Back to Journals » Journal of Blood Medicine » Volume 13
Evaluation of Minimal Optimal Dose of Intravenous Ferric Carboxymaltose for Treatment of Iron Deficiency Anemia and Risk of Transient Hyperferritinemia
Authors Alharbi AA, Alharbi AA, Bashen DS , Owaidah T
Received 15 May 2022
Accepted for publication 21 October 2022
Published 17 November 2022 Volume 2022:13 Pages 681—690
DOI https://doi.org/10.2147/JBM.S374780
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Martin H Bluth
Ahmad A Alharbi,1,2 Abdullah A Alharbi,2,3 Dhafer Salem Bashen,2 Tarek Owaidah4
1Pathology Department, College of Medicine, Majmaah University, Al Majmaah 11952, Riyadh, Kingdom of Saudi Arabia; 2Laboratory Department, Dr. Sulaiman Al-Habib Hospital in Al Takhassusi, Riyadh, Kingdom of Saudi Arabia; 3Pathology Department, College of Medicine, Imam Muhammad Ibn Saud Islamic University, Riyadh, Kingdom of Saudi Arabia; 4Hematology and Transfusion Medicine Department, Alfaisal University, Riyadh, Kingdom of Saudi Arabia
Correspondence: Tarek Owaidah, Consultant Hematology and Transfusion Medicine, Alfaisal University, P.O.Box 5092, Riyadh, 11533, Kingdom of Saudi Arabia, Tel +966 50 531 2925, Email [email protected]
Background: Iron supplementation is administered orally or intravenously to treat iron-deficiency anemia (IDA). Ferric Carboxymaltose (FCM) “Ferinject®” is an intravenous (IV) iron preparation that has emerged as a safe therapeutic option for treating IDA in the past decade.
Aim: This study aimed to evaluate safety and efficacy of carboxymaltose in a cohort of patients with IDA not responding to oral therapy.
Methods: This 12-month retrospective study included 106 patients with IDA, with-or without bariatric surgery, who received (single or multiple doses) of Carboxymaltose 500mg/10mL. Data points included patients’ demographics, baseline data for Hb, platelet, ferritin, and MCV pre–and at 1, 2, and 3 months following different doses of IV-Carboxymaltose. Changes in Hb, MCV, platelets, and ferritin levels were recorded in response to Carboxymaltose to assess the optimal dose, risk of hyperferritinemia, and hypophosphatemia.
Results: At three months (95 days) follow-up, the median change pre-and post-therapy in hemoglobin was from 9.5 to 11.9g/dL (p < 0.01), MCV 73.6– 80.5fL (p < 0.01), and ferritin 5.3– 93.8ng/mL. A significant difference was observed between platelet count of patients who underwent bariatric surgery and those who did not. An optimal ferritin response (> 30ng/mL) was observed in 87.8% of patients who received first dose, and none of the full three doses showed no response. 37% of patients who received two doses developed hyperferritinemia. Serum phosphate levels were assessed in 28 cases, and hypophosphatemia was observed in 25% of these patients.
Conclusion: Carboxymaltose is a reliable option for IDA. IV-FCM therapy helps achieve significant improvement in hemoglobin concentration and MCV from the first dose carrying a low reversible risk of hyperferritinemia following multiple doses. An interesting finding of this study is the discovery of a population of IDA patients requiring periodic assessment for iron reinfusion to sustain normal levels, mostly post-bariatric surgery. Changes in serum phosphate levels reported to occur consecutively with FCM treatment should be further studied.
Keywords: iron deficiency, anemia, ferrous carboxymaltose, hypophosphatemia
Impact of Findings on Practice Statements
● We identified the minimal optimal dose of Ferric Carboxymaltose for correcting anemia, which may be helpful in clinical practice in managing noncompliant patients.
● The hyperferritinemia which developed after multiple dose infusion proved to be transient, and resolved at follow-up. This should minimize the concerns among physicians and patients.
● Hypophosphatemia developing in a small portion of the cohort after infusion also proved to be transient on follow-up.
Introduction
Optimal iron balance plays a critical role in disease management, as iron is an integral component of hemoglobin-mediated oxygen transport essential for survival and health. Iron deficiency is a major cause of anemia, affecting one-third of the world population,1 while 50% of anemia cases worldwide are due to iron deficiency anemia (IDA).2 Iron deficiency can be absolute (lack of total iron stores in the body) or functional (impaired iron bioavailability).3 Usually, iron deficiency develops gradually and does not have clinically apparent symptoms until anemia becomes severe. IDA is the fifth leading cause of disability, affecting 1.24 billion people.1 Iron deficiency results from prolonged iron imbalance due to nutritional deficiency, impaired iron absorption, worm infestations, chronic blood loss, or multiple pregnancies.4
Oral or intravenous (IV) iron supplementation or rarely blood transfusion is prescribed to combat iron deficiency. The oral route of iron administration is historically favorable; however, in addition to stomach upset including (pain, bloating and sometimes vomiting) and constipation side effects, poor absorption and compliance can compromise the effectiveness of the interventions. Second, there are multiple risks associated with blood transfusion, including transmission of infections such as human immunodeficiency virus, mismatched transfusions, immune modulation, and other risks.5 IV iron therapy is safe and more cost-effective than blood transfusion and overcomes the many hurdles faced by oral supplementation, such as poor absorption and gastrointestinal side effects with few side effects mainly allergic reactions.
The prevalence of anemia in Europe is around 20%.6 In contrast, regional studies on anemia present varied results, with the prevalence of anemia in adolescents in the Kingdom of Saudi Arabia (KSA) as 16–34%.7 IDA is the most common cause of anemia, especially among females, in KSA. However, the prevalence of IDA is not well established by epidemiological surveys in KSA, with reports limited to single institutes with specific age groups or gender indicating a wide 6–56% prevalence.8–12 In a recent multicenter epidemiological study, the prevalence of IDA was found to be 10.7% among Saudi university students.13
Aim
Although iron supplementation is often prescribed, the most effective route for this patient population is unclear to attain stable hemoglobin (Hb) levels. Therefore, the current study aimed to describe the response to IV iron in different approved doses. It also estimates the minimal optimal dose and the risk of hyperferritinemia through evaluating the efficacy and safety of IV iron supplementation (carboxymaltose) with its effect on Hb, Mean Corpuscular Volume (MCV), ferritin, and platelet levels in IDA patients in both bariatric and non-bariatric subgroups and evaluate the related health conditions such as menorrhagia, ulcerative colitis, anticoagulation or thalassemia.
Methodology
Study Design and Data Collection
This retrospective study was approved by our institutional review board. The inclusion criteria were age >18 years with a confirmed IDA diagnosis based on Hb <12 g/dL for women and <13 g/dL for men with ferritin levels <30 ng/mL, who could not tolerate oral iron or had poor response defined with no improvement after 2-month therapy.
This study was conducted in a hematology outpatient clinic for 12 months at a major secondary care center, where data was collected from the medical records system for 106 patients with IDA who received (single or multiple doses) of Carboxymaltose “Ferinject®” 500 mg/10 mL at a dose of 500mg in 200 mL normal saline over 30 minutes. A total of 94 (88.7%) patients were included in the statistical analysis, while 12 (11.3%) patients were excluded from the analysis because they had no follow-up data for the primary efficacy endpoint assessment. Data points included patients’ demographics and baseline data for Hb, platelet, ferritin, and MCV pre– and at 1, 2, and 3 months following different doses of IV Carboxymaltose.
Statistical Methods
Categorical variables are presented as counts and percentages (eg, sex, bariatric surgery, medical history, and total administered dose of IV iron). Numerical variables are presented as means and standard deviations if normally distributed (eg, age). Laboratory results are presented as the median, interquartile range (IQR), and range. The Wilcoxon signed-rank test was used to compare the laboratory values pre- and post-therapy with Carboxymaltose “Ferinject”. The magnitude of change was recorded for laboratory results such as Hb, MCV, platelets, and ferritin in response to different doses of Carboxymaltose to assess the optimal dose, risk of hyperferritinemia, and hypophosphatemia as an outcome. The magnitude of change was compared between the subgroups (age groups, bariatric surgery, and total administered dose) using the Kruskal–Wallis test. Statistically significance was set at p < 0.05. IBM SPSS (Statistical Package for the Social Sciences; IBM Corp, Armonk, NY, USA) was used to perform all statistical calculations, version 21 for Microsoft Windows. No data imputation was carried out for missing data.
Results
The mean age of the cohort was 37 ±12.3 years. There was a female preponderance, with 95.7% of subjects being female. The median pre-therapy Hb concentration and MCV in our subjects were 9.5 g/dL and 73.6 fL, respectively, which increased to 11.9 g/dL and 80.5 fL post-therapy. Of our cohort, 3.2% had menorrhagia, 4.3% were on anticoagulants with bleeding, and 2.1% had a concomitant vitamin B12 deficiency. 39.4% of subjects received one dose, 53.2% received two doses, and 7.4% received three doses of Carboxymaltose “Ferinject” 500 mg/10 mL. Only 32 (34%) patients underwent bariatric surgery (Table 1).
 |
Table 1 Socio-Demographic Variables |
A median (IQR) increase of 1.8 (2.5) g/dL was observed in hemoglobin levels. The median change observed after three months of follow-up among patients who received three doses of IV iron was significantly higher (p = 0.003) than those who received one or two doses of IV iron (Table 2). However, no significant difference was found between patients who underwent bariatric surgery and those who did not (p = 0.655). Similar to bariatric surgery, no significant difference was found between the different age groups regarding the increase in Hb levels (p = 0.481). Among the total population, the median hemoglobin concentration pre and post treatment was significantly increased from 9.5 g/dL to 11.9 g/dL (p < 0.01) after almost three months (95 days) of follow-up (Table 2).
 |
Table 2 Hemoglobin Level (g/dl) Before and After Treatment in the Total Population and in the Different Subgroups |
Among the total population, the median MCV was significantly increased from 73.6 fL to 80.5 fL (p < 0.01) after almost three months (95 days). A statistically significant increase was observed among all subgroups. Further assessment after 133 days (~ 4.5 months) post-baseline showed a median (IQR) MCV of 82.3 (12.3) fL with a significant increase from the first post-baseline assessment (p < 0.001) (S1).
A significant drop in the median platelet count from 301.5–272 ×109/L was observed among the total population after almost three months (95 days) of the therapy, regardless of the age group or bariatric surgery (p < 0.05). The total administered doses of IV iron were found to significantly affect the decrease in platelet count in patients who received two doses of IV iron, showing a significant drop in their median platelet count (p < 0.001), while those receiving one did not show a significant drop (p = 0.502). The sample size of those receiving three doses was much smaller than that of their single- or double-dose counterparts; hence, the statistical comparison was not significant (p = 0.236). Further assessment of platelet count after 133 days (≈ 4.5 months) post-baseline revealed a median (IQR) value of 242 (65.0) ×109/L with a statistically non-significant decrease from the first post-baseline assessment (p = 0.935) (Tables 3, S2).
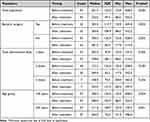 |
Table 3 Platelets Counts Before and After 3 Months Treatment in the Total Population and the Different Subgroups |
Among the total population, the median ferritin level was significantly increased from 5.3 ng/mL to 93.8 ng/mL (p < 0.01) at three months (95 days). A statistically significant increase was observed among all subgroups (Figure 1). In a subgroup analysis of patients who received a single dose of Ferric Carboxymaltose (FCM), the assessment of ferritin level 133 days (~ 4.5 months) post-baseline showed a median (IQR) of 17.5 (30.1) ng/mL with a significant decrease from the first post-baseline assessment (p < 0.047) (Tables 4, S3).
 |
Table 4 Ferritin Level (ng/mL) Before and After 3 Months Treatment in the Total Population and the Different Subgroups Descriptive |
 |
Figure 1 Median Ferritin level (ng/mL) before and after treatment. |
In a subgroup analysis, we found that 37% of the patients who received two doses developed hyperferritinemia. Of these, 19.6% had ferritin levels <300 ng/mL, whereas 17.4% had ferritin levels >300 ng/mL. Approximately 9.1% of patients receiving one dose developed hyperferritinemia, but the level in all patients was <300 ng/mL. Among those who received the three doses, 57.1% developed hyperferritinemia, with 28.6% having >300 ng/mL. An optimal ferritin response (>30 ng/mL) was observed in 87.8% of the patients receiving one dose. This can be explained by the fact that the first dose was successfully administered to most of the patients, while the second and third dose was given to a portion of the cohort. One dose was insufficient to replenish ferritin stores in 3% of the patients, while none of the other full three doses resulted in nonresponse (Tables 5, S5). Serum phosphate levels were assessed in 28 patients 3-months post-infusion, of which seven (25%) had hypophosphatemia. Of the patients in whom the assessment was performed, four patients (14.3%) received one dose, two patients (7.1%) received two doses and only one patient (3.6%) received three doses.
 |
Table 5 Comparing the Prevalence of Hyperferritinemia Between the Different Doses |
A median (IQR) increase of 5.8 (10.9) fL was observed in the MCV level. The median change observed among patients who received three doses of IV iron was significantly higher (p = 0.036) than that observed among patients who received one or two doses of IV iron. On the other hand, no significant difference was found between patients who underwent bariatric surgery and those who did not undergo bariatric surgery (p = 0.191). Like bariatric surgeries, no significant difference was found between the different age groups with respect to the increase in the MCV level (p = 0.889) (S4).
A median (IQR) decrease of 29.5 (72.)3 ×109/L was observed in platelet count. The median decrease observed among patients who received two doses of IV iron was significantly higher (p = 0.024) than that observed among patients who received one dose of IV iron. The sample size of those receiving three doses was much smaller than that of their single- or double-dose counterparts; hence, the statistical comparison was not significant. However, no significant difference was found between patients who underwent bariatric surgery and those who did not undergo bariatric surgery (p = 0.503). Similar to bariatric surgeries, no significant difference was found between the different age groups regarding the decrease in platelet count (p = 0.254) (S2).
Changes were observed in ferritin level after the first dose with a median (IQR) increase of 59.6 (193.2) ng/mL. The median change observed among patients who received three doses of IV iron was significantly higher (p < 0.001) than that observed among patients who received one or two doses of IV iron. In contrast, no significant difference was found between patients who underwent bariatric surgery and those who did not (p = 0.212). Like bariatric surgery, no significant difference was found between the different age groups regarding the increase in ferritin levels (p = 0.929).
Discussion
In the current study, we aimed to investigate the efficacy and safety profiles of various doses of IV iron to identify the minimal optimal dose without the risk of hyperferritinemia in IDA patients, both post-bariatric and non-bariatric subgroups of patients suffering from related health conditions such as menorrhagia, ulcerative colitis, anticoagulation, thalassemia, or bariatric surgery.
FCM is a novel, next-generation complex for IV iron treatment with several advantages over previously used IV preparations including reduced administration time, optimal pH range and lack of reactivity with dextran antibodies.14 We have found that hemoglobin levels increased significantly in the study group. Compared to orally administered ferrous sulfate, FCM is better tolerated, prompts a more rapid hemoglobin response, especially at low or very low Hb levels, and is more reliable.15 The formulation releases a minimal amount of iron into the circulation taken up by macrophages in a controlled manner and delivered via physiological iron metabolism pathways to transferrin and ferritin.14 Other IV iron preparations are also marketed and prescribed in various cases, but they usually cause increased adverse events, including hypersensitivity reactions.16 IV iron sucrose, for instance, carries side effects affecting Hb level enhancement.17 Iron dextran, another IV iron preparation, carries the risk of anaphylactic reactions.18
Although oral iron supplementation is the first-line treatment for IDA, some patients cannot tolerate oral iron owing to gastrointestinal side effects. For some patients with IDA, the rate of chronic loss is greater than the replacement rate of oral iron supplementation.19 A recent observational study published by Das et al compared the safety and efficacy profiles of oral iron with those of IV iron. The increase in Hb and serum ferritin levels was higher for IV iron than for oral iron.20,21 FCM is typically recommended in cases in which the oral preparations are ineffective or cannot be used. FCM can be administered as a single dose providing up to 1000 mg of iron as a rapid infusion or in multiple doses (100–200 mg) without the need for a test dose.22 FCM is a suitable method of iron supplementation, especially in very low Hb levels or cases where multiple doses of IV iron are not convenient, or there is a patient compliance challenge.22,23
In addition to Hb levels, MCV evaluation is also recommended to assess the efficacy of iron supplementation by comparing pre- and post-treatment values.24 Reduced MCV is a marker of anemia. Similar to the increase in Hb levels, we found a significant increase in the levels of MCV in our study group. However, the increase in MCV levels was significantly higher for the individuals receiving three doses of FCM than those receiving a single dose. To our knowledge, this is a novel finding that has not been investigated to date, and the precise molecular mechanisms that lead to increased long-term efficacy of multiple FCM doses in terms of MCV require further investigation. Overall, these findings suggest that FCM can effectively treat iron deficiency in patients with IDA caused by various pathologies.
The risk of developing IDA is higher both pre- and post-operatively in individuals undergoing bariatric surgery due to increased consumption of high-calorie food with low iron content before the procedure,25 and reduced oral intake and decreased iron absorption due to the decline in gastric acid production and bypass of the proximal small intestine after the surgery.26,27 FCM is helpful in the treatment of persistent or relapsing IDA after Roux-en-Y gastric bypass.28 In a retrospective review of five Phase III studies, FCM effectively increased hemoglobin and ferritin levels. The observed adverse effects were similar to those observed for other IV iron products.29 Most studies published to date have evaluated the safety and efficacy profiles of iron supplementation in individuals who underwent bariatric surgery. We evaluated the efficacy of IV FCM administration in individuals undergoing bariatric surgery and found no statistically significant difference between the two groups; however, our results suggested periodic re-evaluation with a possible need for maintenance of IV iron, especially in this group of patients. The hemoglobin concentration and MCV did not differ significantly between the two study groups.
An increase in circulating platelets, referred to as thrombocytosis, may occur secondary to iron deficiency.30 Therefore, correction of IDA leads to a reduction in platelet count to the normal range. We observed a significant decrease in the median platelet count among study subjects. Similar to the Hb concentration and MCV, no significant difference was noted for individuals who underwent bariatric surgery. The decrease was higher for individuals receiving multiple doses of IV iron than for those receiving a single dose, which may indicate that even though one dose can achieve an adequate level of Hb and ferritin, it may not be sufficient to replenish the deficient stores. This finding is similar to that of MCV, indicating at long-term influence on iron homeostasis.
Hypophosphatemia has been reported as a side effect of FCM more often than of other iron formulations.31 FCM treatment leads to a transient increase in the plasma levels of phosphaturic hormone intact FGF23 (iFGF23) which stimulates renal phosphorus excretion.32 As mentioned in various case reports and cohort-based studies, extensive renal excretion of phosphorus leads to low serum phosphate levels.31,33 We also observed that some of our subjects had hypophosphatemia; however, there were fewer cases of hypophosphatemia in patients receiving increased doses. This can be attributed to the relatively small number of patients receiving increasing doses. The hypophosphatemia associated with FCM reportedly resolves spontaneously after 6–12 weeks.34
IV FCM has been reported to produce a rapid and pronounced initial increase in serum ferritin levels that decline over time but remain higher than baseline.35–38 Our study findings are in concordance with the reported data, whereby the ferritin levels remained significantly elevated during the first three months after treatment with FCM but then dropped gradually. In contrast, other forms of IV iron therapy are associated with only a slight increase in serum ferritin level.35,39 To our knowledge, the effects of single and multiple doses of FCM on hyperferritinemia have not been reported in the literature. We found that multiple doses carry an increased risk of transient hyperferritinemia compared with a single dose of IV FCM. Thus, the optimal response is inversely related to the number of doses administered. Interestingly, a population of IDA patients requires periodic review for reinfusion of iron to sustain the level above the required level of >30 ng/mL. Further subgroup studies are needed to determine the optimal dose and the relationship between the number of doses and increase in ferritin levels and the various modifiers of this relationship. This study is limited by its retrospective design and smaller sample size.
Conclusion and Future Prospects
FCM is a robust and reliable option for the IDA treatment. Therapy with IV FCM helps achieve quick significant improvements in Hb concentration, MCV, and reactive thrombocytosis. The risk of transient hyperferritinemia associated with IV FCM administration was tolerable and reversable Furthermore, hypophosphatemia has been reported in some cases following FCM treatment. We observed that the full two or three doses of IV iron resulted in decrease in platelet count although not statistically significant. We recommend conducting a prospective large-scale study to confirm our findings. An interesting finding of this study is the discovery of a population of IDA patients requiring periodic assessment for iron reinfusion to sustain normal levels, mostly post-bariatric surgery.
Data Sharing Statement
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
This study was performed in line with the principles of the Declaration of Helsinki. Approval was granted by the Ethics Committee of Dr. Sulaiman Al Habib Medical Group.
Consent to Participate
Informed consent was obtained from all individual participants included in the study.
Consent to Publish
All authors consent for publication. The authors also affirm that human research participants provided informed consent for publication related to their data.
Acknowledgments
Authors would like to acknowledge Dr. Nazia Sadaf for her freelance medical editing services.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work. All authors read and approved the final manuscript.
Funding
The authors declare that no funds, grants, or other support were received during the preparation of this manuscript.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Vos T, Allen C, Arora M., et al. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1545–1602.
2. Organization UNWH. Iron Deficiency Anaemia: Assessment, Prevention and Control: A Guide for Programme Managers. World Health Organization; 2001.
3. Wish JB. Assessing iron status: beyond serum ferritin and transferrin saturation. Clin J Am Soc Nephrol. 2006;1(Supplement 1):S4–S8. doi:10.2215/CJN.01490506
4. De Benoist B, Cogswell M, Egli I, et al. Worldwide prevalence of anaemia 1993-2005. WHO Global Database of anaemia; 2008.
5. Das SN, Devi A, Mohanta BB, et al. Oral versus intravenous iron therapy in iron deficiency anemia: an observational study. J Family Med Primary Care. 2020;9(7):3619. doi:10.4103/jfmpc.jfmpc_559_20
6. Giordano G, Napolitano M, Di Battista V, et al. Oral high-dose sucrosomial iron vs intravenous iron in sideropenic anemia patients intolerant/refractory to iron sulfate: a multicentric randomized study. Ann Hematol. 2020;1;1–7.
7. Alquaiz A-JM, Khoja TA, Alsharif A, et al. Prevalence and correlates of anaemia in adolescents in Riyadh city, Kingdom of Saudi Arabia. Public Health Nutr. 2015;18(17):3192–3200. doi:10.1017/S1368980015001214
8. Abalkhail B, Shawky S. Prevalence of daily breakfast intake, iron deficiency anaemia and awareness of being anaemic among Saudi school students. Int J Food Sci Nutr. 2002;53(6):519–528. doi:10.1080/09637480220164370
9. Gari MA. Prevalence of iron deficiency anemia among female elementary school children in Northern Jeddah, Saudi Arabia. J King Abdulaziz Univ Med Sci. 2008;15(1):63–75. doi:10.4197/Med.15-1.6
10. Al Hifzi I, Pejaver RK, Qureshi I. Screening for iron deficiency anemia in a well baby clinic. Ann Saudi Med. 1996;16(6):622–624. doi:10.5144/0256-4947.1996.622
11. AlSheikh MH. Prevalence and risk factors of iron-deficiency anemia in Saudi female medical students. Prevalence. 2018;7(3):148–152.
12. Al Hawsawi ZM, Al-Rehali SA, Mahros AM, et al. High prevalence of iron deficiency anemia in infants attending a well-baby clinic in northwestern Saudi Arabia. Saudi Med J. 2015;36(9):1067. doi:10.15537/smj.2015.9.11844
13. Owaidah T, Al-Numair N, Al-Suliman A, et al. Iron deficiency and iron deficiency anemia are common epidemiological conditions in Saudi Arabia: report of the National Epidemiological Survey. Anemia. 2020;2020:6642568. doi:10.1155/2020/6642568
14. Crichton RR, Danielson BG, Geisser P. Iron therapy with special emphasis on intravenous administration. UNI-MED-Verl; 2008.
15. Van Wyck DB, Martens MG, Seid MH, et al. Intravenous ferric carboxymaltose compared with oral iron in the treatment of postpartum anemia: a randomized controlled trial. Obstet Gynecol. 2007;110(2 Pt 1):267–278. doi:10.1097/01.AOG.0000275286.03283.18
16. Mulder MB, van den Hoek HL, Birnie E, et al. Comparison of hypersensitivity reactions of intravenous iron: iron isomaltoside-1000 (Monofer(®)) versus ferric carboxy-maltose (Ferinject(®)). Br J Clin Pharmacol. 2019;85(2):385–392.
17. Christoph P, Schuller C, Studer H, et al. Intravenous iron treatment in pregnancy: comparison of high-dose ferric carboxymaltose vs. J Perinat Med. 2012;40(5):469–474.
18. Fletes R, Lazarus JM, Gage J, et al. Suspected iron dextran-related adverse drug events in hemodialysis patients. Am J Kidney Dis. 2001;37(4):743–749. doi:10.1016/S0272-6386(01)80123-2
19. Bregman DB, Morris D, Koch TA, et al. Hepcidin levels predict nonresponsiveness to oral iron therapy in patients with iron deficiency anemia. Am J Hematol. 2013;88(2):97–101. doi:10.1002/ajh.23354
20. Das SN, Devi A, Mohanta BB, et al. Oral versus intravenous iron therapy in iron deficiency anemia: an observational study. J Family Med Prim Care. 2020;9(7):3619–3622.
21. Litton E, Xiao J, Ho KM. Safety and efficacy of intravenous iron therapy in reducing requirement for allogeneic blood transfusion: systematic review and meta-analysis of randomised clinical trials. BMJ. 2013;1;347.
22. Tagboto S, Cropper L, Turner J, et al. The efficacy of a single dose of intravenous ferric carboxymaltose (Ferinject®) on anaemia in a pre‐dialysis population of chronic. Kidney Dis Patients J Renal Care. 2009;35(1):18–23.
23. Laso-Morales MJ, Vives R, Vallejo-Tarrat A, et al. Single dose of intravenous ferric carboxymaltose infusion versus multiple fractionated doses of intravenous iron sucrose in the treatment of postoperative anaemia in colorectal cancer patients: study protocol for a randomised controlled trial. Trials. 2019;20(1):23. doi:10.1186/s13063-018-3125-2
24. Abdelazim IA, Nusair B, Svetlana S, et al. Treatment of iron deficiency and iron deficiency anemia with intravenous ferric carboxymaltose in pregnancy. Arch Gynecol Obstet. 2018;298(6):1231–1232. doi:10.1007/s00404-018-4943-x
25. Aarts E, Van Wageningen B, Janssen I, et al. Prevalence of anemia and related deficiencies in the first year following laparoscopic gastric bypass for morbid obesity. J Obes. 2012;2012:85.
26. Smith CD, Herkes SB, Behrns KE, et al. Gastric acid secretion and vitamin B12 absorption after vertical Roux-en-Y gastric bypass for morbid obesity. Ann Surg. 1993;218(1):91–96. doi:10.1097/00000658-199307000-00014
27. Salgado W, Modotti C, Nonino CB, et al. Anemia and iron deficiency before and after bariatric surgery. Surg Obes Relat Dis. 2014;10(1):49–54. doi:10.1016/j.soard.2013.06.012
28. Schijns W, Boerboom A, de Bruyn Kops M, et al. A randomized controlled trial comparing oral and intravenous iron supplementation after Roux-en-Y gastric bypass surgery. Clinical Nutrition. 2020;39(12):3779–3785. doi:10.1016/j.clnu.2020.04.010
29. Malone M, Barish C, He A, et al. Comparative review of the safety and efficacy of ferric carboxymaltose versus standard medical care for the treatment of iron deficiency anemia in bariatric and gastric surgery patients. Obes Surg. 2013;23(9):1413–1420. doi:10.1007/s11695-013-0939-6
30. Schafer AI. Thrombocytosis and thrombocythemia. Blood Rev. 2001;15(4):159–166. doi:10.1054/blre.2001.0162
31. Emrich IE, Lizzi F, Siegel JD, et al. Hypophosphatemia after high-dose iron repletion with ferric carboxymaltose and ferric derisomaltose—the randomized controlled HOMe aFers study. BMC Med. 2020;18(1):178. doi:10.1186/s12916-020-01643-5
32. Zoller H, Schaefer B, Glodny B. Iron-induced hypophosphatemia: an emerging complication. Curr Opin Nephrol Hypertens. 2017;26(4):266–275. doi:10.1097/MNH.0000000000000329
33. Fang W, McMahon LP, Bloom S, et al. Symptomatic severe hypophosphatemia after intravenous ferric carboxymaltose. JGH Open. 2019;3(5):438–440. doi:10.1002/jgh3.12150
34. Wolf M, Chertow GM, Macdougall IC, et al. Randomized trial of intravenous iron-induced hypophosphatemia. JCI Insight. 2018;3(23):23. doi:10.1172/jci.insight.124486
35. Seid MH, Derman RJ, Baker JB, et al. Ferric carboxymaltose injection in the treatment of postpartum iron deficiency anemia: a randomized controlled clinical trial. Am J Obstet Gynecol. 2008;199(4):435.e1–e7. doi:10.1016/j.ajog.2008.07.046
36. Breymann C, Gliga F, Bejenariu C, et al. Comparative efficacy and safety of intravenous ferric carboxymaltose in the treatment of postpartum iron deficiency anemia. Int J Gynecol Obstetrics. 2008;101(1):67–73. doi:10.1016/j.ijgo.2007.10.009
37. Van Wyck DB, Martens MG, Seid MH, et al. Intravenous ferric carboxymaltose compared with oral iron in the treatment of postpartum anemia: a randomized controlled trial. Obstet Gynecol. 2007;110(2Part 1):267–278.
38. Qunibi WY, Martinez C, Smith M, et al. A randomized controlled trial comparing intravenous ferric carboxymaltose with oral iron for treatment of iron deficiency anaemia of non-dialysis-dependent chronic kidney disease patients. Nephrology Dialysis Transplantation. 2011;26(5):1599–1607. doi:10.1093/ndt/gfq613
39. Kulnigg S, Stoinov S, Simanenkov V, et al. A novel intravenous iron formulation for treatment of anemia in inflammatory bowel disease: the ferric carboxymaltose (FERINJECT®) randomized controlled trial. Official j Am College Gastroenterol. 2008;103(5):1182–1192. doi:10.1111/j.1572-0241.2007.01744.x
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
