Back to Journals » Risk Management and Healthcare Policy » Volume 15
Duration and Determinants of Delayed Diagnosis with Tuberculosis in Shenzhen, China: A Cross-Sectional Study
Authors Jiang Y , Luo L, Gui M, Liu L, Lin Y, Deng G , Chen J , Zhang P
Received 1 April 2022
Accepted for publication 17 July 2022
Published 29 July 2022 Volume 2022:15 Pages 1473—1481
DOI https://doi.org/10.2147/RMHP.S367998
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Jongwha Chang
Youli Jiang,1,* Lan Luo,2,3,* Min Gui,1 Linlin Liu,1 Yi Lin,2,3 Guofang Deng,2,3 Jingfang Chen,1,3 Peize Zhang2,3
1Hengyang Medical School, School of Nursing, University of South China, Hengyang, People’s Republic of China; 2Department of Pulmonary Medicine and Tuberculosis, The Third People’s Hospital of Shenzhen, Shenzhen, People’s Republic of China; 3National Clinical Research Center for Infectious Diseases, The Third People’s Hospital of Shenzhen, The Second Affiliated Hospital of Southern University of Science and Technology, Shenzhen, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Jingfang Chen; Peize Zhang, Email [email protected]; [email protected]
Background: Early diagnosis and timely treatment of tuberculosis are critical for disease control and management. However, diagnostic delay remains severe around the world. We aim to evaluate the duration and factors associated with diagnostic delay of tuberculosis in Shenzhen, China.
Methods: We conducted a face-to-face interview to collect the whole care-seeking process of patients diagnosed with active TB in Shenzhen, China, from April 1 to September 30, 2021. The duration from symptom onset to confirmed diagnosis was recorded. The risk factors of diagnostic delay were identified by binary stepwise logistic regression analysis.
Results: Among 288 confirmed TB cases, 170 (59.0%) were delayed diagnosis. The median diagnostic delay was 39.5 days. Median patient delay was 23 days and health system delay was 7 days. Income ≤ 315USD/month (OR = 2.97 [95% CI: 1.15– 7.69]), cough (OR = 3.00 [95% CI: 1.16– 7.76]), weight loss (OR = 15.59 [95% CI: 1.85– 131.56]), use of traditional Chinese Medicine (OR = 5.03 [95% CI: 1.04– 24.31]) and over-the-counter cough syrup (OR = 2.73 [95% CI: 1.10– 6.76]) were significant risk factors for patient delay. Fever (OR = 0.13[95% CI: 0.04– 0.48]) and hemoptysis (OR = 0.06 [95% CI0.01– 0.30]) were protective factors for patient delay. Cough (OR = 2.85 [95% CI: 1.49– 5.49]) and availability of chest X-ray (OR = 0.21[CI: 0.11– 0.39]) were factors associated with health system delay.
Conclusion: Delayed diagnosis of tuberculosis remains an unresolved problem. Patients with low income, self-treatment with over-the-counter medicine and accepting TCM suffered from a higher risk of patient delay. It is important to give more help to the vulnerable people and strengthen tuberculosis knowledge among primary health providers. Keeping all health providers alert to TB symptoms can facilitate earlier TB diagnosis and better disease control.
Keywords: tuberculosis, diagnosis, delay, patient delay, health system delay
Introduction
Tuberculosis (TB) is one of the top ten causes of death and is the leading cause of death from a single infectious disease worldwide.1 In 2019, the number of TB infections was estimated at 10 million, but the registered number of TB patients was only 7.1 million.1 With increased global attention and the adoption of efficient diagnostic assays during the past decades, the gap between the estimated number of TB cases and the number of diagnosed patients has narrowed.2
The End TB Strategy launched by the World Health Organization (WHO) advocates the importance of early diagnosis in TB control.3 Anti-TB-treatment initiated on time not only helps to cure the disease and reduce treatment costs but also prevents the spread of mycobacterium tuberculosis in the community4.
Despite enormous efforts being devoted to tackling TB around the world, delayed diagnosis remains a common public health problem, especially in countries with high TB burden.5 Previous studies have described the problem as having varying severity of diagnostic delays across different countries. The median total delay is 24 days in India, 62 days in Indonesia and 49 days in Cambodia.6–8 Many factors are associated with inability to diagnose TB in a timely way. Early screening using chest X-ray for cough patients can help to reduce TB diagnostic delays, and the availability of mycobacterium tuberculosis testing equipment can also benefit.9,10 Targeted measures can be effective in reducing the diagnostic delay.
Our study aims to assess the duration of TB symptoms onset for confirmed diagnosis of TB, as well as to identify independent factors influencing diagnostic delay in TB patients in Shenzhen, China. We expect that the findings of this study will help to improve Shenzhen’s TB screening program for early disease detection and management.
Method
Study Design
In order to assess the diagnostic delay and all possible influencing factors, we compiled a questionnaire of TB diagnostic delay. The initial version of the questionnaire was designed by a team of dedicated investigators, four clinical experts and a questionnaire framework expert in March 2021. Then, to determine the feasibility of the questionnaire, we conducted a pre-survey. The final version of the questionnaire was refined based on the results of patients’ feedback. We then conducted face-to-face interviews at patients’ bedside and assisted them in filling out the questionnaire via a mobile survey app named “Wen Juan Xing”. All data access on the website will be controlled by a unique login and password. Only designated researchers can log into the account for data management and record information throughout the study.
All participants provided written consent to take part in this study. Written informed consent of patients younger than age of 18 were signed by their parents or legal guardians. This study was approved by The Ethics Committee of The Third People’s hospital for the National Key Project for Disease. The hospital undertakes that, in using these statistics, no personal information of any patients was involved. It also complies with the Declaration of Helsinki in regard to confidentiality and ethical standards.
Study Population
We included patients with newly diagnosed pulmonary TB who were being treated at The Third People’s Hospital of Shenzhen between April 1 to September 30, 2020. During this period, a total of 293 hospitalized patients were enrolled. Five questionnaires were considered invalid due to patients provided erroneous dates, rendering an efficiency of 98.29%.
Key Definitions
The key definitions in this study are according to the WHO’s guidelines on detection of TB11 and the strategic framework of tuberculosis control and prevention.12 Total diagnostic delay is defined as the total time (days) from symptoms onset to confirmed diagnosis. Diagnostic delay was broadly divided into patient delay and health system delay. Patient delay (healthcare-seeking delay) was mainly caused by patients and was defined as >2 weeks from TB symptoms onset to the first visit to a professional healthcare provider. Health system delay is defined as >2 weeks from the first consultation in a facility that has TB screening capabilities (such as Chest X-ray) to TB confirmation.
Data Collection
Our study collected information on demographic characteristics (sex, age, education level, marital status, monthly income, etc.) and medical history (patient’s underlying disease, primary symptoms, substance abuse, first consultation facility, and whether TB-related tests were taken at the first visit, etc.). In addition, the survey also covered questions on individuals’ disease awareness and their healthcare-seeking behaviors.
Statistical Analysis
SPSS version 25 was used for statistical analysis. The key results were the proportion of patient delay and health system delay. First, we performed descriptive analysis on patient characteristics and clinical data, reporting numerical variables as means and standard deviations (SDs), median and Inter Quartile Range (IQR). Categorical variables were presented as frequencies and percentages. Then, the chi-square (χ2) test was employed to compare categorical variables. To analyze the potential influenced factors of patient delay and health system delay, univariate logistic regression analysis was done and the variables with the χ2 test of findings P< 0.1 were retained to avoid the loss of possible factors. Statistically significant results of univariate analysis were subjected to binary stepwise logistic regression analysis, and all results were two-tailed, with p< 0.05 considered statistically significant.
Result
Sociodemographic and Clinical Characteristics
The average age of 288 patients was 40.7 years, with 56.9% (n = 164) being male. Married folks accounted for 57.6% (n = 166). The patients’ highest level of education was junior high school (81.6%). 47.9% (n = 138) of the patients were manual worker. 72.2% (n = 209) of patients earned more than 315USD/month. The majority of patients (94.4%) had health insurance and 79.9% (n = 230) of them were long-term residents in Shenzhen. The main symptom at disease onset was coughing (49.7%). 62.2% (n = 174) patients had another underlying disease. 22.2% (n = 37) patients ignored their symptoms and did not seek further medical care. 49.3% (n = 142) patients visited pharmacies or other primary healthcare providers. Self-medication was obtained by 60.8% (n = 175) of the patients (Traditional Chinese medicine n = 63, antibiotics n = 113 and over-the-counter cough syrup n = 118). 19.4% patients did not get a chest X-ray examination on their first medical visit. In addition, 92.7% (n = 267) patients were lacking the knowledge of TB and were unaware they may have contracted the disease (Tables 1 and 2).
 |
Table 1 Demographic and Clinical Characteristics of Participants and Mean Duration of Diagnostic Delay in Tuberculosis in Shenzhen |
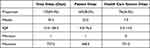 |
Table 2 Duration of Diagnosis Delay |
Patient Delay and Health System Delay
Among the 288 participants, patient delay was reported in 58.0% (n = 167) of TB patients, with a median of 23 days (IQR: 4–76). In comparison, delays caused by care providers showed a relatively lower ratio (24.3%, n = 70) and the medians were 7 days (IQR: 3–14). The total proportion of diagnostic delay was 59.0% (n = 170) with a median of 39.5 days (IQR: 13.5–106.5) (Table 2).
Factors Associated with Patient Delay and Health System Delay
Gender, employment status, income, marital status, primary symptoms, underlying disease, venue for first consultation, means of self-medication and consultation method were identified as factors that had lengthened patient delay via univariate analysis; and income, primary symptoms, self-medication and availability of a chest X-ray on first medical consultation were associated with healthcare system delay (Table 1).
Results from multivariate stepwise regression analysis indicated that income ≤315USD/ month (OR = 2.97 [95% CI: 1.15–7.69]), cough (OR = 3.00 [95% CI: 1.16–7.76]), weight loss (OR = 15.59 [95% CI: 1.85–131.56]), fever (OR = 0.13[95% CI: 0.04–0.48]), hemoptysis (OR = 0.06 [95% CI: 0.01–0.30]), usage of traditional Chinese medicine (OR = 5.03 [95% CI: 1.04–24.31]) and over-the-counter cough syrup (OR = 2.73 [95% CI: 1.10–6.76]) were associated with a higher risk of patient delay. On the other hand, cough (OR = 2.85[95% CI: 1.49–5.49]) increased the risk of health system delay. Availability of a chest X-ray (OR = 0.21[95% CI: 0.11–0.39]) was a protective factor of health system delay (Table 3).
 |
Table 3 Effect Factors of Patient and Healthcare System Delay by Binary Stepwise Logistic Regression Analysis |
Discussion
Our study found that diagnostic delay is a common problem among TB patients. The patient delay was more severe than the system delay. Patient delay was influenced by income level, TB symptoms, use of traditional Chinese medicine, antibiotic and over-the-counter cough syrup. Early receiving a chest x-ray in a professional clinic or hospital was an important factor in protecting patients from delayed diagnosis.
We demonstrated that a large number of TB patients spent a lengthy period of time from symptoms onset to final care-seeking in a professional medical unit. The proportion of patient delay in our study is 58%, which is quite higher than other parts of China. It had been reported that patients delay was 40.% in Shandong Province and 21.54% in Hubei province.13,14 As for the duration of patient delays, we found that median days of patient delay was 23 days in our study, which is close to 28 days reported by a recent systematic review of other Asian and African countries.15 However, the median delay of the health care system was only 7 days in our study, which was much shorter than 12–34 days of health system delay in low- to middle-income countries found in a meta-analysis.16 A recent study from Ethiopia also reported a 20.5-day delay in health system delay.22 We supposed that our healthcare system responds quickly when taking care of patients. This may contribute to the availability of diagnostic assays, better facilities, higher accessibility and a well-structured health care system. Furthermore, after the COVID-19 outbreak, many doctors are alert to respiratory symptoms.
Many studies reported that low-income was associated with longer patient delay.17,18 Medical care affordability is limited for most low-income individuals, leading to delayed visit to health care institutions. Our study also demonstrated that patients with incomes ≤315 USD/month were associated with longer healthcare seeking delays. These economically fragile persons were forced to self-treat with drugs purchased from pharmacies or TCM practitioners rather than going directly to a hospital for help. These might lead to further exacerbation of the tuberculosis.19 When tackling an infectious disease associated with poverty, we should pay more attention to economically vulnerable people for better disease control.
In our study, we found that almost none of the patients related chronic cough and weight loss to TB. Chronic cough and weight loss were independent factors associated with patient delays. The probability of patient delay is approximately 12 times higher in patients who had a cough as their initial symptom. As a common respiratory symptom, many patients overlooked the seriousness of chronic cough until it progressed to severe coughing or hemoptysis.20 Weight loss is another independent risk factor that may easily be neglected by patients. A cross-sectional study of Uzbekistan demonstrated that weight loss as an early symptom was associated with a longer time to reach the health care system.21
According to our findings, 60.8% of the patients (n = 175) used self-medication before visiting a professional healthcare institution, such as Traditional Chinese Medicine (TCM), antibiotics and over-the-counter cough syrup. Self-treatment was associated with longer patient delay.22 Consultation with traditional medicine providers may also cause a delay in TB diagnosis.23 The majority of the TCM clinics and pharmacies in China are privately owned and do not possess the necessary diagnostic devices for TB. No herbal medicine had been proved to be bactericidal activity for TB until now. Many patients take TCM or over-the-counter medicine for a period of time for symptom relief. They only visited the hospital when symptoms recurred or worsened.
There is no doubt that chest X-ray is an important examination for screening TB in those who have respiratory symptoms.24 Our findings indicated that receiving a chest X-ray during the initial care seeking was a protective factor in avoiding healthcare system delay. We found that when a chest X-ray is unavailable, it would take up to 46.5 days to confirm TB diagnosis. This is consistent with the previous study that patients who took a chest X-ray had a shorter diagnosis delay.25 However, many primary medical care centers and clinics in Shenzhen do not have chest X-ray equipment. Some private practitioners are unaware of TB symptoms. When they take care of patients with respiratory symptoms, they only considered bacterial infection or allergic reaction and prescribed antibiotics, antihistamines or antitussives. Some patients’ symptom might relieve slightly or persist for a long time before TB getting worsened.26,27 TB associated knowledge should be strengthened among private practitioners and staff in drug stores so that they can refer patients with suspected respiratory symptoms in time for further examination by a specialist.
There are several limitations of this study. Firstly, the subjects in this study were only selected from the Third People’s Hospital of Shenzhen. The results were possibly limited by the geographical area. It can only represent the current situation of in China’s big cities. Secondly, following the outbreak of COVID-19 in China, people might be cautious in care seeking or might be quarantined to limit access to hospitals. These could be some confounding factors of diagnosis delay in our study. Thirdly, we did not include patients with negative sputum culture results from our investigation. The delayed diagnosis in TB patients without bacterial evidence is still uncertain.
Conclusion
In summary, diagnostic delay remains an unresolved problem in Shenzhen. Patients with fragile economic, self-treatment with over-the-counter medicine and TCM before seeking professional care suffered from a higher risk of patient delay. Propaganda on TB associated knowledge, preventive measures in citizens and primary care units, and appropriate guidance to designated healthcare providers for TB screening should be enhanced to reduce care-seeking time. Keeping all health providers alert to TB could contribute to earlier TB diagnosis and better disease control.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from Jingfang Chen ([email protected]) and Youli Jiang ([email protected]) on reasonable request.
Acknowledgment
A special thanks to the study participants for their contribution to the research.
Funding
This study was supported by a grant from Guangdong Provincial Clinical Research Center for Infectious Diseases (tuberculosis) (No.2020B1111170014) and Summit Plan for Foshan High-level Hospital Construction (No. FSSYKF-2020001).
Disclosure
The authors have no competing interests to declare.
References
1. World Health organization. Global Tuberculosis Report 2020. Geneva: WorldHealth organization; 2020.
2. World Health organization. Global Tuberculosis Report 2021. Geneva: WorldHealth organization; 2021.
3. World Health Organization. Gear up to end TB: introducing the end TB strategy. World Health Organization; 2015. Available from: https://apps.who.int/iris/handle/10665/156394.
4. Marks GB, Nguyen NV, Nguyen PTB, et al. Community-wide screening for tuberculosis in a high-prevalence setting. N Engl J Med. 2019;381(14):1347–1357. doi:10.1056/NEJMoa1902129
5. Kim J, Keshavjee S, Atun R. Health systems performance in managing tuberculosis: analysis of tuberculosis care cascades among high-burden and non-high-burden countries. J Glob Health. 2019;9(1):010423. doi:10.7189/jogh.09.010423
6. Basa S, Venkatesh S. Patient and healthcare system delays in the start of pulmonary tuberculosis treatment among tribal patients registered under DOTS, Odisha. J Clin Diagn Res. 2016;10(9):LC21–LC24. doi:10.7860/JCDR/2016/20136.8567
7. Lestari BW, McAllister S, Hadisoemarto PF, et al. Patient pathways and delays to diagnosis and treatment of tuberculosis in an urban setting in Indonesia. Lancet Reg Health West Pac. 2020;5:100059. doi:10.1016/j.lanwpc.2020.100059
8. Teo AKJ, Ork C, Eng S, et al. Determinants of delayed diagnosis and treatment of tuberculosis in Cambodia: a mixed-methods study. Infect Dis Poverty. 2020;9(1):49. doi:10.1186/s40249-020-00665-8
9. Mohammed H, Oljira L, Teji Roba K, et al. Who to involve and where to start integrating tuberculosis screening into routine healthcare services: positive cough of any duration as the first step for screening tuberculosis in Ethiopia. Risk Manag Healthc Policy. 2021;14:4749–4756. doi:10.2147/RMHP.S337392
10. Mohammed H, Oljira L, Roba KT, et al. Impact of early chest radiography on delay in pulmonary tuberculosis case notification in Ethiopia. Int J Mycobacteriol. 2021;10(4):364–372. doi:10.4103/ijmy.ijmy_216_21
11. World Health Organization. Early detection of tuberculosis: an overview of approaches, guidelines and tools; 2011.
12. Li J, Chung PH, Leung CLK, et al. The strategic framework of tuberculosis control and prevention in the elderly: a scoping review towards End TB targets. Infect Dis Poverty. 2017;6(1):70. doi:10.1186/s40249-017-0284-4
13. Yang Q, Tong Y, Yin X, et al. Delays in care seeking, diagnosis and treatment of patients with pulmonary tuberculosis in Hubei, China. Int Health. 2020;12(2):101–106. doi:10.1093/inthealth/ihz036
14. Tobe RG, Xu L, Zhou C, et al. Factors affecting patient delay of diagnosis and completion of Direct Observation Therapy, Short-course (DOTS) among the migrant population in Shandong, China. Biosci Trends. 2013;7(3):122–128.
15. Getnet F, Demissie M, Assefa N, et al. Delay in diagnosis of pulmonary tuberculosis in low-and middle-income settings: systematic review and meta-analysis. BMC Pulm Med. 2017;17(1):202. doi:10.1186/s12890-017-0551-y
16. Butsorn A, Suggaravetsiri P, Tesama N, et al. Delay of treatment among new smear-positive pulmonary tuberculosis patients in Thai-Cambodia border: cases study in Surin and Sisaket Province, Thailand. Res J Med Sci. 2010;4:340–345. doi:10.3923/rjmsci.2010.340.345
17. Cai J, Wang X, Ma A, et al. Factors associated with patient and provider delays for tuberculosis diagnosis and treatment in Asia: a systematic review and meta-analysis. PLoS One. 2015;10(3):e0120088. doi:10.1371/journal.pone.0120088
18. Zhang T, Tang S, Jun G, et al. Persistent problems of access to appropriate, affordable TB services in rural China: experiences of different socio-economic groups. BMC Public Health. 2007;7. doi:10.1186/1471-2458-7-19
19. Ayisi JG, Van’t Hoog AH, Agaya JA, et al. Care seeking and attitudes towards treatment compliance by newly enrolled tuberculosis patients in the district treatment programme in rural western Kenya: a qualitative study. BMC Public Health. 2011;11:515. doi:10.1186/1471-2458-11-515
20. Makwakwa L, Sheu M, Chiang C, et al. Patient and health system delays in the diagnosis and treatment of new and retreatment pulmonary tuberculosis cases in Malawi. BMC Infect Dis. 2014;14:132. doi:10.1186/1471-2334-14-132
21. Belkina TV, Khojiev DS, Tillyashaykhov MN, et al. Delay in the diagnosis and treatment of pulmonary tuberculosis in Uzbekistan: a cross-sectional study. BMC Infect Dis. 2014;14:624. doi:10.1186/s12879-014-0624-y
22. Rabin AS, Kuchukhidze G, Sanikidze E, et al. Prescribed and self-medication use increase delays in diagnosis of tuberculosis in the country of Georgia. Int J Tuberc Lung Dis. 2013;17(2):214–220. doi:10.5588/ijtld.12.0395
23. Li Y, Ehiri J, Tang S, et al. Factors associated with patient, and diagnostic delays in Chinese TB patients: a systematic review and meta-analysis. BMC Med. 2013;11. doi:10.1186/1741-7015-11-156
24. Kim JH, Kim ES, Jun KI, et al. Delayed diagnosis of extrapulmonary tuberculosis presenting as fever of unknown origin in an intermediate-burden country. BMC Infect Dis. 2018;18(1):426. doi:10.1186/s12879-018-3349-5
25. Auer C, Kiefer S, Zuske M, et al. Health-seeking behaviour and treatment delay in patients with pulmonary tuberculosis in Switzerland: some slip through the net. Swiss Med Wkly. 2018;148:w14659. doi:10.4414/smw.2018.14659
26. Daniels B, Dolinger A, Bedoya G, et al. Use of standardised patients to assess quality of healthcare in Nairobi, Kenya: a pilot, cross-sectional study with international comparisons. BMJ Glob Health. 2017;2(2):e000333. doi:10.1136/bmjgh-2017-000333
27. Sylvia S, Xue H, Zhou C, et al. Tuberculosis detection and the challenges of integrated care in rural China: a cross-sectional standardized patient study. PLoS Med. 2017;14(10):e1002405. doi:10.1371/journal.pmed.1002405
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
