Back to Journals » Advances in Medical Education and Practice » Volume 14
Experience of Sudden Shift from Traditional to Virtual Problem-Based Learning During COVID-19 Pandemic at a Medical College in Saudi Arabia
Authors Alsaif F, Neel L , Almuaiqel S, Almuhanna A, Feda J , Alrumaihi N, Alanazi O, Almansour M, Saeed MF, Soliman M
Received 5 February 2023
Accepted for publication 10 April 2023
Published 3 May 2023 Volume 2023:14 Pages 453—461
DOI https://doi.org/10.2147/AMEP.S404461
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Balakrishnan Nair
Faisal Alsaif,1 Lina Neel,2 Saleh Almuaiqel,1 Abdulaziz Almuhanna,1 Jude Feda,3 Nouf Alrumaihi,4 Omar Alanazi,3 Mohammed Almansour,3 Majda Fuad Saeed,3 Mona Soliman3
1College of Medicine, King Saud University, Riyadh, Saudi Arabia; 2College of Medicine, Alfaisal University, Riyadh, Saudi Arabia; 3Medical Education Department, College of Medicine, King Saud University, Riyadh, Saudi Arabia; 4Saudi Commission of Health Specialties, College of Medicine, King Saud University, Riyadh, Saudi Arabia
Correspondence: Mona Soliman, Head of Medical Education Department, Professor of Medical Education and Physiology, College of Medicine, King Saud University, Riyadh, Saudi Arabia, Tel +966505468581, Email [email protected]
Background: COVID-19 pandemic has resulted in a sudden shift to online education. PBL was one of the components that was transformed to online. The aim of the present study was to investigate the impact of the sudden shift to virtual PBL during COVID-19 pandemic in achieving the intended learning objectives of the PBL and to explore the students’ perception of the virtual versus traditional PBL.
Methods: This is a retrospective study that was conducted in the college of medicine, King Saud University. We compared the perception of third year students who participated in traditional face-to-face PBL in 2019– 2020 and in the virtual PBL in 2020– 2021. We compared the performance of the students in the traditional face-to-face and in virtual PBL. An online survey was distributed from October to December 2021. The survey contained 7 sections. Each section included several questions comparing virtual and traditional PBL in that aspect.
Results: Out of 284 third year medical students, 124 students responded with a response rate of 43.66%. More than half of the students (n = 77, 63%) felt significantly motivated to actively participate in PBL sessions in a virtual learning environment, motivated to learn and support group work and gained critical thinking skills (mean = 3.54 ± 0.12 versus 3.59 ± 0.14, p < 0.001). The majority of students (n = 82, 66%) felt significantly more satisfied about their learning during the virtual PBL versus traditional PBL (mean = 3.48 ± 0.42 versus 3.91 ± 0.59, p < 0.001). There was no significant difference in the students’ performance in traditional versus virtual PBL (mean = 4.77 ± 0.22 versus 4.79 ± 0.29, p = 0.2).
Conclusion: The results of this study showed that students were significantly more satisfied with the experience in the virtual versus traditional PBL. Medical students’ performances in virtual PBL were comparable to the traditional face-to-face approach.
Keywords: COVID-19, problem-based learning, PBL, traditional, virtual, learning, medical students
Introduction
In 2020, COVID-19 pandemic has challenged medical education worldwide due to the sudden lockdown and the shift to online education.1,2 Medical students were not allowed to enter hospitals for practice and all the teaching was shifted to online education to maintain social distancing and stop the spread of the pandemic.3,4 Medical education was challenged to adopt new teaching methods suddenly to achieve the intended learning objectives and ensure mastering of the desired essential competencies to graduate a safe general practitioner.5
The aim of the present study was to investigate the impact of the sudden shift to virtual PBL during COVID-19 pandemic in achieving the intended learning objectives of the PBL and to explore the students’ perception of the virtual versus traditional PBL.
Methods
This retrospective study was conducted in the College of Medicine, King Saud University. The study was approved by the Institutional Review Board at the College of Medicine, King Saud University, Ref. No. 21/01098/IRB on 13/12/2021. All methods were carried out in accordance with relevant guidelines and regulations or declaration of Helsinki.
In the College of Medicine at King Saud University, Riyadh, Saudi Arabia, there are a wide variety of teaching methods, including lectures, practical sessions, clinical bed – side teaching, clinical teaching at the clinical skills and simulation center and problem – based learning sessions. Some of these teaching methods were adopted easily online such as lectures. Others were shifted suddenly to the first time to online education. PBL was one of the teaching methods that was shifted to online education. The experience of the online education during the COVID-19 pandemic should be evaluated.6 Some of the positive experiences of online education should be investigated and utilized after the pandemic.7
The College of Medicine’s undergraduate curriculum adopted a hybrid problem-based learning format where the students are in the center of instructional strategy. They work collaboratively to discuss and solve a well-designed problem.8 The PBL sessions take place in the first two years of the curriculum where a small group of students meet with a facilitator twice a week to solve the structured problem related to the course. All facilitators received structured training before enrollment in PBL facilitation. With the COVID-19 situation, teaching in PBL sessions has shifted to online education by using Zoom accounts for each small group. Breakout rooms were activated to encourage active student participation during the sessions. The same number of PBL sessions was delivered with no changes in the cases or the time allocated to the sessions. Training on the online facilitation was conducted for faculty and staff before the beginning of the new academic year to maintain the same quality and standards of PBL.9
Students Perception
We compared the perception of third year students (284) who participated in traditional face-to-face PBL in 2019–2020 and in the virtual PBL in 2020–2021.
An online survey was distributed from October to December 2021. A written informed consent was obtained before the study. The survey contained 7 sections, including motivation, satisfaction, subjective learning gains, tutor’s quality, design of the cases, amount of work and e-learning modules. Each section included several questions comparing virtual and traditional PBL in that aspect.
Students Performance
We compared the performance of the students in the traditional face-to-face versus virtual PBL. The students were given the grades by the PBL facilitators according to the standardized scoring system, including five key areas (score range 0 to 5).
Statistical Analysis
The quantitative data was analyzed using the SPSS software. Data were grouped and tabulated according to the study variables, and appropriate parametric and nonparametric tests were used for analysis. Data represented with a P-value <0.05 was considered a significant result.
Results
Out of 284 third year medical students, 124 responses have been received with a response rate of 43.66% (Table 1).
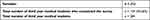 |
Table 1 Demographic Data of the Students Participated in the Study |
Table 2 reveals the students’ perceptions of traditional PBL. The survey on motivation revealed that 63% (n = 77) of the students felt motivated to actively participate in traditional PBL sessions. Half of the students (n = 64, 51%) felt an improvement in motivation to learn when the PBL session was in a traditional learning environment. The results also showed that 59% (n = 73) of the students felt motivated to support group work when a PBL session is in a traditional environment. More than half of the students (n = 75, 61%) revealed that they gained more critical thinking skills in a problem-based approach when PBL was placed in a traditional setting.
 |
Table 2 Students’ Perception of Traditional PBL |
When the students were asked about satisfaction, the results showed that more than half of the students (n = 64, 52%) agreed that they were satisfied about their learning when PBL was placed in a traditional environment. The same case applied when they were asked about subjective learning gains, where more students still showed positive subjective learning gains (n = 56, 45%). However, less than half of the students (n = 46, 37%) were not sure about the subjective learning gains.
The majority of students agreed that the tutor was able to facilitate brainstorming (n = 86, 69%), was able to facilitate hypothesis recognition (n = 83, 67%), was able to facilitate reporting sessions (n = 76, 54%), was able to manage time (n = 72, 58%), and was able to keep the group focused on tasks (n = 99, 80%).
When the students were asked about the design of the case, the majority of the students (n = 95, 77%) agreed that the learning objectives were clear compared to 12% (n = 15) who did not agree. The same scenario was also revealed when the students were asked whether pre-existing knowledge learned from the lectures helped them understand the case when PBL was placed in a traditional environment (n=93, 75%) confirmed that pre-existing knowledge from the lectures helped them understand the case objectives.
More students (n = 58, 47%) were also satisfied with the amount of work assigned to them on learning needs when they were asked about the amount of work. When students were asked about e-learning modules and traditional PBL, more students (n = 48, 39%) did not feel that traditional PBL stimulated the utilization of e-learning resources. Less than half of the students (n = 36, 29%) agreed that e-learning resources were utilized.
Table 3 shows that more than half of the students felt motivated to actively participate in PBL sessions in a virtual learning environment (n = 81, 65%), 62% (n = 77) were motivated to learn and support group work, and 66% (n = 83) gained critical thinking skills in virtual PBL sessions. More than half of the students (n = 82, 66%) felt satisfied about their learning when PBL was placed in a virtual environment. Also, 52% (n = 64) felt that the intended learning objectives were achieved in virtual PBL sessions.
 |
Table 3 Students’ Perception of Virtual PBL |
Regarding the tutor’s quality, the majority of students (n = 92, 74%) felt that tutors were able to facilitate the brainstorming, 72% (n = 89) felt that the tutors were able to facilitate the hypothesis recognition, and 64% (n = 80) facilitate the reporting session during the virtual PBL sessions. The majority (n = 75, 85%) felt that the tutors managed the time appropriately and helped to keep the group focused on the task (n = 80, 65%) during the virtual sessions.
Almost all students (n = 109, 88%) felt that the learning objectives for the case were clear when they attended virtual PBL sessions, also 84% (n = 104) confirmed that pre-existing knowledge from the lectures helped them understand the case objectives during virtual learning. The majority of the students (n = 89, 72%) were also satisfied with the amount of work assigned to them on learning needs in the virtual PBL sessions when they were asked about the amount of work. Seventy-eight percent (n = 97) of students felt that virtual PBL sessions stimulated the utilization of eLearning resources.
When the result from the survey on students’ perception of traditional PBL was compared to that of the perception of virtual PBL, the following was revealed. First, the perception of traditional PBL showed a lower mean throughout except for the quality of the tutor, where it had a mean of 3.721 compared to the participants’ perception of virtual PBL, which had a mean of 3.719. This means that more students had a higher perception and approval of the virtual PBL compared to traditional. However, the traditional PBL would still perform better than the virtual PBL on tutor quality. For instance, many students felt that the tutor was able to facilitate brainstorming, was able to facilitate hypothesis recognition, was able to facilitate reporting sessions, was able to manage time, and was able to keep the group focused on tasks in traditional PBL compared to the virtual PBL environment.
Table 3 shows that more than half of the students felt motivated to actively participate in PBL sessions in a virtual learning environment, motivated to learn and support group work and gained critical thinking skills. The majority of students (n = 82, 66%) felt satisfied about the virtual PBL (Table 3). More than half of the students (n = 64, 52%) felt that the intended learning objectives were achieved in virtual PBL sessions (Table 3). The majority of students (n = 92, 74%) felt that tutors were able to facilitate the brain storming, facilitate the hypothesis recognition (n = 89, 72%) and facilitate the hypothesis recognition (n = 80, 64%) during the virtual PBL sessions (Table 3). Table 3 shows that the majority of students (n = 75, 85%) felt that the tutors managed the time appropriately and helped to keep the group focused on the task (n = 80, 65%) during the virtual sessions. Almost all students (n = 109, 88%) felt that learning objectives for the case were clear when you attended virtual PBL sessions. Ninety-seven (75%) of students felt that virtual PBL sessions stimulated the utilization of eLearning resources (Table 3).
Table 4 shows the students’ perception of traditional versus virtual PBL presented as mean ± SD. The students felt significantly motivated to actively participate in PBL sessions in a virtual learning environment, motivated to learn and support group work and gained critical thinking skills (mean = 3.54 ± 0.12 versus 3.59 ± 0.14, p < 0.001). The students felt significantly more satisfied with their learning in the virtual PBL more than the traditional PBL (mean = 3.48 ± 0.42 versus 3.91 ± 0.59, p < 0.001). The students (n = 64, 52%) felt that the intended learning objectives were achieved in virtual PBL sessions significantly better than the traditional PBL (mean = 3.36 ± 0.45 versus 3.57 ± 0.45, p < 0.001). There was no significant difference in the students’ perception of the tutor quality between traditional versus virtual PBL (mean = 3.72 ± 0.11 versus 3.72 ± 0.13, p = 0.98). There was a significant difference in student’s perception of the design of the cases (mean = 3.97 ± 0.36 versus 4.28 ± 0.45, p < 0.001), amount of work and utilization of e-learning resources (mean = 2.84 ± 0.33 versus 4.18 ± 0.79, p < 0.001) in virtual PBL compared to traditional PBL.
 |
Table 4 Mean Scores ± SD of Students’ Perception of Traditional versus Virtual PBL |
Table 5 shows that there was no significant difference in the students’ performance in traditional versus virtual PBL (mean = 4.77 ± 0.22 versus 4.79 ± 0.29, p = 0.2).
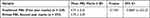 |
Table 5 Students’ Performance in Traditional versus Virtual PBL |
Discussion
E-Learning in Medical Education
The role of e-learning in medical education has been well established.8–10 During COVID-19 pandemic, there has been extensive adoption of e-learning in medical education, especially during the lockdown and the implications of the pandemic that required social distancing.1,11–15 Further investigation is essential to ensure that the intended learning outcomes are achieved as planned with the sudden shift to online education. Therefore, it is essential to evaluate the different experiences during the pandemic and to retain the positive experiences in medical education.16
Problem-Based Learning & Medical Education
PBL was first approved and implemented in McMaster University, Ontario, Canada, in 1969.17 Since then, PBL has been adopted widely in medical education as an alternative to the traditional strategy of teaching. PBL is a strategy of learning in medical education that facilitates students’ active learning, communication skills, team work and ability to solve problems. Students work in small groups to solve a problem that is given to them as a case scenario. PBL facilitators help students to determine their learning needs, encourage students’ active participation and provide constructive feedback.18
Problem-Based Learning During COVID-19
During the pandemic and the implications of lockdown, there has been a complete shift to online education worldwide.19 PBL was one of the components of teaching in medical education that was transformed to online. The present study investigated the impact of the sudden shift to virtual PBL during COVID-19 pandemic in achieving the intended learning objectives of the PBL and the explored the students’ perception of the virtual versus traditional PBL. The results of this study showed that students were significantly more satisfied with the experience and achievement of the intended learning outcomes in the virtual PBL in terms of motivation, satisfaction, learning gains, amount of work and utilization of the e-learning modules. There was no significant difference in the quality of tutors in traditional versus virtual PBL. However, medical students’ performances in virtual PBL were comparable to the traditional face-to-face approach.
Online PBL (e-PBL) has been implemented in medical education before the pandemic, as technology is increasingly integrated into medical education.20,21 Previous study by Kim and Kee in 201320 revealed that students perceived e-PBL significantly more positive than the traditional PBL and found the learning process effective, which illustrates the potential of e-PBL to enhance traditional PBL and offers practical example for the utilization of technology in PBL. Kim and Kee recommended that e-PBL can be used as a tool to promote individual reasoning in supplement to traditional PBL. Previous studies have demonstrated that e-PBL is as effective as traditional PBL.22–24 The present study evaluated the students’ perception of the virtual PBL that was implemented during the lockdown due to COVID-19 pandemic. The results of this study will help to utilize and implement positive experiences in medical education that were practiced during the pandemic. The question is that whether the virtual PBL can achieve educational goals in undergraduate medical education where the face-to-face traditional educational method is the predominant method of teaching.
However, another study by Foo et al,5 that was done to compare the virtual and the face-to-face approach in conducting PBL, revealed that the performance of students in virtual PBL was lower than that of students participating in the face-to-face PBL approach. Previous studies showed that virtual PBL is associated with reduced student engagement, reduced communication and poor motivation.25–27 Further studies are needed to compare the virtual and the face-to-face PBL and to define the benefits of utilizing the virtual PBL while ensuring the achievement of the intended learning outcomes of PBL.
Limitations
One of the limitations to this study is that it was conducted on the same group of students. However, the results of the present study showed that students were significantly more satisfied with the experience and achievement of the intended learning outcomes in the virtual versus traditional PBL. Further research is needed to guide the effective implementation and utilization of virtual PBL to ensure the achievement of the intended learning outcomes of PBL. Another limitation is that the present study investigated the virtual PBL from student perception level only with the impact on the students’ achievement. Further studies are needed to study the perception of faculty.
Conclusions
The results of this study showed that students were significantly more satisfied with the experience and achievement of the intended learning outcomes in the virtual versus traditional PBL in terms of motivation, satisfaction, learning gains, amount of work and learning modules. There was no significant difference in the quality of tutors in traditional versus virtual PBL. However, medical students’ performances in virtual PBL were comparable to the traditional face-to-face approach.
Data Sharing Statement
The datasets generated and/or analysed during the current study are not publicly available but are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
The study was approved by the Institutional Review Board at the College of Medicine, King Saud University, Ref. No. 21/01098/IRB on 13/12/2021. A written informed consent was obtained from all the participants before the study.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
This study did not receive funding.
Disclosure
The authors declare that they have no competing interest.
References
1. Rose S. Medical student education in the time of COVID-19. JAMA. 2020;323(21):2131–2132. doi:10.1001/jama.2020.5227
2. Ferrel MN, Ryan JJ. The impact of COVID-19 on medical education. Cureus. 2020;12(3):e7492. doi:10.7759/cureus.7492
3. Quilty BJ, Diamond C, Liu Y, et al. The effect of travel restrictions on the geographical spread of COVID-19 between large cities in China: a modelling study. BMC Med. 2020;18(1):259. doi:10.1186/s12916-020-01712-9
4. Liang ZC, Ooi SBS, Wang W. Pandemics and their impact on medical training: lessons from Singapore. Acad Med. 2020;95(9):1359–1361. doi:10.1097/ACM.0000000000003441
5. Foo CC, Cheung B, Chu KM. A comparative study regarding distance learning and the conventional face-to-face approach conducted problem-based learning tutorial during the COVID-19 pandemic. BMC Med Educ. 2021;21(1):141. doi:10.1186/s12909-021-02575-1
6. Shahrvini B, Baxter SL, Coffey CS, et al. Pre-clinical remote undergraduate medical education during the COVID-19 pandemic: a survey study. BMC Med Educ. 2021;21(1):13. doi:10.1186/s12909-020-02445-2
7. Venkatesh S, Rao Y, Nagaraja H, et al. Factors influencing medical students’ experiences and satisfaction with blended integrated E-learning. Med Princ Pract. 2020;29(4):396–402. doi:10.1159/000505210
8. Kim S. The future of E-Learning in medical education: current trend and future opportunity. J Educ Eval Health Prof. 2006;3:3. doi:10.3352/jeehp.2006.3.3
9. Ruiz JG, Mintzer MJ, Leipzig RM. The impact of E-learning in medical education. Acad Med. 2006;81(3):207–212. doi:10.1097/00001888-200603000-00002
10. Lau F, Bates J. A review of e-learning practices for undergraduate medical education. J Med Syst. 2004;28(1):71–87. doi:10.1023/B:JOMS.0000021522.30587.ff
11. Zheng M, Bender D, Lyon C. Online learning during COVID-19 produced equivalent or better student course performance as compared with pre-pandemic: empirical evidence from a school-wide comparative study. BMC Med Educ. 2021;21(1):495. doi:10.1186/s12909-021-02909-z
12. Khalil R, Mansour AE, Fadda WA, et al. The sudden transition to synchronized online learning during the COVID-19 pandemic in Saudi Arabia: a qualitative study exploring medical students’ perspectives. BMC Med Educ. 2020;20(1):285. doi:10.1186/s12909-020-02208-z
13. AlQhtani A, AlSwedan N, Almulhim A, et al. Online versus classroom teaching for medical students during COVID-19: measuring effectiveness and satisfaction. BMC Med Educ. 2021;21(1):452. doi:10.1186/s12909-021-02888-1
14. Gismalla MD, Mohamed MS, Ibrahim OSO, et al. Medical students’ perception towards E-learning during COVID 19 pandemic in a high burden developing country. BMC Med Educ. 2021;21(1):377. doi:10.1186/s12909-021-02811-8
15. Al Zahrani EM, Al Naam YA, AlRabeeah SM, et al. E- Learning experience of the medical profession’s college students during COVID-19 pandemic in Saudi Arabia. BMC Med Educ. 2021;21(1):443. doi:10.1186/s12909-021-02860-z
16. Ahmed SA, Hegazy NN, Abdel Malak HW, et al. Model for utilizing distance learning post COVID-19 using (PACT) a cross sectional qualitative study. BMC Med Educ. 2020;20(1):400. doi:10.1186/s12909-020-02311-1
17. Neufeld VR, Woodward CA, MacLeod SM. The McMaster M.D. program: a case study of renewal in medical education. Acad Med. 1989;64(8):423–432. doi:10.1097/00001888-198908000-00001
18. Maudsley G. Roles and responsibilities of the problem based learning tutor in the undergraduate medical curriculum. BMJ. 1999;318(7184):657–661. doi:10.1136/bmj.318.7184.657
19. Eva KW, Anderson MB. Medical education adaptations: really good stuff for educational transition during a pandemic. Med Educ. 2020;54(6):494. doi:10.1111/medu.14172
20. Kim KJ, Kee C. Evaluation of an e-PBL model to promote individual reasoning. Med Teach. 2013;35(3):e978–83. doi:10.3109/0142159X.2012.717185
21. Bizzocchi J, Schell R. Rich-narrative case study for online PBL in medical education. Acad Med. 2009;84(10):1412–1418. doi:10.1097/ACM.0b013e3181b6ead0
22. Dennis JK. Problem-based learning in online vs. face-to-face environments. Educ Health. 2003;16(2):198–209. doi:10.1080/1357628031000116907
23. Taradi SK, Taradi M, Radić K, et al. Blending problem-based learning with Web technology positively impacts student learning outcomes in acid-base physiology. Adv Physiol Educ. 2005;29(1):35–39. doi:10.1152/advan.00026.2004
24. Woltering V, Herrler A, Spitzer K, et al. Blended learning positively affects students’ satisfaction and the role of the tutor in the problem-based learning process: results of a mixed-method evaluation. Adv Health Sci Educ Theory Pract. 2009;14(5):725–738. doi:10.1007/s10459-009-9154-6
25. Lee ICJ, Koh H, Lai SH, et al. Academic coaching of medical students during the COVID-19 pandemic. Med Educ. 2020;54(12):1184–1185. doi:10.1111/medu.14272
26. Longhurst GJ, Stone DM, Dulohery K, et al. Strength, Weakness, Opportunity, Threat (SWOT) analysis of the adaptations to anatomical education in the United Kingdom and Republic of Ireland in response to the covid-19 pandemic. Anat Sci Educ. 2020;13(3):301–311. doi:10.1002/ase.1967
27. Kaup S, Jain R, Shivalli S, et al. Sustaining academics during COVID-19 pandemic: the role of online teaching-learning. Indian J Ophthalmol. 2020;68(6):1220–1221. doi:10.4103/ijo.IJO_1241_20
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
