Back to Journals » Journal of Multidisciplinary Healthcare » Volume 15
A Prediction Model for Rapid Identification of Ischemic Stroke: Application of Serum Soluble Corin
Authors Lu Y, Wang W, Tang Z, Chen L , Zhang M , Zhang Q, Wu L, Jiang J, Zhang X , He C, Peng H
Received 2 November 2022
Accepted for publication 12 December 2022
Published 22 December 2022 Volume 2022:15 Pages 2933—2943
DOI https://doi.org/10.2147/JMDH.S395896
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Ying Lu,1,* Weiqi Wang,1,* Zijie Tang,1 Linan Chen,1 Min Zhang,2 Qiu Zhang,3 Lei Wu,4 Jun Jiang,5 Xiaolong Zhang,5 Chuan He,1 Hao Peng1,5,6
1Department of Epidemiology, School of Public Health, Medical College of Soochow University, Suzhou, People’s Republic of China; 2Department of Central Office, Suzhou National New and Hi-tech Industrial Development Zone Center for Disease Control and Prevention, Suzhou, People’s Republic of China; 3Department of Chronic Disease, Gusu Center for Disease Control and Prevention, Suzhou, People’s Republic of China; 4Department of Maternal and Child Health, Suzhou Industrial Park Center for Disease Control and Prevention, Suzhou, People’s Republic of China; 5Department of Tuberculosis Control, Suzhou Center for Disease Control and Prevention, Suzhou, People’s Republic of China; 6Jiangsu Key Laboratory of Preventive and Translational Medicine for Geriatric Diseases, Soochow University, Suzhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Hao Peng; Chuan He, Department of Epidemiology, School of Public Health, Medical College of Soochow University, 199 Renai Road, Industrial Park District, Suzhou, 215123, People’s Republic of China, Tel +86 512 6588 0079, Email [email protected]; [email protected]
Objective: Rapid identification is critical for ischemic stroke due to the very narrow therapeutic time window. The objective of this study was to construct a diagnostic model for the rapid identification of ischemic stroke.
Methods: A mixture population constituted of patients with ischemic stroke (n = 481), patients with hemorrhagic stroke (n = 116), and healthy individuals from communities (n = 2498) were randomly resampled into training (n = 1547, mean age: 55 years, 44% males) and testing (n = 1548, mean age: 54 years, 43% males) samples. Serum corin was assayed using commercial ELISA kits. Potential risk factors including age, sex, education level, cigarette smoking, alcohol consumption, obesity, blood pressure, lipids, glucose, and medical history were obtained as candidate predictors. The diagnostic model of ischemic stroke was developed using a backward stepwise logistic regression model in the training sample and validated in the testing sample.
Results: The final diagnostic model included age, sex, cigarette smoking, family history of stroke, history of hypertension, systolic blood pressure, total cholesterol, high-density lipoprotein cholesterol, fasting glucose, and serum corin. The diagnostic model exhibited good discrimination in both training (AUC: 0.910, 95% CI: 0.884– 0.936) and testing (AUC: 0.907, 95% CI: 0.881– 0.934) samples. Calibration curves showed good concordance between the observed and predicted probability of ischemic stroke in both samples (all P> 0.05).
Conclusion: We developed a simple diagnostic model with routinely available variables to assist rapid identification of ischemic stroke. The effectiveness and efficiency of this model warranted further investigation.
Keywords: ischemic stroke, serum corin, biomarker, prediction model
Introduction
Stroke, the leading cause of long-term disability and mortality, can result in a rapid loss of neurological function due to disturbance of blood supply to the brain.1 It is a heterogeneous disorder with two major subtypes – ischemic and hemorrhagic stroke, with fundamentally different pathogenesis and thus needs different treatment strategies.2 Proper medical treatment of stroke relies on accurate and rapid differentiation between ischemic and hemorrhagic stroke due to a narrow therapeutic time window for the former. Currently, neuroimaging remains the gold standard to distinguish the two subtypes, but it is limited temporally3 and may thereby lead to missing treatment golden time for stroke, the ischemic subtype in particular. Many efforts have been made to improve the differential diagnosis of ischemic stroke at a very early occurrence. For example, many candidate biomarkers in blood and cerebrospinal fluid have been identified as potential diagnostic markers, such as Glial protein (S100β),4 glial fibrillary acidic protein (GFAP),5 matrix metalloproteinase-9 (MMP-9),6 ubiquitin C-terminal hydrolase-L1 (UCH-L1), nucleoside diphosphate kinase A (NDKA), C-reactive protein (CRP)7 and myelin basic protein (MBP).8 However, none of them achieved sufficient discrimination in clinical settings. In addition, several prediction scores have been developed aiming to clinically differentiate ischemic stroke from stroke patients, such as the Guy’s Hospital score,9 the Siriraj score,10 and the score developed by Besson et al.11 These scores were not sufficient enough to initiate thrombolytic therapy for ischemic stroke without further diagnostics to rule out hemorrhage.12,13 Recently, our group found that serum corin was significantly decreased in patients with stroke and further lower in those with hemorrhagic stroke, compared to healthy controls.14 Corin is a physiological convertase of atrial natriuretic peptide,15 and its circulating levels have also been associated with other cardiovascular disorders, eg, hypertension,16 heart failure,17 and coronary syndrome.18 Circulating corin appears to participate in stroke development and may therefore possess a potential for risk prediction and prognostic assessment of stroke.19 However, no study has examined the effect of circulating corin on the differentiation of stroke subtypes. Here, we aimed to develop a diagnostic model incorporating serum corin with conventional risk factors for differentiation between ischemic and hemorrhagic stroke subtypes. This model could be applied as assistance in the differential diagnosis of ischemic stroke and speed up the initiation of thrombolysis, for patients whose therapeutic window is going to past in particular.
Methods
Participants
As illustrated in Figure 1, this study included a mixture population constituted of patients with ischemic stroke (n = 481), patients with hemorrhagic stroke (n = 116), and healthy controls from communities (n = 2498). The detailed methods of study participants’ recruitment have been described previously.14 In brief, a total of 597 patients with hospitalized first-ever stroke were consecutively recruited from January to May 2014. The inclusion criteria were as follows: (1) age ≥22 years; (2) stroke onset within 48 hours confirmed by imaging; (3) willing to sign informed consent by patients or their direct family members. Patients with one of the following were excluded: (1) recurrent stroke; (2) current pregnancy; (3) unable to participate in the follow-up examination. Stroke including ischemic and hemorrhagic subtypes was diagnosed by a trained neurologist and confirmed by brain computed tomography (CT) or magnetic resonance imaging (MRI) scan. A total of 2498 healthy controls who never had cardiovascular diseases were selected from the Gusu cohort study,16 a community-based prospective study including Chinese Han adults in Suzhou city. The study protocols were approved by the Ethics Committee of Soochow University. All participants provided written informed consent. Our study complies with the Declaration of Helsinki.
Measurement of Serum Soluble Corin
As detailed previously,14 levels of serum soluble corin were quantified in the Central Laboratory of the School of Public Health at Soochow University by trained staff who were blind to the clinical characteristics of the study participants, using commercial ELISA kits (R&D Systems, Inc., Minneapolis, USA). All the samples were processed in a duplicate assay. Intra- and inter-assay coefficients of variation were less than 2.7% and 6.3%, respectively.
Collection of Conventional Risk Factors
The methods of data collection of conventional risk factors of stroke have been described in our previous study.14 Briefly, information on demographic characteristics (age and sex), lifestyle risk factors (cigarette smoking and alcohol consumption), metabolic risk factors (obesity, diabetes, dyslipidemia, and hypertension), and medical history was obtained using a structured questionnaire administered by trained staff. Three consecutive blood pressure measurements were measured by trained staff according to a common protocol recommended by the American Heart Association.20 Blood pressure was measured with the participant in a supine or sitting position using a standard mercury sphygmomanometer and appropriate cuff size. The means of the three measurements were recorded as systolic blood pressure (SBP) and diastolic blood pressure (DBP), respectively. Fasting plasma glucose, total cholesterol, triglycerides, low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), and serum uric acid were assayed using commercial reagents.
Statistical Analysis
Data were analyzed using R statistical software (version 4.1.3). As shown in Figure 1, we randomly divided the mixture population into training and testing samples for model development and validation, respectively. The clinical characteristics of study participants were presented according to the two samples.
Model Development
To derive the diagnostic model for the identification of ischemic stroke, we first developed the diagnostic model in the training sample. Easily available conventional risk factors such as age, sex, cigarette smoking, alcohol consumption, family history of stroke, hypertension, diabetes mellitus, SBP, DBP, total cholesterol, triacylglycerol, HDL-C, LDL-C, fasting plasma glucose, and serum uric acid were considered candidate predictors. Of them, a univariable logistic regression model with ischemic stroke as the dependent variable was constructed to select predictors. Variables showing a significant univariable association (P<0.05) were included to fit a multivariable logistic regression model, and backward stepwise selection was applied to select final predictors. Together with serum corin, the selected predictors were used to develop the final prediction model by constructing a multivariable logistic regression model. Serum corin was forced into the model fitting because it was a predictor for stroke independent of conventional risk factors in our previous study.21 To ease the clinical application of the final prediction model, a nomogram was developed using the R package “rms” to determine the predicted probability of being ischemic stroke.
Model Validation
To estimate the performance of the diagnostic model developed in the training sample, discrimination, calibration, and utility of the model were assessed in the testing sample. In specific, the receiver operating characteristic (ROC) curve was drawn with the R package “pROC” to evaluate the discrimination. Calibration curve analysis was applied by plotting the observed probability against the predicted probability to evaluate the calibration. Decision curve analysis (DCA) was conducted with the R package “rmda” to determine the clinical practicability of the prediction model based on the net benefit under different threshold probabilities. These model assessments were also conducted in the testing sample.
Evaluation of the Diagnostic Test
We first determined the cut-off value of the predicted probability by the ROC curve, followed by evaluations of its validity and predictive value. Sensitivity, specificity, Youden’s index, and likelihood ratio were used to assess the validity. Positive and negative predictive values were estimated based on the sensitivity, specificity, and prevalence of ischemic stroke in China.22
Results
Characteristics of Study Participants
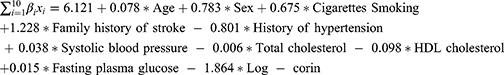
A total of 1547 participants in the training sample (mean age: 55 years, 44% men) and 1548 participants in the testing sample (mean age: 54 years, 43% men) were included in the current study. Their clinical characteristics are presented in Table 1. Most variables were equally distributed, except for history of CHD (1.23% vs 2.45%), and levels of triglycerides (mean level: 1.55 vs 1.44) between the training and testing samples (all P<0.05).
 |
Table 1 Clinical Characteristics of Study Participants |
Development of the Diagnostic Model in the Training Sample
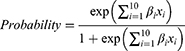
Univariable logistic regression found that age, sex, cigarette smoking, alcohol consumption, family history of stroke, history of hypertension, history of diabetes, SBP, total cholesterol, HDL-C, fasting plasma glucose, and serum uric acid were significantly associated with ischemic stroke (Supplementary Table S1). Of these variables, age, sex, cigarette smoking, family history of stroke, history of hypertension, SBP, total cholesterol, HDL-C, and fasting plasma glucose survived from the multivariable regression with backward stepwise selection. As expected, the prediction performance was significantly improved after adding log-corin, as indicated by the increased Nagelkerke’s R² (from 47.6% to 50.5%), area under the ROC curve (from 0.902 to 0.910, P=0.016) and decreased Akaike information criterion (from 626 to 601), Brier score (from 0.061 to 0.058). Therefore, ten predictors including age, sex, cigarette smoking, family history of stroke, history of hypertension, SBP, total cholesterol, HDL-C, fasting plasma glucose, and Log-corin were included in the final model (Table 2). The probability of the diagnostic model developed in the training sample was shown below:
 |
Table 2 The Final Diagnostic Model Developed in the Training Sample |
The area under the ROC curve for the diagnostic model was 0.910 (95% CI: 0.884–0.936), suggesting a good discriminatory capacity (Figure 2A). The calibration plots showed an almost perfect overlap between the observed and predicted probability of ischemic stroke (P=0.619), suggesting a good predictive accuracy of the diagnostic model (Figure 3A). The DCA curves showed that the prediction model could be applied clinically if the risk threshold was 1–79% (Figure 4A), suggesting a wide clinical application.
Validation of the Diagnostic Model in the Testing Sample
We further conducted an external validation of the diagnostic performance of the model developed in the training sample. The results showed that this diagnostic model also achieved a good discrimination, calibration, and clinical applicability in the testing sample, as suggested by an area under the ROC curve of 0.907 (95% CI: 881–0.934, Figure 2B), an overlap between the observed and predicted probability of ischemic stroke (P=0.157, Figure 3B), and a wide range of application between 2% and 70% of the risk of ischemic stroke determined by the DCA curves (Figure 4B), respectively.
Application and Evaluation of the Diagnostic Test
To ease the clinical application of the diagnostic model, we drew a nomogram that can be used to manually obtain predicted probability of ischemic stroke from the final diagnostic model (Figure 5). Supplementary Table S2 shows the validity and predictive value of the diagnostic test obtained from the final diagnostic model. The ROC curve analysis showed that the cut-off value of the diagnostic score was 0.190, with a sensitivity of 79.2% and a specificity of 90.4% in the training sample, with a sensitivity of 72.9% and a specificity of 90.1% in the testing sample as well. A higher diagnostic score over 0.190 indicates a higher probability of being ischemic stroke. This diagnostic test received an ideal Youden’s index, a large positive likelihood ratio and a small negative likelihood ratio in both samples, indicating that the diagnostic test could be reliable. The latest Global Burden of Disease Study showed that the prevalence of ischemic stroke in China was 1700/100,000 in 2019. Based on this prevalence, we estimated the predictive value of the diagnostic test. The positive and negative predictive values were 0.125 and 0.996 in the training sample and 0.113 and 0.995 in the testing sample.
 |
Figure 5 The nomogram for the probability of being ischemic stroke predicted by the diagnostic model. Abbreviations: HDL, high-density lipoprotein cholesterol; Log-corin, Log-transformed corin. |
Discussion
Leveraging a large mixture sample including patients with ischemic stroke, patients with hemorrhagic stroke, and healthy individuals, we constructed a simple-to-use diagnostic model to assist rapid identification of ischemic stroke. This diagnostic model can have immediate practical implications as routinely available variables can be easily obtained before admission. Therefore, this model could be used in predicting the risk of ischemic stroke for community members, applied as assistance in the differential diagnosis of ischemic stroke, and used in speeding up the initiation of thrombolysis for patients with neurological symptoms.
Several key risk factors have been established to account for ischemic stroke risk in previous studies. Age and male sex are robust non-modifiable risk factors and influence the epidemiology, pathophysiology, and treatment efficacy for ischemic stroke. The risk of ischemic stroke doubles every 10 years after the age of 55, and almost 75% of strokes occur in people aged >65 years.23,24 The male gender was a significantly stronger predictor of ischemic stroke since males have a higher prevalence of cardiovascular conditions such as higher blood pressure25 and stroke.26,27 The EPIC Potsdam Study28 indicated that almost 60% of ischemic stroke risk could be attributed to hypertension, hypercholesterolemia, and cigarette smoking. There is a strong dose–response relationship between the number of cigarettes smoked and the risk of ischemic stroke, cigarette smoking causes a twofold increase in the risk of ischemic stroke.29 Reducing blood pressure in individuals with hypertension is highly effective in preventing ischemic stroke.30 Family history of stroke, elevated fasting plasma glucose, and low cumulatively averaged HDL-C were associated with an increased IS risk.31–33 In line with previous studies, our study shows that these risk factors are independent risk factors for ischemic stroke. All variables in our final prediction model are related to patient demographics and laboratory measurements, enabling the prediction of ischemic stroke risk using only clinical data. This provides a simpler method for assistance in the clinical diagnosis of ischemic stroke.
Thrombolysis is currently recommended for IS patients within 4.5 hours of stroke onset. However, disappointingly, thrombolysis in patients with acute ischemic stroke is infrequent due to reasons such as high cost, not always being available, and possible contraindications. An alternative approach in acute stroke diagnosis is to identify stroke biomarkers that reflect the body’s response to the damage caused by the different types of stroke. Over 150 candidate biomarkers have been studied. For example, S100β,34 a glial protein, was one of the first molecules suggested as a candidate to aid the diagnosis of ischemic stroke, but its measurement had poor sensitivity.35 GFAP5 was the best candidate to date for differentiating hemorrhage and ischemic stroke. Controversially, it was previously reported that, when measured early (<1 h after stroke onset), serum GFAP did not distinguish hemorrhagic and ischemic stroke.36 The concentration of MMP-9 was reported to peak at 24 h post stroke,6 where the therapeutic window has been passed. Other markers include, but are not limited to, UCH-L1, NDKA, and CRP7 and MBP.8,37 Nevertheless, measurements of candidate biomarkers have usually occurred beyond the time window for thrombolysis and no individual candidate has proven to have adequate performance for use in an acute clinical setting where decisions about an individual patient are being made.38–40 More importantly, none of the biomarkers have entered routine clinical use. There are also several clinical scores to distinguish between hemorrhagic and ischemic stroke, such as the Guy’s Hospital score,9 the Siriraj score,10 and the score developed by Besson et al,11 but these scores are insufficient to initiate treatment for ischemic stroke without further diagnostics to rule out hemorrhage stroke.12 CT, the golden diagnostic method, is very popular now, especially in developed areas. The assistance diagnostic methods including markers and scores mentioned above seemed usefulness in clinical settings and not studied anymore. However, it is not very easy to transport patient timingly to stroke units in undeveloped areas, those with inconvenient traffic in particular. Therefore, we developed a diagnostic model that may help individuals in undeveloped areas.
Corin was thought to be a physiological activator of atrial natriuretic peptides,41 which correspond to the decreased natriuretic peptides in stroke. Its circulating levels have also been associated with other cardiovascular disorders, eg, hypertension, heart failure, and coronary syndrome. Studies have shown that the activity of corin on activation of ANP has been reduced in patients with heart failure17 and corin was associated with atrial fibrillation42 and heart failure.43 These disease states may therefore affect the association between serum corin and stroke. Recently, our group demonstrated that serum corin was significantly decreased in patients with stroke and further lower in those with hemorrhagic stroke, compared to healthy controls.16
Our study is not devoid of limitations. First, although we found that serum corin could predict future risk of ischemic stroke independently of conventional risk factors, including age, sex, cigarette smoking, family history of stroke, blood pressure, lipids, and glucose, serum corin just slightly (but not significantly) improved the prediction performance for ischemic stroke over these conventional risk factors. Second, the study was a case–control study only and a prospective study is needed to confirm the model. We also need to confirm the use of this model with other populations. Third, specific markers that are uniquely response to ischemic stroke are ideal markers for the construction of diagnostic model. However, such markers are rare. In our study, we developed a diagnostic model incorporating serum corin with conventional risk factors. Although these markers are not disease-specific, the performance of the diagnostic model is relatively acceptable.
In summary, we developed a simple diagnostic model with routinely available variables to assist rapid identification of ischemic stroke. The effectiveness and efficiency of this model warranted further investigation.
Abbreviations
AUC, area under the receiver-operating characteristic curve; CI, confidence interval; S100β, glial protein; GFAP, glial fibrillary acidic protein; MMP-9, matrix metalloproteinase-9; UCH-L1, ubiquitin C-terminal hydrolase-L1; NDKA, nucleoside diphosphate kinase A; CRP, C-reactive protein; MBP, myelin basic protein; CT, computed tomography; MRI, magnetic resonance imaging; SBP, systolic blood pressure; DBP, diastolic blood pressure; LDL-C, low-density lipoprotein cholesterol; HDL-C, high-density lipoprotein cholesterol; Log-corin, Log-transformed corin; ROC, receiver operating characteristic; CHD, coronary heart disease; DCA, decision curve analysis; IQR, interquartile range.
Acknowledgments
We gratefully acknowledge the cooperation and participation of the members of the Gusu cohort. We especially thank the clinical staff at all participating hospitals for their support and contribution to this project. Without their contribution, this research would not have been possible.
Funding
This study was supported by the National Natural Science Foundation of China (NO. 82173596, 81903384, and 81872690), the Soochow University Undergraduate Extracurricular Academic Research Program (KY20220120A), the Suzhou Municipal Science and Technology Bureau (NO. SYS2020091 and SKJY2021040), and a Project of the Priority Academic Program Development of Jiangsu Higher Education Institutions.
Disclosure
None of the authors have financial associations that might pose a conflict of interest in connection with the submitted article. The datasets used during the current study are available from the corresponding author on a reasonable request.
References
1. Lloyd-Jones D, Adams RJ, Brown TM, et al. Executive summary: heart disease and stroke statistics–2010 update: a report from the American heart association. Circulation. 2010;121:948–954. doi:10.1161/CIRCULATIONAHA.109.192666
2. Abdu H, Tadese F, Seyoum G, Milligan C. Comparison of ischemic and hemorrhagic stroke in the medical ward of Dessie referral hospital, northeast Ethiopia: a retrospective study. Neurol Res Int. 2021;2021:9996958. doi:10.1155/2021/9996958
3. Chalela JA, Kidwell CS, Nentwich LM, et al. Magnetic resonance imaging and computed tomography in emergency assessment of patients with suspected acute stroke: a prospective comparison. Lancet. 2007;369:293–298. doi:10.1016/S0140-6736(07)60151-2
4. Zhou S, Bao J, Wang Y, Pan S. S100β as a biomarker for differential diagnosis of intracerebral hemorrhage and ischemic stroke. Neurol Res. 2016;38:327–332. doi:10.1080/01616412.2016.1152675
5. Eng LF, Ghirnikar RS, Lee YL. Glial fibrillary acidic protein: gfap-thirty-one years (1969–2000). Neurochem Res. 2000;25:1439–1451. doi:10.1023/A:1007677003387
6. Ramos-Fernandez M, Bellolio MF, Stead LG. Matrix metalloproteinase-9 as a marker for acute ischemic stroke: a systematic review. J Stroke Cerebrovasc Dis. 2011;20:47–54. doi:10.1016/j.jstrokecerebrovasdis.2009.10.008
7. Hasan N, McColgan P, Bentley P, Edwards RJ, Sharma P. Towards the identification of blood biomarkers for acute stroke in humans: a comprehensive systematic review. Br J Clin Pharmacol. 2012;74:230–240. doi:10.1111/j.1365-2125.2012.04212.x
8. Matias-Guiu J, Martinez-Vazquez J, Ruibal A, Colomer R, Boada M, Codina A. Myelin basic protein and creatine kinase bb isoenzyme as csf markers of intracranial tumors and stroke. Acta Neurol Scand. 1986;73:461–465. doi:10.1111/j.1600-0404.1986.tb04585.x
9. Allen CM. Clinical diagnosis of the acute stroke syndrome. Q J Med. 1983;52:515–523.
10. Poungvarin N, Viriyavejakul A, Komontri C. Siriraj stroke score and validation study to distinguish supratentorial intracerebral haemorrhage from infarction. BMJ. 1991;302:1565–1567. doi:10.1136/bmj.302.6792.1565
11. Sandercock PA, Allen CM, Corston RN, Harrison MJ, Warlow CP. Clinical diagnosis of intracranial haemorrhage using guy’s hospital score. Br Med J. 1985;291:1675–1677. doi:10.1136/bmj.291.6510.1675
12. Bamford J. Clinical examination in diagnosis and subclassification of stroke. Lancet. 1992;339:400–402. doi:10.1016/0140-6736(92)90085-H
13. Weir CJ, Murray GD, Adams FG, Muir KW, Grosset DG, Lees KR. Poor accuracy of stroke scoring systems for differential clinical diagnosis of intracranial haemorrhage and infarction. Lancet. 1994;344(8928):999–1002. doi:10.1016/S0140-6736(94)91648-9
14. Peng H, Zhu F, Shi J, et al. Serum soluble corin is decreased in stroke. Stroke. 2015;46:1758–1763. doi:10.1161/STROKEAHA.114.008368
15. Yan W, Wu F, Morser J, Wu Q. Corin, a transmembrane cardiac serine protease, acts as a pro-atrial natriuretic peptide-converting enzyme. Proc Natl Acad Sci U S A. 2000;97:8525–8529. doi:10.1073/pnas.150149097
16. Peng H, Zhang Q, Cai X, et al. Association between high serum soluble corin and hypertension: a cross-sectional study in a general population of China. Am J Hypertens. 2015;28:1141–1149. doi:10.1093/ajh/hpv002
17. Ibebuogu UN, Gladysheva IP, Houng AK, Reed GL. Decompensated heart failure is associated with reduced corin levels and decreased cleavage of pro-atrial natriuretic peptide. Circ Heart Fail. 2011;4:114–120. doi:10.1161/CIRCHEARTFAILURE.109.895581
18. Peleg A, Ghanim D, Vered S, Hasin Y. Serum corin is reduced and predicts adverse outcome in non-st-elevation acute coronary syndrome. Eur Heart J Acute Cardiovasc Care. 2013;2:159–165. doi:10.1177/2048872613483588
19. Yu R, Han X, Zhang X, Wang Y, Wang T. Circulating soluble corin as a potential biomarker for cardiovascular diseases: a translational review. Clin Chim Acta. 2018;485:106–112. doi:10.1016/j.cca.2018.06.036
20. Pickering TG, Hall JE, Appel LJ, et al. Recommendations for blood pressure measurement in humans: an aha scientific statement from the council on high blood pressure research professional and public education subcommittee. J Clin Hypertens. 2005;7:102–109. doi:10.1111/j.1524-6175.2005.04377.x
21. Chen L, Zhang Q, Zhang M, et al. Soluble corin predicts the risk of cardiovascular disease. JACC. 2022;2:490–501. doi:10.1016/j.jacasi.2022.01.004
22. Roth GA, Mensah GA, Johnson CO, et al. Global burden of cardiovascular diseases and risk factors, 1990–2019: update from the gbd 2019 study. J Am Coll Cardiol. 2020;76:2982–3021. doi:10.1016/j.jacc.2020.11.010
23. Yousufuddin M, Young N. Aging and ischemic stroke. Aging. 2019;11:2542–2544. doi:10.18632/aging.101931
24. Roy-O’Reilly M, McCullough LD. Age and sex are critical factors in ischemic stroke pathology. Endocrinology. 2018;159:3120–3131. doi:10.1210/en.2018-00465
25. Wiinberg N, Høegholm A, Christensen HR, et al. 24-h ambulatory blood pressure in 352 normal Danish subjects, related to age and gender. Am J Hypertens. 1995;8:978–986. doi:10.1016/0895-7061(95)00216-2
26. de Miguel-Yanes JM, Jiménez-García R, López-de-Andrés A, et al. The influence of sex on ischemic stroke incidence, therapeutic procedures and in-hospital mortality: results of the Spanish national hospital discharge. Int J Clin Pract. 2021;75:e14984. doi:10.1111/ijcp.14984
27. Poorthuis MHF, Algra AM, Algra A, Kappelle LJ, Klijn CJM. Female- and male-specific risk factors for stroke: a systematic review and meta-analysis. JAMA Neurol. 2017;74:75–81. doi:10.1001/jamaneurol.2016.3482
28. Weikert C, Berger K, Heidemann C, et al. Joint effects of risk factors for stroke and transient ischemic attack in a German population: the epic Potsdam study. J Neurol. 2007;254:315–321. doi:10.1007/s00415-006-0358-x
29. Markidan J, Cole JW, Cronin CA, et al. Smoking and risk of ischemic stroke in young men. Stroke. 2018;49:1276–1278. doi:10.1161/STROKEAHA.117.018859
30. Diener HC, Hankey GJ. Primary and secondary prevention of ischemic stroke and cerebral hemorrhage: jacc focus seminar. J Am Coll Cardiol. 2020;75:1804–1818. doi:10.1016/j.jacc.2019.12.072
31. Fan M, Lv J, Yu C, et al. Family history, tobacco smoking, and risk of ischemic stroke. J Stroke. 2019;21:175–183. doi:10.5853/jos.2018.03566
32. Madsen TE, Long DL, Carson AP, et al. Sex and race differences in the risk of ischemic stroke associated with fasting blood glucose in regards. Neurology. 2021;97:e684–e694. doi:10.1212/WNL.0000000000012296
33. Li H, Qian F, Zuo Y, et al. U-shaped relationship of high-density lipoprotein cholesterol and incidence of total, ischemic and hemorrhagic stroke: a prospective cohort study. Stroke. 2022;53:1624–1632. doi:10.1161/STROKEAHA.121.034393
34. Takahashi M, Chamczuk A, Hong Y, Jackowski G. Rapid and sensitive immunoassay for the measurement of serum s100b using isoform-specific monoclonal antibody. Clin Chem. 1999;45:1307–1311. doi:10.1093/clinchem/45.8.1307
35. Hill MD, Jackowski G, Bayer N, Lawrence M, Jaeschke R. Biochemical markers in acute ischemic stroke. CMAJ. 2000;162:1139–1140.
36. Dvorak F, Haberer I, Sitzer M, Foerch C. Characterisation of the diagnostic window of serum glial fibrillary acidic protein for the differentiation of intracerebral haemorrhage and ischaemic stroke. Cerebrovasc Dis. 2009;27:37–41. doi:10.1159/000172632
37. Foerch C, Wunderlich MT, Dvorak F, et al. Elevated serum s100b levels indicate a higher risk of hemorrhagic transformation after thrombolytic therapy in acute stroke. Stroke. 2007;38:2491–2495. doi:10.1161/STROKEAHA.106.480111
38. Cuadrado E, Rosell A, Colomأ╚ N, et al. The proteome of human brain after ischemic stroke. J Neuropathol Exp Neurol. 2010;69:1105–1115. doi:10.1097/NEN.0b013e3181f8c539
39. Lescuyer P, Allard L, Zimmermann-Ivol CG, et al. Identification of post-mortem cerebrospinal fluid proteins as potential biomarkers of ischemia and neurodegeneration. Proteomics. 2004;4:2234–2241. doi:10.1002/pmic.200300822
40. Whiteley W, Chong WL, Sengupta A, Sandercock P. Blood markers for the prognosis of ischemic stroke: a systematic review. Stroke. 2009;40:e380–e389. doi:10.1161/STROKEAHA.108.528752
41. Wu F, Yan W, Pan J, Morser J, Wu Q. Processing of pro-atrial natriuretic peptide by corin in cardiac myocytes. J Biol Chem. 2002;277:16900–16905. doi:10.1074/jbc.M201503200
42. Chen F, Xia Y, Liu Y, et al. Increased plasma corin levels in patients with atrial fibrillation. Clinica Chimica Acta. 2015;447:79–85. doi:10.1016/j.cca.2015.05.017
43. Dong N, Chen S, Yang J, et al. Plasma soluble corin in patients with heart failure. Circ Heart Fail. 2010;3:207–211. doi:10.1161/CIRCHEARTFAILURE.109.903849
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.