Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 17
Patients with Chronic Obstructive Pulmonary Disease and Evidence of Eosinophilic Inflammation Experience Exacerbations Despite Receiving Maximal Inhaled Maintenance Therapy
Authors Chen S , Miravitlles M , Rhee CK , Pavord ID , Jones R, Carter V, Emmanuel B , Alacqua M, Price DB
Received 28 June 2022
Accepted for publication 22 August 2022
Published 9 September 2022 Volume 2022:17 Pages 2187—2200
DOI https://doi.org/10.2147/COPD.S378649
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Stephanie Chen,1 Marc Miravitlles,2 Chin Kook Rhee,3 Ian D Pavord,4 Rupert Jones,5 Victoria Carter,6 Benjamin Emmanuel,1 Marianna Alacqua,7 David B Price6,8
1BioPharmaceuticals Medical, Respiratory & Immunology, AstraZeneca, Gaithersburg, MD, USA; 2Pneumology Department, Hospital Universitari Vall d’Hebron, Vall d’Hebron Institut de Recerca (VHIR), Vall d’Hebron Barcelona Hospital Campus, CIBER de Enfermedades Respiratorias (CIBERES), Barcelona, Spain; 3College of Medicine, Seoul St Mary’s Hospital, the Catholic University of Korea, Seoul, South Korea; 4Oxford Respiratory NIHR BRC, Nuffield Department of Medicine, University of Oxford, Oxford, UK; 5Faculty of Health, University of Plymouth, Plymouth, UK; 6Observational and Pragmatic Research Institute, Singapore, Singapore; 7BioPharmaceuticals Medical, Respiratory & Immunology, AstraZeneca, Cambridge, UK; 8Centre of Academic Primary Care, Division of Applied Health Sciences, University of Aberdeen, Aberdeen, UK
Correspondence: David B Price, Observational and Pragmatic Research Institute, 22 Sin Ming Lane, #06-76, Midview City, Singapore, 573969, Singapore, Tel +65 3105 1489, Email [email protected]
Background: Some patients with chronic obstructive pulmonary disease (COPD) experience frequent exacerbations despite maximal inhaled therapy (“triple therapy”), possibly leading to high health care resource utilization (HCRU).
Aim: Describe characteristics, future HCRU, and mortality of patients with COPD who experience frequent exacerbations despite triple therapy; characterize individuals who may be candidates for biologic therapies.
Methods: This descriptive observational study used primary care data of patients aged ≥ 40 years in the United Kingdom receiving maintenance therapy for COPD who had ≥ 1 year of data prior to index date and ≥ 1 year of follow-up data. We described these patients’ clinical and demographic characteristics, including blood eosinophil counts (BEC), pattern of exacerbations, hospitalizations, and corticosteroid exposure, as well as future exacerbations, hospitalizations, and death.
Results: Of 43,753 patients with maintenance-treated COPD, 6480 experienced exacerbations despite ≥ 3 months of triple therapy. Of these, 5669 had available BEC: 1287 (22.7%) had BEC ≥ 250 cells/μL and ≥ 3 exacerbations in the year prior to the index date; 471 (36.6%) received ≥ 4 acute courses of oral corticosteroids. Patients with a pattern of high disease burden continued to have high disease burden: 51.1% experienced ≥ 3 exacerbations and 2.6% experienced ≥ 3 hospitalizations. Patients who experienced exacerbations despite triple therapy had a significantly higher risk of COPD-related death than other maintenance-treated patients (5.8% vs 2.1%).
Conclusion: Nearly one-quarter of patients receiving triple therapy for COPD who experienced frequent exacerbations had elevated BEC and ≥ 3 exacerbations, suggesting a potential mechanism of persistent eosinophilic inflammation that could be a target for eosinophil-depleting biologic therapy.
Keywords: chronic obstructive pulmonary disease, disease burden, eosinophils, exacerbations, health care resource utilization
Plain Language Summary: BLANCA2
Patients with Chronic Obstructive Pulmonary Disease May Experience Flare-ups Despite High Levels of Therapy
Patients with chronic obstructive pulmonary disease (COPD) may use up to 3 types of inhaled medicines at once, called “triple therapy.” Triple therapy is the highest level of treatment that patients can take. It helps improve COPD symptoms by decreasing inflammation and relaxing muscles in the lungs and opening the airways.
A COPD exacerbation, or flare-up, is a short-term worsening of symptoms. Flare-ups may include difficulty breathing and feeling tired. Some patients taking triple therapy still have frequent flare-ups. Flare-ups can lead to higher costs, additional medicines, or time in hospital. We aimed to describe patients who experience flare-ups in order to guide treatment decisions.
We used a medical record database to describe adults with COPD in the United Kingdom. Of 43,000 patients with COPD, nearly 6500 taking triple therapy had frequent flare-ups. These patients were almost 3 times as likely to die of COPD as other patients with COPD. Nearly one-quarter had increased levels of a white blood cell that is a marker of inflammation and experienced 3 or more flare-ups in the year before the study started. Of these, more than half had 3 or more flare-ups and nearly 3% were admitted to hospital in the year after the study started.
Overall, patients with frequent flare-ups in the past were likely to have frequent flare-ups in the future. Many of these patients have evidence of inflammation. Biologic medicines that decrease white blood cells related to inflammation may be considered as treatment options for COPD in the future.
Introduction
Chronic obstructive pulmonary disease (COPD) is a heterogeneous condition that leads to substantial morbidity and mortality.1–3 The Global Initiative for Chronic Obstructive Lung Disease (GOLD) strategy describes COPD as a group of preventable, treatable lung conditions that are characterized by persistent respiratory symptoms and airflow limitation due to airway and/or alveolar abnormalities usually caused by significant exposure to noxious particles or gases.2 GOLD offers evidence-based reference tools for the implementation of effective management plans for COPD and represents the current best practices for the care of patients with COPD.3,4 Despite guideline-based management, COPD is often complicated by comorbidities and exacerbations,5 which negatively affect patients’ health status and prognosis and have high societal and economic costs.1,3,6–8 Therefore, minimization and/or management of comorbidities and prevention of exacerbations are major therapeutic goals for patients with COPD.6,8
Maximal inhaled therapy (also called “triple therapy”), which comprises an inhaled corticosteroid (ICS), a long-acting muscarinic antagonist (LAMA), and a long-acting β2 agonist (LABA), has resulted in decreased moderate or severe COPD exacerbations and a lower rate of COPD-related hospitalizations.9–11 Still, some patients receiving triple therapy may continue to experience frequent exacerbations,12 some of which have been associated with eosinophilic inflammation with high blood eosinophil counts (BEC).4,13,14 These patients represent a relevant unmet need that accounts for high health care resource utilization (HCRU).15
A new paradigm in COPD management—the concept of “treatable traits”—uses a personalized approach to treatment to improve outcomes through individualized and multifaceted assessments of factors that may lead to decreased lung function and quality of life. Treatable traits may be pulmonary, extrapulmonary, or behavioral in nature,5,16,17 but they must be clinically relevant, identifiable and measurable, and treatable.5,16,18 One such trait may be an elevated BEC, which is recommended by GOLD as a valid identifying marker of 3 important factors: the presence of eosinophilic airway inflammation, a higher exacerbation risk, and better treatment response to ICS.16,19–23 This suggests a COPD sub-phenotype with an eosinophilic type of airway inflammation similar to that observed in some patients with asthma,24 and, as such, could be treated like eosinophilic asthma with eosinophil-depleting biologic therapy.
To enhance understanding of patients with COPD who remain at risk for frequent exacerbations and to work toward identifying potential treatment targets, we conducted a historical cohort study. The goals were to describe characteristics of patients with COPD who experienced a high exacerbation burden despite maximal maintenance treatment in the year prior to the index date and to assess HCRU, as well as all-cause and COPD-related mortality, in this patient group during 1 year of follow-up. We also characterized individuals with COPD who continued to experience exacerbations despite maintenance therapy and had an eosinophilic phenotype as demonstrated by an elevated BEC, as these patients may be potential candidates for biologic therapy.
Patients and Methods
Study Design and Patient Population
This was a descriptive historical cohort study using primary care data from the Clinical Practice Research Datalink (CPRD) with linkage to Hospital Episode Statistics (HES), including data for hospital admissions, specialist outpatient visits, emergency room visits, and the Office of National Statistics (ONS) mortality data in the United Kingdom. Patient data were extracted from the CPRD during March 2019.
The entire study population included patients with COPD who were 40 years of age or older at their most recent COPD diagnosis or review and who received ≥1 prescription for maintenance therapy. This was defined as at least 1 prescription for a LABA, a LAMA, and/or an ICS as monotherapy or in free-dose or fixed-dose combination as dual or triple therapy. Individuals with a diagnosis of chronic lower respiratory conditions other than COPD or asthma (eg, lung cancer, tuberculosis, cystic fibrosis, or asbestosis) were excluded (Supplementary Figure 1).
Two cohorts of patients were defined (Figure 1). The “maintenance-treated cohort” encompassed the entire population of patients with maintenance-treated COPD. The “frequently exacerbating cohort” included patients who experienced at least 1 severe or at least 2 moderate exacerbations despite at least 3 months of continuous treatment with triple therapy in the year prior to the index date. Subgroups of patients in the frequently exacerbating cohort with elevated BEC (≥250 and ≥350 cells/µL) and the highest frequency of exacerbations (≥3 in the year prior to the index date) were also identified.
 |
Figure 1 Study design. Abbreviations: COPD, chronic obstructive pulmonary disease; HCRU, health care resource utilization. |
For both cohorts, the index date was defined as a randomly selected date of a prescription for maintenance therapy for COPD within a time window of 12 to 24 months before the most recent date when data were extracted from the general practice (to select all patients with maintenance-treated COPD with ≥1 year of follow-up after the index date). Patients in both cohorts had to be registered with a primary care physician for at least 1 year prior to and after the index date.
Definitions
A COPD exacerbation was defined as an occurrence of COPD-related hospital admission (recorded in HES-Admitted Patient Care with International Classification of Diseases-10 code J40-J44.9 in the first position in any finished consultant episode) and/or emergency room visit and/or prescription in primary care for an acute oral corticosteroids (OCS) course or antibiotics course with evidence of a lower respiratory consultation. Events occurring within 2 weeks of each other were considered the result of the same exacerbation as used in prior publications by this group.25
Main Outcome Measures
Clinical and demographic characteristics of patients in both cohorts were evaluated, including the rate of COPD exacerbations, COPD-related hospitalizations, and corticosteroid exposure in the year prior to the index date; BEC within 2 years prior to the index date; and the number of years with ≥1 and ≥2 exacerbations in 10 years prior to the index date. The numbers of HCRU events, including exacerbations and hospitalizations, and the risk of COPD-related death were evaluated in the year after the index date. The predictive values of clinical characteristics of patients in the frequently exacerbating cohort were also identified.
Statistical Analysis
The study was descriptive in nature. Categorical variables are described as means with standard deviations and/or medians with interquartile ranges and numbers with percentages. Mortality was described using Kaplan-Meier curves and the number and percentage of patients who died. P-values for the Kruskal–Wallis equality-of-populations rank test or the Pearson’s chi-square test of independent categories were calculated to compare the frequency of HCRU events among patient cohorts.
Analyses were completed with STATA version 15 software.
Results
A total of 43,753 patients with maintenance-treated COPD were identified (maintenance-treated cohort). Of these patients, 43% received at least 1 prescription for triple therapy and 36% received triple therapy for ≥3 months during the year prior to the index date. In all, 14.8% (N=6480) experienced ≥1 severe or ≥2 moderate exacerbations in the year prior to the index date despite triple therapy (frequently exacerbating cohort).
Patient Demographics and Clinical Characteristics
Patient characteristics during the year prior to the index date are presented in Table 1. Roughly one-half of patients in the maintenance-treated cohort were male. Their average age was approximately 70 years.
 |
Table 1 Characteristics of Patient Cohorts and Subgroups in the Year Prior to the Index Date |
Slightly less than half of the patients reported respiratory and cardiovascular comorbidities. Patients in the frequently exacerbating cohort were less frequently male than those in the maintenance-treated cohort (46.8% vs 50.8%) and were more likely to have received a previous diagnosis of asthma (45.5% vs 40.1%). Approximately one-fifth (20.8% [n=1350]) of patients in the frequently exacerbating cohort experienced a COPD-related hospitalization and more than one-half (59.6% [n=3864]) experienced ≥3 exacerbations during the year prior to the index date (Table 1). Roughly the same percentages of patients in the maintenance-treated cohort and the frequently exacerbating cohort reported ever having a diagnosis of hypertension (45.3% [n=19,801] vs 44.5% [n=2881]), ischemic heart disease (19.7% [n=8634] vs 20.9% [n=1353]), and heart failure (5.5% [n=2412] vs 6.5% [n=424]).
Of those in the frequently exacerbating cohort, 5669 (87.5%) had available BEC: 2111 (37.2%) had BEC ≥250 cells/µL, and 1149 (20.3%) had BEC ≥350 cells/µL. The distribution of BEC was similar between the maintenance-treated cohort and the frequently exacerbating cohort. In both the maintenance-treated cohort and the frequently exacerbating cohort, those with elevated BEC were more likely to have asthma and nasal polyps than patients with BEC <250 cells/µL. No meaningful differences in COPD burden were noted in terms of exacerbations or ICS or OCS use according to BEC.
Overall, the OCS burden of maintenance-treated patients with COPD was high, with individuals in the frequently exacerbating cohort using more OCS than the general COPD population. Nearly 90% of patients in the frequently exacerbating cohort received acute courses of OCS, with approximately one-fifth (n=1389 [21.4%]) receiving ≥4 courses during the year prior to the index date. Of patients with BEC ≥250 cells/µL and ≥3 exacerbations in the year prior to the index date, 471 (36.6%) patients received ≥4 courses. Only 2259 (5.2%) of patients in the entire maintenance-treated cohort met this criterion.
High doses of daily ICS were also prevalent among the frequently exacerbating cohort: 44.8% of the cohort (n=2902) and of the subgroup with BEC ≥250 cells/µL and ≥3 exacerbations (n=576) had an average daily exposure of ≥800 mcg fluticasone equivalent in the year prior to the index date. Only 21.5% (n=9405) in the overall maintenance-treated cohort had the same.
HCRU in the Outcome Year
Patients in the frequently exacerbating cohort continued to experience a high disease burden, including exacerbations, emergency room visits, outpatient visits, and hospitalizations related to COPD, in the outcome year. In the entire maintenance-treated COPD cohort, patients had roughly the same risk of experiencing ≥1 exacerbation in the year prior to the index date as in the outcome year (52.8% and 52.4%, respectively). More than 60% of patients in the frequently exacerbating cohort experienced at least 2 moderate/severe exacerbations in the outcome year (Table 2).
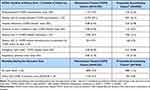 |
Table 2 HCRU Events and Mortality During the Outcome Year |
Mortality
During the outcome year, 7.9% of patients in the maintenance-treated COPD cohort and 11.6% in the frequently exacerbating cohort died. Patients in this cohort had a significantly (p<0.0001) higher risk of COPD-related death than other patients (5.8% vs 2.1%) in the outcome year (Table 2).
Characteristics in the Year Prior to the Index Date as Predictors of Future HCRU
In both the maintenance-treated and frequently exacerbating cohorts, a higher number of exacerbations, more years with a high occurrence of exacerbations, and a higher number of hospitalizations in the year prior to the index date predicted a higher disease burden in the outcome year. Neither OCS use nor BEC during the year prior to the index date predicted exacerbations in either cohort (Supplementary Table 1).
Exacerbation Burden
Most patients (n=34,312) in the maintenance-treated COPD cohort had ≥10 years of continuous data available. Of those with available data, 37.3% (n=12,801) experienced ≥1 exacerbation per year for at least 5 years; 12.9% (n=4411) had ≥2 exacerbations per year for at least 5 years. In the frequently exacerbating cohort, 74.4% (n=3772) and 40.2% (n=2039) met these criteria, respectively. For both cohorts, the rate of exacerbations in the outcome year increased with the exacerbation burden over the past 10 years (Figure 2).
Almost one-half (47.6%) of individuals with ≥3 exacerbations in the year prior to the index date experienced ≥3 exacerbations in the outcome year (Figure 3A). In the frequently exacerbating cohort, 82.5% of patients had ≥1 exacerbation in the outcome year. More than one-half of patients (51.1%) in this cohort with ≥3 exacerbations in the year prior to the index date experienced ≥3 exacerbations in the outcome year (Figure 3B).
Hospitalizations
Most patients were not hospitalized for COPD in the outcome year (Table 2). In both cohorts, patients who had a higher number of exacerbations and those who had a higher number of hospitalizations in the year prior to the index date experienced more hospitalizations in the outcome year (Figure 3). Among patients in the frequently exacerbating cohort with ≥3 hospitalizations in the year prior to the index date, 66.7% had ≥1 hospitalization in the outcome year.
In the frequently exacerbating cohort, similar rates of exacerbation and hospitalization were observed in the outcome year in patients with and without hospitalization in the year prior to the index date. Individuals in the frequently exacerbating cohort experienced a slightly elevated exacerbation rate in the outcome year compared with the year prior to the index date when hospital admission was needed for ≥1 exacerbation (Supplementary Table 2).
Consistent with the findings of the larger cohort, among patients in the frequently exacerbating cohort with BEC ≥250 cells/µL and BEC ≥350 cells/µL, a higher number of exacerbations, regardless of the need for hospital admission, during the year prior to the index date predicted more exacerbations and hospitalizations in the outcome year (Supplementary Table 2).
Discussion
We identified more than 43,000 patients with maintenance-treated COPD. A substantial portion of these patients (nearly 6500) received the highest level of maintenance therapy (triple therapy) but continued to experience a relatively high burden of disease, including high rates of OCS use in the year prior to the index date and frequent moderate to severe exacerbations in both the year before and the year after the index date. These patients also demonstrated substantially higher numbers of HCRU events than were observed for the total population of patients with maintenance-treated COPD. Notably, in all subgroups evaluated, a higher burden of exacerbations and HCRU predicted higher future disease burden and increased mortality. Our findings support those of another observational study that demonstrated substantial HCRU, costs, and exacerbation rates among patients with COPD who were receiving triple therapy but continued to experience exacerbations.26
Of patients who experienced exacerbations despite receiving triple therapy, nearly one-quarter (n=1287/5669; 22.7%) had BEC ≥250 cells/µL and experienced ≥3 exacerbations in the year prior to the index date. This represents approximately 3.0% (n=1287/43,753) of the entire maintenance-treated cohort, which is a slightly higher proportion than the proportion of patients with asthma who have severe, uncontrolled eosinophilic disease despite therapy (<1%), according to a large analysis of patients with asthma who were receiving systemic corticosteroids.26 Despite the small size of the group, patients with severe, uncontrolled eosinophilic asthma experience a nearly four-fold increase in HCRU events and a four-fold increase in costs (£861.0 vs £222.0 per year) compared with all patients with asthma.27 This is similar to the findings in our cohort, which revealed that individuals with severe COPD and frequent exacerbations experience a significantly higher number of HCRU events than the general COPD population, even though they are receiving maximal, guideline-directed therapy.
ICS inhaler therapy has been recommended for COPD treatment for more than 25 years; more recently, ICS therapy was added to the GOLD recommendations for COPD due to its effectiveness for patients with BEC ≥300 cells/µL and a history of exacerbations.2 However, in our study, a substantial portion of patients with elevated BEC continued to experience exacerbations despite ICS treatment. This suggests that such patients have persistent eosinophilic inflammation underlying the exacerbations, which could potentially be a treatable trait targeted with biologic therapy.
The fact that a group of patients continues to experience a high exacerbation burden despite maximal therapy begets the question: Are patients receiving triple therapy, namely ICS, still experiencing exacerbations because they are not adherent to therapy or because the therapy is not targeting the right mechanism of inflammation? Earlier work conducted at the Observational Pragmatic Research Institute (OPRI) confirmed the increased risk of exacerbations with high BEC (≥450 cells/µL) in a real-world study of non-smoking patients with COPD in the United Kingdom.28 Significant associations were consistently found across all therapy categories, with high adherence to ICS noted among patients with more frequent exacerbations, which suggests that current treatments are insufficient in preventing an excess risk of exacerbations for patients with COPD who have high BEC.19
OPRI also completed a study to assess the impact of exacerbations on lung function decline.29 Among patients who were not treated with ICS-containing therapy, those with an elevated BEC (≥350 cells/µL; 17%) had significantly more accelerated lung function declines with increasing exacerbation rates than those with normal BEC (50–340 cells/µL).29 Additionally, Hancox et al completed a longitudinal study that analyzed BEC and changes in lung function in patients from age 21 to 38 years: high BECs were associated with increased airflow obstruction and decreased lung function, even in patients without symptoms.30 Together, these findings support the need for adequate treatment of underlying eosinophilic inflammation for patients with COPD as well as for those who are not adequately responding to the highest concentrations of inhaler therapy.29 The role of eosinophilia in COPD remains unclear, and no reliable threshold of blood eosinophilia has been identified to discriminate a higher risk of exacerbations,18,26,31 but BEC is showing promise as a marker of COPD outcomes.
One particular strength of this study was its inclusion of a large, broad population of patients with COPD who were representative of maintenance-treated persons with COPD in the UK’s general population. This vast dataset allowed for accurate descriptions of characteristics in addition to subpopulations that showed relatively low frequencies. Also, the completeness of the data, which were prospectively collected and, thus, not subject to recall bias, strengthen the findings. The data source used is well-regarded and often employed for pharmacoepidemiologic studies.32–35
Given the findings here and the overall strength of this dataset, future areas of research should encompass further analysis of patient populations by exacerbation type; the impact of corticosteroids, given their high use in this dataset; and types of morbidity and mortality in COPD populations beyond all-cause, including cardiac, respiratory, lung cancer, and related deaths.
Limitations
This study is limited by the fact that the data were collected for routine clinical use, not for research. Despite extensive quality control and validation, the completeness of individual data cannot be confirmed. Though full blood count measurements are a routine part of primary care for patients with COPD, individuals with an indication for BEC measurements may differ from those without an indication and may not be representative of the total COPD population. Finally, prescriptions are used to estimate drug exposure, but this does not guarantee the correct use of all doses.
Conclusions
Patients with COPD who experience frequent moderate to severe exacerbations despite maximal inhaler therapy represent a considerable unmet medical need and may benefit from future therapy with eosinophil-depleting biologics. Nearly one-quarter of these patients experience ≥3 exacerbations per year with elevated BEC.
Data Sharing Statement
Data underlying the findings described in this manuscript may be requested in accordance with AstraZeneca’s data-sharing policy described at https://astrazenecagroup-dt.pharmacm.com/DT/Home.
Ethics Approval
The study was approved by the Independent Scientific Advisory Committee (ISAC) and registered with the European Network of Centres for Pharmacoepidemiology and Pharmacovigilance (ENCEPP).
ISAC approval number was ISAC_18_290.
ENCEPP registration for the study was EUPAS17543.
Patients can opt out of data sharing.
Acknowledgments
This work uses data provided by patients and collected by the National Health Service as part of their care and support. Medical writing and editorial support were provided by Jennifer Gibson, PharmD, and Leonard Lionnet, PhD, of Kay Square Scientific, LLC. This support was funded by AstraZeneca.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was funded by AstraZeneca.
Disclosure
SC and BE are employees of AstraZeneca.
MA was an employee of AstraZeneca at the time of the study. Her current affiliation is CSL Behring, Milan, Italy.
DBP has advisory board membership with Amgen, AstraZeneca, Boehringer Ingelheim, Chiesi, Circassia, Mylan, Mundipharma, Novartis, Regeneron Pharmaceuticals, Sanofi Genzyme, Teva Pharmaceuticals, Thermofisher, Zentiva (Sanofi Generics); consultancy agreements with Amgen, AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Mylan, Mundipharma, Novartis, Pfizer, Teva Pharmaceuticals, Theravance; grants and unrestricted funding for investigator-initiated studies (conducted through Observational and Pragmatic Research Institute Pte Ltd) from AKL Research and Development Ltd, AstraZeneca, Boehringer Ingelheim, British Lung Foundation, Chiesi, Circassia, Mylan, Mundipharma, Novartis, Pfizer, Regeneron Pharmaceuticals, Respiratory Effectiveness Group, Sanofi Genzyme, Teva Pharmaceuticals, Theravance, UK National Health Service, Zentiva (Sanofi Generics); payment for lectures/speaking engagements from AstraZeneca, Boehringer Ingelheim, Chiesi, Cipla, GlaxoSmithKline, Kyorin, Mylan, Merck, Mundipharma, Novartis, Regeneron Pharmaceuticals, Sanofi Genzyme, Teva Pharmaceuticals, Zentiva (Sanofi Generics); payment for the development of educational materials from Mundipharma, Novartis; payment for travel/accommodation/meeting expenses from AstraZeneca, Boehringer Ingelheim, Mundipharma, Mylan, Novartis, Thermofisher; funding for patient enrolment or completion of research from Novartis; stock/stock options from AKL Research and Development Ltd, which produces phytopharmaceuticals; Consultancy agreements - Fees paid to Observational and Pragmatic Research Institute from Airway Vista Secretariat, EPG Communication Holdings Ltd, FIECON Ltd, Fieldwork International, OM Pharma SA, PeerVoice, Phadia AB, Spirosure Inc, Strategic North Limited, Synapse Research Management Partners S.L, Talos Health Solutions, WebMD Global LLC; owns 74% of the social enterprise Optimum Patient Care Ltd (Australia and UK) and 74% of Observational and Pragmatic Research Institute Pte Ltd (Singapore); 5% shareholding in Timestamp, which develops adherence monitoring technology; is peer reviewer for grant committees of the Efficacy and Mechanism Evaluation programme, and Health Technology Assessment; and was an expert witness for GlaxoSmithKline.
In the last 5 years, IDP has received speaker’s honoraria for speaking at sponsored meetings from AstraZeneca, Boehringer Ingelheim, Aerocrine, Almirall, Novartis, Teva, Chiesi, Sanofi, Regeneron, Menarini, and GlaxoSmithKline and payments for organizing educational events from AstraZeneca, GlaxoSmithKline, Sanofi/Regeneron, and Teva. He has received honoraria for attending advisory panels with Genentech, Sanofi/Regeneron, AstraZeneca, Boehringer Ingelheim, GlaxoSmithKline, Novartis, Teva, Merck, Circassia, Chiesi, and Knopp and payments to support Food and Drug Administration approval meetings from GlaxoSmithKline. He has received sponsorship to attend international scientific meetings from Boehringer Ingelheim, GlaxoSmithKline, AstraZeneca, Teva, and Chiesi. He has received a grant from Chiesi to support a Phase 2 clinical trial in Oxford. He is co-patent holder of the rights to the Leicester Cough Questionnaire and has received payments for its use in clinical trials from Merck, Bayer, and Insmed. In 2014-5, he was an expert witness for a patent dispute involving AstraZeneca and Teva.
VC is affiliated with the Observational and Pragmatic Research Institute and an employee of Optimum Patient Care Global.
CKR received consulting/lecture fees from MSD, AstraZeneca, GlaxoSmithKline, Novartis, Takeda, Mundipharma, Boehringer Ingelheim, Teva, Sanofi, and Bayer.
RJ declares grants from AstraZeneca, GlaxoSmithKline, Novartis, and Teva and personal fees for consultancy, speaker’s fees, or travel support from AstraZeneca, Boehringer Ingelheim, GlaxoSmithKline, Nutricia, and the Observational and Pragmatic Research Institute. RJ was an employee of the University of Plymouth at the time of the study. His current affiliation is Plymouth Marjon University, Plymouth, UK.
MM has received speaker’s fees from AstraZeneca, Boehringer Ingelheim, Chiesi, Cipla, Menarini, Rovi, Bial, Sandoz, Takeda, Zambon, CSL Behring, Grifols, and Novartis; consulting fees from AstraZeneca, Atriva Therapeutics, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Bial, Gebro Pharma, Kamada, CSL Behring, Laboratorios Esteve, Ferrer, Inhibrx, Mereo Biopharma, ONO Pharma, Palobiofarma SL, Takeda, Verona Pharma, TEVA, Spin Therapeutics, pH Pharma, Novartis, Sanofi, and Grifols and research grants from Grifols.
References
1. Eisner MD, Anthonisen N, Coultas D, et al. An official American Thoracic Society public policy statement: novel risk factors and the global burden of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2010;182(5):693–718.
2. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease: 2021 report. Available from: https://goldcopd.org/wp-content/uploads/2020/11/GOLD-REPORT-2021-v1.1-25Nov20_WMV.pdf.
3. Patel AR, Patel AR, Singh S, Singh S, Khawaja I. Global Initiative for Chronic Obstructive Lung Disease: the changes made. Cureus. 2019;11(6):e4985.
4. Singh D, Badadhel M, Brightling CE, et al. Blood eosinophil counts in clinical trials for chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2020;202(5):660–671.
5. Sarwar MR, McDonald VM, Abramson MJ, Paul E, George J. Treatable traits in an English cohort: prevalence and predictors of future decline in lung function and quality of life in COPD. ERJ Open Res. 2021;7(2):00934–2020.
6. Criner GJ, Bartolome RC, Brightling CE, et al. Benralizumab for the prevention of COPD exacerbations. N Engl J Med. 2019;381(11):1023–1034.
7. MacIntyre N, Huang YC. Acute exacerbations and respiratory failure in chronic obstructive pulmonary disease. Proc Am Thorac Soc. 2008;5(4):530–535.
8. Narendra DK, Hanania NA. Targeting IL-5 in COPD. Int J Chron Obstruct Pulmon Dis. 2019;14:1045–1051.
9. Lipson DA, Barnhart F, Brealey N, et al. Once-daily single-inhaler triple versus dual therapy in patients with COPD. N Engl J Med. 2018;378(18):1671–1680.
10. Papi A, Vestbo J, Fabbri L, et al. Extrafine inhaled triple therapy versus dual bronchodilator therapy in chronic obstructive pulmonary disease (TRIBUTE): a double-blind, parallel group, randomised controlled trial. Lancet. 2018;391(10125):1076–1084.
11. Rabe KF, Martinez FJ, Ferguson GT, et al. Triple inhaled therapy at two glucocorticoid doses in moderate-to-very-severe COPD. N Engl J Med. 2020;383(1):35–48.
12. Chen S, Small M, Lindner L, Xu X. Symptomatic burden of COPD for patients receiving dual or triple therapy. Int J Chron Obstruct Pulmon Dis. 2018;13:1365–1376.
13. Bathoorn E, Liesker JJW, Postma DS, et al. Change in inflammation in out-patient COPD patients from stable phase to a subsequent exacerbation. Int J Chron Obstruct Pulmon Dis. 2009;4:101–109.
14. Yun JH, Lamb A, Chase R, et al. Blood eosinophil count thresholds and exacerbations in patients with chronic obstructive pulmonary disease. J Allergy Clin Immunol. 2018;141(6):2037–2047.
15. Müllerová H, Hahn B, Simard EP, Mu G, Hatipoğlu U. Exacerbations and health care resource use among patients with COPD in relation to blood eosinophil counts. Int J Chron Obstruct Pulmon Dis. 2019;14:683–692.
16. McDonald VM, Osadnik CR, Gibson PG. Treatable traits in acute exacerbations of chronic airway diseases. Chron Respir Dis. 2019;16:1479973119867954.
17. Van‘t Hul AJ, Koolen EH, Antons JC, et al. Treatable traits qualifying for nonpharmacological interventions in COPD patients upon first referral to a pulmonologist: the COPD sTRAITosphere. ERJ Open Res. 2020;6(4):00438–2020.
18. David B, Bafadhel M, Koenderman L, De Soyza A. Eosinophilic inflammation in COPD: from an inflammatory marker to a treatable trait. Thorax. 2021;76(2):188–195.
19. Kerkhof M, Sonnappa S, Postma DS, et al. Blood eosinophil count and exacerbation risk in patients with COPD. Eur Respir J. 2017;50(1):1700761.
20. Bafadhel M, Peterson S, De Blas MA, et al. Predictors of exacerbation risk and response to budesonide in patients with chronic obstructive pulmonary disease: a post-hoc analysis of three randomised trials. Lancet Respir Med. 2018;6(2):117–126.
21. Bafadhel A, Singh S, Jenkins C, et al. Reduced risk of clinically important deteriorations by ICS in COPD is eosinophil dependent: a pooled post-hoc analysis. Respir Res. 2020;21(1):17.
22. Kerkhof M, Chaudhry I, Pavord ID, et al. Blood eosinophil count predicts treatment failure and hospital readmission for COPD. ERJ Open Res. 2020;6(4):00188–2020.
23. Voorham J, Corradi M, Papi A, et al. Comparative effectiveness of triple therapy versus dual bronchodilation in COPD. ERJ Open Res. 2019;5(3):00106–2019.
24. Price DB, Rigazio A, Campbell JD, et al. Blood eosinophil count and prospective annual asthma disease burden: a UK cohort study. Lancet Respir Med. 2015;3(11):849–858.
25. Halpin DMG, de Jong HJI, Carter V, Skinner D, Price D. Distribution, temporal stability and appropriateness of therapy of patients with COPD in the UK in relation to GOLD 2019. EClinicalMedicine. 2019;14:32–41.
26. Alcazar-Navarrete B, Garcia-Rop F, Sanchesz G, et al. Burden of disease among exacerbating patients with COPD treated with triple therapy in Spain. Int J Chron Obstruct Pulmon Dis. 2020;16:2149–2161.
27. Kerkhof M, Tran TN, Soriano JJB, et al. Healthcare resource use and costs of severe, uncontrolled eosinophilic asthma in the UK general population. Thorax. 2018;73(2):116–124.
28. Kerkhof M, Sonnappa S, Postma DS, et al. Blood eosinophil count and exacerbation risk in patients with COPD. Eur Resp J. 2017;50(1):1700761.
29. Kerkhof M, Voorham J, Dorinsky P, et al. Association between COPD exacerbations and lung function decline during maintenance therapy. Thorax. 2020;75(9):744–753.
30. Hancox RJ, Pavord ID, Sears MR. Associations between blood eosinophils and decline in lung function among adults with and without asthma. Eur Resp J. 2018;51(4):1702536.
31. Miravitlles M, Monteagudoc M, Solntsevac I, Alcázar B. Blood eosinophil counts and their variability and risk of exacerbations in COPD: a population-based study. Arch Bronconeumol. 2021;57(1):13–20.
32. UK National Health Service. Quality and Outcomes Framework (QOF), enhanced services and core contract extraction specifications (business rules). Available from: http://www.hscic.gov.uk/qof.
33. Clinical Practice Research Datalink. Available from: http://www.cprd.com/home.
34. Boston Collaborative Drug Surveillance Program. The Clinical Practice Research Datalink. Available from: http://www.bu.edu/bcdsp/gprd.
35. UK National Health Service. Hospital Episode Statistics (HES). Available from: http://content.digital.nhs.uk/hes.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


