Back to Journals » International Journal of General Medicine » Volume 15
The Clinical and Biological Manifestations in Women with Iron Deficiency Without Anemia Compared to Iron Deficiency Anemia in a General Internal Medicine Setting: A Retrospective Cohort Study
Authors Hirosawa T , Hayashi A, Harada Y , Shimizu T
Received 27 May 2022
Accepted for publication 16 August 2022
Published 23 August 2022 Volume 2022:15 Pages 6765—6773
DOI https://doi.org/10.2147/IJGM.S376405
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Takanobu Hirosawa, Arisa Hayashi, Yukinori Harada, Taro Shimizu
Department of Diagnostic and Generalist Medicine, Dokkyo Medical University, Tochigi, Japan
Correspondence: Taro Shimizu, Department of Diagnostic and Generalist Medicine, Dokkyo Medical University, 880 Kitakobayashi, Mibu-cho, Shimotsuga, Tochigi, 321-0293, Japan, Tel + 81 282 87 2498, Fax + 81-282-87-2502, Email [email protected]
Purpose: The clinical presentation of iron deficiency is not well understood. We aimed to identify the clinical manifestations of iron deficiency without anemia in women.
Patients and Methods: We conducted a retrospective cohort study of women who visited the general internal medicine outpatient department of a university hospital in Japan between 2016 and 2022. Women who were prescribed iron supplements were included in the study. Anemia was defined as hemoglobin levels below 12 g/dl. Iron deficiency was defined as serum ferritin levels < 30.0 μg/l. The primary outcome was the difference in symptoms between patients with iron deficiency with and without anemia. The secondary outcome was the ratio of symptom, hemoglobin, and serum ferritin improvement (levels > 30.0 μg/l after treatment), comparing the measurements at the beginning and after supplementation.
Results: A total of 147 women were included in the final analysis. There were no significant differences in the initial symptoms and the ratio of symptom improvement between the groups. Compared to patients with iron deficiency anemia, patients with iron deficiency without anemia had high initial serum ferritin levels (14.8 vs 7.1 μg/l, p< 0.001), and hemoglobin (13.2 vs 9.9 g/dl, p< 0.001). Iron supplements significantly improved the serum ferritin level in two groups and the hemoglobin in iron deficiency anemia. After treatment, iron deficiency without anemia still had high serum ferritin levels (37.7 vs 28.2 μg/l, p=0.017) and hemoglobin (13.3 vs 12.3 g/dl, p < 0.001).
Conclusion: There were no differences in any of the investigated symptoms and the ratio of the symptom improvement depending on the anemic state in iron deficiency. After iron supplementation, the serum ferritin levels in the iron deficiency without anemia group improved. Hemoglobin and serum ferritin in iron deficiency without anemia were still highly comparable to that of iron deficiency anemia.
Keywords: women, hemoglobin, iron deficiency without anemia, serum ferritin
Introduction
Iron deficiency is a common form of nutritional deficiency worldwide.1,2 The overall mean prevalence of iron deficiency is > 20%.3 Although more common in developing countries, the estimated prevalence of iron deficiency was 9–16% in young females in the United States in 1999–2000.4 Classification of iron deficiency without anemia or iron deficiency with anemia is based on hemoglobin levels. Hemoglobin levels below 12 g/dl in women is conventionally defined as anemia by the World Health Organization.5 Approximately half of all anemia cases are caused by iron deficiency.5 Iron deficiency anemia is a late manifestation of iron deficiency, with a clear predominance in adolescents and menstruating females.6
Iron deficiency is a multisystem condition with a wide range of clinical manifestations, including reduced cognitive function,7–9 poor physical performance,10 pica, restless legs syndrome, and impaired immunological function.11 Anemia is an extreme manifestation of iron deficiency. Even without anemia, fatigue can be observed in people with iron deficiency.12 Iron deficiency is defined when an abnormal value is detected in at least two of the following three indicators: serum ferritin, transferrin saturation, and free erythrocyte protoporphyrin.4 Serum ferritin concentration is the most sensitive and specific test used for iron deficiency.13 The utility of the red cell distribution width, and mean corpuscular volume in diagnosing iron deficiency has also been reported.14 These characteristics, observed in complete blood counts, could be markers of iron deficiency and would help the study of iron kinetics to be considered in general clinical practice. Iron deficiency without anemia may be challenging to diagnose because of its nonspecific symptoms and the lack of awareness of the existence of such a variety in healthcare providers.
In our general internal medicine department, some of the women presenting with a variety of symptoms, including fatigue, who were undiagnosed after the usual clinic-based investigation were eventually diagnosed with iron deficiency without anemia. Iron supplementation occasionally improves the symptoms, especially fatigue.15,16 Since iron deficiency anemia is an extreme form of iron deficiency, diagnosing iron deficiency without anemia before it progresses to iron deficiency anemia will have a positive effect on the subsequent clinical consequences. Clinicians could detect iron deficiency early on by focusing on the manifestations caused by iron deficiency without anemia. However, these clinical and biological manifestations are not known well. Therefore, we investigated the differences in clinical and biological symptoms depending on the anemic state of iron deficiency. We also attempted to evaluate whether the effect of iron supplementation intervention on iron deficiency without anemia would be different from the effect of iron supplementation intervention on iron deficiency anemia.
Materials and Methods
This retrospective, single-center cohort study included all women who were prescribed iron supplementation in the general internal medicine outpatient department (Department of Diagnostic and Generalist of Medicine) of Dokkyo Medical University Hospital, Mibu, Tochigi, Japan, from April 1, 2016 to March 31, 2022. The institution is a tertiary teaching hospital. This study was conducted in accordance with the current version of the Declaration of Helsinki. The protocol was approved by the Ethics Committee of Dokkyo Medical University (No. R-56-13J). As this was a retrospective cohort study, and the study data were anonymous, the requirement for informed consent was waived by the ethics committee.
Patient Population
Of 187 women aged > 15 years who were prescribed iron supplementation in the general internal medicine department during the study period, 16 were excluded because of iron supplement use within two weeks prior to the index visit. A further 11 women were excluded because their serum ferritin levels were > 30 μg/l (2 for viral infection, 2 collagen disease, 1 menopause, 1 ulcer colitis, 1 post bleeding, 1 anxiety disorder, 3 unknown). Eight women were excluded because of blood transfusion therapy within two weeks prior to the index visit. Five other women were excluded because of the lack of data. In total, 147 women were enrolled in this study. A flow diagram of the patient selection is shown in Figure 1. All iron supplements were prescribed at the discretion of the treating doctor.
 |
Figure 1 Flowchart of patient inclusion and exclusion in the study. |
Definition and Outcome
Anemia was assessed using hemoglobin, hematocrit, and complete blood count. In this study, we defined hemoglobin levels below 12 g/dl for women, according to the World Health Organization.5
Iron deficiency was defined as an abnormal value for at least two of the following three indicators: serum ferritin, transferrin saturation, and free erythrocyte protoporphyrin.4 Serum ferritin concentration is the most sensitive and specific test used for iron deficiency (without inflammation), with levels less than 30 µg/l being generally indicative of low body iron stores.13 Therefore, we defined iron deficiency as a serum ferritin level < 30 µg/l in this study. Iron supplementation included ferrous fumarate, sodium ferrous citrate, dried ferrous sulfate, and ferric pyrophosphate.
The primary study outcome was the difference in the symptoms between the iron deficiency without anemia and iron deficiency anemia groups. The secondary outcome was the ratio of symptom, hemoglobin, and serum ferritin improvement, comparing the measurements at the beginning and after supplementation. We defined symptom improvement as any symptom improving within 12 weeks of treatment with iron supplementation. We collected the latest laboratory data following iron supplementation as post-treatment data. Improvement in serum ferritin was defined as serum ferritin levels above 30 µg/l within 12 weeks of treatment with iron supplementation.
Data Collection
Data collected was for the purpose of conducting this study. The patients’ medical records were reviewed by the primary researcher (TH). Another researcher (AH) independently double-checked the symptom classification17 and clinical course. In cases of disagreement, both researchers discussed together to decide the final judgment. All data were collected by the treating doctors in the context of clinical management. The baseline characteristics included age. We collected data on the presence of the following symptoms: fatigue, muscle pain/joint pain, dizziness/vertigo, menorrhea, headache, anorexia, body weight loss, fever, palpitations, dyspnea, insomnia, edema, anxiety/depressive mood, hair loss, heartburn, pica, genital bleeding, melena, and memory loss. For symptoms and hemoglobin levels, the data up to 12 weeks prior to the index visit were included in the analysis. Laboratory findings for iron deficiency assessment included hematocrit, red blood cell count, mean corpuscular volume, mean corpuscular hemoglobin, mean corpuscular hemoglobin concentration, red cell distribution width, transferrin saturation, iron, unsaturated iron-binding capacity, total iron-binding capacity, white blood cells, platelets, C-reactive protein, erythrocyte sedimentation rate, serum folate, serum vitamin B12, and thyroid-stimulating hormone. All laboratory data were analyzed using automated methods.
Analysis
First, we compared the baseline characteristics between iron deficiency without anemia and iron deficiency with anemia. Then, we analyzed the change after treatment for symptoms and laboratory data of both groups.
Continuous variables are presented as medians and standard deviation (SD) or interquartile ranges (IQR) and were compared using the Mann–Whitney U-test. Categorical or binary variables are presented as numbers and were compared using the chi-squared test. A statistical power analysis was performed using the program G*power version 3.1.9.6 (Department of Psychology of Heinrich Heine University Düsseldorf, Düsseldorf, Germany). Statistical significance was set at P-value < 0.05. All statistical tests were performed using R 3.6.0 for MacOS X (The R Foundation for Statistical Computing, Vienna, Austria).
Results
Baseline characteristics and symptoms were not different between patients with ferritin > 30 μg/l (N=11) and patients with ferritin < 30 μg/l (N=147), except for edema (5/11 [45.6%] vs 15/147 [10.2%], p<0.001) and menorrhea (0/11 [0%] vs 44/147 [29.9%], p=0.034).
In total, 147 women were enrolled in the final analysis. Of these, the mean age of all patients was 41.5 ± 15.6 (SD) years. Fifty-five patients (55/147, 37.4%) complained of fatigue. The mean hemoglobin level was 11.6 ± 1.9 g/dl, while the mean serum ferritin level was 11.1 ± 9.1 μg/l. Ferrous fumarate was the most frequently prescribed iron supplement (68/147, 46.3%), followed by sodium ferrous citrate (46/147, 31.3%), dried ferrous sulfate (24/147, 16.3%), and ferric pyrophosphate (9/147, 6.1%). The median duration of iron supplementation was 106 (IQR 32–150) days.
Anemia was not observed in 77 patients (77/147, 52.3%) during the study period. The baseline characteristics and symptoms of the patients with iron deficiency without anemia and iron deficiency anemia are shown in Table 1. There were no significant differences between the groups in age (mean age 38.6 vs 44.7, p=0.46), the prevalence of fatigue (31/77 [40.3%] vs 24/70 [34.2%], p=0.46), muscle pain or joint pain (25/77 [32.5%] vs 21/70 [30.0%], p=0.75), dizziness or vertigo (26/77 [33.8%] vs 19/70 [27.1%], p=0.39), menorrhea (21/77 [27.3%] vs 23/70 [32.9%], p=0.46), headache (22/77 [28.6%] vs 19/70 [27.1%], p=0.85), anorexia (16/77 [20.8%] vs 15/70 [21.4%], p=0.93), body weight loss (16/77 [20.8%] vs 12/70 [17.1%], p=0.58), and fever (12/77 [15.6%] vs 16/70 [22.9%], p=0.26).
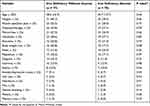 |
Table 1 Baseline and Symptoms of the Iron Deficiency Without Anemia Group Compared to the Iron Deficiency with Anemia Group |
The details of the complete blood counts are shown in Table 2. Compared to patients with iron deficiency anemia, the hemoglobin (mean 13.2 vs 9.9, p< 0.001), hematocrit (40.2 vs 32.7, p< 0.001), the red blood cells (4.57 vs 4.23, p< 0.001), mean corpuscular volume (88.2 vs 78.0, p< 0.001), mean corpuscular hemoglobin (28.9 vs 23.7, p< 0.001), and mean corpuscular hemoglobin concentration (32.7 vs 30.3, p< 0.001) of the iron deficiency without anemia group were high. Meanwhile, the red cell distribution width (13.5 vs 16.4, p< 0.001) and platelet count (290 vs 338, p=0.0045) in the iron deficiency without anemia group were low.
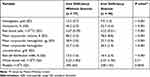 |
Table 2 Complete Blood Count Comparison Between Those with Iron Deficiency with and without Anemia |
The details of the laboratory tests are shown in Table 3. Compared with patients with iron deficiency anemia, the initial serum ferritin (mean 14.8 vs 7.1, p< 0.001), serum iron (80.1 vs 26.8, p< 0.001), and serum transferrin saturation (22.3 vs 5.9, p< 0.001) of the iron deficiency without anemia group were high. The total iron-binding capacity (mean 388 vs 414, p=0.0049), the unsaturated iron-binding capacity (311 vs 390, p< 0.001) and erythrocyte sedimentation rate (13.4 vs 24.0, p=0.003) of the patients with iron deficiency without anemia were low.
 |
Table 3 Laboratory Findings of Those with Iron Deficiency with and without Anemia |
The change in symptoms and laboratory data before and after treatment are shown in Table 4. The change in hemoglobin and serum ferritin before and after treatment for the iron deficiency without anemia group and the iron deficiency with anemia group are shown in Figures 2 and 3, respectively. Iron supplementation improved hemoglobin in iron deficiency anemia (mean 9.9 to 12.3, p<0.001) and mean corpuscular volume (78.0 to 84.9, p<0.001). It also improved serum ferritin in iron deficiency without anemia (14.8 to 37.7, p<0.001) and iron deficiency anemia (7.1 to 28.2, p<0.001). After treatment, hemoglobin (mean 13.3 vs 12.3, p < 0.001), mean corpuscular volume (89.4 vs 84.9, p=0.024), and serum ferritin (37.7 vs 28.2, p= 0.017) with iron deficiency without anemia were still highly comparable to patients with iron deficiency anemia. Red cell distribution width (13.4 vs 17.7, p<0.001) with iron deficiency without anemia was still low compared to iron deficiency anemia. There were no significant differences between the groups in terms of symptom improvement (46/77 [59.7%] vs 43/70 [61.4%], p=0.75) and the ratio of serum ferritin improvement (33/53 [62.3%] vs 20/53 [37.7], p= 0.07).
 |
Table 4 Changes After Treatment for Symptoms and Laboratory Data of Those with Iron Deficiency with and without Anemia |
 |
Figure 2 Change in hemoglobin by treatment of those with iron deficiency with and without anemia. Abbreviations: ID, iron deficiency; w/o, without; w/, with; IQR, interquartile range. |
 |
Figure 3 Serum ferritin change by treatment of those with iron deficiency with and without anemia. Abbreviations: ID, iron deficiency; w/o, without; w/, with; IQR, interquartile range. |
There were no significant differences in terms of the type of iron supplementation or duration of prescription between the groups. The details of the treatments are shown in Supplementary Table 1.
Power analysis revealed that the statistical power for comparing symptom improvement between both groups was 0.06. However, corresponding values in hemoglobin, serum ferritin, and serum ferritin improvement exceeded 0.99.
Discussion
This study has several main findings. First, there were no differences in any of the investigated symptoms and the ratio of symptom improvement depending on the anemic state. This suggests that the symptoms studied are not related to the severity of iron deficiency. In future studies, iron deficiency and non-iron deficiency should be compared in a nonanemic population, especially for edema and menorrhea. The relationship of each symptom with iron deficiency should be clarified. Second, biological data suggested that iron deficiency anemia is an extreme form of iron deficiency.6,13 Smaller red blood cell indices, higher red cell distribution, and higher platelet counts of iron deficiency anemia suggested a bone marrow response to anemia. Third, iron supplements improved serum ferritin levels in both groups and hemoglobin in iron deficiency anemia. However, hemoglobin, mean corpuscular volume and ferritin were still high (approximately 1.0 g/dl, 5 femtoliters, and 10 µg/l, respectively) and red cell distribution width was still low (approximately 5%) in iron deficiency without anemia compared to those of iron deficiency anemia. This could be because iron deficiency anemia is a severe manifestation of iron deficiency and may require a longer treatment period. These findings suggest that the early detection of iron deficiency would require a shorter duration of iron supplementation to normalize biological manifestations than iron deficiency anemia.
Red cell distribution width > 15% and mean corpuscular volume < 80 femtoliters are useful in diagnosing iron deficiency anemia in hospitalized patients.14 In this study, we also found similar results in the outpatient setting. Additionally, iron supplements reduced the mean corpuscular volume in iron deficiency anemia (approximately 7 femtoliters), but not the red cell distribution width. This suggested that the change in mean corpuscular volume could be used as an indicator to evaluate the efficacy of the ongoing treatment; these findings are similar to the results of the previous study.14
Iron supplementation reportedly decreases fatigue by 48% in non-anemic women with iron deficiency.16 Although a simple comparison is not accurate due to the differences in symptom evaluation and the lower serum ferritin cut-off levels (< 30 μg/l in ours vs < 50 μg/l in the previous study), the symptom improvement in our study (46% in iron deficiency without anemia) was similar to that of the previous study. This suggested that iron supplements could improve the investigated symptoms including fatigue.
This study had several limitations. First, as it was conducted in a single department at a single center, these results cannot be easily generalized to other settings. Fully powered research is required, especially for further investigating symptoms. Second, the treating doctors decided to investigate iron supplementation and other nutritional deficiencies and prescribed iron supplementation (including the interval) without clear criteria. Hence, 21.4% of iron supplementation cases were excluded. Therefore, there may have been selection bias when excluding cases of severe iron deficiency anemia with recent iron supplementation and blood transfusion. The bias may lead the difference of the investigated symptoms in both groups smaller. Third, we did not assess the change in symptoms in formatted questionnaires, such as the Likert scale, visual analog scale,14 or the multidimensional assessment of fatigue score.15 Fourth, we did not investigate the cost-effectiveness of the diagnosis and treatment of iron deficiency without anemia. In future studies, it would be necessary to investigate the cost-effectiveness of iron deficiency without anemia in the appropriate setting. Fifth, we did not compare iron deficiency and normal iron status. Therefore, we could not justify the link between iron deficiency and the investigated symptoms. The investigated symptoms could be the cause of either iron deficiency or anemia. For example, menorrhea, bleeding, or fever would be the cause of anemia.1 Therefore, in future studies the cause-effect association should be investigated.
Conclusion
There were no differences in any of the investigated symptoms or in the ratio of the symptom improvement depending on the anemic state of the patients with iron deficiency. After iron supplementation, the serum ferritin levels in the iron deficiency without anemia group improved. Hemoglobin and serum ferritin in iron deficiency without anemia were still high compared to that of iron deficiency anemia. Further studies that compare patients with iron deficiency and those with normal iron levels are required to validate the link between iron deficiency and the investigated symptoms.
Data Sharing Statement
The data used to support the findings of this study have not been made available for protection of privacy.
Acknowledgments
This study was made possible by using the resources from the Department of Diagnostic and Generalist Medicine, Dokkyo Medical University.
Funding
This work was supported by the Chairman’s Special Support from the Dokkyo Medical University Alumni Association (No: 0001).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Snook J, Bhala N, Beales ILP, et al. British Society of Gastroenterology guidelines for the management of iron deficiency anaemia in adults. Gut. 2021;70(11):2030–2051. doi:10.1136/gutjnl-2021-325210
2. United Nations. Administrative committee on coordination. Subcommittee on nutrition. Fourth Report on the World Nutrition Situation. Nutrition Throughout the Life Cycle; 2000.
3. Petry N, Olofin I, Hurrell RF, et al. The proportion of anemia associated with iron deficiency in low, medium, and high human development index countries: a systematic analysis of national surveys. Nutrients. 2016;8(11):693. doi:10.3390/nu8110693
4. Centers for Disease Control and Prevention (CDC). Iron deficiency—United States, 1999–2000. MMWR Morb Mortal Wkly Rep. 2002;51(40):897–899. PMID: 12418542.
5. World Health Organization. The Global Prevalence of Anaemia in 2011. Geneva: World Health Organization; 2015.
6. Clénin GE. The treatment of iron deficiency without anaemia (in otherwise healthy persons). Swiss Med Wkly. 2017;147:w14434. doi:10.4414/smw.2017.14434
7. Jáuregui-Lobera I. Iron deficiency and cognitive functions. Neuropsychiatr Dis Treat. 2014;10:2087–2095. doi:10.2147/NDT.S72491
8. Halterman JS, Kaczorowski JM, Aligne CA, Auinger P, Szilagyi PG. Iron deficiency and cognitive achievement among school-aged children and adolescents in the United States. Pediatrics. 2001;107(6):1381–1386. doi:10.1542/peds.107.6.1381
9. Bruner AB, Joffe A, Duggan AK, Casella JF, Brandt J. Randomised study of cognitive effects of iron supplementation in non-anaemic iron-deficient adolescent girls. Lancet. 1996;348(9033):992–996. doi:10.1016/S0140-6736(96)02341-0
10. Brownlie IVT, Utermohlen V, Hinton PS, Haas JD. Tissue iron deficiency without anemia impairs adaptation in endurance capacity after aerobic training in previously untrained women. Am J Clin Nutr. 2004;79(3):437–443. doi:10.1093/ajcn/79.3.437
11. Powers JM, Buchanan GR. Diagnosis and management of iron deficiency anemia. Hematol Oncol Clin North Am. 2014;28(4):
12. Houston BL, Hurrie D, Graham J, et al. Efficacy of iron supplementation on fatigue and physical capacity in non-anaemic iron-deficient adults: a systematic review of randomised controlled trials. BMJ Open. 2018;8(4):e019240. doi:10.1136/bmjopen-2017-019240
13. Camaschella C. Iron-deficiency anemia. N Engl J Med. 2015;372(19):1832–1843. doi:10.1056/NEJMra1401038
14. Thompson WG, Meola T, Lipkin M Jr, Freedman ML. Red cell distribution width, mean corpuscular volume, and transferrin saturation in the diagnosis of iron deficiency. Arch Intern Med. 1988;148(10):2128–2130. doi:10.1001/archinte.1988.00380100026006
15. Verdon F, Burnand B, Stubi CLF, et al. Iron supplementation for unexplained fatigue in non-anaemic women: double blind randomised placebo controlled trial. BMJ. 2003;326(7399):1124. doi:10.1136/bmj.326.7399.1124
16. Vaucher P, Druais PL, Waldvogel S, Favrat B. Effect of iron supplementation on fatigue in nonanemic menstruating women with low ferritin: a randomized controlled trial. Can Med Assoc J. 2012;184(11):1247–1254. doi:10.1503/cmaj.110950
17. Pasricha SR, Tye-Din J, Muckenthaler MU, Swinkels DW. Iron deficiency. Lancet. 2021;397(10270):233–248. doi:10.1016/S0140-6736(20)32594-0
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Evaluation of Minimal Optimal Dose of Intravenous Ferric Carboxymaltose for Treatment of Iron Deficiency Anemia and Risk of Transient Hyperferritinemia
Alharbi AA, Alharbi AA, Bashen DS, Owaidah T
Journal of Blood Medicine 2022, 13:681-690
Published Date: 17 November 2022
Iron Deficiency and Blood Donation: Links, Risks and Management
Mantadakis E, Panagopoulou P, Kontekaki E, Bezirgiannidou Z, Martinis G
Journal of Blood Medicine 2022, 13:775-786
Published Date: 10 December 2022
Anemia and Associated Risk Factors in Pediatric Patients
Martinez-Torres V, Torres N, Davis JA, Corrales-Medina FF
Pediatric Health, Medicine and Therapeutics 2023, 14:267-280
Published Date: 4 September 2023
Assessing Nutritional Anemia Among University Students in Jazan, Saudi Arabia: A Public Health Perspective
Hakami W, Dobie G, Alneami KA, Shaabi M, Essawi K, Saboor M, Madkhali AM, Nahari MH, Almasoudi HH, Akhter MS, Hakami FH, Zarbatan FA, Hakamy A, Chandika RM, Fageehi AA, Mobarki AA, Hamali HA
Journal of Blood Medicine 2024, 15:51-60
Published Date: 9 February 2024
Anemia in Heart Failure: A Perspective from 20-Year Bibliometric Analysis
Yang Q, Dong T, Lyu D, Xue D, Zhuang R, Ma L, Zhang L
International Journal of General Medicine 2024, 17:1845-1860
Published Date: 2 May 2024
