Back to Journals » Journal of Multidisciplinary Healthcare » Volume 15
Risk Factors of Microvascular Complications Among Type 2 Diabetic Patients Using Cox Proportional Hazards Models: A Cohort Study in Tabuk Saudi Arabia
Authors Saiyed NS , Yagoub U, Al Qahtani B, Al Zahrani AM, Al Hariri I, Syed MJ, Elmardi ME, Tufail MA, Manajreh M
Received 24 March 2022
Accepted for publication 30 June 2022
Published 27 July 2022 Volume 2022:15 Pages 1619—1632
DOI https://doi.org/10.2147/JMDH.S367241
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Nasrin S Saiyed,1 Umar Yagoub,1 Bandar Al Qahtani,2 Attiya Mohammed Al Zahrani,3 Ibrahim Al Hariri,4 Meerab Javed Syed,5 Mohammed Elmujtaba Elmardi,6 Muhammad Abdullah Tufail,7 Marwan Manajreh1
1Research Department, King Salman Armed Forces Hospital, Tabuk, Saudi Arabia; 2Academic Affairs Department, King Salman Armed Forces Hospital, Tabuk, Saudi Arabia; 3Surgery Department, King Salman Armed Forces Hospital, Tabuk, Saudi Arabia; 4Family Medicine Department, King Salman Armed Forces Hospital, Tabuk, Saudi Arabia; 5Internal Medicine Department, King Salman Armed Forces Hospital, Tabuk, Saudi Arabia; 6Cardiology Department, King Salman Armed Forces Hospital, Tabuk, Saudi Arabia; 7Ophthalmology Department, King Salman Armed Forces Hospital, Tabuk, Saudi Arabia
Correspondence: Umar Yagoub, Director of Research Department, Research Department, King Salman Armed Forces Hospital, Tabuk, Saudi Arabia, Email [email protected]
Purpose: The burden of type 2 diabetes (T2D) is high in Saudi Arabia, but data related to its complications are limited. This study aimed to determine the incidence of microvascular complications caused by T2D and evaluate the impact of the associated risk factors.
Patients and Methods: This retrospective cohort study was conducted at two military hospitals in Tabuk, Saudi Arabia. Data on the socio-demographics, glycaemic profile, blood lipid indices, duration of T2D, and associated microvascular complications were collected from electronic health records and medical files. Descriptive statistics and Cox proportional hazards models were used for data analysis.
Results: This study included 1563 T2D patients. The incidence of microvascular complications was 34.3% (95% confidence interval [CI], 32.0– 36.6). Retinopathy was the most common complication (incidence=20.0%; 95% CI, 18.0– 22.0%), while nephropathy was the least common complication (incidence=12.2%; 95% CI, 10.6– 13.8%). Advanced age (≥ 65 years) showed the highest risk of retinopathy (Hazard ratios [HR], 2.86; 95% CI, 2.56– 3.21), neuropathy (HR, 2.70; 95% CI, 2.40– 3.05), and nephropathy (HR, 2.37; 95% CI, 2.12– 2.64) compared with their counterparts. After adjusting for potential confounders, the study found that the significant risk factors for microvascular complications were longer duration (≥ 10 years) of T2D (HR, 5.3; 95% CI, 5.1– 5.6), uncontrolled hypertension (HR, 3.9; 95% CI, 3.3– 4.2), poor glycaemic control (HR, 4.6; 95% CI, 4.3– 5.1), obesity (HR, 2.3; 95% CI, 2.2– 2.6), and dyslipidaemia (HR, 1.6; 95% CI, 1.2– 2.0).
Conclusion: Given the high burden of microvascular complications in military healthcare facilities in Tabuk, Saudi Arabia, a context-specific accessible public health program focusing on the promotion of a healthy lifestyle, physical activity, and consumption of a healthy diet, as well as the early diagnosis and management of diabetes, needs to be developed and implemented.
Keywords: diabetes, microvascular complications, retinopathy, peripheral neuropathy, nephropathy, Saudi Arabia
Introduction
Diabetes is a serious endocrine disease caused by elevated blood glucose levels. Its prevalence and incidence are increasing at an alarming rate worldwide. Recent studies indicated that approximately 422,000,000 people have diabetes, and approximately 1,600,000 deaths are directly attributed to diabetes every year. About 90–95% of all patients with diabetes are diagnosed with type 2 diabetes (T2D).1–3 Due to the rapid economic growth, urban development, and lifestyle changes in the Middle East and North Africa region over the past two decades, the total number of diabetes cases has also increased. Saudi Arabia is not exempted from this worldwide epidemic; diabetes is acknowledged as the country’s most serious health problem.4,5
Novel discoveries in basic diagnostics and affordable insulin have increased the overall mean years lived with diabetes, which could ultimately lead to more diverse diabetes-related morbidities. Chronic hyperglycaemia plays a major role in the development of diabetic complications through a variety of metabolic and structural abnormalities.6,7 T2D causes various complications, among which microvascular complications are the most devastating. It adversely affects the small blood vessels in the eye, kidney, and peripheral nervous system and contributes significantly to the morbidity and mortality in T2D patients. Retinopathy, peripheral neuropathy, and nephropathy are the three classical microvascular complications of T2D.8,9
Patients with a longer T2D duration are at higher risk of developing microvascular complications, which can lead to the reduction in the quality of life, disability, or death. Diabetic retinopathy is the most common microvascular complication of T2D, which leads to visual impairment and blindness. _ENREF_10 Diabetic peripheral neuropathy leads to substantial morbidity, including pain, foot ulcers, and lower limb amputation. Diabetic kidney disease is highly prevalent among T2D patients and is the primary cause of end-stage renal disease.11 Older age, obesity, lack of physical exercise, unhealthy food intake, smoking, hypertension, and a family history of diabetes are the major risk factors for T2D microvascular complications.12,13
The incidence of microvascular complications caused by T2D is increasing, primarily in low- and middle-income countries.14 In Saudi Arabia, the incidence of T2D microvascular complications among people aged 18 years and older is approximately 10%–40%, which increases over time. An increase in the incidence of T2D microvascular complications in Saudi Arabia could be attributed largely to the modifiable behavioural risk factors, such as sedentary lifestyle, excess weight, unhealthy diet, and smoking tobacco products.15,16 As the risk factors contributing to the development of T2D microvascular complications are multifactorial and traditional, it is extremely essential to evaluate their combined effects on the development of microvascular complications.
Saudi Arabia reported the second highest diabetes rate in the Middle East and ranked seventh worldwide.4 Despite the high incidence of T2D in Saudi Arabia, only a few cross-sectional studies have investigated its complications.13,17,18 In the cross-sectional study the outcome and the exposure are examined at the same time which will not provide the temporal link between them. To address this important gap, an up-to-date three years cohort study on the epidemiology of T2D microvascular complications considered, which is essential to establish preventive strategies and plan treatment guidelines to minimise the impact of these complications. Therefore, this study aimed to determine the incidence of T2D microvascular complications and to examine its association with the risk factors among Saudi Arabian residents.
Materials and Methods
Study Design and Data Source
This multicentre, 3-year retrospective cohort study was conducted in King Salman Armed Forces Hospital (KSAFH) and King Khalid Military (KKMH) Hospital in Tabuk, Saudi Arabia, between 1 January 2019 and 31 December 2021. Only one common hospital information system automates the clinical and electronic health records and the administrative and inventory functions of both hospitals. The electronic health records included personal information, health-related behaviours, laboratory test results, diagnoses, prescriptions, admission, and discharge dates. These comprehensive longitudinal health records have been extensively validated by the medical records department. Only doctors, nurses, and other authorised staff members have access to this system. In this database system, diagnoses are coded by attending doctors according to the International Classification of Disease, version 10 (ICD-10).
Study Population
This hospital-based study was conducted in Tabuk, Saudi Arabia. Tabuk is located in the north-western part of the Arabian Peninsula, bordering Jordan, and has a population of more than half a million. It houses the largest air force base in Saudi Arabia. The KSAFH and KKMH hospitals are managed by the Saudi Armed Forces Medical Services Department. These hospitals provide preventive services and medical care to armed force members and their families. Both hospitals were fully equipped and operated according to the international hospital standards. KSAFH is a joint commission internationally credited hospital that provides all major and advanced interventional and non-interventional services. There was one common administration in both hospitals.
Inclusion-Exclusion Criteria
The majority of diabetes patients at KSAFH and KKMH admitted in the internal medicine, family medicine, neurology, renal, diabetes clinic, and medical/surgical wards were followed up. All adult T2D patients who had one or more admissions to any of these hospitals or had two or more hospital visits within 1 year (during the study period) were included in the study. In contrast, (1) T2D patients who had experienced any microvascular disease prior to their T2D diagnosis; (2) patients who were newly diagnosed with T2D and were on T2D treatment for less than 3 months; (3) patients with any gastrointestinal, infectious, or hepatic disease (severe, acute, or chronic); (4) pregnant women or breastfeeding mothers; (5) patients with any major psychiatric disorder having psychotic symptoms; and (6) T2D patients with incomplete and inactive records (no visits in one year or more) in the electronic health records were excluded.16–18
Sample Size
The sample size was calculated using the incidence of the least common microvascular complication of diabetic peripheral neuropathy (19%) in Saudi Arabia.15 A single proportion sample size calculation formula was used, which was based on the function of expected incidence and precision for a certain degree of confidence expressed by the z-statistic. The following formula was used:
The minimum sample size was 1479, considering an acceptable margin of error Δ=2%, a level of significance of α=5%, and an estimated incidence  of 0.19. The final sample size was 1627, taking into account 10% of the patients with incomplete records.
of 0.19. The final sample size was 1627, taking into account 10% of the patients with incomplete records.
Sampling Procedure
A two-stage stratified cluster sampling procedure with a primary sampling unit as clinics/wards (clusters) selected from the two hospitals was used. Considering the initial 2-month data collected from the hospital information system, the sample size was allocated proportionally using the proportionate to population size. The estimated sample size for this study (n) was divided by the total number of patients (N) registered in a randomly selected clinic within the last 2 months, which yielded proportionate (P) value. Then, by multiplying the proportionate value with the 2-month sample, a proportional sample was allocated to each selected clinic/ward. A list of patients diagnosed with T2D was prepared. Finally, systematic random sampling was used to take every 5th T2D patient from this list. If a patient was eligible for the study, information was collected from the patient. If not, the record was ignored and the next 5th record was obtained.
Definitions of Terms
- The microvascular complications of diabetes are caused by chronic hyperglycaemia. When T2D is not well controlled, increased level of circulating blood sugar sticks to the small blood vessels and makes it difficult for the blood to flow, which damages multiple organs, such as the eyes, feet, and kidneys. The different microvascular complications are follows:
- Diabetic retinopathy (DR) is an eye disease caused by diabetes mellitus. This complication can occur when there is damage to the blood vessels in the light-sensitive tissue of the retina. Chronic hyperglycemia causes endothelial damage.11
- Diabetic nephropathy (DN) refers to a condition where damage to the kidney occurs due to diabetes. When diabetes is not properly controlled, it can cause damage to the blood vessel clusters in the kidneys, which filter waste from the blood.11
- Neuropathy is a heterogeneous condition associated with the blood vessels and is caused by damage or dysfunction of one or more nerves in the body that results in numbness, tingling, muscle weakness, and pain in the affected area.11
- Educated: The patient who can read and write Arabic was considered as “educated”.
- Smoking habit: Smoking habit was recorded as “no” if the patients did not smoke tobacco and “yes” if the patients had tobacco smoking.
- Uncontrolled hypertension was defined as an average systolic blood pressure ≥140 mmHg or an average diastolic blood pressure ≥90 mmHg.
- Poor glycaemic control: The glycaemic control was defined as “poor” if the haemoglobin A1c (HbA1c) level was greater than or equal 6.5%.
- Body mass index (BMI) was calculated as weight in kilograms divided by height in meters squared and classified as follows: (1) underweight: < 18.5 kg/m2, (2) normal: 18.5–24.99 kg/m2, (3) overweight: 25.0–29.9 kg/m2, and (4) obese≥ 30.0 kg/m2.
- Dyslipidaemia was defined as a total cholesterol (TC) level >5.2 mmol/L, low-density lipoprotein cholesterol (LDL-c) level >3.4 mmol/L, high-density lipoprotein cholesterol (HDL-c) level <0.9 mmol/L, or triglyceride (TG) level >1.7 mmol/L, or a combination thereof.19
Data Collection Tool
A structured data collection form was prepared to retrieve information from the electronic health records and medical files. It comprised three different sections: (1) general characteristics and anthropometric measurements, (2) blood pressure measurements and laboratory test results, and (3) macro- and/or microvascular complications caused by T2D. The patients’ general characteristics included age, sex, nationality, education, smoking habits, family history of diabetes, duration of T2D, and BMI. Data on the following laboratory test results were obtained: glycaemic profile [haemoglobin A1c (HbA1c), random blood glucose (RBS), fasting blood glucose (FBS]), lipid profile [TG, TC, LDL-c, HDL-c], urine albumin-to-creatinine ratio, and estimated glomerular filtration rate.
Case Identification
The data used in the current study were obtained from the electronic health records, and some information was extracted from the medical files (hard copies). The biomarkers used in routine clinical practice for the diagnosis, screening, monitoring, and prognosis of patients are available in electronic health records. Established coding algorithms were used to identify potential T2D cases from the records. Patients with a T2D ICD-10 code E11, an HbA1c level ≥6.5%, an RBS ≥11.1 mmol/L, and an FBS ≥7.0 mmol/L, and with a prescription for or who used antidiabetic medications were considered eligible for the study.
Data Extraction
Data on T2D complications were obtained from the electronic health records and medical files. All non-fatal complications during the study period were evaluated. The duration of T2D from the point of diagnosis until 31 December 2021 was also extracted and calculated using the earliest fulfilment of any of the stated criteria in this order: (1) earliest HbA1c level ≥6.5% and (2) earliest FBS level >7.0 mmol/L. The chronic microvascular complications included retinopathy, peripheral neuropathy, and nephropathy.
Primary Outcome and Assessment of Covariates
The primary study endpoint was microvascular complication(s) caused by T2D. The most recent HbA1C level within 1 year before 31 December 2021 was also recorded. The covariates evaluated in this analysis were demographics (age, sex, nationality, and education level); smoking habit; family history of diabetes; duration of T2D; blood pressure measurements; laboratory findings within 6 months after the study start date, including the estimated glomerular filtration rate (eGFR) and urinary albumin excretion (microalbuminuria or proteinuria); and BMI. The incidence of T2D microvascular complications was recorded as “no” if the patients with diabetes had neither acute nor chronic complications and “yes” if the patients had a chronic microvascular complication. The associated medical conditions, including hypertension and dyslipidaemia, were also reported.
Data Management
Cohort data were extracted from the electronic health records and medical files. A trained research assistant filled out the data collection forms. Each data form was assigned with a unique study number (beginning with DM0001). The data were entered and stored on a computer, and the information was password protected. Double data entry validation was performed to ensure data quality. Furthermore, 10% of the entered data was rechecked for accuracy. Only the principal investigator and co-investigators had access to the data for analysis. Participants were identified by their unique study numbers, and only the principal investigator had access to the identifiers that linked the data to the individual participant. De-identified data were collected and analysed.
Statistical Analysis
The baseline characteristics of patients were reported as frequencies and percentages. The normally distributed continuous data were expressed as mean and standard deviation (SD). The non-normally distributed data were presented as median and interquartile ranges. The recorded T2D microvascular complications were defined as the prevalent cases. Cox regression models were used to examine the putative risk factors for each prevalent T2D microvascular complication by calculating the hazard ratios (HR) and their 95% confidence intervals (CI). Crude models were considered for the following three types of microvascular complications: diabetic retinopathy, diabetic peripheral neuropathy, and diabetic nephropathy. The assumptions of the Cox regression model were validated using Schoenfeld residual plots. The incidence of microvascular complications was considered as an “event”, while the absence of microvascular complications was marked as “censored” in the analyses. One combined outcome was referred to as “any complications” and was defined as the presence of any or multiple microvascular complications. An adjusted model for any complications was developed, which was adjusted for age, sex, nationality, education, smoking habits, and family history of T2D. All statistical analyses were performed using IBM Statistical Package for the Social Sciences statistics version 25. The significance level was set at p < 0.05. All p values were two tailed.
Results
Flowchart
Of the 1630 T2D patients, 67 were excluded at the time of enrolment for one or more of the following reasons: incomplete records (n=22), inactive cases (n=9), and patients with other comorbidities (n=36). The final sample consisted of 1563 patients. Patients with complete records were included in the final analysis. The flow chart below shows the selection of patients in the cohort (Figure 1).
 |
Figure 1 Flowchart showing selection of patients in the study cohort. |
Baseline Characteristics of Patients with Type 2 Diabetes in the Cohort
The baseline characteristics of the patients with T2D in the cohort are shown in Table 1. The earliest observation, which was close to the start date of the study, was considered. A total of 1563 patients were included in the final analysis [992 men, 571 women; mean age: 51.3 years (SD: 12.8 years)]. Six out of ten patients had a positive family history of diabetes (59.8%). The majority of patients had T2D for more than 5 years (89.1%). In addition, 24.6% of the patients had hypertension. (Table 1)
 |
Table 1 Baseline Characteristics of Patients with Type 2 Diabetes (Total =1563) |
Anthropometric Measurements and Laboratory results
The median and interquartile ranges of the baseline anthropometric measurements and laboratory results are presented in Table 2. The median HbA1c level was 8.5% (6.8–9.7%). Most patients were obese with a median BMI of 30.3 kg/m2 (27.0–36.0 kg/m2). The T2D patients showed high eGFR [median eGFR: 82.3 mL/min/1.73 m2 (70.3–95.7 mL/min/1.73 m2)] (Table 2).
 |
Table 2 Anthropometric Measurements and Laboratory Results |
Incidence of Microvascular Complications Among Type 2 Diabetes Patients
During the study, 536 (34.3%) patients had microvascular complications (95% CI, 32.0–36.6), of whom 312 (20.0%) had diabetic retinopathy (95% CI, 18.0–22.0), 219 (14.0%) had peripheral neuropathy (95% CI, 12.3–15.7), and 191 (12.2%) had diabetic nephropathy (95% CI, 10.6–13.8). Among the total patients, 361 (23.1%) had one microvascular complication (95% CI, 21.0–25.3), 164 (10.5%) had two microvascular complications (95% CI, 9.0–12.1), and 11 (0.7%) had all three microvascular complications (95% CI, 0.3–1.3) (Figure 2).
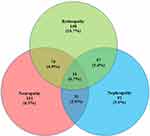 |
Figure 2 Microvascular complications among type 2 diabetes patients. |
Cox Regression Analysis of the Microvascular Complications Among Type 2 Diabetes Patients
To identify the putative risk factors for developing microvascular complications, a multivariate Cox regression analysis was performed in all enrolled patients. The results are presented in Table 3. Based on the crude analysis, a significantly increased risk of developing diabetic retinopathy was associated with poor glycaemic control (HR, 6.37; 95% CI, 6.21–6.54) and a T2D duration of more than 10 years (HR, 5.24; 95% CI, 4.51–6.53). The risk of developing peripheral neuropathy was higher in patients with a baseline age of ≥65 years (HR, 2.70; 95% CI, 2.40–3.05) and in male patients (HR, 2.67; 95% CI, 2.52–2.98). The risk of diabetic nephropathy was higher among smokers (HR, 1.53, 95% CI, 1.06–1.76) and patients with dyslipidaemia (HR, 1.46; 95% CI, 1.22–1.75) (Table 3).
 |
Table 3 Results of the Cox Regression Analysis of Prevalent Microvascular Complications Among Type 2 Diabetes Patients |
After controlling the effect of potential confounders in the multivariate Cox analysis, the hazard of developing microvascular complications was five times higher in patients with a disease duration of ≥10 years than in their counterparts (adjusted HR [AHR], 5.31; 95% CI, 5.12–5.67). Furthermore, the risk of developing microvascular complications was increased by more than fourfold in patients who had poor glycaemic control than in those who had good glycaemic control (AHR, 4.65, 95% CI, 4.37–5.19) (Figure 3).
T2D patients with uncontrolled hypertension had a threefold increased risk of developing microvascular complications than their counterparts (AHR, 3.93; 95% CI, 3.36–4.25). Similarly, patients with obesity were two times more likely to develop microvascular complications than those with normal body weight (AHR, 2.37; 95% CI, 2.21–2.69). Likewise, patients with dyslipidaemia were 1.7 times more likely to develop hypertension than their counterparts (AHR, 1.69; 95% CI, 1.22–2.03) (Figure 3).
Discussion
In this hospital-based, multicentre, retrospective cohort study conducted in the northwest region of Saudi Arabia, the overall incidence of microvascular complications was 34.3% in T2D patients. The incidence rates of retinopathy, peripheral neuropathy, and nephropathy were 20.0%, 14.0%, and 12.2%, respectively. Among patients who developed microvascular complications, approximately one-third had two or more complications. The highest increases in microvascular complications were observed among men, older adults, and smokers. Some proven and hypothesised risk factors associated with T2D microvascular complications were described in this study. Longer duration of T2D, poor glycaemic control, obesity, family history of diabetes, and comorbid uncontrolled hypertension were strongly associated with the development of microvascular complications.
A high incidence of microvascular complications was observed among T2D patients, which might be due to the accessibility and advancement of healthcare institutions, which helps ascertain more patients with microvascular complications. This proportion is in line with that of previous studies on lower- and middle-income countries.20,21 However, the yields in this investigation were lower compared with those in other studies.2,10,22 The present study concludes that diabetic retinopathy is the most common microvascular complication observed among the studied population, which closely matches with the global incidence estimates and lower than the numbers reported in the United States, Australia, Europe, and Asia.23,24 On the contrary, diabetic nephropathy is the least common microvascular complication. The observed results confirm the previous findings from a recent regional review and the international literature.25,26
Of greater relevance to epidemiological research, it is important to examine the role of the risk factors for progressive long-term chronic diseases. The risk factors related to T2D complications are multifactorial and traditional.12,27 The present study found a positive association between microvascular complications and some aforementioned prognostic factors, which is consistent with the findings of several previous studies.16,28 The present study demonstrates that poor glycaemic control and a longer duration of T2D were the strongest predictors of microvascular complications. Overall, the dose-response association was observed between the risk of microvascular complications and age; the risk increased with age, and the highest risk was observed in the oldest age groups among male patients. This finding is in accordance with the results of previous studies conducted in Asian and Western countries.29–32 In this study, nationality and educational status did not cause a significant increase in the risk of developing microvascular complications. This finding is consistent with the results of previous studies. Additionally, the increased risk of developing microvascular complications persisted even after controlling for variations in baseline characteristics. Hence, these results should be confirmed by reviewing a considerable body of literature.33–35
Age is an important predictor of vascular damage in patients with diabetes. These data suggest that the risk of developing diabetic retinopathy in the middle and older age groups (aged ≥45 years) of T2D patients was more than two times higher than that in younger patients (aged 18–44 years). Similar results were obtained in a recent review from the United States and in a prospective observational study from South Asia.36,37 This is most likely due to the cumulative effect of insulin resistance and beta-cell loss with increasing age, which results in hyperglycaemia, thus causing microvascular damage.38 Furthermore, sex plays a major role in the incidence and natural course of many diseases. Sex differences in the diagnosis and management of vascular illnesses have been discussed previously. The incidence of diabetic retinopathy was consistently higher in men than in women. Likewise, a large-scale, multicentre, retrospective cross-sectional study found that male sex per se might be a risk factor for diabetic retinopathy development.39 On the contrary, a nationwide study of diabetic retinopathy conducted in Poland claimed that women are more prone to developing diabetic retinopathy.40 Moreover, smoking is one of the biggest causes of death and illness, and the findings of the current study indicate a higher risk of retinopathy among smokers. Most previous studies investigating the association between smoking and microvascular complications demonstrated that smoking tobacco significantly increased the risk of developing retinopathy,41,42 although several other studies showed significantly decreased or no association.43,44
A family history of diabetes is another well-investigated predictor of T2D microvascular complications. In addition to genetic risk factors, numerous studies have supported the role of genetic determinants in the susceptibility to diabetes-related complications. The results of this study showed that a family history of diabetes was a significant risk factor for diabetic peripheral neuropathy and was reviewed for patients in Saudi Arabia.17 The patients who had T2D for more than or equal to 10 years were more likely to develop chronic diabetes complications compared with their counterparts. There are several possible explanations for this finding. Long-standing hyperglycaemia affects the blood vessels. Furthermore, these injuries can cause problems to the kidneys, eyes, feet, and nerves. This study revealed that the patients had a longer duration of diabetes. This finding supports the results of a recent meta-analysis that included 171 studies on T2D patients from different cities in China from 2014 to 2019.45,46 Additionally, previous studies from various settings had documented that around 25–50% of T2D patients have coexisting hypertension, and that T2D doubles the risk of peripheral neuropathy development. Previous epidemiological studies have shown a possible association between uncontrolled hypertension and adverse outcomes. This may be because uncontrolled hypertension accelerates the progression and development of microvascular complications.47 In this study, the results of the Cox regression analysis showed that uncontrolled hypertension is a risk factor for peripheral neuropathy, with a HR of uncontrolled hypertension of 1.52. Based on the present findings, a review conducted in the United Kingdom concluded that there is a significant association between diabetic peripheral neuropathy and hypertension.48
As evidenced by the data presented in the current study, poor glycaemic control is another major contributing factor. Several studies have unequivocally demonstrated the negative impact of poor glycaemic control on the patient outcomes. In a single-centre study, glycated haemoglobin variability was independently associated with the development of nephropathy.14,49 The results of this single-centre study lend further support to this finding reported in Saudi Arabian residents. In addition, high BMI was significantly associated with diabetic nephropathy. Although a variety of factors can affect the development of microvascular complications in the T2D population, lifestyle habits typically associated with suburbanisation are likely the most significant factors. This finding is in accordance with the results of a previous study conducted in Canada.50 Moreover, evidence from the present study suggests that participants with dyslipidaemia have a higher likelihood of developing diabetic nephropathy. Previous studies evaluating the association between nephropathy and blood lipid profiles reported controversial results. Some studies51 reported a positive association between blood lipid parameters and nephropathy, while others52 showed negative associations. The findings of the present study were concordant with the results of previous studies.
Strengths and Limitations of the Study
This study has several strengths, including a large patient population that reflects the communities examined. This study was carried out using electronic health records, and the benefit of using the electronic system decreased the risk of potential confounding factors. Furthermore, excluding patients with a T2D diagnosis of <6 months allows the selection of a cohort that is consistently followed up in the system. This study provides insights that are relevant to regional and international audiences. Meanwhile, this study has some limitations. It does not provide estimates of the number of patients in the database who sought care outside of these two hospitals, which could lead to either underestimation or overestimation of the incidence of microvascular complications. Second, at the time of analysis, HbA1c levels were only available at baseline, and the impact of the changes in glycaemic control level with time should be the focus of future studies. Third, due to the limited resources, not all risk factors related to microvascular complications were included in this study. Forth, these two hospitals provide preventive services and medical care to armed force members and their families. This study findings could have limited generalizability to the overall Saudi population.
Conclusions
In conclusion, the present study attempted to depict the current incidence of diabetes-related microvascular complications in Tabuk, Saudi Arabia. Glycaemic, traditional, and non-traditional risk factors contribute to the occurrence of these complications. Thus, additional multi-dimensional and multi-sectoral studies are highly recommended to strengthen the evidence and consolidate more facts as a framework for establishing policies and programs to prevent diabetes and its complications. There is also an urgent need to develop strategies and programs to prevent and control high blood sugar levels and promote healthy lifestyle behaviours in the Saudi Arabian population.
Abbreviations
T2D, type 2 diabetes; KSAFH, King Salman Armed Forces Hospital; KKMH, King Khalid Military Hospital; ICD, International Classification of Disease; HbA1c, haemoglobin A1c; BMI, body mass index; RBS, random blood glucose; FBS, fasting blood glucose; TG, triglycerides; TC, total cholesterol; LDL-c, low-density lipoprotein cholesterol; HDL-c, high-density lipoprotein cholesterol; eGFR, estimated glomerular filtration rate; SD, standard deviation; HR, hazard ratio; CI, confidence interval; SPSS, Statistical Package for the Social Sciences; CHR, crude hazard ratio; AHR, adjusted hazard ratio.
Data Sharing Statement
The supporting data used in this study are available from King Salman Armed Forces Hospital and King Khalid Military Hospital, with some restrictions on their application due to the availability of these data. These data were used under license for the present study; hence, they are not publicly available. The data are however available from the research and ethics committee at King Salman Armed Forces Hospital (contact via email: [email protected] and telephone number: +966144411088extensions:84571) for investigators who meet the criteria for the right to use confidential information.
Ethics Approval and Informed Consent
All ethical issues in King Salman Armed Forces Hospital and King Khalid Military Hospital were handled by a single research ethics committee. This study was reviewed and approved by the Research & Ethics Committee at King Salman Armed Forces Hospital, Tabuk, Saudi Arabia (project no. KSAFH-REC-2022-436). The ethical committee waived the need for obtaining a written informed consent due to the retrospective nature of the study, which involved anonymised patient data. Patients’ identities were kept confidential. The research was carried out in accordance with the 1964 Declaration of Helsinki. All procedures were performed according to the ethical standards.
Acknowledgments
The authors would like to thank King Salman Armed Forces Hospital and King Khalid Military Hospital for their support. We would also like to acknowledge all the registry staff for their efforts in data management.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The study was fully funded by Research Department, King Salman Armed Forces Hospital Tabuk, Kingdom of Saudi Arabia.
Disclosure
The authors declare that they have no potential conflicts of interest concerning the research, authorship, and/or publication of this article.
References
1. Forouhi NG, Wareham NJ. Epidemiology of diabetes. Medicine. 2019;47(1):22–27. doi:10.1016/j.mpmed.2018.10.004
2. Harding JL, Pavkov ME, Magliano DJ, Shaw JE, Gregg EW. Global trends in diabetes complications: a review of current evidence. Diabetologia. 2019;62(1):3–16. doi:10.1007/s00125-018-4711-2
3. Misra A, Gopalan H, Jayawardena R, et al. Diabetes in developing countries. J Diabetes. 2019;11(7):522–539. doi:10.1111/1753-0407.12913
4. Robert AA, Al Dawish MA. The worrying trend of diabetes mellitus in Saudi Arabia: an urgent call to action. Curr Diabetes Rev. 2020;16(3):204–210. doi:10.2174/1573399815666190531093735
5. Abuyassin B, Laher I. Diabetes epidemic sweeping the Arab world. World J Diabetes. 2016;7(8):165. doi:10.4239/wjd.v7.i8.165
6. Buse JB, Davies MJ, Frier BM, Philis-Tsimikas A. 100 years on: the impact of the discovery of insulin on clinical outcomes. BMJ Open Diabetes Res Care. 2021;9(1):e002373. doi:10.1136/bmjdrc-2021-002373
7. Gregg EW, Sattar N, Ali MK. The changing face of diabetes complications. Lancet Diabetes Endocrinol. 2016;4(6):537–547. doi:10.1016/S2213-8587(16)30010-9
8. Liu J, Liu Z. Muscle insulin resistance and the inflamed microvasculature: fire from within. Int J Mol Sci. 2019;20(3):562. doi:10.3390/ijms20030562
9. Mauricio D, Alonso N, Gratacòs M. Chronic diabetes complications: the need to move beyond classical concepts. Trends Endocrinol Metab. 2020;31(4):287–295. doi:10.1016/j.tem.2020.01.007
10. Hussein M, Menasri S. Prevalence of microvascular complications in type 2 diabetics attending a primary healthcare centre in Sudan. Dubai Diabetes Endocrinol J. 2019;25(3–4):127–133. doi:10.1159/000500914
11. Faselis C, Katsimardou A, Imprialos K, Deligkaris P, Kallistratos M, Dimitriadis K. Microvascular complications of type 2 diabetes mellitus. Curr Vasc Pharmacol. 2020;18(2):117–124. doi:10.2174/1570161117666190502103733
12. Zheng Y, Ley SH, Hu FB. Global aetiology and epidemiology of type 2 diabetes mellitus and its complications. Nat Rev Endocrinol. 2018;14(2):88–98. doi:10.1038/nrendo.2017.151
13. Alramadan MJ, Magliano DJ, Alhamrani HA, et al. Lifestyle factors and macro-and micro-vascular complications among people with type 2 diabetes in Saudi Arabia. Diabetes Metab Syndrome Clin Res Rev. 2019;13(1):484–491. doi:10.1016/j.dsx.2018.11.007
14. Aschner P, Galstyan G, Yavuz DG, et al. Glycemic control and prevention of diabetic complications in low-and middle-income countries: an expert opinion. Diabetes Ther. 2021;12(5):1491–1501. doi:10.1007/s13300-021-00997-0
15. Alwin Robert A, Al Dawish MA. Microvascular complications among patients with diabetes: an emerging health problem in Saudi Arabia. Diabetes Vasc Dis Res. 2019;16(3):227–235. doi:10.1177/1479164118820714
16. Cheema S, Maisonneuve P, Zirie M, et al. Risk factors for microvascular complications of diabetes in a high-risk Middle East population. J Diabetes Res. 2018;2018. doi:10.1155/2018/8964027
17. Sendi RA, Mahrus AM, Saeed RM, Mohammed MA, Al-Dubai SAR. Diabetic peripheral neuropathy among Saudi diabetic patients: a multicenter cross-sectional study at primary health care setting. J Family Med Primary Care. 2020;9(1):197. doi:10.4103/jfmpc.jfmpc_927_19
18. Al-Ayed MY, Ababneh M, Robert AA, Salman A, Al Saeed A, Al Dawish MA. Evaluation of risk factors associated with diabetic foot ulcers in Saudi Arabia. Curr Diabetes Rev. 2019;15(3):224–232. doi:10.2174/1573399814666180816165848
19. Eng E, Quaggin S. Putting it all together: practical approach to the patient with diabetic kidney disease. In: Diabetes and Kidney Disease. Springer; 2022:637–659.
20. Bui HDT, Jing X, Lu R, et al. Prevalence of and factors related to microvascular complications in patients with type 2 diabetes mellitus in Tianjin, China: a cross-sectional study. Ann Transl Med. 2019;7:14. doi:10.21037/atm.2019.06.08
21. Seid MA, Akalu Y, Gela YY, et al. Microvascular complications and its predictors among type 2 diabetes mellitus patients at Dessie town hospitals, Ethiopia. Diabetol Metab Syndr. 2021;13(1):1–8.
22. Khalil SA, Megallaa MH, Rohoma KH, et al. Prevalence of chronic diabetic complications in newly diagnosed versus known type 2 diabetic subjects in a sample of Alexandria population, Egypt. Curr Diabetes Rev. 2019;15(1):74–83. doi:10.2174/1573399814666180125100917
23. Teo ZL, Tham Y-C, Yu M, et al. Global prevalence of diabetic retinopathy and projection of burden through 2045: systematic review and meta-analysis. Ophthalmology. 2021;128(11):1580–1591. doi:10.1016/j.ophtha.2021.04.027
24. Ting DSW, Cheung GCM, Wong TY. Diabetic retinopathy: global prevalence, major risk factors, screening practices and public health challenges: a review. Clin Experiment Ophthalmol. 2016;44(4):260–277. doi:10.1111/ceo.12696
25. Lin YK, Gao B, Liu L, et al. The prevalence of diabetic microvascular complications in China and the USA. Curr Diab Rep. 2021;21(6):1–11. doi:10.1007/s11892-021-01387-3
26. Afroz A, Zhang W, Loh AJW, Lee DXJ, Billah B. Macro-and micro-vascular complications and their determinants among people with type 2 diabetes in Bangladesh. Diabetes Metab Syndrome Clin Res Rev. 2019;13(5):2939–2946. doi:10.1016/j.dsx.2019.07.046
27. Nørgaard CH, Mosslemi M, Lee CJ-Y, Torp-Pedersen C, Wong ND. The importance and role of multiple risk factor control in type 2 diabetes. Curr Cardiol Rep. 2019;21(5):1–10. doi:10.1007/s11886-019-1123-y
28. Nanayakkara N, Ranasinha S, Gadowski A, et al. Age, age at diagnosis and diabetes duration are all associated with vascular complications in type 2 diabetes. J Diabetes Complications. 2018;32(3):279–290. doi:10.1016/j.jdiacomp.2017.11.009
29. Khanam PA, Hoque S, Begum T, Habib SH, Latif ZA. Microvascular complications and their associated risk factors in type 2 diabetes mellitus. Diabetes Metab Syndrome Clin Res Rev. 2017;11:S577–S81. doi:10.1016/j.dsx.2017.04.007
30. Szwarcbard N, Villani M, Earnest A, et al. The association of smoking status with glycemic control, metabolic profile and diabetic complications–results of the Australian National diabetes audit (ANDA). J Diabetes Complications. 2020;34(9):107626. doi:10.1016/j.jdiacomp.2020.107626
31. Gedebjerg A, Almdal TP, Berencsi K, et al. Prevalence of micro-and macrovascular diabetes complications at time of type 2 diabetes diagnosis and associated clinical characteristics: a cross-sectional baseline study of 6958 patients in the Danish DD2 cohort. J Diabetes Complications. 2018;32(1):34–40. doi:10.1016/j.jdiacomp.2017.09.010
32. Kosiborod M, Gomes MB, Nicolucci A, et al. Vascular complications in patients with type 2 diabetes: prevalence and associated factors in 38 countries (the DISCOVER study program). Cardiovasc Diabetol. 2018;17(1):1–13. doi:10.1186/s12933-018-0787-8
33. Zhao H, Shu L, Huang W, Wang W, Song G. Difference analysis of related factors in macrovascular and microvascular complications in Chinese patients with Type 2 diabetes mellitus: a case-control study protocol. Diabetes, Metab Syndrome Obesity Targets Ther. 2019;12:2193. doi:10.2147/DMSO.S213848
34. Narindrarangkura P, Bosl W, Rangsin R, Hatthachote P. Prevalence of dyslipidemia associated with complications in diabetic patients: a nationwide study in Thailand. Lipids Health Dis. 2019;18(1):1–8. doi:10.1186/s12944-019-1034-3
35. Tilahun M, Gobena T, Dereje D, Welde M, Yideg G. Prevalence of diabetic retinopathy and its associated factors among diabetic patients at Debre Markos referral hospital, Northwest Ethiopia, 2019: hospital-Based Cross-Sectional Study. Diabetes, Metab Syndrome Obesity Targets Ther. 2020;13:2179. doi:10.2147/DMSO.S260694
36. Leley SP, Ciulla TA, Bhatwadekar AD. Diabetic retinopathy in the aging population: a perspective of pathogenesis and treatment. Clin Interv Aging. 2021;16:1367. doi:10.2147/CIA.S297494
37. Sultan S, Fawwad A, Siyal NA, Butt A, Khokar AR, Basit A. Frequency and risk factors of diabetic retinopathy in patients with type 2 diabetes presenting at a tertiary care hospital. Int J Diabetes Dev Ctries. 2020;40(1):87–92. doi:10.1007/s13410-019-00756-9
38. Giri B, Dey S, Das T, Sarkar M, Banerjee J, Dash SK. Chronic hyperglycemia mediated physiological alteration and metabolic distortion leads to organ dysfunction, infection, cancer progression and other pathophysiological consequences: an update on glucose toxicity. Biomed Pharmacother. 2018;107:306–328.
39. Cherchi S, Gigante A, Spanu MA, et al. Sex-gender differences in diabetic retinopathy. Diabetology. 2020;1(1):1–10. doi:10.3390/diabetology1010001
40. Kozioł M, Nowak MS, Udziela M, Piątkiewicz P, Grabska-Liberek I, Szaflik JP. First nation-wide study of diabetic retinopathy in Poland in the years 2013–2017. Acta Diabetol. 2020;57(10):1255–1264. doi:10.1007/s00592-020-01540-6
41. Wu Y-B, Wang C-G, Xu L-X, Chen C, Zhou X-B, Su G-F. Analysis of risk factors for progressive fibrovascular proliferation in proliferative diabetic retinopathy. Int Ophthalmol. 2020;40(10):2495–2502. doi:10.1007/s10792-020-01428-y
42. West SK. Smoking and the risk of eye diseases. In: Nutritional and Environmental Influences on the Eye. CRC Press; 2021:151–164.
43. Cai X, Chen Y, Yang W, Gao X, Han X, Ji L. The association of smoking and risk of diabetic retinopathy in patients with type 1 and type 2 diabetes: a meta-analysis. Endocrine. 2018;62(2):299–306. doi:10.1007/s12020-018-1697-y
44. Chan JCY, Chee ML, Tan NYQ, Cheng C-Y, Wong TY, Sabanayagam C. Differential effect of body mass index on the incidence of diabetes and diabetic retinopathy in two Asian populations. Nutr Diabetes. 2018;8(1):1–11. doi:10.1016/j.cegh.2019.08.019
45. Yuanyuan C, Shuli Q, Yanjun L, Yuqi Z, Wenjie X, Li C. Meta-analysis of the epidemiology of microvascular complications in people with Type 2 diabetes in mainland China. Global J Obesity, Diabetes Metab Syndrome. 2020;7(2):018–23. doi:10.17352/2455-8583.000042
46. Fawwad A, Mustafa N, Zafar AB, Khalid M. Incidence of microvascular complications of type 2 diabetes: a 12 year longitudinal study from Karachi-Pakistan. Pak J Med Sci. 2018;34(5):1058. doi:10.12669/pjms.345.15224
47. Yildiz M, Esenboga K, Oktay AA. Hypertension and diabetes mellitus: highlights of a complex relationship. Curr Opin Cardiol. 2020;35(4):397–404. doi:10.1097/HCO.0000000000000748
48. Yamazaki D, Hitomi H, Nishiyama A. Hypertension with diabetes mellitus complications. Hypertens Res. 2018;41(3):147–156. doi:10.1038/s41440-017-0008-y
49. Alramadan MJ, Magliano DJ, Almigbal TH, et al. Glycaemic control for people with type 2 diabetes in Saudi Arabia–an urgent need for a review of management plan. BMC Endocr Disord. 2018;18(1):1–12. doi:10.1186/s12902-018-0292-9
50. D’Souza MS, Labrague LJ, Karkada SN, Kamble P. Relationship between socio-demographic, clinical factors, and quality of life in adults living with diabetic nephropathy. Clin Epidemiol Global Health. 2020;8(2):343–349.
51. Savelieff MG, Callaghan BC, Feldman EL. The emerging role of dyslipidemia in diabetic microvascular complications. Curr Opin Endocrinol Diabetes Obes. 2020;27(2):115–123. doi:10.1097/MED.0000000000000533
52. Singh SS, Rashid M, Lieverse AG, et al. Lipoprotein (a) plasma levels are not associated with incident microvascular complications in type 2 diabetes mellitus. Diabetologia. 2020;63(6):1248–1257. doi:10.1007/s00125-020-05120-9
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.