Back to Journals » Journal of Multidisciplinary Healthcare » Volume 16
Machine Learning in Cardiology: A Potential Real-World Solution in Low- and Middle-Income Countries
Authors Alabdaljabar MS , Hasan B, Noseworthy PA, Maalouf JF, Ammash NM, Hashmi SK
Received 28 July 2022
Accepted for publication 7 November 2022
Published 28 January 2023 Volume 2023:16 Pages 285—295
DOI https://doi.org/10.2147/JMDH.S383810
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Mohamad S Alabdaljabar,1,2 Babar Hasan,3 Peter A Noseworthy,4 Joseph F Maalouf,4,5 Naser M Ammash,4,5 Shahrukh K Hashmi5,6
1Department of Internal Medicine, Mayo Clinic, Rochester, MN, USA; 2College of Medicine, Alfaisal University, Riyadh, Saudi Arabia; 3Sindh Institute of Urology and Transplantation (SIUT), Karachi, Pakistan; 4Department of Cardiovascular Medicine, Mayo Clinic, Rochester, MN, USA; 5Department of Medicine, Sheikh Shakhbout Medical City, Abu Dhabi, United Arab Emirates; 6Division of Hematology, Department of Medicine, Mayo Clinic, Rochester, MN, USA
Correspondence: Shahrukh K Hashmi, Department of Medicine, SSMC, Abu Dhabi, United Arab Emirates, Email [email protected]
Abstract: Artificial intelligence (AI) and machine learning (ML) is a promising field of cardiovascular medicine. Many AI tools have been shown to be efficacious with a high level of accuracy. Yet, their use in real life is not well established. In the era of health technology and data science, it is crucial to consider how these tools could improve healthcare delivery. This is particularly important in countries with limited resources, such as low- and middle-income countries (LMICs). LMICs have many barriers in the care continuum of cardiovascular diseases (CVD), and big portion of these barriers come from scarcity of resources, mainly financial and human power constraints. AI/ML could potentially improve healthcare delivery if appropriately applied in these countries. Expectedly, the current literature lacks original articles about AI/ML originating from these countries. It is important to start early with a stepwise approach to understand the obstacles these countries face in order to develop AI/ML-based solutions. This could be detrimental to many patients’ lives, in addition to other expected advantages in other sectors, including the economy sector. In this report, we aim to review what is known about AI/ML in cardiovascular medicine, and to discuss how it could benefit LMICs.
Keywords: artificial intelligence, machine learning, cardiology, low, middle, income, countries
Plain Language Summary
- AI/ML is a rapidly developing field that could improve healthcare delivery and disease outcome in many medical fields, and cardiology in particular.
- AI/ML could potentially improve healthcare delivery in LMICs if appropriately applied; however, this necessitates a thorough understanding of the obstacles that these countries face in the health-care sector.
- AI implementation in LMICs is not only the issue of finding the problem and developing an ML-based solution. It is a collective teamwork between physicians, AI/ML developers, policy makers, researchers, and educators to fully understand the issues and subsequently find practical solutions. All components are vital, and the absence of any of them could be detrimental to AI/ML implementation in LMICs.
Introduction
Artificial Intelligence (AI), specifically Machine Learning (ML), is expected to improve health-care operations and delivery.1 In some countries, it is already revolutionizing the health-care sector. Economically, it is expected that AI can reduce United States (US) healthcare expenditure by 150 billion dollars by 2026.1 Hence, it is speculated that ML could be of particular aid to low- and middle-income countries (LMICs) where human and financial resources are comparatively constrained.2 Cardiology is of central importance in LMICs since cardiovascular disease (CVD) prevalence and death rates are the highest in these countries and cardiovascular care is costly and often complex.3,4
Late diagnosis and presentation, co-morbidities including infections and malnutrition, fragmented referral system, lack of advanced diagnostic facilities, shortage of skilled teams, and inadequate financial support systems are among the leading causes of poor outcomes associated with cardiac diseases and their management in LMICs.5,6 AI technology can potentially bring considerable expertise close to where patients live by better focusing on population health, functioning as a clinical decision supporting tool for physicians, assisting in virtual health care for continuity of care, and triaging patients as a front-line server. Such a solution may help bridge the gaps in a patient’s care continuum with CVD in LMICs. However, AI application in these countries will likely face some challenges on both, systemic (ie, less-developed health informatics ecosystems) and individual levels (ie, access to internet, smart devices). This report provides an overview of AI/ML, discusses what is known about ML in LMICs and explores how AI/ML can potentially improve cardiovascular medicine in LMICs.
AI Basics: The Process of Learning
To analyze complex input, one can breakdown inputs using pattern recognition in a step-by-step approach. Figure 1S shows a simple representation of an assumed algorithm for our brain. Within this theoretical framework, the learning process can be broken down into smaller parts of 1) feeding and 2) neural networks that interact in a dynamic way to reach a final decision. According to the American Psychological Association (APA) dictionary of psychology, learning is defined as “the acquisition of novel information, behaviors, or abilities after practice, observation, or other experiences, as evidenced by a change in behavior, knowledge, or brain function”.7
To understand ML, it is crucial to describe common terms used in the AI field.8 There are several types of ML, including deep learning, supervised learning (SL), unsupervised learning (UL), and reinforcement learning.9 DL is made of numerous algorithms arranged to give machines the ability to learn from a vast amount of data using multilayer neural networks. SL and UL refer to teaching machines with labeled versus unlabeled data, respectively. The former can aid in pattern recognition, whereas UL can be used to discover unnoticed patterns. Reinforcement learning, derived from the psychological term “reinforcement”, functions using a trial-and-error mode, wherein systems are reward-driven, so they keep going back and forth trying different steps to achieve the desired outcome. All these ways receive input, process the data, and generate a certain outcome (Figure 1).
AI/ML in Medicine
Although the efficacy of most of the AI software has been demonstrated in many research applications, their effectiveness in practice is yet to be as well established. The potential utility of AI has been demonstrated in pharmaceutical, medical (diagnosis, treatment, and follow-up), and analytical purposes.10 For instance, systems have been created that can recognize consolidation on chest x-rays with minimal human input. Figure 2S depicts a simplified diagram of a presumed AI algorithm for consolidation detection. Behzadi-Khormouji et al published an AI model that can detect consolidation on CXR with an accuracy of 94.7%.11
Current literature has numerous articles, with promising results, that shed the light on AI applications in different fields of medicine (Figure 3S) including nephrology12 (acute kidney injury and chronic kidney disease alert systems, wearable dialysis devices, kidney transplantation prognosis), neurology13 (epilepsy, stroke, dementia, movement disorders), dermatology14 (tumors, ulcers, inflammatory lesions, dermatopathology), endocrinology,15 surgery,16 obstetrics and gynecology17 (risk assessment of preterm labor, pregnancy complication, gynecological surgery) in addition to cardiology. AI was an important tool against the coronavirus during the pandemic, with different successful applications. During the COVID-19 pandemic, AI has been used as a warning system, diagnostic and prognostic tool, and in building robots that aid in food and medications delivery to quarantined patients,18 although with high risk of bias in majority of tools during the COVID-19 pandemic, perhaps due to short period between development to application because of the pandemic.19 Many AI-based software packages have already been approved by the US Food and Drug Administration (US-FDA), including diagnostic software for CVD.20
Cardiology and ML in Low- and Middle-Income Countries: What is Already Known?
As per the World Development Indicators, 2016, countries can be categorized based on income.21,22 Around 90% of the worldwide CVD burden is present in the LMICs, yet surprisingly, they only have 10% of research and health-care resources required to deal with this issue.23 The greatest percentage of deaths due to CVD worldwide is present in LMICs, which is estimated to be around 80%.24 Due to this burden, it is believed that efforts to decrease CVD’s impact would have the greatest global effect in these countries.25 Interestingly, Rosengren et al showed that the risk factor profile for CVD is considered optimum in low-income countries among all income groups, except for high blood pressure, in which low-income countries rank first.26 However, it is impractical to generalize this since many of the LMIC do not have population-based studies on CVD incidence, prevalence, and associated risk profiles.
Another challenge is the inappropriate number of physicians in different parts of the world. As of 2020, according to the WHO, there is one medical doctor for 3324 persons in Africa, 1239 Southeast Asia, 989 Eastern Mediterranean, 533 Western Pacific, 417 Americas, and 293 in Europe.27 Most low-income countries are located in Africa and Southeast Asia, which can further support the linear relationship between their weak economies and numbers of physicians in these countries, since increased numbers of physicians is associated with overall better healthcare quality.28 The lack of resources has been inversely proportional to major adverse cardiovascular events. By targeting patients with high CVD risk, a study assessed the association between major adverse cardiovascular events and the availability and affordability of three classes of medications that are essential and commonly used in cardiology (anti-hypertensive agents, antiplatelets, and statins). They included patients from low, lower-middle, upper-middle, and high-income countries. They were divided into three groups based on medications availability and affordability (group: 1 available and affordable; 2: available but not affordable; 3: not available). In comparison to group 1, major CVD events were higher in group 2 (hazard ratios [HR] 1.19, 95% CI 1.07 to 1.31) and group 3 (HR 1.25, 95% CI 1.08 to 1.50). Expectedly, low and lower-middle-income countries had the lowest percentages in group 1 and group 2; in other words, medications availability and affordability were directly proportional to the country’s income (ie, low-income countries had the lowest percentages in both groups).29 This example highlights the important relationship between limited resources of lower-income countries with CVD outcomes.
LMICs have a low expenditure on healthcare and its workforce, which is expected to be inversely linked to the number of deaths from CVD since the management requires both resources and well-trained personnel.30 Delay of diagnosis and treatment is among the most important reasons which make CVD the top cause of death. While this delay is often related to the fact that heart diseases develop insidiously and present acutely, in LMICs, this might not be the only reason behind their high fatality, where resources are scarce compared to the other countries.
Potential Advantages of AI/ML in Cardiology
In cardiology, AI has been well studied and has various applications. AI can be applied at least to 5 domains of cardiology, including electrophysiology, imaging, heart failure, preventive, and interventional cardiology. Atrial fibrillation (AF) is an example that can be diagnosed with an ECG where AI/ML can be applied to aid in this. Algorithmically speaking, ECGs can be broken down to heart rate, regularity, waves (P-QRS-T), intervals, and segments. Figure 2 shows a suggested AI algorithm that can detect AF. Noteworthy, AI not only uses the classical ECG findings to diagnose AF but also can do that with subtle ECG changes that often go unnoticed by the naked eye. A recently developed AI model was able to detect AF using a single normal sinus rhythm (NSR) ECG with an accuracy of 79.4% (receiver operating characteristic [ROC] curve, area under the curve [AUC] = 0.87), which increased to an accuracy of 83.3% (AUC = 0.90) when multiple ECGs were used.31 Thus, one can speculate that shortly a low cost, widely available test such as ECGs can function as a great diagnostic tool for AF before it is clinically apparent, with high diagnostic abilities that are comparable to other tests such as B-type natriuretic peptide for heart failure (AUC 0.60–0.70)32 and the CHA2DS2-VASc Score33 for stroke risk assessment (AUC 0.57–0.72).31 However, this would first need a rigorous validation in a particular geographic location before considering implementing clinically.
 |
Figure 2 Simplified algorithm in the field of cardiology that can help in atrial fibrillation diagnosis and treatment. Abbreviation: AC, Anti-coagulation. |
Data is extracted from ECGs; however, this type of data needs special means to detect the hidden patterns, since in our example, NSR was used for AF detection. These commonly appearing ECGs carried a particular AF “signature”, as described by Attia et al.31 This could also aid in decreasing the time to initiate treatment. In our example, time refers to the fact that early detection of AF allows early initiation of therapy (if indicated) or stroke prevention measures, which may potentially reduce the risk of AF complications (ie cardiovascular, neurological), its associated significant socio-economic impact given the potential for long-term morbidity and even death. If well implemented in countries with limited resources, this AF AI algorithm could provide substantial clinical (eg, early AF detection) and economic (eg, less testing, less loss of productivity) benefits.34 Nonetheless, it is essential to consider that detecting AF in NSR could lead to more downstream testing (eg, long-term monitors), and this could increase incidental ECG findings. More testing means higher demand for resources, which could be detrimental to LMICs.
To date, many randomized clinical trials (RCT) have been published about ML in Cardiology. To evaluate this, PubMed Search was done (June 6th, 2022) using the following search string: machine learning AND Cardiology, and by applying “clinical trials” filter. This search string generated 43 results, 37 studies of which are focused on cardiology and ML and are RCT. These RCT focused on all 5 different fields of cardiology and started to be published in 2017 onward. Gevaert et al have shown that clinical phenotypes are more helpful than left ventricular ejection fraction (LVEF) in predicting heart failure outcomes (n = 1693).35 This was done through cluster analysis of UL, which detected 6 phenotypes that are LVEF-independent. Primary composite outcome (all-cause death or rehospitalization) at 6 months had an HR of 1.25 (95% CI 1.00–1.58 for AF) and 2.04 (95% CI 1.62–2.57 for chronic obstructive pulmonary disease) (log-rank P < 0.001), while HR at 12 months was 1.15 (95% CI 0.94–1.41 for AF) and 1.87 (95% 1.52–3.20 for chronic obstructive pulmonary disease) (P < 0.002). LVEF-based categorization did not show such separation (6 months [P = 0.69] and 12 months [P = 0.30]). This evidence may suggest that UL cluster analysis (a form of ML) may be a better prognostic tool than LVEF in outcome prediction. Another study36 showed that ML though ML and cluster analysis was able to generate various echocardiographic phenotypes in asymptomatic community-based cohorts (n = 827), which were divided into 3 groups including mostly normal (MN), diastolic changes (D), and diastolic changes with structural remodeling (D/S). These results were externally validated, and they were associated with an adjusted HR of 1.87; (95% CI: 1.04 to 3.37) in the D phenotype, and an adjusted HR of 3.02 (95% CI: 1.71 to 5.34) in the D/S phenotype for both cardiovascular mortality and heart failure hospitalization. These RCT are examples of potential applications of ML in heart failure and heart imaging, but many others are available in other fields including electrophysiology,37 interventional38,39 and preventive cardiology.40,41 That is one way to look at ML in cardiology. Another way to look at various aspects wherein ML could be applied in cardiovascular care, including improving diagnosis,31,42 risk prediction,43,44 disease monitoring,45 access to care,46 point-of-care testing,47 and decision support tools.48–50
The advancement we are witnessing in the medical field is also associated with a proportional increase in complexity. This not only makes it more challenging to reach a decision but also becomes a time- and money-consuming process if these algorithms are operated by humans, with a possible chance of missing important information altogether. Besides, with the increase in patient number that is being dealt with on daily basis, error rates can rise when using these algorithms, rendering patient care in jeopardy. These issues are most prominent in LMICs, where cardiovascular health is deteriorating. In the current era of smart machines,51 it is crucial to consider employing these tools in discovering a more precise and quicker way to analyze the vast data in various medical fields, especially in cardiology.
Discussion
We presented data on the role of AI/ML in CVD, but the essential question that arises is whether AI has already been deployed to improve the health-care sector in LMICs or will be soon. To have an idea about the current use of AI-cardiology in LMICs, we searched PubMed using the following search string: ((cardiology) AND (artificial intelligence) AND (countries)) AND ((low) OR (middle) OR (high) OR (poor) OR (developing)) on the March 15th, 2021. A total of 21 studies were found, most of which were related to AI-cardiology. However, only two articles focused on the issue of AI-cardiology use in resource-limited countries/LMICs. The first study was done in a tertiary care center in the UK and did not examine AI’s outcomes on LMICs.52 The second study was a review that focused on AI’s potential benefits and advice for resource-limited countries.53 A bibliometric analysis published in 2021 on AI/ML-cardiology found out that research output on PubMed in this field is mainly achieved by developed countries, with the US, United Kingdom, and China ranking as the top three countries, respectively.54 The insufficient number of articles arising from LMICs shows the gap between AI advancement and its applications in the countries that need it the most. This is not unexpected. The relatively new development of AI-cardiology, the underdeveloped research structure in LMICs, and their poor economies, altogether may account for the delay in AI-cardiology application in these countries. Of note, this search string is not inclusive since some studies might describe an application of AI without using its terms explicitly.
AI/ML may come into play in such scenarios where it can help potentially improve work productivity,55 by occupying vacancies, as an independent, functional entity. A recently published prospective study assessed cardiovascular events in patients (n = 154,169) from different countries (low, middle, and high-income) and their association with socioeconomic status (education and wealth) over a follow-up mean of 7.5 years. They found out that major cardiovascular events (deaths, strokes, infarction, and heart failure) and all-cause mortality are inversely proportional to the level of education, and this association was much more apparent in low-income countries among the three. Contrary to that, there was no clear association between individual wealth and these two outcomes between the three groups.26 This might indicate that households with good financial status who are living in low-income countries are, nevertheless, impacted in a similar way to poor families, perhaps due to lack of good and reliable medical care, even if they are willing to spend on it. It is unlikely that implementing AI in healthcare in the LMICs will directly improve any outcomes based on economic benefits. It can help improve clinical efficacy, safety, effectiveness, and productivity in healthcare.
CVD, as a group, is of special importance, particularly in LMICs since it puts these countries in a vicious cycle. These countries face a substantial financial and disease burden of CVD,56 and each of these two further exacerbates the other infinitely (Figure 3). AI can play a very effective and efficient role in CVD management in LMICs. By reducing the healthcare expenditure on CVD, it might be possible to achieve better medical and financial outcomes (eg, budget allocation, redistribution/acquisition of human resources).
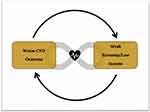 |
Figure 3 The “Positive Feedback Effect” of CVD in LMICs. Abbreviation: CVD, Cardiovascular Disease. |
The applications of AI-cardiology in LMICs can take many forms and shapes. In LMICs, detecting myocardial infarction using the standard criteria and prompt activation of the closest health-care center for possible intervention might be a valuable evolution to these countries. Having an AI tool that can detect AF in “normal” ECGs is interesting, but to the people in LMICs, early myocardial infarction detection and arranging for a possible intervention is, likely, far more valuable. Detection or diagnosis is an essential step in managing any disease, but not the only one that AI can potentially improve. Care continuum refers to health-care delivery that spans all phases of an illness, including recognition, diagnosis, prioritization, referral, transportation, treatment, and follow-up.57–59 In AI-Cardiology, it is essential to consider each one of these steps in the care continuum of any single disease to improve outcomes.
Another example in LMICs is the use of echocardiography, which technicians can operate. The data obtained from each echocardiogram for each patient can be overwhelming. But if the basic findings of each echocardiogram are employed in a way that alerts the responsible physician when an abnormality is detected, this can solve a part of the problem (ie, low ejection fraction is automatically reported to the assigned cardiologist). Many other examples can be thought of in LMIC-cardiology, which revolve around two main factors that are probably deficient in LMICs: adequate human power and resources. Another issue is that although many AI-cardiology tools have been proven to be efficacious, the effectiveness is yet to be established, especially in LMICs where many unforeseen factors might influence the functionality and applicability of these tools.
A promising example from the literature shows that AI could potentially be used in resource-limited countries. In a study that was done in Bangalore, India, mobile health (mHealth) clinics were compared to the standard-care clinics in patients with rheumatic and structural heart diseases. This study aimed to see which of these two clinics have shorter time-to-intervention and better clinical outcomes. mHealth clinics gathered data from pocket echocardiography, smartphones, 6-minute walk test, and BNP point-of-care testing. On the other hand, the standard-care clinics collected data from 12-lead ECG, imaging, and lab tests. Patients in both groups underwent transthoracic echocardiography. The mHealth group was found to have shorter time until intervention and better outcomes.60 This randomized clinical trial highlights the important role that AI-cardiology could play when applied in resource-limited countries (ie, LMICs), but it is important to note that this was not a decision support system. Another paper highlighted the promising applications of AI-cardiology which were driven from electro-cardiographical-based studies. In this review, it was shown that AI-cardiology can be employed for diagnostic, prognostic, and therapeutic purposes, in addition to disease monitoring and risk stratification in a multitude group of CVDs including AF, heart failure, hyperkalemia, and hypertrophic cardiomyopathy.61 Of note, all of these applications were derived from ECG mainly, which may suggest that other fields of cardiology are fertile fields for AI. Although most of these applications are still being studied and will likely take time until they become ready for clinical use, they carry huge potentials if applied in LMICs. Moreover, while AI/ML development in high-income countries is mainly focused on improving diagnostic time and accuracy, it is crucial to employ this tool to target each step of the care continuum of CVDs diagnosis and treatment, including improving patient triage (ie, avoid unnecessary ER visits, while decrease time for true emergent cases), finding cheaper diagnostic tests, augmenting human power by establishing independent AI units that can be operated with minimal human input, and avoiding unnecessary care by creating AI prognostic tools. These interventions would be designed to streamline care rather than generate additional “new” patients to treat and would be valuable in LMICs.
AI-Cardiology in LMICs: Implementation and Ethical Consideration
Nowadays, many AI-cardiology softwares have been approved by the US-FDA. One of the main issues with echocardiography is that it is operator-dependent; thus, clinical decisions that are based on certain echocardiograms can be biased due to many limitations including a problem in image acquisition. Image acquisition of diagnostic quality requires special training, which is deficient in LMICs. One of the possible solutions is the recently and first US-FDA approved cardiac ultrasound software, Caption Guidance. Caption Guidance guides the users to capture echocardiograms in a quality that is comparable to trained echocardiographers.62 A recently published study assessed Caption Guidance on 240 patients by allowing 8 nurses with no prior training in echocardiography to acquire echocardiograms to assess different cardiac parameters. 90% of the cases the nurses were able to acquire images that were of diagnostic quality. No significant differences were detected when these images were compared to other images taken by expert sonographers.63 The US-FDA has also approved the AI-ECG Platform for clinical use.64 It is a fully automated, accurate (98.3%), rapid (3s), and economical tool that can help in ECG interpretation through AI neural networks.65 Other examples of US-FDA AI tools in the field of cardiology include Arterys Cardio DL, EchoGo Core, AliveCor, BioFlux, eMurmer ID, and many more.66 This highlights that AI is not only a promising idea that is being studied but also a reality with many approved options for clinical use. These tools, if appropriately implemented, could dramatically improve the health-care systems in LMICs, especially in remote areas where subspecialized cardiologists are few in numbers. The turn now is on policymaker in the LMICs to carefully study and assess the situation to start with AI/ML implementation in their health-care systems to be ready for clinical use.
Figure 4 depicts a suggested algorithm for the application of AI/ML in LMICs. High-risk cardiac patients in resource-limited areas can be monitored using wearable devices that work based on the Internet-of-Things, which include simple accessories (eg, a watch or a wristband). These devices are connected to a central AI unit, streaming data continuously about the status of the patients from different parameters. These units would analyze the signal using the embedded algorithms and send signals if an abnormal rhythm is detected. True abnormal rhythms are subsequently sent to a cardiologist who can decide whether urgent action is needed. These units will be working in parallel with healthcare and call centers, which will also supply AI units with data, and aid in contacting patients and delivering care. Quer et al have recently published an excellent review on ML in cardiology to help simplify ML concepts and to offer a roadmap for cardiologists on how to evaluate and use newly available AI/ML products in clinical practice.54 However, this could represent another potential challenge towards the application of AI/ML in LMICs due to many factors. This includes issues with access of the general population to such devices (ie, smart phones/watches), access and cost of high-speed internet, presence of infrastructure on governmental level to support such system, training challenges, and many others. Taking these points into consideration would help in choosing which aspects of AI/ML could be used in which population, and when can they be used. Current literature highlights the underdeveloped health informatics systemic in the majority of LMICs.67,68
 |
Figure 4 The use of IoT and AI in CVD (eg, arrhythmia) management. Abbreviations: AI, Artificial intelligence; IoT, Internet of things; F/U, Follow-up. |
Another vital issue that should be considered when discussing AI is the ethical aspect of it, which is affected by several factors, including the storage and use of patients’ information, “black box” dilemma, health inequalities, errors, and legal responsibilities, among others.69 The ethical consideration is of great importance since each one of these factors can be amplified when dealing with a huge number of patients (which is expected in the growing cardiac population of LMICs70). The application of AI-cardiology in LMICs will need efforts related to the policies, logistics, technicalities, and financial support (Table 1). However, this is not to say that it is impossible to apply AI-cardiology but to identify the possible problems that might arise during the process of ML implementation.
 |
Table 1 Future Directions to Help AI/ML Implementation in LMIC |
Abbreviations
AF, Atrial fibrillation; AI, Artificial Intelligence; AUC, Area under the curve; CVD, Cardiovascular disease; HR, Hazard ratios; LMICs, Low- and middle-income countries; LVEF, Left ventricular ejection fraction; ML, Machine learning; NSR, Normal sinus rhythm; RCT, Randomized clinical trials; ROC, Receiver operating characteristic; SL, Supervised learning; SLUL, Unsupervised learning; ULUS, United States; USUS-FDA, US Food and Drug Administration.
Acknowledgments
We would like to thank Dr. Mohamad Adnan Alkhouli (Mayo Clinic, Cardiovascular Medicine) for his efforts in reviewing the manuscript and for his valuable feedback.
Funding
There is no funding to report.
Disclosure
SKH has received honoraria from Novartis, Mallinckrodt, Pfizer, and Janssen. SKH has received travel grants from MSD, Gilead, Sanofi, and Amgen. PAN reports Licensed IP (potential Royalty) from Anumana, during the conduct of the study; In addition, Dr Peter Noseworthy has a patent Various AI-ECG algorithms pending to Anumana. The authors report no other conflicts of interest in this work.
References
1. Bohr A, Memarzadeh K. The rise of artificial intelligence in healthcare applications. In: Artificial Intelligence in Healthcare. Academic Press; 2020:25–60.
2. Peters DH, Garg A, Bloom G, Walker DG, Brieger WR, Hafizur Rahman M. Poverty and access to health care in developing countries. Ann N Y Acad Sci. 2008;1136(1):161–171. doi:10.1196/annals.1425.011
3. Hasan BS, Rasheed MA, Wahid A, Kumar RK, Zuhlke L. Generating evidence from contextual clinical research in low- to middle income countries: a roadmap based on theory of change. Front Pediatr. 2021;9:764239. doi:10.3389/fped.2021.764239
4. Anand S, Bradshaw C, Prabhakaran D. Prevention and management of CVD in LMICs: why do ethnicity, culture, and context matter? BMC Med. 2020;18(1):7. doi:10.1186/s12916-019-1480-9
5. Reichert HA, Rath TE. Cardiac surgery in developing countries. J Extra Corpor Technol. 2017;49(2):98.
6. Saxena A. Status of pediatric cardiac care in developing countries. Children. 2019;6(2):34. doi:10.3390/children6020034
7. Dictionary.apa.org. n.d. APA dictionary of psychology. Available from: https://dictionary.apa.org/learning.
8. Mathur P, Srivastava S, Xu X, Mehta JL. Artificial Intelligence, Machine Learning, and Cardiovascular Disease. Clin Med Insights Cardiol. 2020;14:1179546820927404. doi:10.1177/1179546820927404
9. Hoodbhoy Z, Jiwani U, Sattar S, Salam R, Hasan B, Das JK. Diagnostic accuracy of machine learning models to identify congenital heart disease: a meta-analysis. Front Artificial Intelligence. 2021;8(4):97.
10. Amisha PM, Pathania M, Rathaur VK. Overview of artificial intelligence in medicine. J Family Med Primary Care. 2019;8(7):2328. doi:10.4103/jfmpc.jfmpc_440_19
11. Behzadi-khormouji H, Rostami H, Salehi S, et al. Deep learning, reusable and problem-based architectures for detection of consolidation on chest X-ray images. Comput Methods Programs Biomed. 2020;185:105162. doi:10.1016/j.cmpb.2019.105162
12. Yuan Q, Zhang H, Deng T, et al. Role of Artificial Intelligence in Kidney Disease. Int J Med Sci. 2020;17(7):970. doi:10.7150/ijms.42078
13. Patel UK, Anwar A, Saleem S, et al. Artificial intelligence as an emerging technology in the current care of neurological disorders. J Neurol. 2019;26:1–20.
14. Gomolin A, Netchiporouk E, Gniadecki R, Litvinov IV, Liangpunsakul S. Artificial Intelligence Applications in Dermatology: where Do We Stand? Front Med. 2020;7:7. doi:10.3389/fmed.2020.00007
15. Gubbi S, Hamet P, Tremblay J, Koch CA, Hannah-Shmouni F. Artificial intelligence and machine learning in endocrinology and metabolism: the Dawn of a new era. Front Endocrinol (Lausanne). 2019;28(10):185. doi:10.3389/fendo.2019.00185
16. Jarvis T, Thornburg D, Rebecca AM, Teven CM. Artificial Intelligence in Plastic Surgery: current Applications, Future Directions, and Ethical Implications. Plastic Reconstructive Surgery Global Open. 2020;8(10):e3200. doi:10.1097/GOX.0000000000003200
17. Iftikhar P, Kuijpers MV, Khayyat A, Iftikhar A, De Sa MD. Artificial Intelligence: a New Paradigm in Obstetrics and Gynecology Research and Clinical Practice. Cureus. 2020;12(2):548.
18. Dananjayan S, Raj GM. Artificial Intelligence during a pandemic: the COVID‐19 example. Int J Health Plann Manage. 2020;1:20.
19. Wynants L, Van Calster B, Collins GS, et al. Prediction models for diagnosis and prognosis of covid-19: systematic review and critical appraisal. BMJ. 2020;7:369.
20. Benjamens S, Dhunnoo P, Meskó B. The state of artificial intelligence-based FDA-approved medical devices and algorithms: an online database. NPJ Digital Med. 2020;3(1):1–8. doi:10.1038/s41746-020-00324-0
21. Fernholz T The World Bank is eliminating the term “developing country” from its data vocabulary [Internet]. Quartz; 2016. Available from: https://qz.com/685626/the-world-bank-is-eliminating-The-term-developing-country-from-its-data-vocabulary/.
22. Vasconcellos AG. Revisiting the Concept of Innovative Developing Countries (Idcs) for Its Relevance to Health Innovation and Neglected Tropical Diseases and for the Prevention and Control of Epidemics. PLoS Neglected Trop Dis. 2018;12(7):e0006469.
23. Owolabi M, Miranda JJ, Yaria J, Ovbiagele B. Controlling cardiovascular diseases in low and middle income countries by placing proof in pragmatism. BMJ Global Health. 2016;1(3):e000105. doi:10.1136/bmjgh-2016-000105
24. Bovet P, Paccaud F. Cardiovascular disease and the changing face of global public health: a focus on low and middle income countries. Public Health Rev. 2011;33(2):397–415. doi:10.1007/BF03391643
25. Bloomfield GS, Peña MS. Five Reasons Why Global Health Matters to Cardiologists. Cardiol Clin. 2017;35(1):xiii–v. doi:10.1016/j.ccl.2016.10.001
26. Rosengren A, Smyth A, Rangarajan S, et al. Socioeconomic status and risk of cardiovascular disease in 20 low-income, middle-income, and high-income countries: the Prospective Urban Rural Epidemiologic (PURE) study. Lancet Global Health. 2019;7(6):e748–60. doi:10.1016/S2214-109X(19)30045-2
27. World Health Statistics 2020 visual summary [Internet]. Who.int. Available from: https://www.who.int/data/gho/whs-2020-visual-summary.
28. Cooper RA. States With More Physicians Have Better-Quality Health Care: at the state level, increased numbers of both family physicians and specialists per capita are associated with higher quality of health care. Health Aff. 2008;27(Suppl1):w91–102. doi:10.1377/hlthaff.28.1.w91
29. Chow CK, Nguyen TN, Marschner S, et al. Availability and affordability of medicines and cardiovascular outcomes in 21 high-income, middle-income and low-income countries. BMJ Global Health. 2020;5(11):e002640. doi:10.1136/bmjgh-2020-002640
30. Celermajer DS, Chow CK, Marijon E, Anstey NM, Woo KS. Cardiovascular disease in the developing world: prevalences, patterns, and the potential of early disease detection. J Am Coll Cardiol. 2012;60(14):1207–1216. doi:10.1016/j.jacc.2012.03.074
31. Attia ZI, Noseworthy PA, Lopez-Jimenez F, et al. An artificial intelligence-enabled ECG algorithm for the identification of patients with atrial fibrillation during sinus rhythm: a retrospective analysis of outcome prediction. Lancet. 2019;394(10201):861–867. doi:10.1016/S0140-6736(19)31721-0
32. Bhalla V, Isakson S, Bhalla MA, et al. Diagnostic ability of B-type natriuretic peptide and impedance cardiography: testing to identify left ventricular dysfunction in hypertensive patients. Am J Hypertens. 2005;18(S2):73S–81S. doi:10.1016/j.amjhyper.2004.11.044
33. Wu JT, Wang SL, Chu YJ, et al. CHADS2 and CHA2DS2-VASc scores predict the risk of ischemic stroke outcome in patients with interatrial block without atrial fibrillation. J Atheroscler Thromb. 2016;1:34900.
34. Increase Productivity | control Health Care Costs | model | workplace Health Promotion | CDC [Internet]. Available from: https://www.cdc.gov/workplacehealthpromotion/model/control-costs/benefits/productivity.html.
35. Gevaert AB, Tibebu S, Mamas MA, et al. Clinical phenogroups are more effective than left ventricular ejection fraction categories in stratifying heart failure outcomes. ESC Heart Failure. 2021;8(4):2741–2754. doi:10.1002/ehf2.13344
36. Kobayashi M, Huttin O, Magnusson M, et al. Machine learning-derived echocardiographic phenotypes predict heart failure incidence in asymptomatic individuals. Cardiovascular Imaging. 2022;15(2):193–208.
37. Kim M, Kang Y, You SC, et al. Artificial intelligence predicts clinically relevant atrial high-rate episodes in patients with cardiac implantable electronic devices. Sci Rep. 2022;12(1):10. doi:10.1038/s41598-021-04021-0
38. Sampedro-Gómez J, Dorado-Díaz PI, Vicente-Palacios V, et al. Machine learning to predict stent restenosis based on daily demographic, clinical, and angiographic characteristics. Canadian J Cardiol. 2020;36(10):1624–1632. doi:10.1016/j.cjca.2020.01.027
39. Min HS, Ryu D, Kang SJ, et al. Prediction of coronary stent underexpansion by pre-procedural intravascular ultrasound–based deep learning. Cardiovascular Interventions. 2021;14(9):1021–1029. doi:10.1016/j.jcin.2021.01.033
40. Cho H, Kang SJ, Min HS, et al. Intravascular ultrasound-based deep learning for plaque characterization in coronary artery disease. Atherosclerosis. 2021;1(324):69–75. doi:10.1016/j.atherosclerosis.2021.03.037
41. Eisenberg E, McElhinney PA, Commandeur F, et al. Deep learning–based quantification of epicardial adipose tissue volume and attenuation predicts major adverse cardiovascular events in asymptomatic subjects. Circ Cardiovasc Imaging. 2020;13(2):e009829. doi:10.1161/CIRCIMAGING.119.009829
42. Fernández-Ruiz I. Artificial intelligence to improve the diagnosis of cardiovascular diseases. Nat Rev Cardiol. 2019;16(3):133. doi:10.1038/s41569-019-0158-5
43. Miller RJ, Huang C, Liang JX, Slomka PJ. Artificial intelligence for disease diagnosis and risk prediction in nuclear cardiology. J Nuclear Cardiol. 2022;4:1–9.
44. Christopoulos G, Graff-Radford J, Lopez CL, et al. Artificial intelligence–electrocardiography to predict incident atrial fibrillation: a population-based study. Circ Arrhythm Electrophysiol. 2020;13(12):e009355. doi:10.1161/CIRCEP.120.009355
45. Siontis KC, Friedman PA. The Role of Artificial Intelligence in Arrhythmia Monitoring. Card Electrophysiol Clin. 2021;13(3):543–554. doi:10.1016/j.ccep.2021.04.011
46. Tsay D, Patterson C. From machine learning to artificial intelligence applications in cardiac care: real-world examples in improving imaging and patient access. Circulation. 2018;138(22):2569–2575. doi:10.1161/CIRCULATIONAHA.118.031734
47. Vashistha R, Dangi AK, Kumar A, Chhabra D, Shukla P. Futuristic biosensors for cardiac health care: an artificial intelligence approach. Biotech. 2018;8(8):1. doi:10.1007/s13205-018-1368-y
48. Massalha S, Clarkin O, Thornhill R, Wells G, Chow BJ. Decision support tools, systems, and artificial intelligence in cardiac imaging. Canadian J Cardiol. 2018;34(7):827–838. doi:10.1016/j.cjca.2018.04.032
49. Schwalm JD, Di S, Sheth T, et al. A machine learning–based clinical decision support algorithm for reducing unnecessary coronary angiograms. Cardiovascular Digital Health j. 2022;3(1):21–30. doi:10.1016/j.cvdhj.2021.12.001
50. Sardar P, Abbott JD, Kundu A, Aronow HD, Granada JF, Giri J. Impact of artificial intelligence on interventional cardiology: from decision-making aid to advanced interventional procedure assistance. JACC Cardiovasc Interv. 2019;12(14):1293–1303. doi:10.1016/j.jcin.2019.04.048
51. Sim I. Mobile devices and health. N Eng J Med. 2019;381(10):956–968. doi:10.1056/NEJMra1806949
52. Holzer R, Ladusans E, Kitchiner D, Peart I, Gladman G, Miles G. Prioritization of congenital cardiac surgical patients using fuzzy reasoning-a solution to the problem of the waiting list? Cardiol Young. 2006;16(3):289. doi:10.1017/S1047951106000400
53. Thomford NE, Bope CD, Agamah FE, et al. Implementing artificial intelligence and digital health in resource-limited settings? Top 10 lessons we learned in congenital heart defects and cardiology. j Integrative Biol. 2020;24(5):264–277. doi:10.1089/omi.2019.0142
54. Quer G, Arnaout R, Henne M, Arnaout R. Machine Learning and the Future of Cardiovascular Care: JACC State-of-The-Art Review. J Am Coll Cardiol. 2021;77(3):300–313. doi:10.1016/j.jacc.2020.11.030
55. Kshetri N. Artificial Intelligence in Developing Countries. IEEE Ann Hist Comput. 2020;22(4):63–68.
56. Pena MS, Bloomfield GS. Cardiovascular disease research and the development agenda in low-and middle-income countries. Glob Heart. 2015;10(1):71. doi:10.1016/j.gheart.2014.12.006
57. Evashwick C. Creating the continuum of care. Health Matrix. 1989;7(1):30–39.
58. National Cancer Institute. NCI Dictionary of Cancer Terms; 2022. Available from: https://www.cancer.gov/publications/dictionaries/cancer-terms/def/continuum-of-care.
59. Nair SM, Zheleva B, Dobrzycka A, Hesslein P, Sadanandan R, Kumar RK. A Population Health Approach to Address the Burden of Congenital Heart Disease in Kerala, India. Glob Heart. 2021;16(1). doi:10.5334/gh.1034
60. Bhavnani SP, Sola S, Adams D, Venkateshvaran A, Dash PK, Sengupta PP. A randomized trial of pocket-echocardiography integrated mobile health device assessments in modern structural heart disease clinics. JACC Cardiovasc Imaging. 2018;11(4):546–557. doi:10.1016/j.jcmg.2017.06.019
61. Siontis KC, Noseworthy PA, Attia ZI, Friedman PA. Artificial intelligence-enhanced electrocardiography in cardiovascular disease management. Nat Rev Cardiol. 2021;1:1–4.
62. FDA Authorizes Marketing of First Cardiac Ultrasound Software That Uses Artificial Intelligence to Guide User [Internet]. U.S. Food and Drug Administration. 2020 Available from: https://www.fda.gov/news-events/press-announcements/fda-authorizes-marketing-first-cardiac-ultrasound-software-uses-artificial-intelligence-guide-user.
63. Narang A, Bae R, Hong H, et al. Utility of a Deep-Learning Algorithm to Guide Novices to Acquire Echocardiograms for Limited Diagnostic Use. JAMA cardiol. 2021;6(6):624. doi:10.1001/jamacardio.2021.0185
64. November 2018 510(k) Clearances [Internet]. U.S. Food and Drug Administration; 2018 Available from: https://www.fda.gov/medical-devices/510k-clearances/november-2018-510k-clearances.
65. AI ECG-products-carewell [Internet]. Available from: https://www.carewellhealth.com/products_aiecg.html.
66. The Medical Futurist [Internet]. The Medical Futurist Available from: https://medicalfuturist.com/fda-approved-ai-based-algorithms/.
67. Lewis T, Synowiec C, Lagomarsino G, Schweitzer J. E-health in low-and middle-income countries: findings from the Center for Health Market Innovations. Bull World Health Organ. 2012;90:332–340. doi:10.2471/BLT.11.099820
68. Babigumira JB, Jenny AM, Bartlein R, Stergachis A, Garrison LP. Health technology assessment in low-and middle-income countries: a landscape assessment. J Pharmaceutical Health Services Res. 2016;7(1):37–42. doi:10.1111/jphs.12120
69. Fenech ME, Buston O. AI in cardiac imaging: a UK-based perspective on addressing the ethical, social, and political challenges. Front Cardiovascular Med. 2020;15(7):54. doi:10.3389/fcvm.2020.00054
70. Gaziano TA, Bitton A, Anand S, Abrahams-Gessel S, Murphy A. Growing epidemic of coronary heart disease in low-and middle-income countries. Curr Probl Cardiol. 2010;35(2):72–115. doi:10.1016/j.cpcardiol.2009.10.002
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

