Hidden blood loss after hip hemiarthroplasty using the superPATH approach: a retrospective study. Injury. 2019;50(12):2282–2286. doi:10.1016/j.injury.2019.10.013
16. Miao K, Ni S, Zhou X, et al. Hidden blood loss and its influential factors after total hip arthroplasty. J Orthop Surg Res. 2015;10(1):36. doi:10.1186/s13018-015-0185-9
17. Cushner FD, Friedman RJ. Blood loss in total knee arthroplasty. Clin Orthop Relat Res. 1991;101(269):98–101.
18. Zhang Y, Shen J, Mao Z, et al. [Risk factors of hidden blood loss in internal fixation of intertrochanteric fracture]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2014;28(5):610–614. Chinese.
19. Cai T, Chen D, Wang S, et al. Perioperative hidden blood loss in elderly cervical spondylosis patients with anterior cervical discectomy fusion and influencing factors. Geriatr Orthop Surg Rehabil. 2021;12:21514593211002164. doi:10.1177/21514593211002164
20. Guan JH, Zheng WB, Huang JH, et al. [Analysis of hidden blood loss after percutaneous kyphoplasty for osteoporotic vertebral compression fracture and its influencing factors]. Zhongguo Gu Shang. 2019;32(5):439–443. Chinese. doi:10.3969/j.issn.1003-0034.2019.05.010
21. Lei F, Li Z, He W, et al. Hidden blood loss and the risk factors after posterior lumbar fusion surgery: a retrospective study. Medicine. 2020;99(19):e20103. doi:10.1097/MD.0000000000020103
22. Inoue Y, Miyashita F, Toyoda K, et al. Low serum calcium levels contribute to larger hematoma volume in acute intracerebral hemorrhage. Stroke. 2013;44(7):2004–2006. doi:10.1161/STROKEAHA.113.001187
23. Wan RR, Wang YL, Wu XC, et al. Hidden blood loss and the influencing factors after laparoscopic cholecystectomy. ANZ J Surg. 2020;90(1–2):103–108. doi:10.1111/ans.15502
24. Zhang C, Fan HW, Yi WW, et al. Hidden blood loss and its influential factors after laparoscopy-assisted gastrectomy for gastric cancer. J Laparoendosc Adv Surg Tech A. 2018;28(3):237–241. doi:10.1089/lap.2017.0468
25. Keith I. Anaesthesia and blood loss in total hip replacement. Anaesthesia. 1977;32(5):444–450. doi:10.1111/j.1365-2044.1977.tb09981.x
26. cui H, Chen K, Lv S, et al. An analysis of perioperative hidden blood loss in femoral intertrochanteric fractures: bone density is an important influencing factor. BMC Musculoskelet Disord. 2021;22(1):6. doi:10.1186/s12891-020-03922-x
27. Thienpont E, Grosu I, Paternostre F, et al. The use of patient-specific instruments does not reduce blood loss during minimally invasive total knee arthroplasty? Knee Surg SportsTraumatol Arthrosc. 2015;23(7):2055–2060. doi:10.1007/s00167-014-2952-2
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Predicting Mucosal Healing in Crohn’s Disease: A Nomogram Model Developed from a Retrospective Cohort
Tang N, Chen H, Chen R, Tang W, Zhang H
Journal of Inflammation Research 2022, 15:5515-5525
Published Date: 23 September 2022
A Nomogram for Predicting Vision-Threatening Diabetic Retinopathy Among Mild Diabetic Retinopathy Patients: A Case–Control and Prospective Study of Type 2 Diabetes
Ke J, Li K, Cao B
Diabetes, Metabolic Syndrome and Obesity 2023, 16:275-283
Published Date: 27 January 2023
Development and Validation of a Risk Nomogram Model for Predicting Constipation in Patients with Type 2 Diabetes Mellitus
Yuan HL, Zhang X, Peng DZ, Lin GB, Li HH, Li FX, Lu JJ, Chu WW
Diabetes, Metabolic Syndrome and Obesity 2023, 16:1109-1120
Published Date: 20 April 2023
A Novel Nomogram for the Preoperative Prediction of Edmondson-Steiner Grade III-IV in Hepatocellular Carcinoma Patients
Zhou Z, Cao S, Chen C, Chen J, Xu X, Liu Y, Liu Q, Wang K, Han B, Yin Y
Journal of Hepatocellular Carcinoma 2023, 10:1399-1409
Published Date: 23 August 2023
Risk Factors and Prediction Nomogram of Cognitive Frailty with Diabetes in the Elderly
Deng Y, Li N, Wang Y, Xiong C, Zou X
Diabetes, Metabolic Syndrome and Obesity 2023, 16:3175-3185
Published Date: 16 October 2023
