Back to Journals » Advances in Medical Education and Practice » Volume 13
Impact of COVID-19 Pandemic on Medical Education: A Cross-Sectional Study in the Western Region of Saudi Arabia
Authors Samannodi M , Bulkhi A, Alwafi H , Bukhari R, Salawati E , Hafiz B, Minshawi F , Dahlawi M , Kamfar S , Halawani H, Naser AY , Mandora R, Alshekh Ali M , Almatrafi MA
Received 3 April 2022
Accepted for publication 8 July 2022
Published 21 July 2022 Volume 2022:13 Pages 741—754
DOI https://doi.org/10.2147/AMEP.S369213
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Md Anwarul Azim Majumder
Mohammed Samannodi,1 Adeeb Bulkhi,1 Hassan Alwafi,2 Rahaf Bukhari,2 Emad Salawati,3 Bayan Hafiz,2 Faisal Minshawi,4 Maryam Dahlawi,2 Sara Kamfar,5 Hanan Halawani,6 Abdallah Y Naser,7 Roaa Mandora,2 Mohamad Alshekh Ali,8 Mohammed A Almatrafi9
1Department of Medicine, College of Medicine, Umm Al-Qura University, Makkah, Saudi Arabia; 2Faculty of Medicine, Umm Al-Qura University, Mecca, Saudi Arabia; 3Department of Family Medicine, Faculty of Medicine, King Abdulaziz University, Jeddah, Saudi Arabia; 4Department of Laboratory Medicine, Faculty of Applied Medical Sciences, Umm Al-Qura University, Makkah, Saudi Arabia; 5Department of Medicine, King Abdulaziz University, Jeddah, Saudi Arabia; 6Computer Science Department, College of Computer Science and Information Systems, Najran University, Najran, Saudi Arabia; 7Department of Applied Pharmaceutical Sciences and Clinical Pharmacy, Faculty of Pharmacy, Al-Isra University, Amman, Jordan; 8Department of Medicine, Batterjee Medical College, Jeddah, Saudi Arabia; 9Department of Pediatrics, Umm Al-Qura University, Makkah, Saudi Arabia
Correspondence: Hassan Alwafi, Faculty of Medicine, Umm Al-Qura University, Mecca, 24381, Saudi Arabia, Tel +966555544319, Email [email protected]
Background: As the Coronavirus Disease 2019 (COVID-19) outbreak has made a tremendous impact on medical education and healthcare institutions, we aimed to measure effects of online classes on medical students’ comprehension in comparison with attending campus classes during the COVID-19 pandemic.
Methods: A cross-sectional survey has been conducted between September 2020 and June 2021 in the western region of Saudi Arabia. The Convenience sampling technique was conducted to collect the data from medical students in their basic and clinical years, using a questionnaire that involved 45 multiple-choice and multiple-answer questions.
Results: Out of 3700 questionnaires, 922 completed the questionnaires from 11 different medical schools. Umm AL-Qura University had the highest response rate with 232 responses (25.2%), followed by King Abdulaziz University with 186 responses (20.2%). The majority of institutions preferred Blackboard and Zoom as platforms for e-learning. A total of 355 (38.5%) believed that it resulted in higher academic achievement, whereas 555 (60.2%) of students believed the limitation of clinical access was one of the biggest disadvantages of e-learning. Overall, 518 (56.2%) of students did not want to continue using e-learning on its own in the future. Whereas 668 (72.5%) wished to keep using e-learning in combination with traditional learning.
Conclusion: According to our findings, advantages of e-learning vary among students. Most of the students thought e-learning to be an interactive system that provides a learning opportunity. In contrast, many of the students believed that there were many disadvantages regarding online teaching methods.
Keywords: COVID-19, e-learning, students, online, learning
Summary of Study
The pandemic of Coronavirus Disease 2019 (COVID-19) has a significant influence on medical education and healthcare institutions. To support the learning objectives during the pandemic, several learning management systems were used. In Saudi Arabia, the majority of colleges adopted the online teaching methods. There is considerable similarity between online and traditional education. While several research have concluded that there are no substantial differences between traditional and e-learning, some have found the opposite. One of the most serious drawbacks of e-learning is the lack of clinical access. In Saudi Arabia, e-learning is not the favored mode of teaching in medical schools. The majority of the students thought of e-learning as an interactive system that allows them to learn.
Background
Coronavirus disease (COVID-19) was discovered in December 2019 in Wuhan, Hubei Province, China-pneumonia-like symptoms characterize the virus. The disease spread rapidly globally, resulting in an outbreak. The World Health Organization (WHO, 2020) declared it a global pandemic on March 11, 2020.1
Since March 25, 2020, over 150 countries have temporarily shut down colleges and educational institutions, affecting more than 80% of the world’s student population. According to the Saudi Ministry of Education, health authorities have recommended “preventive and precautionary” measures to ensure that students and staff are appropriately protected.2
This has led to a shift in education in most academic faculties, transforming learning from traditional to online. Consequently, colleges provided students with several learning management systems.3 One of the most suggested approaches is scheduled live-online video lectures with interactive discussions using different applications or self-study online recorded lectures.4,5 Virtual clinical experience was another approach to the suspension of clinical clerkship rotation. This idea supports the concern of the Ministry of Health regarding medical students’ exposure to the virus during training as well as their potential to act as spreaders of the virus in the community.6 They were limited patient care and bedside learning opportunities during the pandemic, as doctors and other healthcare workers were required to focus on COVID-19 cases. Hence, students were safe at home, complying with social distance guidelines; they learned about the dynamics of patient interaction by interviewing patients, collaborating with treatment planners, assisting with paperwork, and counselling patients.7
Online and traditional education shares several similarities. Students still have to attend class, learn new topics, submit assignments, and participate in group projects. While many studies have found no significant differences between traditional and e-learning, others have reported opposing results.8 E-learning offers more program choices, compared with traditional face-to-face learning. It is classified as synchronous or asynchronous. Synchronous e-learning allows live interactions between tutors and students, such as live-video conferences and chats.9 Asynchronous e-learning can involve e-mails, recorded videos, etc., where there are time lags between the tutor and their students.9
With traditional classroom education, students are confined to taking courses at specific centers on a fixed schedule. Thus, e-learning helps save up to 60% of traditional learning time, with the only requirements being an adequate computer, internet connection, and basic computer skills.10,11
In contrast, online classes involved an absence of in-person, face-to-face classroom, or office interactions. For many students and programs, interpersonal communication is crucial. For example, consulting lecturers in person and discussing matters in groups is an essential motivational activity and learning strategy; however, it is not easy to practice medicine online.12–16
Additionally, the on-campus atmosphere and the opportunity to meet many people face-to-face is another motivation for students; moreover, it has an essential impact on student performance and understanding lectures. Nevertheless, in e-learning, online classes depend on personal factors, such as: student’s home environment, socioeconomic factors, and parents’ level of education. Unfortunately, conducive surroundings are not always available to many students.
Another essential factor in students’ comprehension; online teaching can easily create a sense of boredom while listening to a monotonous lecture, devoid of interaction and visual stimulation. This reduces students’ motivation to attend future lectures.17
The perceived benefits of both teaching methods must be thoroughly outlined and assessed to determine which medium generates better student performance. Both approaches are generally beneficial; however, we still need to examine whether one is more superior compared to the other. Hence, this study aimed to measure the effect of online classes on medical students’ comprehension attending campus classes during the COVID-19 pandemic.
Methods
Study Design
We conducted a cross study using an online survey between 2020 and 2021. Data were collected from medical students in their basic and clinical years in the western region of Saudi Arabia using a questionnaire. Questionnaires with incomplete or missing data were excluded from the analysis.
Questionnaire Tool
The survey was adapted from previously validated assessment scales.3,18 The survey involved 45 multiple-choice and multiple-answer questions, including primary demographic data, such as age, gender, academic year, and the name of the school they attended, without recording any identifying data for confidentiality. Additionally, the survey included general questions about the students’ knowledge of e-learning and the status of the technology tools used during the education process. It also had questions to assess the students’ attitude toward the e-learning system as well as their evaluation and suggestions for improving online teaching. Finally, specific questions were asked to appraise the effect of the COVID-19 pandemic on medical students.
Sampling Strategy
A convenience sampling method was used. All medical students in the Western region of Saudi Arabia were invited to participate in the study. The inclusion criteria were clear in the invitation letter and sent along with the survey link. There was no incentive was provided to the participants to be involved in the study. The survey was conducted online using the Google Forms© and was distributed through social media platforms such as: WhatsApp, and Twitter. A total of 922 respondents were included.
Study Outcomes
The primary outcome was measuring the effect of online classes on medical students’ comprehension of attending campus classes during the COVID-19 pandemic. Secondary outcomes included comparing the level of medical students’ morning excitement for attending lectures before and during COVID-19; further, we also assessed medical students’ attendance rate before and during COVID-19 and the effect of students’ limited clinical exposure on their knowledge. A copy of the questionnaire will be found in Supplementary Section.
Statistical Analysis
Descriptive statistics were used to summarize the data and synthesize a report of the variables. The data description includes proportions and frequencies, for continuous variables. The statistical analyses were carried out using S.P.S.S. (version 27).
Results
Demographics Characteristics
Of the 3700 questionnaires, we collected 922 completed online questionnaires from students of 11 medical schools in the western region of Saudi Arabia. Participants were predominantly women; the sample included 693 (75.2%) women and 229 (24.8%) men; their mean age was 22 (28.3%) years. Umm AL-Qura University had the highest response rate with 232 responses (25.2%), followed by King Abdulaziz University with 186 responses (20.2%) and Taibah University with 112 responses (12.1%). Two (0.2%) of those who completed the survey were not included in the western region of Saudi Arabia. A more significant number of respondents included medical students who had finished their fourth year with a response rate of 325 (35.2%), followed by those who completed the fifth year with 310 responses (33.6%). Finally, 33 (3.6%) responses completed by prior-year students or interns were not included in the sample size. For details see Table 1.
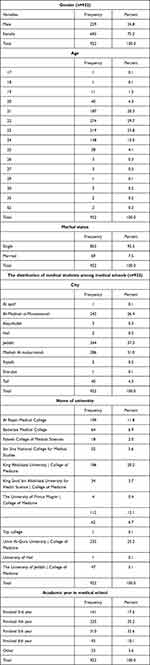 |
Table 1 Demographic Data of the Study Participants |
Students’ Experience About e-Learning
Approximately 49.2% students started online classes during the first week of lockdown. The majority of institutions preferred Blackboard and Zoom as video-conferencing platforms for e-learning. A total of 624 (67.7%) students used Blackboard, whereas 612 (66.4%) used Zoom. Microsoft Teams and Webex Meet were less preferred, as 237 (25.7%) and 128 (13.9%) used Microsoft Teams and Webex Meet, respectively. Overall, 727 (78.9%) students had five or more online classes per week, 30.3% of them had live classes (synchronous), 6% had recorded classes (asynchronous), and 63.8% had both (synchronous and asynchronous) (see Table 2).
 |
Table 2 Students’ Experience About e-Learning |
Effect of COVID-19 on the Medical Education Process and Evaluation of e-Learning
A total of 395 (42.8%) had experienced suspension of their education by the faculty, and 529 (57.4%) had suspended their clinical training. In addition, 17.4% students suspended their education program by themselves due to social status and personal responsibilities. Thus, 410 (44.5%) students stated that the COVID-19 pandemic did not affect their career plans and future interests, but 331 (35.9%) reported the opposite. Moreover, owing to the lockdown students had more free time than earlier. Overall, 490 (53.1%) students spent their time resting and relaxing, 456 (49.5%) spent time with family, and 386 (41.9%) spent their time watching television. However, our study showed that many students invested their time wisely, as 619 (67.1%) students participated in programs related to medical education. Further, approximately 396 (43%) participated in medical research activities and 401 (43.5%) in volunteering activities; for details (see Tables 3 and S1).
 |
Table 3 Effect of COVID-19 on the Medical Education Process |
Student’s Attitude During COVID-19 Pandemic
Regarding students’ attitudes toward e-learning, 391 (42.4%) students were worried about losing opportunities to apply for specialty training due to the lockdown. Regarding the students’ perspectives on e-learning, the study shows that a majority of students, that is 451 (48.9%), believed that e-learning depends on the comprehensive digital electronic environment displaying educational curriculum through electronic networks. In comparison, 423 (45.9%) students believed it was an interactive system that provided an opportunity to learn information and telecommunication technology. Moreover, 367 (39.8%) students believed that e-learning provides digital multimedia content (ie, written text, audio, video, and images). Less than one-third of the students, that is 255 (27.7%), believed that e-learning in the medical field is not less expensive than conventional learning. A total of 248 (26.9%) students considered e-learning as a type of tele-education, and for 207 (22.5%) instant feedback from the instructor was a benefit of online-learning. E-learning has benefits and drawbacks that affect students’ lives differently. Overall, 603 (65.4%) students agreed e-learning helps save money and energy, that is typically expended during commuting; moreover, they believed it was a more straightforward learning method.
Furthermore, 365 students (39.6%) believed that it limits the consequences of social contact and 355 (38.5%) thought it causes fewer absences than traditional teaching, whereas 296 (32.1%) students believed that e-learning caused more absences. A total of 232 (25.2%) students believed that it resulted higher academic achievement, whereas 230 (24.9%) agreed that results in better student interaction in classes. However, as Table 4 shows, 555 (60.2%) of students believed the limitation of clinical access was one of the biggest disadvantages of e-learning. Moreover, 466 (50.5%) students disliked the absence of direct contact with a lecturer in e-learning, whereas 386 (41.9%) believed that technical requirements were a disadvantage of e-learning. In contrast, 323 (35%) students did not have a conducive environment in the house during online classes. Approximately one-third (32.8%) students believed that e-learning courses lower academic achievement; moreover, 160 (17.4%) felt that online classes were not safe, whereas 280 (30.4%) students were unable to adapt to e-learning. Regarding student attendance, 727 (78.9%) students attended five lectures or more per week, and 376 (40.8%) students were able to participate in more than 80% of the classes per week. Moreover, 409 (44.4%) students attended only 50–80% of the classes, whereas 137 (14.9%) were able to participate in only less than 50%. For details see Table 4.
 |
Table 4 Student’s Attitude During COVID-19 Pandemic |
Status of Educational Technology Tools During the COVID-19 Pandemic
Table S2 describes the students’ proficiency with using various electronic devices: 108 (11.7%) reported themselves as proficient, 171 (18.5%) were perfect, 371 (40.2%) were good, 228 (24.7%) had an acceptable level, and 4.8 (44) had an inadequate level. In medical education, the students’ computers varied between tablets (683 [74.1%]) and smartphones (457 [49.6%]). Further, 543 (58.9%) students used personal computers. Around, 698 (75.7%) were dependent on the university’s lectures for their study, 619 (67.1%) were dependent on self-study and utilized various educational sources, whereas 254 (27.5%) attended extra courses provided by private education centers.
E-Learning Improvement
Finally, the students could help assess e-learning, as shown in Table S3. Overall, 518 (56.2%) students did not want to continue using e-learning on its own in the future, whereas 668 (72.5%) wished to use e-learning in combination with traditional learning.
Discussion
The COVID-19 pandemic has resulted in a remarkable shift in education and learning methods. Additionally, some medical colleges have adopted open-book examinations, which have shifted toward an entirely new online teaching and examination system. Therefore, studying the effects of e-learning using several parameters on medical students is imperative e-learning. This study aimed to measure the impact of online classes on medical students’ comprehension of attending campus classes during the COVID-19 pandemic. Moreover, we compared the different changes in medical students’ levels of excitement and rate of attendance in e-learning before and after the pandemic.
According to medical students’ responses, our findings revealed that the advantages of e-learning vary among students. Of the students, 423 (45.9%) thought e-learning to be an interactive system that provides a learning opportunity. In contrast, a minimal number of students agreed that they had interactive classes. Consequently, 232 (25.2%) believed that it offered high academic achievement. Likewise, in the study conducted by Cicha et al, the majority of participants demonstrated a positive feedback about distance learning.19 In contrast, when asked about the disadvantages, most students believed that the limitations of clinical access were one of the worst disadvantages of e-learning. Moreover, 466 (50.5%) students disliked the absence of direct contact with the lecturer during classes. In contrast, 323 (35%) students did not have a calm home environment during online classes. Finally, 280 (30.4%) could not adapt to their online environment. Compared to our study, similar advantages and disadvantages were found in many reports in the literature.17,19–22
Technology knowledge is one of the most important factors for easy transition and success in e-learning.23–25 In our study, the participants reported the need of technical knowledge was one of the major disadvantages of e-learning.
Based on the previous responses of our survey, we noted that medical students believed that e-learning has far more disadvantages, compared with traditional methods that allow for clinical exposure. These disadvantages are considered critical parameters that facilitate each student’s comprehension and understanding. A total of 302 (32.8%) students believed that e-learning lowered academic achievement.
The survey results indicate a change in the attendance rates during the pandemic, compared with those recorded before the pandemic. A total of 376 (40.8%) of students could attend more than 80% of classes per week. In contrast, 137 (14.9%) attended less than 50% of the classes. The underlying reasons behind their absenteeism include poor internet connection, inappropriate class timing, and discomfort with virtual teaching.
Several studies have supported the impact of the COVID-19 pandemic on medical education using different perspectives. A study that took place in United Kingdom has identified the effect of the COVID-19 outbreak on final year medical students’ examinations, electives, and assistantship placements and the subsequent impact on preparedness and confidence. Many students felt less prepared to begin work as doctors. This study shows that disruptions to student assistantships significantly impact preparedness, which results in lowered academic achievement.26
Another study investigated medical students’ perceptions regarding the role of online teaching in facilitating medical education during the COVID-19 pandemic. This study suggests that most students prefer face-to-face teaching.27 This study reported that the cancellation of clinical examinations and the conversion of written examinations into open book ones reduces student engagement, which was in line with the findings of our study.
A few limitations of e-learning mentioned in this study was related to technical issues. Moreover, many teachers are inadequately prepared and face many technical difficulties. The quality of the sessions delivered may have been affected by several factors, such as poor internet connection, family distractions, and the timing of the tutorials, as demonstrated by our results.
Students’ mental health is impacted by the COVID-19 pandemic, which may be adversely affected by the lack of interaction with friends and colleagues, leading to an increase in anxiety.18 As mentioned in the same study, the main advantages of online teaching are the time and money saved from the lack of travel, flexibility, and the ability for students to learn at their own pace.27 This is similar to our results.
Another study conducted in Jordan,3 which assessed students’ class experience, lecturers’ interaction, and e-learning advantages and disadvantages. Their results show that the e-learning experience was not favorable for most medical students due to limitations with regard to technology, and that traditional face-to-face teaching method is preferred for various reasonse-learning. Furthermore, the non-direct contact between lecturers and students is a significant obstacle, as students and lecturers have had on-ground interaction during regular lectures prior to COVID-19. Finally, the lack of clinical access to medical students is one of the most significant disadvantages due to the essentiality of patients’ exposure to medical students in clinical years.3 In contrast, their students’ online attendance rate was lower than ours. Thus, the cause of this difference in attendance rates required further investigation.3
Another study evaluated the comparison between face-to-face learning and e-learning modalities in teaching an environmental science course and additionally evaluated factors of gender and class rank.11
The results of this study did not show significant difference in performance between online and traditional classroom students by modality and gender. Further, as there is no significant difference in student performance between the two mediums, higher education institutions may gradually shift away from traditional instruction and implement web-based teaching to capture a larger worldwide audience.
If administered correctly, this shift to web-based teaching could lead to a higher cost efficiency, and higher university revenue.11
Many hospitals have suspended medical student clerkships during COVID-19 pandemic. Unfortunately, in our study, student clerkships in the hospitals were suspended or postponed in about 50% of participants. This is can be a major defect in their medical education journey and needs to be compensated as soon as applicable (12,J).
Our study had some limitations. First, the design of the study is cross-sectional in nature, some missing data could limit the conclusion of the study. The independent variables were not adjusted for real-life accuracy. Furthermore, students have different skills, abilities, preparation, and familiarity with online instructions. Experienced traditional classroom students who take online-based classes and lectures may lack the technical requirements of e-learning. Therefore, they may not be prepared to use e-learning efficiently, thus leading to lowered scores. Second, some medical schools may have been disproportionately represented with more significant numbers of responses from some schools. Finally, some aspects of our survey depended on students’ memory, which may have influenced their reporting.
Implications and Recommendations
Our study is relevant as it explored a crucial educational topic. Simultaneously, the COVID-19 pandemic has accelerated the widespread use of electronic learning in medical education without pre-preparations. This fast acceleration should be investigated to determine its advantages and disadvantages. The results of this study will help make critical decisions for the future of medical education. Moreover, it would help improve electronic education and adapt it to the needs of medical education and medical students by considering all the benefits. According to the student’s responses, as shown in the results, 72.5% (668) wished to use e-learning in combination with traditional learning. Face-to-face learning is essential to increase the academic achievement of medical students and has higher clinical exposure. Additionally, online-learning helps save time, money, and energy. Additionally, we recommend that medical students should be prepared for online applications and platforms to improve their knowledge and experience.
Future studies are needed to investigate the same topic in the broader field of medical education, including the basic years. Moreover, further examination is necessary to find alternative models of clinical exposure that would be effective in compensation during situations similar to the COVID-19 pandemic. Finally, additional studies are needed to investigate an appropriate and effective way to use e-learning alongside traditional learning.
Conclusion
This study found that advantages of e-learning vary among students. Most of the students thought e-learning to be an interactive system that provides a learning opportunity. In contrast, many of the students believed that there were many disadvantages regarding online teaching methods. These findings has been seen in many reports in the literature recently and indicates that further studies are needed to identify the potential causes.
Ethical Statement and Institutional Review of Board Statement
The study was approved by the Faculty of Medicine at Umm Al-Qura University, Makkah, Saudi Arabia (NO. HAPO-02-K-012-2021-06-696). This study was performed in accordance with the principles stated in the Declaration of Helsinki.
Informed Consent
Informed consent was obtained from all subjects involved in the study.
Disclosure
The authors declare no conflicts of interest.
References
1. World Health Organization. WHO director-general’s opening remarks at the media briefing on COVID-19-11 March 2020; 2020. Available from: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-The-media-briefing-on-covid-19—11-march-2020.
2. Sayed AA. The progressive public measures of Saudi Arabia to tackle Covid-19 and limit its spread. Int J Environ Res Public Health. 2021;18:2. doi:10.3390/ijerph18020783
3. Sindiani AM, Obeidat N, Alshdaifat E, et al. Distance education during the COVID-19 outbreak: a cross-sectional study among medical students in North of Jordan. Ann Med Surg. 2020;59:186–194. doi:10.1016/j.amsu.2020.09.036
4. Mian A, Khan S. Medical education during pandemics: a UK perspective. BMC Med. 2020;18(1):100. doi:10.1186/s12916-020-01577-y
5. Chiodini J. Online learning in the time of COVID-19. Travel Med Infect Dis. 2020;34:101669. doi:10.1016/j.tmaid.2020.101669
6. Khasawneh AI, Humeidan AA, Alsulaiman JW, et al. Medical Students and COVID-19: knowledge, attitudes, and precautionary measures. A Descriptive Study from Jordan. Front Public Health. 2020;8:253. doi:10.3389/fpubh.2020.00253
7. Chandra S, Laoteppitaks C, Mingioni N, Papanagnou D. Zooming-out COVID-19: virtual clinical experiences in an emergency medicine clerkship. Med Educ. 2020;54(12):1182–1183. doi:10.1111/medu.14266
8. Yerby J, Floyd KS. An Investigation of Traditional Education vs Fully-Online Education in Information technology; 2013.
9. Khalil R, Mansour AE, Fadda WA, et al. The sudden transition to synchronized online learning during the COVID-19 pandemic in Saudi Arabia: a qualitative study exploring medical students’ perspectives. BMC Med Educ. 2020;20(1):285. doi:10.1186/s12909-020-02208-z
10. Behzadi Z, Ghaffari A. Characteristics of online education and traditional education. Life Sci J. 2011;8:54–58.
11. Paul J, Jefferson F. A comparative analysis of student performance in an online vs face-to-face environmental science course from 2009 to 2016. Front Comput Sci. 2019;1. doi:10.3389/fcomp.2019.00007
12. Hakami Z. Comparison between virtual and traditional learning methods for orthodontic knowledge and skills in dental students: a Quasi-Experimental Study. Healthcare. 2021;9:9.
13. Petretto DR, Carta SM, Cataudella S, et al. The use of distance learning and E-learning in students with learning disabilities: a review on the effects and some hint of analysis on the use during COVID-19 outbreak. Clin Pract Epidemiol Ment Health. 2021;17:92–102. doi:10.2174/1745017902117010092
14. Li S, Zhang C, Liu Q, Tong K. E-learning during COVID-19: perspectives and experiences of the faculty and students. BMC Med Educ. 2022;22(1):328. doi:10.1186/s12909-022-03383-x
15. Govindaraju V. A review of social cognitive theory from the perspective of interpersonal communication. Multicult Educ. 2021;7:12.
16. Camargo CP, Tempski PZ, Busnardo FF, Martins MA, Gemperli R. Online learning and COVID-19: a meta-synthesis analysis. Clinics. 2020;75:e2286. doi:10.6061/clinics/2020/e2286
17. Garris CP, Fleck B. Student evaluations of transitioned-online courses during the COVID-19 pandemic. Scholarsh Teach Learn Psychol. 2020;8(2):119–139.
18. Alsoufi A, Alsuyihili A, Msherghi A, et al. Impact of the COVID-19 pandemic on medical education: medical students’ knowledge, attitudes, and practices regarding electronic learning. PLoS One. 2020;15(11):e0242905. doi:10.1371/journal.pone.0242905
19. Cicha K, Rizun M, Rutecka P, Strzelecki A. COVID-19 and higher education: first-year students’ expectations toward distance learning. Sustainability. 2021;13(4):1889. doi:10.3390/su13041889
20. Burns D, Dagnall N, Holt M. Assessing the impact of the COVID-19 pandemic on student wellbeing at universities in the United Kingdom: a conceptual analysis. Front Educ; 2020. doi: 10.3389/feduc.2020.582882
21. Al Rawashdeh AZ, Mohammed EY, Al Arab AR, Alara M, Al-Rawashdeh B, Al-Rawashdeh B. Advantages and disadvantages of using e-learning in university education: analyzing students’ perspectives. Electron J e-Learn. 2021;19(3):107–117. doi:10.34190/ejel.19.3.2168
22. Goldenberg MN, Hersh DC, Wilkins KM, Schwartz ML. Suspending medical student clerkships due to COVID-19. Medical Sci Educ. 2020;30(3):1273–1276. doi:10.1007/s40670-020-00994-1
23. Alqahtani AY, Rajkhan AA. E-learning critical success factors during the covid-19 pandemic: a comprehensive analysis of e-learning managerial perspectives. Educ Sci. 2020;10(9):216. doi:10.3390/educsci10090216
24. Turnbull D, Chugh R, Luck J. Transitioning to E-Learning during the COVID-19 pandemic: how have Higher Education Institutions responded to the challenge? Educ Inf Technol. 2021;26(5):6401–6419. doi:10.1007/s10639-021-10633-w
25. Almaiah MA, Al-Khasawneh A, Althunibat A. Exploring the critical challenges and factors influencing the E-learning system usage during COVID-19 pandemic. Educ Inf Technol. 2020;25(6):5261–5280. doi:10.1007/s10639-020-10219-y
26. Choi B, Jegatheeswaran L, Minocha A, Alhilani M, Nakhoul M, Mutengesa E. The impact of the COVID-19 pandemic on final year medical students in the United Kingdom: a national survey. BMC Med Educ. 2020;20(1):206. doi:10.1186/s12909-020-02117-1
27. Dost S, Hossain A, Shehab M, Abdelwahed A, Al-Nusair L. Perceptions of medical students towards online teaching during the COVID-19 pandemic: a national cross-sectional survey of 2721 UK medical students. BMJ Open. 2020;10(11):e042378. doi:10.1136/bmjopen-2020-042378
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
