Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 16
Investigation of the Correlation Between the Polymorphism/Expression Level of RANTES and Its Receptor CCR5 Gene Promoter and Type 2 Diabetes Mellitus
Authors Chen J , Guo W, Yin H, Ma L, Li S , Li H
Received 18 November 2022
Accepted for publication 31 December 2022
Published 24 January 2023 Volume 2023:16 Pages 213—223
DOI https://doi.org/10.2147/DMSO.S398264
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Juei-Tang Cheng
Jie Chen,1,* Weichang Guo,2,* Hejia Yin,1 Liju Ma,3 Shaoyou Li,4 Huifang Li1
1Department of Diabetes, The First Affiliated Hospital of Kunming Medical University, Kunming, 650032, People’s Republic of China; 2Department of Physical Education, Kunming Medical University, Kunming, 650032, People’s Republic of China; 3Department of Clinical Laboratory, The First Affiliated Hospital of Kunming Medical University, Kunming, 650032, People’s Republic of China; 4Department of The Scientific Research Laboratory Center, The First Affiliated Hospital of Kunming Medical University, Kunming, 650032, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Huifang Li, Department of Diabetes, The First Affiliated Hospital of Kunming Medical University, No. 295 Xichang Road, Wuhua District, Kunming, 650032, People’s Republic of China, Email [email protected]
Background: This study aimed to explore relationship among RANTES − 28 (rs2280788) C/G polymorphism or CCR5 59029 (rs1799987) A/G polymorphism, level of self-expression, and type 2 diabetes mellitus (T2DM).
Materials and Methods: Clinical data were collected from 92 subjects with normal blood glucose (NC) and 97 patients with T2DM (DM). CCR5 levels on the surface of monocyte/lymphocyte and plasma RANTES levels were detected by flow cytometry. TaqMan real-time fluorescent quantitative PCR was used to detect genetic polymorphisms of RANTES rs2280788 and CCR5 rs1799987.
Results: There were no significant differences in frequencies of CCR5 rs1799987 genotype and A/G allele and frequencies of RANTES rs2280788 genotype and C/G allele, between subjects in NC and DM group (P > 0.05). Plasma RANTES level in DM group was significantly lower than NC group (P < 0.05), and difference came from patients with T2DM using insulin and subjects with normal blood glucose. CCR5 levels on the surface of monocytes and lymphocytes of patients in DM group were higher than NC group (P < 0.05). There was no significant difference in CCR5 level on the surface of monocytes and lymphocytes (or plasma RANTES level) among different genotypes of CCR5 rs1799987 (or RANTES rs2280788) (P > 0.05). RANTES level was positively correlated with age and TC and negatively correlated with diabetes course and HbA1c. CCR5 level on the surface of monocytes was positively correlated with drinking years, HbA1c, course of diabetes, and negatively correlated with TC. CCR5 on lymphocyte surface was positively correlated with diabetes course, smoking years, HbA1c, and negatively correlated with LDL, TC, HDL (P < 0.05).
Conclusion: RANTES -28 (rs2280788) C/G polymorphism or CCR5 59029 (rs1799987) A/G polymorphism may not be associated with T2DM of Han nationality in Kunming and cannot affect RANTES and CCR5 expression. RANTES and CCR5 levels may be related to T2DM but may also be affected by age, blood lipids, HbA1c, diabetes course, drugs, and other factors.
Keywords: type 2 diabetes, inflammation, cytokines, gene polymorphism, RANTES, CCR5
Introduction
Diabetes (DM) is one of the five diseases with the highest prevalence and mortality in the world.1 In 2019, more than 4 million adults died of diabetes and its complications, resulting in direct economic expenditure of $760 billion US.2,3 Among all types of diabetes, type 2 diabetes (T2DM) accounts for about 90%.4 More and more studies have shown that T2DM is a chronic low-grade inflammatory disease. Insulin resistance and secretion function in patients with T2DM are closely related to the synthesis and secretion of a variety of cytokines by monocyte macrophages, lymphocytes, adipocytes, and other cells after activation of the immune system.5,6 At the same time, this continuous metabolic inflammation will promote the accumulation of leukocytes in damaged tissues and the continuous production of pro-inflammatory mediators. Amplifying the inflammatory response through the positive feedback loop is an important factor in promoting the occurrence and development of diabetes microvascular complications (DMI), such as diabetes nephropathy (DN) and diabetes retinopathy (DR).6,7 Therefore, finding the key cytokines in the inflammatory mechanism of T2DM is of great significance for its prevention and treatment.
Regular activation of normal T cells expressed and secreted (RANTES), also known as C-C chemokine ligand 5 (CCL5), is expressed primarily in activated CD8+ T lymphocytes, fibroblasts, mesangial cells, macrophages and other cells, and is a specific chemokine of monocyte macrophages.8 The receptor of RANTES, the C-C chemokine receptor type 5 (CCR5), is expressed mainly on the surface of NK cells, T lymphocytes, phagocytes, and other immune effector cells. RANTES and CCR5 can play a variety of biological effects after a specific combination, such as chemotaxis and activation of a variety of leukocytes, enhancement of intercellular adhesion, promotion of the release of other cytokines and proliferation of T lymphocytes.9,10 Some studies have shown that RANTES and its CCR5 receptor are associated with insulin resistance and impaired glucose tolerance, but their correlation with diabetes and their correlation mechanism are still controversial.10,11 In view of the influence of ethnic differences of the participants on the research results,12 we conducted a study in Kunming, Yunnan Province, to explore the correlation among the C/G polymorphism of the RANTES gene promoter region-28 (rs2280788) or the A/G polymorphism of the CCR5 gene promoter region 59029 (rs1799987), its own expression level, and the T2DM in the Han population in this region.
Materials and Methods
Subjects
This study included 189 Han people who were treated in the First Affiliated Hospital of Kunming Medical University and divided into the Diabetes mellitus (DM) group (n = 97) and the Normal blood glucose (NC) group (n = 92). Patients in the DM group (57 males and 40 females) aged 49.53 ± 12.52 years and were diagnosed with T2DM, according to the WHO diagnostic criteria in 1999. The exclusion criteria were listed as follows: infection, coronary heart disease, acute complications of diabetes, rheumatoid diseases, and other diseases related to autoimmunity. The subjects in the NC group (43 men and 49 women) were all normal blood glucose after physical examination at the physical examination center of our hospital. These subjects aged 46.22 ± 11.77 years, with fasting plasma glucose (FPG) <6.1 mmol/l, and without a history of diabetes. Furthermore, the patients in the DM group were also divided into the long-term DM group (LDM) and the short-term DM group (SDM) according to the course of diabetes. The LDM group was patients with diabetes with a course of >5 years, and the SDM group was patients with diabetes with a course of diabetes ≤5 years. Both groups of patients were diabetes patients who met the WHO diagnostic criteria in 1999.
This study was approved by the Ethics Committee of the First Affiliated Hospital of Kunming Medical University (Approval No. 2020-L-18, Approval Date: April 10th, 2020). Subjects involved in this study provided their informed consents. This study was carried out in accordance with the Helsinki Declaration of 1975, as revised in 2013 (http://www.wma.net/en/20activities/10ethics/10helsinki/).
Insulin Treatment and Parameter Collection
Insulin Treatment
According to the characteristics of the patient’s condition, the patient’s willingness, the patient’s self-management ability, the accessibility of the patient’s insulin types and the patient’s economic conditions, this study developed different individualized insulin treatment plans.
Waist Circumference (WC) Measurement
Subjects stood naturally, and the measuring staff used an inelastic tape to pass the most prominent part of the subjects’ buttocks around the buttocks, close to but not compressing the skin, and read the readings (accurate to 0.1 cm). Smoking: According to the WHO judgment standard, those who have smoked in the past 30 days and have smoked more than 100 cigarettes so far were considered smokers. Those who met this standard would be judged as smokers, and those who did not meet this standard would be judged as nonsmokers. Drinking: Those who have a history of drinking white wine (Baijiu), beer or rice wine for more than 12 days in the past year were judged as drinkers, and those who did not meet this standard were judged as nondrinkers.
Determination of the −28 C/G Polymorphism and the 59029 A/G Polymorphism
The peripheral venous blood DNA of the subjects was extracted using a Small Amount of Whole Blood Genomic DNA Rapid Extraction Kit (Cat. No. DL110-01, Biomed. Tech. Co., Ltd., Beijing, China.), as instructed by the manufacturer. The polymorphism of the RANTES gene promoter region −28 (rs2280788) C/G and the polymorphism of the CCR5 gene promoter region 59029 (rs1799987) A/G, using the TaqMan real-time fluorescence quantitative PCR system. Genotypes were analyzed according to the fusion curve of the PCR products. The PCR reaction conditions are listed in Table 1. The interpretation of the product fusion curve is shown in Figure 1. The specific fragment primers and probes of the RANTES gene rs2280788 were synthesized by Beijing Qingke Xinye Biotechnology Co., Ltd. (Table 2) and ABI (Foster City, CA, USA) synthesized specific fragment primers and probes of the CCR5 gene rs1799987. The PCR reaction system used in this mainly included the following parameters: 1 μL DNA template, 10 μL 2×T5 fast qPCR mix (probe), 1 μL TaqMan probe and primers upstream and downstream, 0.4 μL 50×ROX Reference Dye I, 7.6 μL ddH2O.
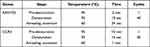 |
Table 1 The Condition of the PCR Assay |
 |
Table 2 Primer Sequence of the Promoter Region of the RANTES Gene −28 (rs2280788) |
Evaluation of Plasma RANTES Concentration and CCR5 Expression on the Leukocyte Surface
The concentration of RANTES in plasma was detected with flow cytometry methods, by the CBA Human Cytokine Detection Kit (Cat. No. 550749, BD Biosciences, San Jose, CA, USA) as described in the manufacturer’s protocol. The level of CCR5 on the surface of lymphocytes and monocytes was detected by flow cytometry. The antibodies, including FITC-conjugated mouse anti-human CD14 (Cat. No. 555397), PE-conjugated mouse anti-human CD195 (Cat. No. 555993), and PE-conjugated mouse IgG (Cat. No. 555787), were purchased from BD Biosciences (San Jose, CA, USA) (Figure 1).
Detection of Clinical and Biochemical Indicators
The indicators, including FPG, total cholesterol (TC), triglycerides (TG), high-density lipoprotein cholesterol (HDL-C) and low-density lipoprotein cholesterol (LDL-C), were detected by an automatic biochemical analyzer. Glycosylated hemoglobin was determined by the HPLC method.
Statistical Analysis
Hardy-Weinberg equilibrium analysis was used to test the group representation of the selected samples. SPSS 26.0 statistical analysis software (IBM Corp., Armonk, NY, USA) was used for statistical analysis. The normal distribution data were expressed as mean ± standard deviation (SD) and analyzed with parametric tests. The nonnormal distribution data were expressed by median (lower quartile, upper quartile) or “rate” and analyzed with nonparametric tests. Two independent sample Student’s t-test was used to compare the normal distribution data between two groups, and two independent sample rank sum test was used to compare the nonnormal distribution data. Normal distribution data among the three groups were compared with the analysis of variance of a completely random design, and the LSD-t test was used for pairwise comparison. The Kruskal Wallis test was used for nonnormal distribution data, and the Chi-square (χ2) test was used to count data comparison. Pearson’s correlation analysis was used for correlation analysis of normal distribution data whose dependent variable was measurement data, and Spearman correlation analysis was used for the correlation analysis of nonnormal distribution data. The difference was statistically significant with P < 0.05. However, the alpha (α) division method was used to compare two groups among three groups. Therefore, P < 0.05 was divided into 3 parts (P < 0.005/3 = 0.017), as statistically significant.
Results
General Characteristics of Subjects in the Diabetes Mellitus (DM) and Normal Blood Glucose (NC) Group
The genotype distribution of the CCR5 rs1799987 gene polymorphism and the RANTES rs2280788 gene polymorphism of the patients in the DM group and the subjects in the NC group was consistent with the Hardy-Weinberg equilibrium law (P > 0.05). FPG level, glycosylated hemoglobin type A1C (HbA1c) level, waist circumference (WC), BMI, systolic blood pressure and TG level of patients in the DM group were significantly higher compared to those of subjects in the NC group (Table 3, P < 0.05). Meanwhile, the TC level and HDL level of the patients in the DM group were significantly lower compared to those of the subjects in the NC group (Table 3, P < 0.05). However, there were no significant statistical differences between the two groups in terms of age, sex, diastolic blood pressure and LDL (Table 3, P > 0.05).
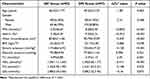 |
Table 3 General Characteristics of Patients in the Normal Control (NC) Group and the Diabetes Mellitus (DM) Group |
Comparison of the Genotype/Allele Frequencies of CCR5 rs1799987 and RANTES rs2280788 Between Subjects in the DM Group and NC Group
There were no significant differences in the frequency of the CCR5 rs1799987 genotype (AA, AG, GG) between the patients in the DM group and the subjects in the NC group (Table 4, P > 0.05). At the same time, there were no significant differences in the frequency of the RANTES rs2280788 genotype (CC+CG, GG) between patients in the DM group and subjects in the NC group (Table 4, P > 0.05). Additionally, there were no significant differences in the A/G allele frequency of CCR5 rs1799987 and the C/G allele frequency of RANTES rs2280788 between patients in the DM group and subjects in the NC group (Table 4, P > 0.05).
 |
Table 4 Genotype and Allele Frequencies of CCR5 rs1799987 and RANTES rs2280788 of Patients in the Normal Control (NC) Group and the Diabetes Mellitus (DM) Group |
Plasma RANTES Level and CCR5 Expression in Leukocyte Surface Comparison Among Subjects in the InsDM, NInsDM, and NC Group
The plasma RANTES level of patients in the DM group was significantly lower than that of subjects in the NC group (Table 5, P < 0.05). However, the expressions of CCR5 on the surface of monocytes and lymphocytes were significantly higher compared to those of subjects in the NC group (Table 5, P < 0.05).
 |
Table 5 Expression of RANTES and CCR5 in Patients in the Normal Control Group (NC) and the Diabetes Mellitus Group (DM) |
Cytokine levels among patients in the NC group (n = 92), diabetes patients with insulin administration (InsDM group, n = 52), and diabetes patients without insulin administration (NInsDM group, n = 45) are shown in Figure 2A–C. There were no significant differences in plasma RANTES level (Figure 2A) and mononuclear CCR5 ratio (Figure 2B) between patients in the NInsDM group and subjects in the NC group and between patients in the NInsDM group and patients in the InsDN group (both P > 0.017). However, the plasma level of RANTES (Figure2A) of the patients was significantly lower and the CCR5 mononuclear ratio (Figure 2B) of the patients was significantly higher in the InsDM group compared to those of the subjects in the NC group (both P < 0.017). The CCR5 lymphoid ratio of patients in the NInsDM group and the InsDM group was significantly higher compared to that of subjects in the NC group (Figure 2C, both P < 0.017), and the CCR5 lymphoid ratio of patients in the InsDM group was significantly higher than that of patients in the NInsDM group (Figure 2C, P < 0.017). Furthermore, there were no significant differences in gender and age between the above three groups (P > 0.05).
Plasma Expression of RANTES and CCR5 in Leukocyte Surface Comparison Between Subjects with Different Diabetes Course and NC Group
Cytokine levels among subjects in the NC group (n = 92), diabetes patients with a 5-year or shorter course (SDM group, n = 43) and diabetes patients with a course of more than 5 years (LDM group, n = 35) are shown in Figure 2D–F. Plasma RANTES level (Figure 2D) of patients in the LDM group and the SDM group were significantly lower compared to those of subjects in the NC group and CCR5 lymphoid ratio (Figure 2F) of patients in the LDM group and the SDM group were significantly higher compared to those of subjects in the NC group (both P < 0.017). The CCR5 mononuclear ratio (Figure 2E) of the patients in the LDM group was significantly higher than that of the subjects in the NC group and the patients in the SDM group (both P < 0.017). There was no significant difference in CCR5 mononuclear ratio (Figure 2E) between patients in the SDM group and subjects in the NC group (P > 0.017). There were no significant differences in plasma RANTES level (Figure 2D) and CCR5 lymphoid ratio (Figure 2F) between patients in the LDM group and patients in the SDM group (both P > 0.017). Furthermore, there were no significant differences in sex and age among the above three groups (P > 0.05).
Comparison of Self-Expression Levels Between Different Genotype Groups in CCR5 rs1799987 and RANTES rs2280788
There were no significant differences in the lymphoid ratio of CCR5 and the mononuclear ratio of CCR5 between different genotype groups (AA, AG, GG) in CCR5 rs1799987 (Table 6, P > 0.05). There were no significant differences in plasma RANTES levels between different genotype groups (CC+CG, GG) at RANTES rs2280788 (Table 6, P > 0.05).
 |
Table 6 Self-Expression Between Different Genotype Groups at the CCR5 rs1799987 Site and the RANTES rs2280788 Gene Site |
Correlation Between RANTES/CCR5 Expression Levels and Clinical/Biochemical Data
RANTES level was weakly positively correlated with age and total cholesterol (TC), and weakly negatively correlated with the course of diabetes and HbA1C (Table 7, all P < 0.05). The mononuclear CCR5 ratio demonstrated a weak positive correlation with drinking years, HbA1c, the course of diabetes, and a weak negative correlation with TC (Table 7, all P < 0.05). The CCR5 lymphoid ratio was moderately positively correlated with the course of diabetes, was weakly positively correlated with smoking years and HbA1c, and was weakly negatively correlated with LDL, TC, and HDL (p < 0.05).
 |
Table 7 Correlation Analysis of RANTES and CCR5 Expression Levels with Clinical and Biochemical Data |
Discussion
Our study showed that the plasma level of RANTES of Han-nationalized patients with T2DM in Kunming, China, is lower than that of normal blood glucose subjects, which is similar to the results of Mohamed et al.13 However, in a German study, there was no difference in serum RANTES levels between diabetes patients and normal health individuals.14 Some studies9,15,16 showed that serum RANTES levels in patients with impaired glucose tolerance and diabetes were significantly higher than in the control group. Through further analysis, we found that the difference in RANTES expression is mainly due to the comparison between patients with T2DM who use insulin and those with normal blood glucose. Therefore, we consider that the decrease in plasma RANTES level in the DM group may be related to inhibition of inflammation by insulin use.13,17 Furthermore, we also found that the level of RANTES was positively correlated with age, which is similar to the research conclusion of Jamali et al.9 Our study also showed that there was a negative correlation between RANTES level and HbA1c, contrary to the research conclusion of Pfleger et al.18 The reasons for this difference are not only related to the ethnic differences of the subjects and different hypoglycemic regimens but also related to the different stages of the disease course of the patients with diabetes. Another study [9] showed that the level of RANTES in patients with diabetes increased with the extension of the duration of diabetes. In this study, the results showed that the level of RANTES was negatively correlated with the course of diabetes, that is, the expression level of RANTES decreases with the extension of the course of diabetes, which is similar to the conclusion of Pfleger et al.18 However, we did not find a statistical difference in plasma RANTES levels between patients with diabetes in 5 years and those with more than 5 years, suggesting that the time point of significant reduction in RANTES levels in patients with T2DM of Han nationality in Kunming, China, is not around the fifth year after diagnosis. In the future, it is necessary to expand the sample size for more detailed course grouping research.
In this study, the level of CCR5 on the surface of monocytes and lymphocytes in patients with diabetes was significantly higher than those with normal blood glucose, which is similar to the results of Inayat et al11 and others, while Lohmann et al14 and others have not found such differences. The results showed that there was a positive correlation between the level of CCR5 on the surface of monocytes and lymphocytes and the course of diabetes. After more than five years of diabetes, the level of CCR5 on the surface of monocytes increased significantly. Furthermore, we also found that the difference in the level of CCR5 in monocytes between patients with diabetes and those with normal blood glucose mainly came from patients with diabetes who used insulin. The CCR5 level on the lymphocyte surface of diabetes patients who used insulin was significantly higher than that of diabetes patients who did not use insulin, which may be related to poor blood glucose control in this group. HbA1c in diabetes patients using insulin (InsDM group) was significantly higher than in the NInsDM group and the NC group, which may be related to oxidative stress and inflammatory factor production11,19 and the interaction between elevated CCR5 and RANTES in the body, islet inflammation mediated by cascade reaction, and the development of diabetes.18,20 The correlation analysis also showed that there was a positive correlation between the level of CCR5 on the surface of monocytes and lymphocytes and HbA1c, while the anti-inflammatory effect of insulin did not appear to significantly inhibit the expression of CCR5. Furthermore, we observed that there was a positive correlation between smoking years and drinking years and the level of CCR5, which is similar to the research conclusion of Jamali et al9 suggesting that tobacco use and alcohol intake can upregulate CCR5 expression, and we should pay attention to smoking cessation and alcohol restriction in the prevention and treatment of diabetes.
Lipid metabolism disorder and subsequent subclinical inflammation are one of the reasons for the appearance and development of insulin resistance.21 This study did not find that the TG level was related to the expression level of RANTES and CCR5, but the TC level was negatively correlated with the level of CCR5 on the surface of monocytes and lymphocytes and positively correlated with the level of RANTES. HDL dysfunction is related to insulin resistance.22 In this study, HDL level was negatively correlated with CCR5 level on the lymphocyte surface, showing the anti-inflammatory effect of HDL, which is similar to the research conclusion of Jonas et al.23 In T2DM, oxidized and/or enzymatically modified forms of low-density lipoprotein (oxLDL) can mediate the activation and maturation of T cells and monocytes/macrophages.24 Our study showed that the higher the LDL level, the lower the CCR5 level on the lymphocyte surface, suggesting that LDL may induce down-regulation of CCR5 expression, but does not rule out interference from other factors. Therefore, LDL, HDL, and TC may participate in the inflammatory response in patients with T2DM by affecting the expression of RANTES and its CCR5 receptor.
Furthermore, CCR5 on the lymphocyte surface was negatively correlated with TC level and LDL level, also suggesting that lipid metabolism can affect the expression level of CCR5, which is similar to Li et al′s report.25 This study showed that the expression of CCR5 mRNA in patients with hyperlipidemia was significantly increased compared to those without hyperlipidemia, while the expression of CCR5 mRNA was significantly decreased after simvastatin treatment. Hyde et al26 showed that CCR5Δ32 mutation is associated with an increase in plasma HDL and a decrease in plasma TG, which means that the level of CCR5 may be negatively correlated with HDL and positively correlated with TG. Slominski et al27 showed that CCR5Δ32 Mutants had higher levels of LDL, TG and lower levels of HDL, suggesting that the level of CCR5 may be negatively correlated with LDL, TG, and positively correlated with HDL. These studies also suggest that the expression level of CCR5 may affect the level of blood lipid and the interaction between them plays an important role in the occurrence and development of atherosclerosis in patients with diabetes.28
Research showed that insulin can play an anti-inflammatory role by inhibiting the expression of RANTES and other cytokines.13,17,29,30 At the same time, metformin can also inhibit NF-κB by activating adenosine monophosphate activated protein kinase (AMPK) plays an anti-inflammatory role.11 In this study, the plasma level of RANTES of patients with T2DM using insulin was significantly lower than that of those with normal blood glucose, which may be related to the insulin inhibition in expression of RANTES. There is no significant statistical difference between plasma RANTES levels of patients with T2DM who use insulin and those who do not use insulin, which may be related to plasma RANTES levels in addition to the effects of insulin treatment and may also be related to the effects of other factors, such as the use of metformin or different glucose metabolism states. The exact mechanism remains to be further studied by experiments with animal models.
In this study, the expression level of CCR5 on the surface of monocytes in patients with diabetes who used insulin was significantly higher than that of patients with normal blood glucose, and the level of CCR5 on the surface of lymphocytes was significantly higher than that of diabetes patients who did not use insulin and those with normal blood glucose, which seemed to contradict the anti-inflammatory effect of insulin. However, our study found that the expression level of CCR5 was affected by a variety of factors, and the HbA1c in patients with diabetes who used insulin was higher than that in patients with normal blood glucose. The TC level is lower than that of the diabetes patients without insulin and the normal blood glucose group. We consider that the difference in the expression of CCR5 among the three groups may also be related to the abnormality of glucose and lipid metabolism and the degree of abnormality. In the future, further exploration such as animal model experiments or cell culture is needed.
The influence of cytokines on disease susceptibility and severity is not only related to their expression level but also related to a single nucleotide polymorphism (SNP) in the regulatory region of their gene coding sequence.12,31 Zhernakova et al32 found that the RANTES rs2280788 G allele will lead to a slight up-regulation of its own expression level, but in this study, we did not find that the polymorphism of the RANTES rs2280788 gene in the Han population in Kunming affects the plasma RANTES level, which is similar to the research conclusion of Herder et al.33 Furthermore, there were no significant differences in genotype frequency and C/G allele frequency of RANTES rs2280788 between patients in the T2DM group and subjects in the NC group in Kunming Han population, suggesting that the polymorphism of the RANTES rs2280788 gene may not be related to the occurrence of T2DM. Studies in the German population27 also did not find that the polymorphism of the RANTES rs2280788 gene was related to the appearance of diabetes. Yadav et al34 showed that the frequency of the CCR5 59029 AA genotype in patients with T2DM was significantly higher than in healthy controls. The reason for increased susceptibility to diabetes in individuals with CCR5 59029 A/- genotype may be related to increased expression of CCR5 on the surface of peripheral blood monocytes and lymphocytes.35 In this study, it was not found that the polymorphism of the CCR5 rs1799987 gene had an impact on its own expression in the Han population in Kunming nor was there a statistical difference in genotype frequency and A/G allele frequency of CCR5 rs1799987 between patients in the DM group and subjects in the NC group, which is similar to the results of previous studies.31,33,36 The reasons for these differences may be related to genetic heterogeneity, the time loci for measuring cytokine levels, and the influence of the hypoglycemic drugs used by patients. Meanwhile, it may also be because the population is small, resulting in the relationship between gene polymorphism and abnormal glucose metabolism, and the level of self-expression is not apparent, which needs to be further studied by expanding the sample size.
Furthermore, in this study, the number of patients with the RANTES rs2280788 CC and CG genotype was 3 cases and 40 cases, respectively. In view of the small number of cases of the RANTES rs2280788 CC genotype (literature query or previous research by our research team also found that the number of carriers of the CC genotype was very small), it would not be statistically significant if we divided them into three groups for comparative analysis. Therefore, we combined RANTES rs2280788 CC with patients with the CG genotype for analysis in this study.
This study also had certain limitations. First, this is an observational cross-sectional study, which cannot determine whether a decrease in plasma RANTES level and an increase in CCR5 level on the surface of leukocytes are the cause or result of diabetes. Second, the causal relationship between lipid metabolism disorders and cytokine levels should be studied prospectively. Third, this is a single-center study, with a limited number of subjects included, which may lack sufficient statistical power to adjust confounders and make a more detailed grouping. Fourth, the primers and probes for rs1799987-specific fragment of CCR5 gene were synthesized by ABI company. However, due to the intellectual property problem, the ABI company did not provide CCR5 primer sequences.
In conclusion, there may be no association between the RANTES gene promoter region −28 (rs2280788) C/G polymorphism or the CCR5 gene promoter region 59029 (rs1799987) A/G polymorphism and the T2DM of Han nationality in Kunming, and it will not affect its own expression level. RANTES and CCR5 levels may be related to T2DM but will be affected by age, blood lipids, HbA1c, course of diabetes, drugs (insulin) and other factors (smoking years, drinking time, duration of hypertension).
Funding
This study was granted by the National Natural Science Fund of China (Grant No. 82160165, 81160104, and 30760087), the “famous doctor” special program of Yunnan Xingdian Talent support plan in 2022 (Grant NO. RLMY20220009), the Training plan for medical discipline leaders of Yunnan provincial health and family planning commission (Grant NO. D-2017039), the young and middle-aged academic and technical leaders reserve talented person project in Yunnan province (Grant NO. 202105AC160093), the science and technology innovation team foundation of Kunming Medical University (Grant NO.CXTD202101) and the subproject of clinical medical research center for metabolic diseases of Yunnan province (Grant No.202102AA100056).
Disclosure
The authors report no conflicts of interest regarding the publication of this paper.
References
1. Esquivel Zuniga R, DeBoer MD. Prediabetes in adolescents: prevalence, management and diabetes prevention strategies. Diabetes Metab Syndr Obes. 2021;14:4609–4619. doi:10.2147/DMSO.S284401
2. Saeedi P, Salpea P, Karuranga S, et al. Mortality attributable to diabetes in 20-79 years old adults, 2019 estimates: results from the international diabetes federation diabetes atlas. Diabetes Res Clin Pract. 2020;162:108086. doi:10.1016/j.diabres.2020.108086
3. Williams R, Karuranga S, Malanda B, et al. Global and regional estimates and projections of diabetes-related health expenditure: results from the international diabetes federation diabetes atlas. Diabetes Res Clin Pract. 2020;162:108072. doi:10.1016/j.diabres.2020.108072
4. Keshavarzi F, Golsheh S. IRS1- rs10498210 G/A and CCR5-59029 A/G polymorphisms in patients with type 2 diabetes in Kurdistan. Mol Genet Genomic Med. 2019;7(5):e631. doi:10.1002/mgg3.631
5. Fernández-Real JM, Pickup JC. Innate immunity, insulin resistance and type 2 diabetes. Trends Endocrinol Metab. 2008;19(1):10–16. doi:10.1016/j.tem.2007.10.004
6. O’Brien PD, Hinder LM, Parlee SD, et al. Dual CCR2/CCR5 antagonist treatment attenuates adipose inflammation, but not microvascular complications in ob/ob mice. Diabetes Obes Metab. 2017;19(10):1468–1472. doi:10.1111/dom.12950
7. Zhang Z, Zhang X, Dong J, et al. Association of chemokine ligand 5/chemokine receptor 5 gene promoter polymorphisms with diabetic microvascular complications: a meta-analysis. J Diabetes Investig. 2016;7(2):212–218. doi:10.1111/jdi.12397
8. Zhu J, Wilding JPH. The 1α,25(OH)2D3 analogs ZK159222 and ZK191784 show anti-inflammatory properties in macrophage-induced preadipocytes via modulating the NF-κB and MAPK signaling. Diabetes Metab Syndr Obes. 2020;13:1715–1724. doi:10.2147/DMSO.S245080
9. Jamali Z, Nazari M, Khoramdelazad H, et al. Expression of CC chemokines CCL2, CCL5, and CCL11 is associated with duration of disease and complications in type-1 diabetes: a study on Iranian diabetic patients. Clin Lab. 2013;59(9–10):993–1001. doi:10.7754/Clin.Lab.2012.120810
10. Chou SY, Ajoy R, Changou CA, Hsieh YT, Wang YK, Hoffer B. CCL5/RANTES contributes to hypothalamic insulin signaling for systemic insulin responsiveness through CCR5. Sci Rep. 2016;6:37659. doi:10.1038/srep37659
11. Inayat H, Azim MK, Baloch AA. Analysis of inflammatory gene expression profile of peripheral blood leukocytes in type 2 diabetes. Immunol Invest. 2019;48(6):618–631. doi:10.1080/08820139.2019.1586917
12. Kochetova OV, Avzaletdinova DS, Morugova TV, Mustafina OE. Chemokine gene polymorphisms association with increased risk of type 2 diabetes mellitus in Tatar ethnic group, Russia. Mol Biol Rep. 2019;46(1):887–896. doi:10.1007/s11033-018-4544-6
13. Mohamed HG, Idris SB, Ahmed MF, et al. Influence of type 2 diabetes on local production of inflammatory molecules in adults with and without chronic periodontitis: a cross-sectional study. BMC Oral Health. 2015;15:86. doi:10.1186/s12903-015-0073-z
14. Lohmann T, Laue S, Nietzschmann U, et al. Reduced expression of Th1-associated chemokine receptors on peripheral blood lymphocytes at diagnosis of type 1 diabetes. Diabetes. 2002;51(8):2474–2480. doi:10.2337/diabetes.51.8.2474
15. Dworacka M, Krzyżagórska E, Iskakova S, Bekmukhambetov Y, Urazayev O, Dworacki G. Increased circulating RANTES in type 2 diabetes. Eur Cytokine Netw. 2014;25(3):46–51. doi:10.1684/ecn.2014.0355
16. Tokarz A, Konkolewska M, Kuśnierz-Cabala B, et al. Retinopathy severity correlates with RANTES concentrations and CCR 5-positive microvesicles in diabetes. Folia Med Cracov. 2019;59(3):95–112. doi:10.24425/fmc.2019.131139
17. Longo PL, Artese HP, Rabelo MS, et al. Serum levels of inflammatory markers in type 2 diabetes patients with chronic periodontitis. J Appl Oral Sci. 2014;22(2):103–108. doi:10.1590/1678-775720130540
18. Pfleger C, Kaas A, Hansen L, et al; Hvidøre Study Group On Childhood Diabetes. Relation of circulating concentrations of chemokine receptor CCR5 ligands to C-peptide, proinsulin and HbA1c and disease progression in type 1 diabetes. Clin Immunol. 2008;128(1):57–65. doi:10.1016/j.clim.2008.03.458
19. Esposito K, Nappo F, Marfella R, et al. Inflammatory cytokine concentrations are acutely increased by hyperglycemia in humans: role of oxidative stress. Circulation. 2002;106(16):2067–2072. doi:10.1161/01.CIR.0000034509.14906.AE
20. Carvalho-Pinto C, García MI, Gómez L, et al. Leukocyte attraction through the CCR5 receptor controls progress from insulitis to diabetes in non-obese diabetic mice. Eur J Immunol. 2004;34(2):548–557. doi:10.1002/eji.200324285
21. Boon J, Hoy AJ, Stark R, et al. Ceramides contained in LDL are elevated in type 2 diabetes and promote inflammation and skeletal muscle insulin resistance. Diabetes. 2013;62(2):401–410. doi:10.2337/db12-0686
22. Hui N, Barter PJ, Ong KL, Rye KA. Altered HDL metabolism in metabolic disorders: insights into the therapeutic potential of HDL. Clin Sci. 2019;133(21):2221–2235. doi:10.1042/CS20190873
23. Jonas K, Magoń W, Podolec P, Kopeć G. Triglyceride-to-high-density lipoprotein cholesterol ratio and systemic inflammation in patients with idiopathic pulmonary arterial hypertension. Med Sci Monit. 2019;25:746–753. doi:10.12659/MSM.912766
24. Sieg SF, Bazdar DA, Zidar D, Freeman M, Lederman MM, Funderburg NT. Highly oxidized low-density lipoprotein mediates activation of monocytes but does not confer interleukin-1β secretion nor interleukin-15 transpresentation function. Immunology. 2020;159(2):221–230. doi:10.1111/imm.13142
25. Li Q, Wang D, Wang Y, Xu Q. Simvastatin down regulates mRNA expression of RANTES and CCR5 in posttransplant renal recipients with hyperlipidemia. Transplant Proc. 2006;38(9):2899–2904. doi:10.1016/j.transproceed.2006.08.136
26. Hyde CL, Macinnes A, Sanders FA, et al. Genetic association of the CCR5 region with lipid levels in at-risk cardiovascular patients. Circ Cardiovasc Genet. 2010;3(2):162–168. doi:10.1161/CIRCGENETICS.109.897793
27. Słomiński B, Ławrynowicz U, Ryba-Stanisławowska M, Skrzypkowska M, Myśliwska J, Myśliwiec M. CCR5-Δ32 polymorphism is a genetic risk factor associated with dyslipidemia in patients with type 1 diabetes. Cytokine. 2019;114:81–85. doi:10.1016/j.cyto.2018.11.005
28. Cipriani S, Francisci D, Mencarelli A, et al. Efficacy of the CCR5 antagonist maraviroc in reducing early, ritonavir-induced atherogenesis and advanced plaque progression in mice. Circulation. 2013;127(21):2114–2124. doi:10.1161/CIRCULATIONAHA.113.001278
29. Wu Y, Liu F, Zhang X, Shu L. Insulin modulates cytokines expression in human periodontal ligament cells. Arch Oral Biol. 2014;59(12):1301–1306. doi:10.1016/j.archoralbio.2014.07.002
30. Ghanim H, Korzeniewski K, Sia CL, et al. Suppressive effect of insulin infusion on chemokines and chemokine receptors. Diabetes Care. 2010;33(5):1103–1108. doi:10.2337/dc09-2193
31. Yang B, Houlberg K, Millward A, Demaine A. Polymorphisms of chemokine and chemokine receptor genes in type 1 diabetes mellitus and its complications. Cytokine. 2004;26(3):114–121. doi:10.1016/j.cyto.2004.01.005
32. Zhernakova A, Alizadeh BZ, Eerligh P, et al. Genetic variants of RANTES are associated with serum RANTES level and protection for type 1 diabetes. Genes Immun. 2006;7(7):544–549. doi:10.1038/sj.gene.6364326
33. Herder C, Illig T, Baumert J, et al. RANTES/CCL5 gene polymorphisms, serum concentrations, and incident type 2 diabetes: results from the MONICA/KORA Augsburg case-cohort study, 1984-2002. Eur J Endocrinol. 2008;158(5):R1–R5. doi:10.1530/EJE-07-0686
34. Yadav AK, Kumar V, Dutta P, Bhansali A, Jha V. Variations in CCR5, but not HFE, ELMO1, or SLC12A3, are associated with susceptibility to kidney disease in north Indian individuals with type 2 diabetes. J Diabetes. 2014;6(6):547–555. doi:10.1111/1753-0407.12128
35. Shieh B, Liau YE, Hsieh PS, Yan YP, Wang ST, Li C. Influence of nucleotide polymorphisms in the CCR2 gene and the CCR5 promoter on the expression of cell surface CCR5 and CXCR4. Int Immunol. 2000;12(9):1311–1318. doi:10.1093/intimm/12.9.1311
36. Buraczynska M, Zukowski P, Wacinski P, Berger-Smyka B, Dragan M, Mozul S. Chemotactic cytokine receptor 5 gene polymorphism: relevance to microvascular complications in type 2 diabetes. Cytokine. 2012;58(2):213–217. doi:10.1016/j.cyto.2012.01.007
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


