Back to Journals » Drug, Healthcare and Patient Safety » Volume 14
Opioid Utilization and Management in the Setting of Stewardship During Inpatient Rehab Care
Authors Murphy L , Leblanc K, Badr S, Ching E, Mao L, Steenhof N, Hamandi B , Rubin B, Seto A, Furlan AD
Received 4 February 2022
Accepted for publication 11 August 2022
Published 11 September 2022 Volume 2022:14 Pages 161—170
DOI https://doi.org/10.2147/DHPS.S360832
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Siew Siang Chua
Laura Murphy,1– 3 Kori Leblanc,1,2,4 Souzi Badr,1,2 Emily Ching,1 Lynda Mao,1,2 Naomi Steenhof,1,2 Bassem Hamandi,1,2,4 Bonita Rubin,1,2 Ada Seto,1 Andrea D Furlan3,5,6
1Department of Pharmacy, University Health Network, Toronto, ON, Canada; 2Leslie Dan Faculty of Pharmacy, University of Toronto, Toronto, ON, Canada; 3KITE Research Institute, University Health Network, Toronto, ON, Canada; 4Toronto General Hospital Research Institute, University Health Network, Toronto, ON, Canada; 5Department of Medicine, University of Toronto, Toronto, ON, Canada; 6Institute for Work & Health, Toronto, ON, Canada
Correspondence: Laura Murphy, Department of Pharmacy, University Health Network, 550 University Ave, Toronto, ON, M5G 2A2, Canada, Tel +1 416-597-3422 x 3657, Fax +1 416-260-2658, Email [email protected]
Background: Opioid utilization and management in an inpatient rehabilitation setting have not been widely described, despite the unique opportunities that exist in this setting to support opioid stewardship across transitions in care. We aimed to characterize opioid utilization and management by interprofessional teams across a large, inpatient rehabilitation setting after incorporation of opioid stewardship principles by pharmacists as part of their daily practice.
Patients and methods: This was a retrospective chart review at Toronto Rehab, University Health Network, Toronto, Canada. Patients with admission orders for any opioid from November 2017 to February 2018 were included. Complex continuing care and palliative care patients were excluded. Descriptive statistics were primarily used to describe the data as well as univariate linear regression to compare associations with milligram morphine equivalent (MME) reduction.
Results: A total of 448 patients were included. A reduction in total daily MME was seen in 49% (n=219) of the patients during their inpatient stay, with 73% (n=159) of these patients having a reduction of ≥ 50%. Sixty-nine percent (n=311) of the patients received an opioid prescription at discharge, with most scheduled (90%, n=98) with a supply of less than 30 days. Rehabilitation length of stay was correlated with a MME decrease during rehab (p< 0.01), suggesting that longer lengths of stay contributed to a greater reduction in MME. Patients with chronic opioid use prior to acute care admission (p=0.01), and those who started extended-release opioids during acute care (p=0.02) were significantly less likely to discontinue opioids during rehab stay.
Conclusion: Opioid utilization and management in the setting of opioid stewardship across inpatient rehab and transitions of care were characterized. Opportunities exist for further quality improvement initiatives within inpatient rehabilitation and acute care settings to identify and support patients with complex pain management needs.
Keywords: opioid, pain management, medication reconciliation, pharmacy practice, medication safety, discharge prescription
Introduction
In 2018, 4.6 million people in Canada, almost 1 in 8 people, were prescribed opioids to treat pain.1 Opioid prescriptions have made a significant contribution to the ongoing opioid epidemic, with 24,626 apparent opioid-related deaths occurring between January 2016 and June 2021 in Canada, though current drivers are primarily fentanyl and fentanyl analogues.2 Action to address the opioid epidemic in Canada by influencing opioid prescribing and de-prescribing practices has unintentionally resulted in stigmatization and suffering for some individuals with pain.3–6
Opioids remain an important part of a multimodal approach to treat acute and some chronic pain conditions. However, long-term use of opioids, particularly at high doses, is associated with significant risk, including an increased risk of opioid-related death, opioid use disorder, hyperalgesia, sleep apnea, fractures, hypogonadism, and immunosuppression.7–10
Prescribing practices in the inpatient hospital setting may be associated with potential patient harms through excessive prescribing of opioids on discharge from hospital, improper handling of unused opioids, and unintentional prolonged opioid use after discharge.11 Opioids prescribed at discharge may frequently go unused by patients. A systematic review reported patients used only 38% of the prescribed opioids after discharge.11 In addition, while 10% of the opioid-naïve patients were still consuming opioids 3-months after hospital discharge from a surgical admission, the rate increased to 78% in those with chronic opioid use prior to hospital admission. Prolonged use after surgical inpatient care was also associated with preoperative opioid use, use of other substances (eg, tobacco, antidepressants, and benzodiazepines), specific comorbidities (eg, preoperative pain disorder and psychiatric disorders), and invasive surgical procedures.11 Opioid stewardship, defined as the use of coordinated interventions to improve, monitor, and evaluate the use of opioids to support and protect human health,12 has been successful in acute inpatient settings to improve opioid prescribing and reduce overprescribing at discharge.13 Pharmacist-directed initiatives in the acute inpatient setting, in particular, including a pharmacist-directed pain management service that reduced opioid prescribing, have also been described.14
Physical medicine and rehabilitation physicians prescribe opioids at high rates amongst the medical specialties,15 but very little research has characterized prescribing and use during inpatient rehabilitation. One study in the United States found that during inpatient rehabilitation, a majority of patients were using low doses throughout the course of their admission and 25% of the patients decreased opioid utilization between admission and discharge.16 As an inpatient rehabilitation length of stay is typically longer than in acute care and rehabilitation is likely the last institutional stay prior to a return to community living, rehabilitation presents unique opportunities for opioid stewardship. A retrospective chart review demonstrated that access to a clinical nurse specialist with pain management expertise allowed for a significantly faster reduction in opioid use in an inpatient rehab hospital, compared to standard pain management from a medical team.17 The role of pharmacists in promoting opioid stewardship in inpatient rehabilitation settings has not been described.
In 2017, all pharmacists at Toronto Rehab, a 429-inpatient bed multisite rehabilitation hospital, part of the University Health Network in Toronto, ON, Canada, incorporated principles of opioid stewardship into their daily practice, which included documentation of milligram morphine equivalents (MME) on admission and collaboration with the interprofessional team and patient to manage opioid therapy balancing safety and efficacy. We aimed to characterize opioid utilization in our inpatient rehabilitation setting and management by the interprofessional team following this initiative and to inform further opioid stewardship initiatives for patients who experience pain as they transition across care settings.
Objectives
- Describe opioid utilization during inpatient rehabilitation admission and through transitions in care.
- Characterize the proportion of patients with a decrease in daily MME during an inpatient rehabilitation admission.
- Describe quantities of opioids provided on discharge prescriptions when patients are discharged from inpatient rehabilitation.
Methods
Study Design and Setting
We conducted a retrospective chart review of adult patients admitted to Toronto Rehab. Patients included those in Musculoskeletal and Multi-system, Brain and Spinal Cord, Geriatric and Geriatric Psychiatry, and Low Tolerance Long Duration rehabilitation programs. This study was approved by the University Health Network Research Ethics Board (REB), reference number 18.5125. The need to obtain informed consent was waived by the REB as all data collected were in the routine process of care and data were extracted retrospectively after individuals were discharged from hospital, the use of information did not impact care and it was considered impractical to obtain consent. Every precaution was taken to protect the privacy of individuals in accordance with the Declaration of Helsinki.
Patients Included
Adult patients admitted to an inpatient rehabilitation program from November 1, 2017, through February 28, 2018, with admission orders for any opioid therapy (codeine and codeine-containing products, buprenorphine, morphine, oxycodone, hydromorphone, fentanyl, tramadol, tapentadol, or methadone) were included. Exclusion criteria were admission to the Complex Continuing Care (longer lengths of stay were unlikely to include both admission and discharge data during the study period) or Palliative Care (unique goals of therapy related to opioids) programs.
Data Collection
Data were retrieved from electronic and paper-based patient and pharmacy records. Study variables included demographics (age and sex), length of stay, medical history and pain diagnosis, opioid use (drug, dose, and formulation), selected concurrent non-opioid medication use (pain medications and benzodiazepines/sedatives), and discharge prescription data (opioid prescription and naloxone prescribing). Pain during admission to inpatient rehabilitation was characterized using the 0-to-10 Numerical Rating Scale at admission, during the admission, or at the time of discharge.
Pain types were classified using the International Classification of Diseases 11th edition.18 Total daily opioid doses were converted to MME using standardized conversion factors.19 Reduction in daily MME during inpatient rehabilitation admission was calculated using the difference between the total opioid dose administered on the day of admission and the total opioid dose administered the day prior to discharge. Daily MMEs were calculated at four time points during a patient’s transition in care: opioid dose prior to acute care admission, on the day of discharge from acute care, and on the first and last day of admission to inpatient rehabilitation.
Data Analysis
Descriptive statistics were characterized using Microsoft Excel® (Microsoft Inc., Redmond, WA, USA). Statistical analyses were performed using SPSS, version 20 (IBM Corp., Armonk, NY, USA). Chi-square tests were used for categorical data, and t-tests were used for continuous data. Univariate linear regression was used to compare associations in daily MME reduction.
Results
In total, 448 consecutive patients at Toronto Rehab with admission orders for opioids were included in this study.
Characteristics of Included Patients
Table 1 describes the characteristics of included patients. Mean age was 68 ± 17 years and 59% (n=266) of the patients included were female. There were 70% (n=313) of the patients with a diagnosis related to chronic pain documented in their medical record and 33% (n=147) had used opioids prior to acute care admission. Of those who used opioids while at home, their median daily MME was 27 (Interquartile range (IQR) 14–63). Of the patients included, median daily MME at the time of admission to inpatient rehabilitation was 20 (IQR 5–50), with a range of 0–575. Forty-three percent (n=194) were admitted to acute care related to a physical injury or trauma, and 77% (n=347) had a surgical procedure in acute care. The median length of rehab stay was 21 days (IQR 13–36). Pain intensity ratings using the Numerical Rating Scale (0–10) were documented on admission for 83% (n=370) of the patients admitted to rehabilitation, with a median rating of 4 (IQR 1–6). These were documented again prior to discharge in 70% (n=312) of the patients, with a median of 0 (IQR 0–3.75).
 |
Table 1 Characteristics of Included Patients |
Opioid Management Across Transitions in Care
On the first day of admission to inpatient rehabilitation, 16% (n=70/448) had a daily MME=0, despite having admission orders for opioids. Figure 1 illustrates the distribution of daily MME utilization (for patients with daily MME>0) at different time points across transitions in care.
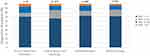 |
Figure 1 Opioid utilization by milligram morphine equivalent (MME) category at time points across transitions in care. |
The most commonly used opioid drug at home was codeine and codeine-containing combination products (eg, acetaminophen-caffeine-codeine) at 33% (n=51). Hydromorphone was the most commonly used opioid in acute care (81%, n=365) and inpatient rehabilitation (83%, n=371). One percent (n=6) of the patients were using methadone (n=4) or buprenorphine/naloxone (n=2) for opioid agonist therapy at home and this was continued across transitions in care.
Six percent (n=27) of the people used extended-release (ER) opioids at home, 17% (n=74) used ER opioids in acute care, and 26% (n=115) were using ER opioids at the time of discharge from rehabilitation. Ten percent (n=47) of the people were started on new long-acting opioids in acute care and 9% (n=41) were started on long-acting opioids during their inpatient rehabilitation stay.
Opioid Management During Inpatient Rehabilitation
Forty-nine percent (n=219) of the patients had a reduction in total daily MME during their inpatient rehabilitation stay and of these, 73% (n=159) had a reduction of ≥50%. Eighteen percent (n=82) discontinued opioids completely prior to discharge from rehab. Twenty-five percent of the patients included (n=111) had an increase in their daily MME during their inpatient rehabilitation stay. The median change in daily MME during the rehabilitation stay was −29% (IQR −88% to +13%). Within the subgroup of patients using a daily MME>200 (n=17), 59% (n=10) had any decrease in their daily MME, 29% (n=5) had no change, and 12% (n=2) had a further increase in their daily MME during their rehabilitation stay. One patient achieved a reduction in daily MME of ≥50%.
Patients with a ≥ 50% daily MME decrease compared with those with a <50% reduction were more likely to be in the Brain and Spinal cord rehab programs or have documented reasons for acute pain during hospitalization, such as surgery or trauma in acute care. Patients with a <50% daily MME decrease were more likely to be in the Musculoskeletal and Multi-system rehab program (p=0.03), have a pre-admission diagnosis of chronic pain (p=0.03), or use opioids prior to hospital admission (p=0.002). Univariate linear regression analysis is described in Table 2. Median daily MME on the day of discharge from inpatient rehab was 10 (IQR 0–45), with a range of 0–550.
 |  |  |
Table 2 Univariate Linear Regression: Decrease in Milligram Morphine Equivalent (MME) |
Concurrent Non-Opioid Medications
During inpatient rehabilitation, 94% (n=421) of the patients included used acetaminophen, 46% (n=205) used non-steroidal anti-inflammatory drugs, 17% (n=77) used gabapentinoids, 10% (n=45) used tricyclic antidepressants, 8% (n=37) used serotonin-norepinephrine reuptake inhibitors, 11% (n=51) used muscle relaxants, and 2% (n=11) used cannabinoids. Thirteen percent (n=59) received concurrent benzodiazepines, and 21% (n=94) received sedatives.
Discharge Opioid Prescriptions
At discharge, 69% (n=311) of the patients sampled received a prescription for opioids. Of those prescriptions, 94% (n=292) included “as-needed” opioids, and 42% (n=132) included scheduled opioids. Figure 2 illustrates the quantities of “as-needed” and scheduled opioids prescribed at discharge from rehabilitation. Twenty-three percent (n=105) received a discharge prescription that included an extended-release (ER) opioid. Of the people using opioids prior to hospital admission, 23% (n=35) did not receive a discharge prescription for opioids. All patients (n=17) with a daily MME >200 at the time of admission to rehab were discharged with an opioid prescription. Two percent (n=7) of the patients received a recommendation for naloxone at discharge.
 |
Figure 2 Opioid prescriptions at discharge from inpatient rehabilitation, as (A) quantity of “as-needed” doses and (B) days supply of scheduled opioids. |
Discussion
This study characterized opioid utilization in a large inpatient rehabilitation setting guided by the interprofessional team which included pharmacists empowered as opioid stewards. Key findings from this study were that one in two people with admission orders for opioids in rehab had a reduction in their daily MME prior to discharge and one in three people decreased their dose by 50% or more prior to discharge. These changes were in the context of a median pain intensity decrease from admission to when they were assessed at follow-up during the admission or at the time of discharge from rehab. A reduction in daily MME was more likely for patients with a longer length of stay and less likely if a long-acting opioid had been initiated in acute care. This may have been because the longer length of stay provides time for healing and likely allows interprofessional team more time to work collaboratively with patients to implement individualized pain management care plans. Starting an ER opioid in acute care may reflect an underlying complexity in pain management needs.
One in five patients stopped their opioids before they were discharged. This proportion was not different in people using opioids at home prior to hospital admission. A high proportion of patients (70%, n=313) had a diagnosis related to chronic pain documented in their chart, compared with an expected 20% of the Canadian population. We believe this highlights the medical complexity of people who are admitted for inpatient rehabilitation in our facility post-acute care. Despite the high rate of chronic pain diagnoses, many patients were not on opioids prior to acute care admission and the median daily MME on the day of discharge from inpatient rehab was low, with only a small proportion of patients using higher daily doses including those above 200 MME. The median daily MME from our study was similar to the findings of Przybysz et al at discharge from another rehabilitation setting.16 Notably, both were lower than the 152.5 median daily MME reported in a systematic review of five studies involving opioid-naïve adults in the acute care setting.11 Despite these overall positive results, there was less success within the small subgroup of people admitted to rehabilitation with daily MME >200 (n=17), a dose which presents the highest risk long-term. Only one person reached a daily MME reduction of >50% and two people increased their MME further during rehab. Clinically, this is not unexpected, given the complexity of opioid management for people using very high doses of opioids as they may be experiencing problems such as acute-on-chronic pain or opioid-induced hyperalgesia.
The most commonly used opioid in hospital was hydromorphone, both in acute care and rehabilitation, despite it being five times more potent than morphine. This is likely because hydromorphone poses no concern for accumulation in renal insufficiency. There may be some opportunities to shift prescribing practice to use of a lower potency opioid in hospitals for appropriate patients, which would then impact the choice of opioid on discharge prescriptions and/or may facilitate opioid discontinuation by the time of discharge. Most patients also received non-opioid pain medications, often in an effort to take a multimodal approach to pain management, with daily MME reduction being a major objective. A low proportion of patients received concurrent benzodiazepines.
Worth noting were the significant number of patients with admission orders for opioids who did not have a rating for pain intensity documented on admission to rehabilitation (n=78). Documentation of a follow-up score during the stay was also absent from many charts (n=136). Supporting appropriate pain management with standardized assessment tools of intensity and functional impairment could be beneficial for individualized care plans. Encouraging the use of these tools by building them into documentation templates and hospital guidelines would support best practices. There may also be an opportunity to improve early identification of people who may need more education or management, since this tool was previously found to be useful to identify people who are likely to continue on opioids long-term.20
One-third of patients did not receive a discharge prescription for opioids, which was similar to the findings of Przybysz et al, also from a rehabilitation setting.16 Most of the discharge prescriptions were for hydromorphone, reflecting the preference for use of hydromorphone at our hospital. Of the prescriptions for scheduled opioids, most scheduled opioid prescriptions were for a supply of <30 days. The goal of providing an appropriate quantity after rehabilitation is to ensure continuity of care, by providing patients with sufficient time to connect with their primary care provider after discharge. The quantities of “as-needed” doses seem to be in line with this approach. We do not know if opioid tablets after discharge from rehabilitation were unused, though it has been reported that there is a high proportion of opioids prescribed post-surgery in acute care are not used by patients.21 This presents a potential point of opportunity for prescribers to reduce opioid quantities, waste, and risk to patients once they are home. A very low proportion of discharge opioid prescriptions from rehabilitation included recommendations for naloxone kits to be dispensed by the community pharmacist, representing another possible area of improvement from a patient safety and harm reduction perspective.
The strengths of this study are its size and detailed characterization of an inpatient rehabilitation opioid utilization with links to management across care transitions and discharge prescribing practices. We acknowledge the limitations of retrospective studies, including incomplete chart documentation. Further quality improvement studies are needed to address the opportunities identified and to follow up with patients long-term to understand the implications of management in the inpatient setting. Particular attention to the management of pain and opioid use for patients admitted to rehabilitation settings using daily MME >200 is warranted. Characterization of opioid utilization in acute care, with a focus on new start of ER opioids may be useful for understanding the implications downstream opioid use in during rehabilitation stays.
Conclusion
Results from this study describe opioid utilization and management in the setting of opioid stewardship by pharmacists and the interprofessional teams at Toronto Rehab and across transitions in care. These results offer new perspectives on the current state and areas of opportunity for quality improvement initiatives within inpatient rehabilitation and acute care settings to identify and support patients with complex pain management needs.
Acknowledgments
The authors would like to acknowledge the contributions of Cynthia Selvanathan, Kristen Conte, Kuo-En Huang, Cheng-Yu Lin, Caylie Poirier, Ashley Sharifara and Tiffany Wu, who contributed to this work while they were pharmacy students of the Leslie Dan Faculty of Pharmacy, University of Toronto. They would also like to acknowledge the contributions of Jordanne Feldberg and Shiming Sun, who volunteered their time while they were pharmacy students at the Leslie Dan Faculty of Pharmacy, University of Toronto.
Disclosure
Dr Andrea Furlan reports grants from Canadian Generic Product Association, outside the submitted work, and Dr Andrea Furlan has a YouTube monetized channel and she receives payments from Ads. The channel is about chronic pain. The authors report no other conflicts of interest in this work.
References
1. Canadian Institute for Health Information. Opioid Prescribing in Canada: how are Practices Changing? Ottawa, ON: CIHI; 2019. Available from: https://www.cihi.ca/sites/default/files/document/opioid-prescribing-canada-trends-en-web.pdf.
2. Special Advisory Committee on the Epidemic of Opioid Overdoses. Opioid and stimulant-related harms in Canada. Ottawa: Public Health Agency of Canada; 2021. Available from: https://health-infobase.canada.ca/substance-related-harms/opioids-stimulants.
3. Antoniou T, Ala-Leppilampi K, Shearer D, Parsons JA, Tadrous M, Gomes T. “Like being put on an ice floe and shoved away”: a qualitative study of the impacts of opioid-related policy changes on people who take opioids. Int J Drug Policy. 2019;66:15–22. doi:10.1016/j.drugpo.2019.01.015
4. Dassieu L, Heino A, Develay É, et al. “They think you’re trying to get the drug”: qualitative investigation of chronic pain patients’ health care experiences during the opioid overdose epidemic in Canada. Can J Pain. 2021;5:66–80. doi:10.1080/24740527.2021.1881886
5. Darnall BD, Juurlink D, Kerns RD, et al. International stakeholder community of pain experts and leaders call for an urgent action on forced opioid tapering. Pain Med. 2019;20(3):429–433. doi:10.1093/pm/pny228
6. Sinha CB, Bakshi N, Ross D, Krishnamurti L. Management of chronic pain in adults living with sickle cell disease in the era of the opioid epidemic: a qualitative study. JAMA Netw Open. 2019;2(5):e194410. doi:10.1001/jamanetworkopen.2019.4410
7. Yi P, Pryzbylkowski P. Opioid Induced Hyperalgesia. Pain Med. 2015;16(Suppl 1):S32–6. doi:10.1111/pme.12914
8. Gomes T, Mamdani A, Dhalla I, Paterson J, Juurlink D. Opioid dose and drug-related mortality in patients with nonmalignant pain. Arch Intern Med. 2011;171:686–691. doi:10.1001/archinternmed.2011.117
9. Baldini A, Von Korff M, Lin EHB. A review of potential adverse effects of long-term opioid therapy: a practitioner’s guide. Prim Care Companion CNS. 2012;14(3):
10. Voon P, Karamouzian M, Kerr T. Chronic pain and opioid misuse: a review of reviews. Subst Abuse Treat Prev Policy. 2017;12(1):36. doi:10.1186/s13011-017-0120-7
11. Arwi GA, Schug SA. Potential for harm associated with discharge opioids after hospital stay: a systematic review. Drugs. 2020;80(6):573–585. doi:10.1007/s40265-020-01294-z
12. ISMP Canada. Opioid Stewardship; 2021. Available from: https://www.ismp-canada.org/opioid_stewardship/.
13. Burns S, Urman R, Pian R, Coppes OJM. Reducing new persistent opioid use after surgery: a review of interventions. Curr Pain Headache Rep. 2021;25(5):27. doi:10.1007/s11916-021-00943-6
14. Poirier RH, Brown CS, Baggenstos YT, et al. Impact of a pharmacist-directed pain management service on inpatient opioid use, pain control, and patient safety. Am J Health Syst Pharm. 2019;76(1):17–25. doi:10.1093/ajhp/zxy003
15. Levy B, Paulozzi L, Mack KA, Jones CM. Trends in opioid analgesic–prescribing rates by specialty, U.S., 2007–2012. Am J Prev Med. 2015;49(3):409–413. doi:10.1016/j.amepre.2015.02.020
16. Przybysz AG, Khudeira Z, Khudeira S, et al. Opioid prescribing and utilization during acute inpatient rehabilitation admissions. Pain Med. 2021. doi:10.1093/pm/pnab107
17. Urton MS, Rohlik E, Farrell M, Ng W, Woodard EK. Decreasing opioid utilization in rehabilitation patients using a clinical nurse specialist pain consultant program. Arch Phys Med Rehabil. 2017;98(12):2491–2497. doi:10.1016/j.apmr.2017.05.026
18. Treede RD, Rief W, Barke A, et al. Chronic pain as a symptom or a disease: the IASP classification of chronic pain for the international classification of diseases (ICD-11). Pain. 2019;160(1):19–27. doi:10.1097/j.pain.0000000000001384
19. Busse J. The 2017 Canadian Guideline for Opioids for Chronic Non-Cancer Pain. Hamilton (ON): McMaster University; 2017. Available from: nationalpaincentre.mcmaster.ca.
20. Furlan AD, Hassan S, Famiyeh IM, Wang W, Dhanju J. Long-term opioid use after discharge from inpatient musculoskeletal rehabilitation. J Rehabil Med. 2016;48(5):464–468. doi:10.2340/16501977-2080
21. Bui T, Grygiel R, Konstantatos A, et al. The impact of an innovative pharmacist-led inpatient opioid de-escalation intervention in post-operative orthopedic patients. J Opioid Manag. 2020;16(3):167–176. doi:10.5055/jom.2020.0565
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
