Back to Journals » Journal of Pain Research » Volume 15
Therapy for Psychiatric Comorbidities in Patients with Episodic Cluster Headache: A Prospective Multicenter Study
Authors Liu Q , Zhang Y, Hu C, Yuan D, Wang K, Fan W, Pan F, Li Q, Wang Y, Tan G
Received 16 April 2022
Accepted for publication 4 October 2022
Published 18 October 2022 Volume 2022:15 Pages 3245—3254
DOI https://doi.org/10.2147/JPR.S371062
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Alexandre F DaSilva
Qinlin Liu,1 Yixin Zhang,1 Chuan Hu,2 Dongli Yuan,3 Kuiyun Wang,4 Wen Fan,5 Feibao Pan,6 Qin Li,7 Yunfeng Wang,1 Ge Tan1
1Department of Neurology, The First Affiliated Hospital of Chongqing Medical University, Chongqing, People’s Republic of China; 2Department of Neurology, People’s Hospital of Bishan District, Bishan, People’s Republic of China; 3Department of Intelligent Medical Systems, Chongqing Medical University, Chongqing, People’s Republic of China; 4Department of Neurology, Jintang First People’s Hospital, Sichuan, People’s Republic of China; 5Department of Neurology, Guizhou Provincial People’s Hospital, Guiyang, People’s Republic of China; 6Department of Neurology, Suining Central Hospital, Suining, People’s Republic of China; 7Department of Neurology, Chongqing General Hospital, Chongqing, People’s Republic of China
Correspondence: Ge Tan, The First Affiliated Hospital of Chongqing Medical University, 1 Youyi Road, Chongqing, People’s Republic of China, Email [email protected]
Purpose: To explore changes of depression, anxiety and sleep disturbance in patients with episodic cluster headache inside and outside the attack period and assess the therapy to improve the treatment.
Patients and Methods: We prospectively recruited 396 patients from 11 specialized headache outpatients and analyzed their headache characteristics, Hospital Anxiety Depression Scale scores, Pittsburgh sleep quality index scores, and the usage of psychiatric medications during as well as 1 month after the attack period.
Results: A total of 220 patients completed the follow-up, 52.73% of whom had anxiety, 47.27% had depression and 49.09% had sleep disturbance inside the attack period. At follow-up, the percentage of these patients significantly decreased to 16.36%, 21.82% and 14.55% in the remission period, respectively (p < 0.05). Antidepressants and mood stabilizers were prescribed to 58.18% of the patients. However, both of the changes of Hospital Anxiety Depression Scale scores after the end of the attack period for anxiety (3.52± 2.91 vs 3.32± 3.09, p =0.61) and depression (3.41± 3.33 vs 2.90± 3.58, P =0.28) were comparable in patients with and without taking these medications. Nocturnal onset of headache was positively correlated with Pittsburgh score (OR=8.71), anxiety (OR=2.33) and depression scores (OR=3.56) (p < 0.05).
Conclusion: Depression, anxiety and sleep disturbance were significantly alleviated after the attack period. However, psychiatric medications showed limited effect on depression and anxiety. Additionally, the nocturnal attack may cause anxiety and depression in episodic cluster headache.
Keywords: cluster headache, depression, anxiety, sleep disturbance, psychiatric comorbidities
Introduction
The typical clinical manifestations of cluster headache (CH), the most common type of primary trigeminal autonomic headache, are unilateral, severe episodic headache with ipsilateral autonomic nervous symptoms or restlessness. The duration of each attack ranges from 15 to 180 minutes, and the frequency ranges from 1 every other day to 8 times in 24 hours.1 The pathophysiological mechanism of CH is related to the dysfunction of hypothalamus,1,2 trigeminovascular system,3,4 and autonomic nervous system.5,6 The prevalence of CH in the population is approximately 0.1%, and the male-to-female ratio is approximately 3:1.2 Severe headache reduces patients’ quality of life and may even lead to suicidal intention; therefore, it is also known as suicide headache.1,2
Patients with CH often have sleep disturbance, and they usually complain of headaches after falling asleep. Recently, a certain relationship between CH attacks and rapid eye movement (REM) sleep was identified.7,8 Nevertheless, whether nocturnal attack can lead to sleep disturbance has no final conclusion. Accompanying anxiety or depression is also common in patients with CH, and the hypothalamus plays a core role in psychiatric comorbidities in CH. One study proposed the benefits of behavioral therapies to manage the psychiatric comorbidities in primary headache9; however, the medication treatment of psychiatric comorbidities in CH patients has not been investigated yet.
By studying anxiety, depression, sleep disturbance, and the use of psychiatric medications in patients with episodic cluster headache(eCH), we aimed to explore the correlation among the CH attack, psychiatric comorbidities and assess the efficacy of these drugs in order to facilitate the clinical treatment.
Materials and Methods
Study Design
This study used prospective data from consecutive eCH patients from 11 headache clinics in southwest China (headache clinic of The First Affiliated Hospital of Chongqing Medical University, Yongchuan Hospital of Chongqing Medical University, Chongqing People’s Hospital, Chongqing Fifth People’s Hospital, Chongqing Ninth People’s Hospital, Chongqing Sanxia Central Hospital, Chongqing Hechuan District People’s Hospital, Jintang First People’s Hospital, Suining Central Hospital, Sichuan Nanchong Central Hospital and Guizhou Provincial People’s Hospital) between January 2018 and January 2020.
All of the patients with eCH were screened by headache specialists. As described previously, the diagnosis of eCH, through a semi-structured face-to-face interview,10 was based on ICHD-3.11 The inclusion criteria were as follows: 1) age between 18 and 65 y; 2) during the cluster period. The exclusion criteria were as follows: 1) headache attributed to secondary causes; 2) pregnancy and lactation; 3) serious organic diseases, such as malignant tumors, severe hepatic and renal impairment, myocardial infarction, etc; 4) diagnosed with depression, anxiety, sleep disorders or other severe mental illness before the first attack of CH; and 5) unable to complete questionnaires and follow-ups.
Detailed clinical data of target patients were recorded at their initial visit and 1 month after the last CH attack (Figure 1). To ensure the second date record was in the remission period, we excluded the patients who had CH attack relapses after the second date record and followed up the other patients at least 3 months after the last CH attack.
 |
Figure 1 Study flow. |
Measures
Clinical demographics were collected, including sex, age, course of headache, duration of the attack period, headache frequency, duration of each attack, headache areas, migraine-like features, autonomic nervous symptoms, and using of psychiatric medications. Since some patients complained of multiple CH attacks in 1 day, we asked them about the onset time of their most severe and disturbing CH attack in 1 day.
Headache intensity was measured using the visual analogue scale (VAS), with 0 representing no headache and 10 representing very severe headache. The Headache Impact Test (HIT-6) scale was used to measure headache burden on patients’ daily life. A higher score indicated a higher degree of disability caused by headache.12
The Hospital Anxiety Depression Scale (HADS) was a self-assessment scale for outpatient to detect anxiety and depression. Patients with scores between 8 and 10 were considered to have doubtful anxiety or depression, and patients with scores greater than 10 were considered to have definite anxiety or depression.13
The Pittsburgh Sleep Quality Index (PSQI) was used to measure sleep quality of patients. If a patient scored more than 5 points, he/she had sleep disturbance.14
Statistical Method
Baseline data were described as the means ± standard deviation (SD) or percentages (%). The differences of HADS and PSQI between the attack period and 1 month after the end of the attack were analyzed using paired-sample t-tests. Differences in proportions were analyzed using χ2 tests. HADS ≥8 was included as the dependent variable, and a binary logistic regression analysis was conducted with sex, duration of each attack, frequency, VAS, PSQI, migraine-like features and autonomic nervous symptoms as independent variables. The results were reported as odds ratios (ORs) with 95% confidence intervals (CIs). Patients were divided into subgroups according to whether they took psychiatric medications. We used t-tests to analyze the differences of HADS and PSQI between subgroups. t-tests were also used to analyze the differences of HADS and PSQI between patients whose most severe and disturbing CH attack onset at night and in daytime. Meanwhile we conducted a binary logistic regression analysis to test the association between the most severe and disturbing attack occurring at night and HADS ≥8, PSQI >5 and sleep disturbance. The results were reported as odds ratios (ORs) with 95% CIs. P values <0.05 were considered statistically significant. All data were analyzed using SPSS 26.0 software (IBM Corp., USA).
Results
Participants
A total of 396 eCH patients were screened in the study, 327 patients participated in the study, of whom 107 were excluded in the assessment, and 220 patients completed the follow-up and were included in analysis (Figure 1).
Clinical Features
Baseline data are shown in Table 1. Patients with eCH were mostly middle aged (40±12 years), among which male patients (136/220, 61.82% vs female 84/220, 38.18%, p<0.05) accounted for the majority. The VAS scores (8.25±1.15) showed that headache intensities of CH patients were mostly severe. The most common headache area was the temporal region (92/220, 41.82%), followed by the orbital (60/220, 27.27%), forehead (40/220, 18.18%) and top of the head (20/220, 9.09%). The main types of pain were distending pain (116/220, 52.73%) and pulsating pain (112/220, 50.91%). The majority of patients (140/220, 63.63%) had migraine-like features, among which patients with nausea and vomiting (104/220, 47.27%) accounted for the highest proportion. Table 1 shows the psychiatric medications prescribed for eCH patients. Over one-third of them (80/220, 36.36%) took antidepressant, including serotonin-noradrenaline reuptake inhibitor (SNRI), selective serotonin reuptake inhibitor (SSRI) and mirtazapine, and nearly half of patients (48/220, 21.82%) took mood stabilizers, lithium. Besides, 41.82% patients (92/220) in our study took hypnotics, including benzodiazepines and Z-drug hypnotics.
 |
Table 1 Baseline Characteristics of eCH |
Anxiety and CH
The HADS-A 1 month after the end of the attack period was significantly lower than that during the attack period (4.25±3.72 vs 7.69±3.28, P<0.01). We found 52.72% (116/220) of patients had HADS-A≥8, in which 18.18% (40/220) had HADS-A≥11 during the attack period, whilst at 1 month after the attack period, only 16.36% (36/220) of the patients had HADS-A≥8, in which 9.09% (20/220) of the patients had HADS-A≥11, and these differences were statistically significant (P < 0.01) (Table 2). The logistic regression analysis showed that female gender (OR=4.34, P < 0.01), frequent headache attacks (OR=1.49, P=0.03), severe sleep disturbance (OR=1.09, P=0.02), and co-existing migraine-like features (OR=3.14, P<0.01) were more likely to have a higher HADS for anxiety (Table 3). Table 4 shows no significant differences in HADS-A between subgroups based on whether patients using antidepressants or mood stabilizers (7.75±3.28 vs 7.61±3.30, P =0.75). As for the changes of HADS-A 1 month after the end of the attack comparing with that during the attack period, there were no differences between the subgroups (3.52±2.91 vs 3.32±3.09, P =0.61) (Table 4).
 |
Table 2 HADS and PSQI Scores of eCH |
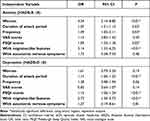 |
Table 3 Logistic Analysis of Psychiatric Comorbidities in eCH |
 |
Table 4 HADS and PSQI in the Subgroups |
Depression and CH
The HADS-D 1 month after the end of the attack period were significantly lower than that during the attack period (4.25±3.72 vs 7.71±3.04, P < 0.01). We found 47.27% (104/220) of patients had HADS-D≥8, in which 21.82% (48/220) had HADS-D≥11 during the attack period, whilst at 1 month after the attack period, only 21.82% (48/220) of the patients had HADS-D≥8, in which 9.09% (20/220) of the patients had HADS-D≥11, and these differences were statistically significant (P<0.01) (Table 2). The logistic regression analysis showed that patients with long attack periods (OR=1.14, P<0.01), serious sleep disturbance (OR=1.15, P<0.01), and co-existing migraine-like features (OR=2.73, P<0.01) were more likely to have a higher HADS indicating depression (Table 3). The HADS-D, in the subgroup of taking antidepressants and mood stabilizers, was 7.86±3.05 during the attack period and 4.45±3.74 1 month after the end of attack period. Although the changes differed from that of the patients not using these psychiatric medications, the result was still without statistically significant (3.41±3.33 vs 2.90±3.58, P =0.28) (Table 4).
Sleep and CH
The PSQI of patients 1 month after the end of the attack period was significantly improved compared with that during the attack period (6.05±4.43 vs 3.07±2.84, P<0.01) (Table 2). In addition, we divided patients into two subgroups according to whether they took hypnotics. The changes of PSQI 1 month after the attack period in the two subgroups were significantly different (5.30±2.19 vs 1.32±1.80, P<0.01) (Table 4).
At the same time, we summarized the onset time of most severe and disturbing attack and found that the peak time was 2:00 am and 3:00 am, followed by 12:00 am (Figure 2). Then, we compared the HADS-A (8.60±3.05 vs 6.93±3.29), HADS-D (8.60±2.85 vs 6.96±3.00), and PSQI (8.52±4.56 vs 4.00±3.07) of patients with the most severe and disturbing headache onset at night and in daytime (22:00 to 6:00 was defined as night, and 7:00 to 21:00 was defined as day) and observed the significant differences (P<0.01) (Table 5).
 |
Table 5 HADS and PSQI of eCH with the Most Severe and Disturbing Attacks at Night or in Daytime |
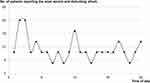 |
Figure 2 The time of the most severe and disturbing headache onset. |
The result of logistic regression analysis in Table 6 indicates that patients with the most severe and disturbing attack at night were more likely to suffer from sleep disturbance (OR=8.71, P<0.01), anxiety (OR=2.33, P<0.01) and depression (OR=3.56, P<0.01).
 |
Table 6 Logistic Associations Between the Most Severe and Disturbing Attack Occurring at Night and Anxiety, Depression, and Sleep Disturbance |
Discussion
Cluster headache is one of the most severe primary headaches. In our study, when patients were in the attack period, approximately half of them experienced anxiety and depression. Previous studies have reported that the incidence of anxiety and depression in patients with CH fluctuates substantially, ranging from 3.6% to 43.9%. Different studies have used different scales to evaluate anxiety and depression, such as the HADS, Patient Health Questionnaire (PHQ-9), Center for Epidemiologic Studies-Depression (CES-D), and Generalized Anxiety Disorder (GAD-7), and some studies have also reported the diagnosis of anxiety and depression by psychiatric specialists.15–18 However, in many studies, the prevalence of depression in patients with CH is significantly higher than in the population, and the risk of depression is greater than that in the population.16–18 Logistic regression studies from the Netherlands and South Korea also showed significant correlations between CH and anxiety and depression.17,18 The mechanism of the comorbidity of cluster headache with anxiety and depression may be related to many factors. Headache attack at night and sleep deprivation may lead to anxiety and depression. Repeated moderate-to-severe headaches cause fear and stress that can also lead to anxiety and depression. Relevant studies have shown that the incidence rate of CH and depression are both related to hypothalamic dysfunction.15–18 In addition, the insular lobe is associated with the severity of depression, and increased glucose metabolism in the insular lobe may predict depressive symptoms in individuals with paroxysmal pain, which may also be associated with the CH and depression comorbidity.19
One month after the end of the attack period, the anxiety and depression of patients were significantly alleviated in our study, and the number of patients with anxiety and depression symptoms was remarkably reduced (Table 2). Previous studies have also shown that patients with CH are more anxious and depressed in the attack period than in the remission period.18 The linear regression analysis showed that HADS-D correlated with whether patients were in the attack period; however, after adjusting for the PSQI, no correlation was observed between the attack period and the severity of depression.17 Moreover, a cross-sectional study from the United States revealed that patients with eCH in the attack period and remission period had the same incidence of anxiety and depression.15 These studies indicated that the effect of the attack period on anxiety and depression in patients with CH is not clear. Therefore, long-term follow-up of larger samples and basic medical research on psychiatric disorders in patients with CH are needed.
Migraine-like features are common among patients with CH, between 46% and 63.8% reported these symptoms.20,21 Our logistic regression showed that eCH patients with migraine-like features had a higher risk to get anxiety (OR=3.138) and depression (OR=2.732) compared to eCH without migraine-like features in our study (Table 3). And the American Migraine Prevalence and Prevention (AMPP) study in 2011 showed that CH patients with anxiety or depression were more likely to report nausea and premonitory symptoms.15 Meanwhile, migraine-like features were reported to delay the CH diagnosis, unfortunately, rare studies have investigated the potential relationship between diagnostic delay and psychiatric comorbidities.20 Further studies are needed to determine whether the same mechanism or pathway causes the migraine-like features, depression and anxiety in patients with CH.
A study from Taiwan conducted in 2012 demonstrated that women with CH had a higher risk of depression than men,16 which is similar with this study. The majority of patients with CH were male, but the majority of patients with anxiety or depression were female. We hypothesized that sex hormones and the hypothalamic-pituitary-gonadal axis may be involved in pathophysiological processes.
In order to analyze the effect of psychiatric medications, including antidepressants and mood stabilizers, on HADS among eCH inside the attack period, we divided these patients into two subgroups according to the usage of these medications (use group and not use group). However, no significantl differences on HADS-A and -D were detected between the two subgroups inside the attack period as well as after the attack period. The results indicated that diagnosis and treatment of depression and anxiety was depended on the face-to-face interview between doctors and patients, all the scales were only used as a reference. Meanwhile, according to the similar reduction of HADS in patients took antidepressants and mood stabilizers with patients not took after the attack period, these psychiatric medications seemed to have little improvement on comorbid anxiety and depression for eCH. Thus, we believed the necessity to use antidepressants and mood stabilizers for eCH patients without the past history of mental illness needed further research.
Our results showed that hypnotics could effectively improve sleep disorders in eCH. However, the sleep quality of patients taking hypnotics, who had more severe sleep disturbance in the attack period, was still poorer than patients not taking in the remission period (Table 4). In 2018, Lund et al found that after the end of the attack period, the sleep disturbance of CH was still more serious than those of common people. Their studies using PSG and actigraphy illustrated that the onset of CH at night did not affect the sleep quality of the patients, and no significant differences in sleep duration, efficiency or proportion of REM were observed in patients with CH between the onset and remission period.22,23 Therefore, it seems hard to explain whether CH attack is the cause of sleep disturbance or both of them coexist through the same pathological mechanism.
We observed two peaks of headache onset time, 2:00–3:00 am and 12:00 am. Similar to previous studies, the most common period for CH onset was 21:00 to 10:00 am, especially 2:00 am.8,24 The mechanism of the circadian rhythm of CH still remains unclear. Previous studies revealed that circadian rhythm may be related to sleep as a trigger factor for CH attack, the most common trigger factor was night sleep, followed by daytime napping. Meanwhile, the hypothalamus affects the circadian rhythm of patients through the suprachiasmatic nucleus, and the hypothalamus also participates in the CH pathway, although the specific site has not been clearly determined. In addition, melatonin and hypocretin secreted by the hypothalamus are also involved in the regulation of circadian rhythm, which have not been proven to be related to the onset of CH.7,8
Our results illustrated those patients with the most severe and disturbing CH attack at night had more sleep disturbance and severe anxiety and depression than patients with the most severe and disturbing attack in daytime. The logistic regression analysis showed that nocturnal attack might lead to anxiety, depression, and sleep disturbance. The mood and sleep disorders can be explained by interrupted sleep and delayed treatment due to nocturnal attack. It reminds us that headache specialists should not only pay attention to the sleep quality of patients with nocturnal attacks but also to their mood disorders.
Limitation
First, in our study, the headache specialists were not asked to unify the types and dosages of psychiatric medications, because the diagnosis and treatment of mental illness required individualization. Second, we enrolled patients all visiting at tertiary hospitals instead of sampled in the population or in primary hospitals, because most headache specialists in China were working in tertiary hospitals. China is a vast country with a large population, and nationwide statistical analysis are difficult to conduct.
Conclusion
In our study, the anxiety, depression and sleep disturbance in patients were significantly alleviated 1 month after the end of the attack period. However, depression and anxiety of eCH did not improve significantly by using psychiatric medications. Thus, the necessity to use antidepressants and mood stabilizers for eCH patients without the past history of mental illness need further study. Moreover, the study showed that the nocturnal onset of eCH attack may lead to obvious anxiety and depression, and headache specialists should pay more attention to mood disorders of these patients.
Data Sharing Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Ethics Approval and Informed Consent
This study received ethical approval from the Ethics Committee of the First Affiliated Hospital of Chongqing Medical University (20180618). All patients provided written informed consent to participate and publication. This study complied with the Declaration of Helsinki.
Acknowledgments
Thank all the staff of Chongqing Headache Society for their efforts. We were able to complete this research thanks to their hard work that even during the COVID-19 pandemic, they kept working.
Funding
This study was supported by Chongqing Medical Scientific Research Project of Chongqing Health Commission and Science and Technology Bureau (2020MSXM096) and the Scientific Research Project of Chongqing Yuzhong Science and Technology Commission (20180154).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Hoffmann J, May A. Diagnosis, pathophysiology, and management of cluster headache. Lancet Neurol. 2018;17(1):75–83. doi:10.1016/S1474-4422(17)30405-2
2. May A, Schwedt TJ, Magis D, Pozo-Rosich P, Evers S, Wang SJ. Cluster headache. Nat Rev Dis Primers. 2018;4:18006. doi:10.1038/nrdp.2018.6
3. May A, Goadsby PJ. The trigeminovascular system in humans: pathophysiologic implications for primary headache syndromes of the neural influences on the cerebral circulation. J Cereb Blood Flow Metab. 1999;19(2):115–127. doi:10.1097/00004647-199902000-00001
4. Goadsby PJ, Edvinsson L. Human in vivo evidence for trigeminovascular activation in cluster headache. Neuropeptide changes and effects of acute attacks therapies. Brain. 1994;117(Pt 3):427–434. doi:10.1093/brain/117.3.427
5. Goadsby PJ. Autonomic nervous system control of the cerebral circulation. Handb Clin Neurol. 2013;117:193–201. doi:10.1016/B978-0-444-53491-0.00016-X
6. May A. Cluster headache: pathogenesis, diagnosis, and management. Lancet. 2005;366(9488):843–855. doi:10.1016/S0140-6736(05)67217-0
7. Barloese M, Jennum P, Knudsen S, Jensen R. Cluster headache and sleep, is there a connection? A review. Cephalalgia. 2012;32(6):481–491. doi:10.1177/0333102412441090
8. Naber WC, Fronczek R, Haan J, et al. The biological clock in cluster headache: a review and hypothesis. Cephalalgia. 2019;39(14):1855–1866. doi:10.1177/0333102419851815
9. Caponnetto V, Deodato M, Robotti M, et al. Comorbidities of primary headache disorders: a literature review with meta-analysis. J Headache Pain. 2021;22(1):71. doi:10.1186/s10194-021-01281-z
10. Xie Q, Huang Q, Wang J, Li N, Tan G, Zhou J. Clinical features of cluster headache: an outpatient clinic study from China. Pain Med. 2013;14(6):802–807. doi:10.1111/pme.12101
11. Headache Classification Committee of the International Headache Society (IHS). The international classification of headache disorders, 3rd edition. Cephalalgia. 2018;38(1):1–211. doi:10.1177/0333102417738202
12. Nachit-Ouinekh F, Dartigues JF, Henry P, et al. Use of the headache impact test (HIT-6) in general practice: relationship with quality of life and severity. Eur J Neurol. 2005;12(3):189–193. doi:10.1111/j.1468-1331.2004.00934.x
13. Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370. doi:10.1111/j.1600-0447.1983.tb09716.x
14. Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi:10.1016/0165-1781(89)90047-4
15. Robbins MS, Bronheim R, Lipton RB, et al. Depression and anxiety in episodic and chronic cluster headache: a pilot study. Headache. 2012;52(4):600–611. doi:10.1111/j.1526-4610.2011.02024.x
16. Liang JF, Chen YT, Fuh JL, et al. Cluster headache is associated with an increased risk of depression: a nationwide population-based cohort study. Cephalalgia. 2013;33(3):182–189. doi:10.1177/0333102412469738
17. Louter MA, Wilbrink LA, Haan J, et al. Cluster headache and depression. Neurology. 2016;87(18):1899–1906. doi:10.1212/WNL.0000000000003282
18. Kim BS, Chung PW, Kim BK, et al. The impact of remission and coexisting migraine on anxiety and depression in cluster headache. J Headache Pain. 2020;21(1):58. doi:10.1186/s10194-020-01120-7
19. Seifert CL, Valet M, Pfaffenrath V, et al. Neurometabolic correlates of depression and disability in episodic cluster headache. J Neurol. 2011;258(1):123–131. doi:10.1007/s00415-010-5704-3
20. Taga A, Russo M, Manzoni GC, Torelli P. Cluster headache with accompanying migraine-like features: a possible clinical phenotype. Headache. 2017;57(2):290–297. doi:10.1111/head.12971
21. Frederiksen HH, Lund NL, Barloese MC, Petersen AS, Jensen RH. Diagnostic delay of cluster headache: a cohort study from the Danish Cluster Headache Survey. Cephalalgia. 2020;40(1):49–56. doi:10.1177/0333102419863030
22. Lund NLT, Snoer AH, Petersen AS, et al. Disturbed sleep in cluster headache is not the result of transient processes associated with the cluster period. Eur J Neurol. 2019;26(2):290–298. doi:10.1111/ene.13820
23. Lund NL, Snoer AH, Jennum PJ, Jensen RH, Barloese MCJ. Sleep in cluster headache revisited: results from a controlled actigraphic study. Cephalalgia. 2019;39(6):742–749. doi:10.1177/0333102418815506
24. Barloese M, Lund N, Petersen A, Rasmussen M, Jennum P, Jensen R. Sleep and chronobiology in cluster headache. Cephalalgia. 2015;35(11):969–978. doi:10.1177/0333102414564892
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
