Back to Journals » Adolescent Health, Medicine and Therapeutics » Volume 14
Self-Disclosure Patterns Among Children and Youth with Epilepsy: Impact of Perceived-Stigma
Authors Clifford LM , Brothers SL, Lang A
Received 7 October 2022
Accepted for publication 19 January 2023
Published 5 February 2023 Volume 2023:14 Pages 27—43
DOI https://doi.org/10.2147/AHMT.S336124
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Alastair Sutcliffe
Lisa M Clifford, Shannon L Brothers, Amy Lang
Division of Behavioral Medicine and Clinical Psychology, Cincinnati Children’s Hospital Medical Center, Cincinnati, OH, USA
Correspondence: Lisa M Clifford, Division of Behavioral Medicine and Clinical Psychology, Cincinnati Children’s Hospital Medical Center, 3333 Burnet Ave, MLC 3015, Cincinnati, OH, 45229, USA, Tel +1 513 803 3409, Fax +1 513 636 7756, Email [email protected]
Abstract: This review aimed to synthesize the minimal existing literature on the impact of perceived stigma on self-disclosure patterns among children and youth with epilepsy (YWE). Initial literature searches were conducted in PsycInfo, Scopus, Web of Science, and PubMed using search terms focused on epilepsy, pediatrics, disclosure, and/or stigma. Articles were included if they were original human research articles published in peer-reviewed journals that were accessible in English through Cincinnati Children’s Hospital Medical Center Pratt Library and fit study aims. Thirteen articles, which primarily used qualitative self-report methodologies, fit the study’s inclusion criteria. YWE report greater perceived stigma and lower illness disclosure compared to youth with other chronic health conditions. Across studies, perceived stigma was consistently identified as a barrier to YWE disclosing their epilepsy diagnosis. Consequences of perceived stigma included lower self-esteem, poorer perceived competency, lack of self-confidence, social withdrawal, and lower quality of life. YWE’s reluctance to disclose epilepsy was associated with worry about differential treatment, negative impact on close relationships, negative impact on others’ perceptions, and negative self-perceptions. While WHO and ILAE have identified stigma as contributing to higher disease burden in people with epilepsy and have highlighted the importance of prioritizing social policy focused on decreasing epilepsy-related stigma, progress has been incremental and much work remains. Future research is needed to understand socio-cultural factors perpetuating stigma among YWE in order to further develop, evaluate, and disseminate evidence-based clinical and education programming to combat epilepsy-related stigma.
Keywords: attitudes, enacted stigma, secrecy, adolescent, children, parents
Introduction
Epilepsy is the most common serious neurodevelopmental disorder in childhood impacting approximately 0.9% of the children and adolescents globally.1 Compared to youth with other chronic illnesses, youth with epilepsy (YWE) experience higher rates of comorbid medical conditions, neurological disorders, behavioral health comorbidities (eg, anxiety, depression, ADHD),2 academic underachievement,3 poorer social functioning, and lower health-related quality of life (HRQOL).4 Over the past two decades, there has been a growing recognition of the negative impact that stigma has on the health and well-being of people living with epilepsy (PWE) including diagnosis secrecy to avoid discrimination, consequent social isolation and gaps in treatment (WHO). As a result, there have been a series of global and national initiatives to address the burden of epilepsy since 1997 that have focused on reducing epilepsy-related stigma and increasing knowledge and awareness about epilepsy.5
Stigma is a socially derived concept that defines an attribute as a discrediting mark of difference6 and can be experienced as enacted stigma or perceived stigma. For people with epilepsy (PWE), enacted stigma represents actual acts of discrimination by others due to the perception of PWE as unacceptable or inferior due to their condition. Perceived stigma represents the internalization of epilepsy-related social stigma by PWE and close others (eg, family members, close friends, etc) resulting in feelings of shame, embarrassment, and fear of enacted stigma.6–8 In one population-based study, one-third of people of all ages living with epilepsy identified stigma as the most difficult part of living with the condition.9 Some research also suggests that the effects of perceived stigma are more detrimental to the health and well-being of PWE than enacted stigma.7
To date, most of the research on perceived stigma in epilepsy has focused on adults or a mixed sample of youth and adults without clear delineation of outcomes specific to children and youth. In a recent systematic review on perceived stigma in PWE across age ranges,10 perceived stigma was associated with anxiety, depression, lower quality of life, lower self-esteem, negative self-perceptions (eg, shame, inferiority, sense of being a burden to others, feeling different from others), and changes in social relationships (eg, perceived differential treatment). The limited research specific to YWE found high perceived stigma and negative attitudes toward illness and self; however, compared to adults with epilepsy, younger YWE were more optimistic about their future, while older adolescents with epilepsy had worse attitudes toward illness.10 Two of the most common predictors of perceived stigma specific to YWE were higher seizure severity and lower knowledge about epilepsy.
Recent research documenting global health statistics found significant disparities in adolescent health. This research highlights that adolescents have been largely neglected in global health and social policy,11 resulting in fewer health gains than other age groups irrespective of economic development. This is unfortunate, as adolescence represents a critical stage of development during which competencies that define health trajectories that track into adulthood are formed. During this formative period of life, adolescents experience increased levels of uncertainty and self-consciousness as they navigate the task of identity formation. Their sense of self is heavily influenced by social interactions, especially interactions with peers. While parents continue to be influential, peers become increasingly important, often serving as a social comparison by which youth judge themselves.12 During this period of life when most adolescents are striving for acceptance by peers, for YWE, stigma can disrupt this normative developmental process.13 For instance, epilepsy is predominantly an invisible condition, thus requiring YWE to decide whether to 1) disclose their epilepsy diagnosis and risk disrupting the friendship and possible enacted stigma or 2) conceal their epilepsy diagnosis and miss the opportunity for gaining social support for their condition, as well as risk unintended disclosure as a consequence of a public seizure.
The decision to disclose or conceal health information is complex, involving multiple interacting processes. Greene’s Integrated Model of Health Disclosure Decision-Making14 serves as a framework for the decision-making process and proposes that while perceived stigma decreases the likelihood of disclosure, the quality of a relationship and disclosure efficacy may moderate the relationship between perceived stigma and disclosure. Lambert et al15 also describe five different disclosure strategies including concealment (eg, deliberate secrecy or avoidance of discussing epilepsy), unplanned revelation (eg, others learning about epilepsy as a consequence of witnessing a seizure or cues, such as taking medication and frequent school absences, or disclosure by a third party), selective/partial disclosure (eg, careful selection of confidantes to whom condition is disclosed or disclosure of select information), preventive disclosure (eg, informing others if detection is anticipated to forestall stigmatization, or to increase safety in the case of a seizure), and open disclosure (eg, no restrictions on information shared or parties to whom information is shared). For YWE, disclosure decisions are associated with significant worry about other’s negative responses, stigma, and complicated by the unpredictability of seizures that may lead to unintentional disclosure.16–18
For YWE, disclosure decisions are also influenced by their social environment including family health beliefs and behaviors, peer and teacher perceptions and behaviors and broader societal stigma. Among the many influential social factors, family health beliefs and behaviors are particularly powerful. For instance, disclosure management behaviors in YWE are commonly shaped by parent stigma coaching, a process by which parental concealment shapes YWE’s conceptualization of epilepsy as a discrediting attribute that should be hidden.16 Often, caregivers reinforce concealment of epilepsy in an attempt to protect their children from discrimination and from YWE internalizing feelings of being different or less capable. However, contrary to parental intentions, stigma coaching engenders perceived stigma.16 Further, the unpredictability of seizures creates an inherent risk for unintentional disclosure, fostering anticipatory anxiety in YWE and trepidation that their shameful and discrediting attribute will be exposed.
Research examining perceived stigma and disclosure in YWE is limited. Other literature reviews have either focused specifically on perceived stigma in YWE10 or epilepsy disclosure in YWE,19 or examined perceived stigma or disclosure across the lifespan rather than specifically targeting YWE. Therefore, the objective of this paper was to systematically review and synthesize the extant body of literature examining the impact of perceived-stigma on self-disclosure patterns among children and youth with epilepsy (YWE). Further, we sought to identify specific factors impacting perceived stigma and self-disclosure for YWE, such as disease-specific characteristics, sociodemographic factors, and sociocultural factors. Ultimately, the findings of this literature review have the potential to help inform the development of interventions aimed to decrease perceived stigma, encourage self-disclosure, and promote the self-esteem, health-related quality of life, social supports, and self-management practices among YWE.
Materials and Methods
Search Strategy
The initial literature searches for the current study were conducted in PsycInfo, Scopus, Web of Science, and PubMed using search terms focused on epilepsy, pediatrics, disclosure, and/or stigma. See Table 1 for specific search terms utilized for each search engine. Initial literature search resulted in 1631 articles (see details in Figure 1). The reference list of review articles identified in the initial literature searches that were pertinent to the current study aims (n=13) were also examined to identify additional potential articles for inclusion (n=33). Duplicates were removed.
 |
Table 1 Search Terms |
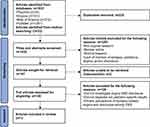 |
Figure 1 Article identification, screening, and inclusion flow chart. |
During the first stage of screening, unique article titles and abstracts (n=1432) were reviewed by study team members with training in pediatric psychology and, specifically, pediatric epilepsy to determine preliminary fit with the aims of the current study. Articles were primarily excluded in the first stage of screening due to not including original human research, being a review article, or not mentioning epilepsy, pediatrics, stigma, and/or disclosure.
In the second stage of screening, study team members reviewed the 139 full-text articles identified for potential inclusion in the first stage of screening in order to determine final inclusion based on the inclusion and exclusion criteria detailed below. Secondary full-text reviews were conducted by study team members if there was uncertainty regarding fit with the inclusion and exclusion criteria. Study team members met to finalize the list of articles to be included in the current study (n=13).
Inclusion and Exclusion Criteria
See Figure 1 for a depiction of the process for identifying and screening articles for inclusion in the current study. The following inclusion criteria were utilized: 1) original research articles; 2) human research; 3) written in English; 4) accessible through the Cincinnati Children’s Hospital Medical Center Pratt Library; 5) published in peer-reviewed journals; and 6) adequate fit with the aims of the current study (ie, related to epilepsy, pediatrics, disclosure, and stigma). Articles were excluded if they 1) did not investigate self-stigma and disclosure in YWE, either as primary, secondary, or incidental findings; 2) did not present pediatric-specific (ie, child, adolescent, and/or young adult, age 0–25 years) data; or 3) focused on others’ (eg, parents, family members, peers, teachers, health care workers, and/or general public) perceptions of epilepsy-related stigma.
Data Extraction
The 13 articles identified for inclusion in the current study were reviewed in detail by three study team members (see Table 2). Data extracted included study characteristics (ie, country of origin and study aims, design, setting, and data collection methods), sample (ie, setting, number of participants, age at participation, gender distribution, race/ethnicity distribution, and socioeconomic status), and epilepsy characteristics (ie, seizure type, time since diagnosis, age of onset, family history of epilepsy, and AED types). Findings delineating the relationship between perceived stigma and disclosure among YWE were also summarized. Additionally, the role of epilepsy characteristics, gender, age, stage of development, and sociocultural factors (if applicable) in perceived stigma and disclosure among YWE were reviewed.
 |
Table 2 Key Findings from Reviewed Studies Related to Perceived Stigma and Disclosure |
Results
Overview of Included Studies
Thirteen articles were included in the current study, as they focused on the role of perceived stigma on illness disclosure in YWE. The majority of these studies were conducted in Europe (10 Europe and Central Asia,16–24 2 North America,25,26 1 East Asia and Pacific)27 and in hospital-based settings. Studies primarily used qualitative research designs (10 qualitative,16,17,19,22–25,27,28 2 quantitative,21,26 1 mixed-method)20 with unstructured or semi-structured interviews and self-report methodologies (10 self-report,17,19,22,24,25,28 3 combined parent–child report).18,20,21 Among quantitative studies, the following validated instruments were used: Child Stigma Scale (CSS,29 n=1),20 Child Attitude Towards Illness Scale (CATIS,30,31 n=1),21 Parent Stigma Scale (PSS,29 n=2),20 and Epilepsy Disclosure Scale (EDS), Child & Parent Versions (n=2).20,21
Perceived Stigma and Disclosure Among YWE
Twelve of the 13 included studies16–25,27,28 identified perceived stigma among YWE as a substantial barrier to disclosure of epilepsy. In 1 quantitative study,26 perceived stigma was not statistically significantly associated with self-disclosure. Regarding targeted outcomes, in most studies perceived stigma and self-disclosure were not primary targets, but rather a result of incidental findings or sub themes of qualitative investigations. Of the 13 studies, 3 studies20,21,26 specifically targeted both perceived stigma and disclosure management, 4 targeted disclosure only,17,19,23,27 and in the 6 remaining studies,16,18,22,24,25,28 perceived stigma and disclosure outcomes were based on incidental findings or sub-themes.
Prevalence rates for perceived stigma were discussed in 5 studies16,18,22,23,26 and rates ranged from 20%16 to 36%.18 One study found that rates of perceived stigma were higher among YWE compared to youth with other chronic illnesses.22 Of the 5 studies22,24,26,28,32 that discussed the prevalence of YWE self-disclosure, rates ranged from 18%22 to 65%.26
Regarding disclosure patterns, across studies YWE endorsed some level of concealment and disclosure, and often engaged in different disclosure behaviors depending on circumstances. In 4 studies, disclosure management was discussed more broadly and did not include information about specific types of disclosure practices.20–22,25 Across studies, none of the participants reported open disclosure.
Unplanned disclosure often resulted from others witnessing a seizure (most commonly at school),28 others overhearing discussions about YWE’s health information (eg, peer overhearing YWE’s parent discuss epilepsy with the teacher), peers asking YWE about school absences, exemptions for school activities23,28 or medication taking.24 Selective disclosure often occurred due to YWE wanting to preserve a sense of control by selecting what health information was shared and to whom18,19 and to elicit social support and connectedness.19,26,27 Preventative disclosure commonly occurred due to YWE’s desire for support in the event of a seizure16–18,23,24 or a desire to prevent disruption to friendships or discrimination due to an unplanned disclosure.16,18,27
Regarding perceived stigma as a barrier to self-disclosure, one of the most common themes was anticipation that disclosure would lead to alienation by friends and peers including loss of friendships,25,27 exclusion from peer social activities24,26 and peer rejection and avoidance.16,25,28 Some YWE also described concern about peer bullying19,23,24 and worry that others would perceive them as different,19,24 less competent,28 or contagious.19 Another common theme was YWE’s internalization of stigma including general feelings of differentness16,18,19,25 and perceived inferiority (less intelligent,25 less capable18). YWE also described negative self-perceptions specific to epilepsy including general feelings of embarrassment, shame and resentment in relation to their epilepsy diagnosis16,17,19,24 and more specifically related to others witnessing seizures17,18,24,28 and medication taking.24
Outcomes associated with YWE self-disclosure were described in 7 studies. Voluntary disclosure was generally associated with greater peer acceptance and support,18,27,28 better quality of life, more positive family communication about epilepsy, and more positive attitudes toward epilepsy in YWE.21 In contrast, unplanned disclosure was more commonly associated with distancing or loss of friends18,27,28 and concealment was associated with more negative communication about epilepsy among family members,20 social withdrawal, loneliness,24 lower self-confidence and self-esteem,16 and lower quality of life.21
Relationship Between YWE Perceived Stigma, Self-Disclosure, and Epilepsy Characteristics
The relationship between perceived stigma, self-disclosure, and epilepsy characteristics was examined in 1 quantitative study and qualitatively explored in 6 studies. In the 1 mixed-methods study, quantitative analysis revealed higher levels of perceived stigma in YWE was associated with more frequent seizures, longer time since diagnosis, polytherapy, and tonic or clonic seizure types.20 Using a semi-structured interview, 1 study compared illness knowledge between YWE and children with other chronic illnesses, and found YWE to have the lowest rates of illness knowledge (77% accurately named their condition but the majority did not know the meaning of epilepsy or why they had seizures vs 100% accuracy for naming and explaining in the comparison group) and the lowest rates of disclosure to friends (18% vs 100% in the comparison group). However, the association between illness knowledge and disclosure was not directly assessed.22 Across the other 5 qualitative studies, YWE reported that lack of sufficient knowledge about epilepsy was a barrier to disclosing their epilepsy to peers,17,19,28 especially for younger YWE.19,28 The invisibility of epilepsy was also identified as a barrier to disclosure. For instance, some YWE reported that their decision to conceal their condition was associated with the lack of physical symptoms,18,19,27 while others explained that lack of public awareness and knowledge about epilepsy contributed to feelings of being different and their decision to conceal their diagnosis.18,19,27
Relationship Between YWE Perceived Stigma, Self-Disclosure, and Sociodemographic Variables
Only 2 of the 13 studies included in this review examined relationships between perceived stigma, self-disclosure, and sociodemographic variables. In 1 study, higher perceived stigma in YWE was associated with female gender, but not age.20 In contrast, the other study found that higher perceived stigma was associated with younger age (12–16 years vs 17–20 years), but not gender.26 Neither study found associations between self-disclosure, age or gender. In the 1 study that examined associations with SES and race/ethnicity, neither variable was associated with perceived stigma or self-disclosure.26 None of the 13 studies examined associations with sociocultural factors.
Discussion
This systematic review is the first to examine and synthesize the extant literature on perceived stigma and self-disclosure patterns of YWE. The vast majority of the available research is based on qualitative studies. The 3 quantitative studies included in this review used standardized measures of perceived stigma and disclosure20,21,26 and were the only studies to specifically target both perceived stigma and self-disclosure as primary variables. Of the remaining 10 studies, only self-disclosure was included as a primary variable in 4 studies.19,23,27 Stigma has repeatedly been recognized as perpetuating the burden of epilepsy.33 While limited, findings from this systematic review suggest that perceived stigma is a substantial barrier to YWE disclosing their epilepsy to important others outside of their immediate family including peers and teachers, creating barriers to optimal functioning. These findings also demonstrate that despite the significant implications for health and wellness, stigma in pediatric epilepsy has continued to be a relatively neglected area of research.
The following discussion summarizes and expands upon findings related to the primary aims of the study, namely to examine the role of perceived stigma on self-disclosure patterns of YWE. Secondly, we discuss findings from our secondary aims, which examined perceived stigma and self-disclosure among YWE in the context of epilepsy-specific characteristics and sociodemographic factors. Lastly, we consider clinical implications and future directions of the findings from our review.
Perceived-Stigma on YWE Disclosure Patterns
In general, evidence suggests that self-disclosure by YWE is associated with more positive outcomes including greater peer acceptance and better HRQoL.18,21,24 However, consistent with the broader pediatric literature, YWE described disclosure management as a complex process that elicits significant apprehension and uncertainty as multiple factors are considered including to whom to disclose, when to disclose, and weighing potential risks (bullying, loss of friendships, gossiping) and benefits (social and emotional support, increased sense of safety).27 YWE reported contemplating disclosure over multiple weeks as they evaluated an individual’s level of trustworthiness and the potential of the individual accepting them upon disclosure, all the while fearing unintentional disclosure (eg, public seizure).27
Consequently, perceived stigma often resulted in youth making the decision to conceal their epilepsy. The most common reasons for concealment were the desire to maintain a sense of normalcy and to avoid bullying and alienation. As adolescents navigate the developmental task of forming a sense of identity and belongingness, a primary goal is peer acceptance. Thus, disclosure of a stigmatized condition risks disruption of this important developmental task and increases risk for alienation.
Similar to other studies on disclosure by youth with other chronic illnesses, the most common motivators for disclosure among YWE were safety and support. In sharing information with others, YWE described using selective and preventative disclosure strategies. To maximize support and reduce risk for stigma, teasing, and peer rejection, YWE carefully manage information by emphasizing aspects of epilepsy perceived to be less stigmatizing while minimizing or omitting characteristics viewed as more stigmatized.27 YWE were most likely to disclose to a best friend and to others they perceived to be trustworthy and were selective about the information shared based on relationship closeness and personal needs (eg, safety, support, etc). Success in developing social supports using these approaches often resulted in decreased epilepsy-related stress, an increased sense of connection and greater confidence to more fully engage in daily activities.27 Information management also provides YWE a degree of control over their illness and may reinforce a sense of mastery, which is particularly important given the high degree of unpredictability inherent in epilepsy and seizures. In contrast, unplanned disclosure increased the likelihood of peer bullying, loss of friendships, reinforced perceived stigma and feelings of shame, and can undermine a youth’s sense of agency. Given that adolescence is inherently a time of uncertainty and insecurity, caregivers and health providers should help to empower YWE by supporting them in considering to whom, how and what they would like to disclosure.
Disclosure decisions were also driven by the degree of knowledge that YWE had about their condition. Epilepsy is more complex than many other chronic illnesses, contributing to knowledge gaps.22 For instance, some YWE reported that despite wanting to disclose their epilepsy, they felt epilepsy was too complex and that they had insufficient knowledge to explain epilepsy to others, especially their peers.19,28 In these studies, younger children were more likely to struggle with knowledge gaps. However, the extant literature also highlights knowledge gaps among adolescents. For instance, in one study, over one-quarter of adolescents incorrectly answered 76% of questions about their epilepsy. This same study also found that adolescents with lower epilepsy knowledge were less likely to disclosure their epilepsy and more likely to endorse higher perceived stigma.34 For some adolescents, lower levels of knowledge may be a consequence of their attempts to avoid thinking and learning about their epilepsy due to difficulty accepting and coping with their condition. This is supported by research that found 70% of the adolescents with epilepsy reported rarely or never talking to anyone about their condition.26 In addition to navigating the social aspects of epilepsy, adolescence is also a time of many transitions (eg, more time away from home, college, employment, greater illness responsibility, etc). Therefore knowledge gaps and reluctance to disclose epilepsy can increase risk for treatment non-adherence, injury, and lower competencies to effectively manage epilepsy-related challenges. While parents often take the lead during medical appointments, health care providers should also actively engage YWE beginning at an early age to optimize their knowledge and understanding and help dispel misconceptions about epilepsy.
Research to understand the relationship between sociodemographic characteristics, perceived stigma and self-disclosure is limited. Consistent with prior research,10,30 our review found some evidence of higher perceived stigma associated with female gender,20 younger age26 and epilepsy characteristics indicative of more severe epilepsy (higher seizure frequency, polytherapy, and tonic or clonic seizure types).20 Research examining associations between sociodemographic characteristics and self-disclosure are lacking. Overall, few studies considered sociodemographic or epilepsy characteristics and some findings were inconsistent across studies (eg, duration of epilepsy and seizure type), therefore findings should be interpreted with caution. Additional research is needed to better understand which YWE populations are at higher risk for perceived stigma and higher risk for experiencing barriers to disclosure in order to develop tailored interventions to effectively meet their unique needs.
Self-disclosure and perceived stigma are shaped within the context of the broader social environment. Illness invisibility (lack of visible evidence of the illness in the absence of seizures and lack of representation in public domains such as the media) and the general lack of public knowledge, perpetuate misconceptions and negative attitudes towards epilepsy, thus increasing reluctance to disclose.16 Following is a discussion of perceived stigma and self-disclosure in the context of YWE primary social environments. These findings highlight the importance of the social environment in fostering openness, acceptance and safe spaces for YWE to discuss and receive needed supports.
Family Members’ Perceptions Impacting Self-Stigma and Disclosure
Parents are key to helping YWE understand their medical condition and to promoting adjustment to their diagnosis.35 Prior research has found lower levels of parent adaptive coping and more negative parent emotional response to seizures (eg, sadness or anxiety) to be associated with higher levels of parent-reported internalizing and externalizing problems in YWE.36–38 YWE’s health beliefs are also shaped by parent health beliefs and behaviors. For instance, perceived stigma in YWE is strongly influenced by parent stigma coaching, a process by which parental concealment shapes YWE’s conceptualization of epilepsy as a discrediting attribute that should be hidden. Our review found that parent perceived stigma was positively correlated with YWE perceived stigma20 and YWE’s concealment of their condition from others outside of the nuclear family.20 For both YWE and their parents, disclosure of epilepsy outside of the family was associated with more positive family communications about epilepsy,21 whereas concealment was associated with more negative family communication about epilepsy.20
Parent’s reluctance to disclose their child’s epilepsy is commonly associated with fear of other’s negative reactions to disclosure (eg, discrimination and felt-stigma), wanting to seek normalcy for their child, the perceived “invisibility” of epilepsy, poor public understanding of epilepsy, lower perceived illness severity, and poor parental adjustment to child’s illness.39,40 In other research, parents have acknowledged that disclosure can promote greater social acceptance and safety.41 In one longitudinal study, both parent and YWE stigma decreased 2 years post-diagnosis regardless of seizure frequency.42 These findings suggest that for some families, perceived stigma may decrease as they adjust to their child’s epilepsy diagnosis. Perhaps, overtime as family’s knowledge and understanding of their child’s epilepsy increases, YWE’s sense of control and empowerment may also increase. Therefore, as families adjust, both education and practice with disclosing epilepsy to trusted supports may decrease epilepsy-related perceived and enacted stigma.
Peers’ Perceptions Impacting Self-Stigma and Disclosure
Peer relationships throughout childhood and adolescence are an important part of development, with friendships having the potential to buffer both mental health symptoms and stigma.23,28,43–45 When YWE disclose their epilepsy diagnosis to a close and trusted friend, friends most often respond with support and acceptance.23,28,43,44 YWE described that disclosing their epilepsy to a trusted friend resulted in feeling more connected and secure, having a space to process epilepsy-related emotions and stress, decreased worry about the unpredictability of seizures and increased confidence in living life more fully knowing they had someone else watching-out for them.27 Thus, disclosure to a close and trusted friend has the potential to protect against anxiety and mood symptoms.45
However, research has found that general epilepsy knowledge in youth without epilepsy is often limited or completely lacking,46 perpetuating negative attitudes towards and misconceptions about YWE. For instance, in a Nigerian study that assessed peer attitudes towards YWE, only 24% of the peers reported that they would invite YWE to a birthday party, 29% believed their parents would not approve of a friendship with YWE, and 37% reported that their family believed epilepsy should be kept a secret from others.47 YWE are also at higher risk for being bullied, teased, or ostracized by peers.48 Consequently, peer’s negative reactions and attitudes lead to greater concealment and greater social isolation in YWE.44
Educators’ Perceptions Impacting Self-Stigma and Disclosure
Throughout development children regularly interact with educators and peers through the school environment and shared activities.49 The support of teachers in promoting student academic success and positive peer relationships can build self-esteem and self-concept, which may buffer psychosocial stressors related to epilepsy.26 However, epilepsy diagnoses are not consistently disclosed to teachers, most often as a consequence of parent perceived stigma and concern that disclosure would lead to stigmatization and differential treatment at school.50 The decision to conceal an epilepsy diagnosis from school not only places the child at risk for injury but also increases the child’s risk for stigmatization and negative self-perceptions especially if a seizure occurs at school. In fact, in one study about 50% of YWE reported having a seizure at school.28 In our review, YWE often described wishing their teachers had a better understanding of epilepsy so that they could provide better supports.24
Across eight studies conducted in seven different countries, the majority of educators had some knowledge of epilepsy, felt it was treatable, believed that YWE should not be treated differently, and had positive attitudes towards YWE.50–54 A minority of teachers reported misconceptions about epilepsy, which often lead to unnecessary activity restrictions and lack of sufficient academic supports to address epilepsy-related learning difficulties.
Sociocultural Factors Impacting Self-Stigma and Disclosure
Cultural beliefs and social norms within a society can also perpetuate misconceptions about YWE. Throughout certain regions in Asia, Eastern Europe, and Africa, poor knowledge of epilepsy’s cause and course leads to misconceptions about epilepsy.55–57 Reported epilepsy causes include psychiatric illness in Georgia,57 paranormal or spiritual in Iran (ie, djinn or “evil eye”)56 and Nigeria (ie, demonic possession, family curse),55 and “mad pig disease” in Lao People’s Democratic Republic,58 with some believing that the course of epilepsy is incurable or transmissible and life-limiting.58,59 Insufficient knowledge and understanding of epilepsy,59 low socioeconomic status, seeking traditional medicine rather than evidence-based medical treatment, and insufficient education about epilepsy provided to YWE by their parents can negatively impact treatment seeking behaviors of families with YWE.59,60
However, there is also variability in perceived stigma across and within regions. For instance, in a study involving 16 European countries, 23% of the parents concealed their child’s epilepsy diagnosis,61 whereas in a more recent study conducted in India, over 92% of the parents reported disclosing their child’s epilepsy diagnosis to extended family members and teachers.41 Cultural beliefs related to epilepsy are also apparent in schools. For instance, 40% of the teachers in Ethiopia felt YWE had lower intelligence, 28% felt YWE experienced behavioral issues, and 15% preferred YWE to be in special education rather than mainstream classes.52 Despite high education level, teachers with poorer knowledge of epilepsy tended to have greater misconceptions based on cultural beliefs (eg, epilepsy is contagious, due to spirit possession, or witchcraft).54 On the contrary, teachers with higher knowledge of epilepsy showed greater tolerance and less stigmatizing practices in the classroom setting.54 However, even with higher knowledge and awareness of epilepsy, some educators reported that they would not allow their children to associate with YWE52 or marry someone with epilepsy.54
Clinical Implications
Findings from this study reinforce previous research elucidating positive associations between perceived stigma and concealment of epilepsy as well as highlight some of the concerns specific to YWE. YWE’s concealment of their epilepsy diagnosis perpetuates stigma and reinforces the cycle of invisibility surrounding epilepsy. This in turn decreases access to the supports (eg, family, friends, teachers) and resources (eg, academic accommodations, extra-curricular activities, treatments) that are critical to YWE optimally navigating the formative adolescent years that shape current and future outcomes. Based on the existing literature, interventions that target knowledge and awareness of epilepsy and social supports have promise. Greater levels of knowledge and understanding of epilepsy are associated with lower levels of perceived and enacted stigma. Similarly, peer acceptance and engagement have been identified as protective against stigma and negative psychosocial outcomes.45
However, in order to effectively mitigate the detrimental effects of stigma on outcomes in YWE, multi-level stigma reduction interventions are needed to address stigma at the intrapersonal (YWE), interpersonal (peers, family), community (culture practices and beliefs, public), institutional (school) and governmental levels (policy). For instance, at the intrapersonal level developmentally appropriate approaches should be used during clinic visits to engage YWE in care plan discussions. For adolescents with epilepsy, media-based educational resources may be particularly salient. Increasing YWE’s understanding of their condition may empower them to educate others including peers and potentially increase social supports. Further, peer support groups for YWE have been shown to decrease internalized stigma.62 YWE can be connected to peer support groups through programming such as support groups, camps, and other activities offered through local epilepsy organizations such as the Epilepsy Alliance and Epilepsy Foundation.
At the interpersonal level, educational interventions targeting families of YWE have shown promise and have demonstrated improvements in caregiver’s ability to effectively advocate for their child’s psychosocial needs63 as well as decreased epilepsy-related anxiety and increased competence and knowledge in both YWE and their caregivers.63,64 Educational interventions targeting peers have also resulted in positive outcomes including improved epilepsy-related knowledge, positive changes in attitudes about epilepsy, and decreases in epilepsy-related stigma in peers across age groups ranging from school-aged65–69 to college.70,71
At the community and institutional levels, interventions have targeted teachers, health care professionals, and the general public. Epilepsy-focused didactic and training interventions targeting teachers have been found to improve educator’s epilepsy knowledge72,73 and attitudes toward epilepsy.72 However, at post-intervention, negative attitudes towards epilepsy remained stable for educators with negative attitudes at baseline, despite improved epilepsy knowledge.73 Among health care professionals, educational epilepsy seminars have shown improvement in staff members’ epilepsy knowledge and attitudes toward epilepsy. From a more general public health perspective, public awareness campaigns for epilepsy have shown evidence of reduced epilepsy-related stigma, improved epilepsy knowledge and more positive attitudes among the public as well as decreased memory difficulties, psychosocial issues, and seizure-related worry in PWE.74
Epilepsy impacts youth across the globe, but disproportionately affects youth from minority and low-income backgrounds.33 Therefore, interventions developed in the context of a person-centered framework will be key to developing and implementing culturally sensitive treatments that can effectively address the combined effects of intersecting forms of stigma (eg, race, class/SES, gender sexual orientation, and disability) experienced by YWE.33 Addressing stigma will be most effective through the engagement and collaboration with influential community leaders and PWE.
Limitations
There are several noteworthy limitations of this review. First, the vast majority of research reviewed in this study employed qualitative methodologies which provided more nuanced insight into the lived experiences of YWE but limits generalizability outside of the individual studies. Among the limited number of quantitative studies included in this review, there was heterogeneity in the utilized measurement instruments limiting generalizability and prohibiting comparisons between studies. Second, there was variability between studies in how perceived stigma and disclosure were conceptualized with only a few studies intentionally targeting our primary variables of interest. Third, across studies there was limited data reported on sociodemographic variables, particularly in qualitative research. Fourth, it is estimated that nearly 80% of PWE live in low- and middle-income countries where treatment gaps are greater than 75%.33 However, all of the studies included in this review were limited to three regions of the world, namely, East Asia and Pacific, Europe and Central Asia, and North America, all representing high- and growing income regions. Thus, findings may not reflect the YWE disproportionally affected by perceived stigma. Fifth, all studies were cross-sectional, thus limiting determinations about causality.
Conclusions
Globally, stigma has been identified as a significant barrier to optimal outcomes in PWE. Over the past two decades, efforts to eliminate epilepsy-related stigma have been at the forefront and have been hallmarks of national and global initiatives. While progress has been made on these fronts, this review highlights that much work is still needed, especially among children and youth. As YWE struggle to cope with and adjust to epilepsy, they often conceal their diagnosis as a consequence of perceived stigma such as worry about discrimination, social exclusion, and differential treatment. YWE especially worry about potential negative reactions from their peers, which can result in YWE limiting social activities and avoiding talking about their epilepsy with others outside of the home. These efforts to conceal epilepsy can limit opportunities for gaining important emotional, social, and functional supports (eg, academic and occupational accommodations), which can in turn, increase YWE’s risk for social isolation, lower self-esteem, lower quality of life, greater emotional and behavioral difficulties, academic underachievement and decrease future socio-economic opportunity. Adolescence is a pivotal stage of development, wherein self-concept is developed and schemas related to the self and others are created and carried over into adulthood. In order to help YWE build a positive sense of self and adaptive illness coping, a multi-system, integrative approach will be required to build effective epilepsy education programs to reduce perceived stigma. Furthermore, future research should also include a focus on socio-cultural factors that may perpetuate stigma and can help inform adaptation of interventions to meet the unique needs of YWE across different regions across the globe.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Olusanya BO, Wright SM, Nair MKC, et al. Global burden of childhood epilepsy, intellectual disability, and sensory impairments. Pediatrics. 2020;146(1):e20192623. doi:10.1542/peds.2019-2623
2. Aaberg KM, Bakken IJ, Lossius MI, et al. Comorbidity and childhood epilepsy: a nationwide registry study. Pediatrics. 2016;138(3). doi:10.1542/peds.2016-0921
3. Dunn DW, Johnson CS, Perkins SM, et al. Academic problems in children with seizures: relationships with neuropsychological functioning and family variables during the 3 years after onset. Epilepsy Behav. 2010;19(3):455–461. doi:10.1016/j.yebeh.2010.08.023
4. Clary LE, Vander Wal JS, Titus JB. Examining health-related quality of life, adaptive skills, and psychological functioning in children and adolescents with epilepsy presenting for a neuropsychological evaluation. Epilepsy Behav. 2010;19(3):487–493. doi:10.1016/j.yebeh.2010.08.002
5. Reynolds EH. The ILAE/IBE/WHO epilepsy global campaign history. International League Against Epilepsy. International Bureau for Epilepsy. Epilepsia. 2002;43(Suppl 6):9–11. doi:10.1046/j.1528-1157.43.s.6.5.x
6. Goffman E. Stigma: Notes on the Management of Spoiled Identity. Simon and Schuster; 1963.
7. Scambler G, Hopkins A. Being epileptic: coming to terms with stigma. Sociol Health Illn. 1986;8(1):26–43. doi:10.1111/1467-9566.ep11346455
8. Weiss MG, Utzinger J. Stigma and the social burden of neglected tropical diseases. PLoS Negl Trop Dis. 2008;2(5):e237. doi:10.1371/journal.pntd.0000237
9. Fisher RS. Epilepsy from the patient’s perspective: review of results of a community-based survey. Epilepsy Behav. 2000;1(4):S9–S14. doi:10.1006/ebeh.2000.0107
10. Kwon CS, Jacoby A, Ali A, et al. Systematic review of frequency of felt and enacted stigma in epilepsy and determining factors and attitudes toward persons living with epilepsy-report from the International League Against Epilepsy Task Force on Stigma in Epilepsy. Epilepsia. 2022;63(3):573–597. doi:10.1111/epi.17135
11. Patton GC, Sawyer SM, Santelli JS, et al. Our future: a Lancet commission on adolescent health and wellbeing. Lancet. 2016;387(10036):2423–2478. doi:10.1016/S0140-6736(16)00579-1
12. Somerville LH. Special issue on the teenage brain: sensitivity to social evaluation. Curr Dir Psychol Sci. 2013;22(2):121–127. doi:10.1177/0963721413476512
13. MacLeod JS, Austin JK. Stigma in the lives of adolescents with epilepsy: a review of the literature. Epilepsy Behav. 2003;4(2):112–117. doi:10.1016/s1525-5050(03)00007-6
14. Greene K. An integrated model of health disclosure decision-making. In: Uncertainty, Information Management, and Disclosure Decisions. Routledge; 2015:242–269.
15. Lambert V, Gallagher P, O’Toole S, Benson A. Stigmatising feelings and disclosure apprehension among children with epilepsy. Nurs Child Young People. 2014;26(6):22–26. doi:10.7748/ncyp.26.6.22.e440
16. Wilde M, Haslam C. Living with epilepsy: a qualitative study investigating the experiences of young people attending outpatients clinics in Leicester. Seizure. 1996;5(1):63–72. doi:10.1016/s1059-1311(96)80065-3
17. Eklund PG, Sivberg B. Adolescents’ lived experience of epilepsy. J Neurosci Nurs. 2003;35(1):40–49. doi:10.1097/01376517-200302000-00008
18. Lewis A, Parsons S. Understanding of epilepsy by children and young people with epilepsy. Eur J Spec Needs Educ. 2008;23(4):321–335. doi:10.1080/08856250802387273
19. Benson A, Lambert V, Gallagher P, Shahwan A, Austin JK. ”I don’t want them to look at me and think of my illness, I just want them to look at me and see me”: child perspectives on the challenges associated with disclosing an epilepsy diagnosis to others. Epilepsy Behav. 2015;53:83–91. doi:10.1016/j.yebeh.2015.09.026
20. Benson A, O’Toole S, Lambert V, Gallagher P, Shahwan A, Austin JK. The stigma experiences and perceptions of families living with epilepsy: implications for epilepsy-related communication within and external to the family unit. Patient Educ Couns. 2016;99(9):1473–1481. doi:10.1016/j.pec.2016.06.009
21. Benson A, Lambert V, Gallagher P, O’Toole S, Shahwan A, Austin JK. Development and psychometric evaluation of the youth and parent versions of the Epilepsy Disclosure Scale (EDS). Epilepsy Behav. 2018;82:111–118. doi:10.1016/j.yebeh.2018.02.015
22. Houston EC, Cunningham CC, Metcalfe E, Newton R. The information needs and understanding of 5–10-year old children with epilepsy, asthma or diabetes. Seizure. 2000;9(5):340–343. doi:10.1053/seiz.2000.0416
23. Jeschke S, Woltermann S, Neininger MP, et al. Why do children and adolescents with epilepsy disclose or not disclose their condition to their friends? Eur J Pediatr. 2020;179(10):1627–1633. doi:10.1007/s00431-020-03661-0
24. Moffat C, Dorris L, Connor L, Espie CA. The impact of childhood epilepsy on quality of life: a qualitative investigation using focus group methods to obtain children’s perspectives on living with epilepsy. Epilepsy Behav. 2009;14(1):179–189. doi:10.1016/j.yebeh.2008.09.025
25. Ronen GM, Rosenbaum P, Law M, Streiner DL. Health-related quality of life in childhood epilepsy: the results of children’s participation in identifying the components. Dev Med Child Neurol. 1999;41(8):554–559. doi:10.1017/S0012162299001176
26. Westbrook LE, Bauman LJ, Shinnar S. Applying stigma theory to epilepsy: a test of a conceptual model. J Pediatr Psychol. 1992;17(5):633–649. doi:10.1093/jpepsy/17.5.633
27. Sheridan K, Salmon N, O’Connell N. Experiences of university students disclosing epilepsy to peers: ‘It’s a shared thing now’. Br J Occup Ther. 2016;79(8):484–491. doi:10.1177/0308022616638672
28. Chew J, Carpenter J, Haase AM. Living with epilepsy in adolescence-a qualitative study of young people’s experiences in Singapore: peer socialization, autonomy, and self-esteem. Child Care Health Dev. 2019;45(2):241–250. doi:10.1111/cch.12648
29. Austin JK, Perkins SM, Dunn DW. A model for internalized stigma in children and adolescents with epilepsy. Epilepsy Behav. 2014;36:74–79. doi:10.1016/j.yebeh.2014.04.020
30. Heimlich TE, Westbrook LE, Austin JK, Cramer JA, Devinsky O. Brief report: adolescents’ attitudes toward epilepsy: further validation of the Child Attitude Toward Illness Scale (CATIS). J Pediatr Psychol. 2000;25(5):339–345. doi:10.1093/jpepsy/25.5.339
31. Austin JK, Huberty TJ. Development of the child attitude toward illness scale. J Pediatr Psychol. 1993;18(4):467–480. doi:10.1093/jpepsy/18.4.467
32. Jeschke S, Woltermann S, Neininger MP, et al. Interviews with patients aged 6–17 years provide valuable insights for physicians who need to deliver an epilepsy diagnosis. Acta Paediatr. 2021;110(5):1556–1561. doi:10.1111/apa.15672
33. World Health Assembly (75th session). Follow-up to the political declaration of the third high-level meeting of the General Assembly on the prevention and control of non-communicable diseases: draft intersectional global action plan on epilepsy and other neurological disorders 2022–2031. 2022.
34. Ryu HU, Lee SA, Eom S, Kim HD. Perceived stigma in Korean adolescents with epilepsy: effects of knowledge about epilepsy and maternal perception of stigma. Seizure. 2015;24:38–43. doi:10.1016/j.seizure.2014.11.010
35. Mendes TP, Crespo CA, Austin JK. Family cohesion, stigma, and quality of life in dyads of children with epilepsy and their parents. J Pediatr Psychol. 2017;42(6):689–699. doi:10.1093/jpepsy/jsw105
36. Austin JK, MacLeod J, Dunn DW, Shen J, Perkins SM. Measuring stigma in children with epilepsy and their parents: instrument development and testing. Epilepsy Behav. 2004;5(4):472–482. doi:10.1016/j.yebeh.2004.04.008
37. Austin JK, Haber LC, Dunn DW, Shore CP, Johnson CS, Perkins SM. Children with new onset seizures: a prospective study of parent variables, child behavior problems, and seizure occurrence. Epilepsy Behav. 2015;53:73–77. doi:10.1016/j.yebeh.2015.09.019
38. Carlton-Ford S, Miller R, Nealeigh N, Sanchez N. The effects of perceived stigma and psychological over-control on the behavioural problems of children with epilepsy. Seizure. 1997;6(5):383–391. doi:10.1016/s1059-1311(97)80038-6
39. Benson A, Lambert V, Gallagher P, Shahwan A, Austin JK. Parent perspectives of the challenging aspects of disclosing a child’s epilepsy diagnosis to others: why don’t they tell? Chronic Illn. 2017;13(1):28–48. doi:10.1177/1742395316648749
40. Elafros MA, Sakubita-Simasiku C, Atadzhanov M, Haworth A, Chomba E, Birbeck GL. Stigma and psychiatric morbidity among mothers of children with epilepsy in Zambia. Int Health. 2013;5(4):288–294. doi:10.1093/inthealth/iht028
41. Lachake AV, Desai N, Udani V. ‘To reveal or to conceal’- disclosure strategies in parents of children with epilepsy in India. Seizure. 2021;91:507–512. doi:10.1016/j.seizure.2021.07.026
42. Rood JE, Schultz JR, Rausch JR, Modi AC. Examining perceived stigma of children with newly-diagnosed epilepsy and their caregivers over a two-year period. Epilepsy Behav. 2014;39:38–41. doi:10.1016/j.yebeh.2014.08.004
43. Admi H, Shaham B. Living with epilepsy: ordinary people coping with extraordinary situations. Qual Health Res. 2007;17(9):1178–1187. doi:10.1177/1049732307307548
44. Elliott IM, Lach L, Smith ML. I just want to be normal: a qualitative study exploring how children and adolescents view the impact of intractable epilepsy on their quality of life. Epilepsy Behav. 2005;7(4):664–678. doi:10.1016/j.yebeh.2005.07.004
45. Engel ML, Shanley R, Scal PB, Kunin-Batson A. Anxiety and depressive symptoms in adolescents and young adults with epilepsy: the role of illness beliefs and social factors. Epilepsy Behav. 2021;116:107737. doi:10.1016/j.yebeh.2020.107737
46. Fernandes PT, Cabral P, Araújo U, Noronha AL, Li LM. Kids’ perception about epilepsy. Epilepsy Behav. 2005;6(4):601–603. doi:10.1016/j.yebeh.2005.02.011
47. Ani C, Ola BA, Coker R. School children’s stigmatising attitude towards peers with epilepsy in Nigeria. Vulnerable Child Youth Stud. 2011;6(4):330–338. doi:10.1080/17450128.2011.630491
48. Bellon M, Walker C, Peterson C, Cookson P. The “E” word: epilepsy and perceptions of unfair treatment from the 2010 Australian Epilepsy Longitudinal Survey. Epilepsy Behav. 2013;27(1):251–256. doi:10.1016/j.yebeh.2013.01.016
49. Bronfenbrenner U, Morris PA. The bioecological model of human development. In: Handbook of Child Psychology. John Wiley \& Sons, Inc; 2007.
50. Kampra M, Tzerakis NG, Losidis S, et al. Teachers’ knowledge about epilepsy in Greece: information sources and attitudes towards children with epilepsy during school time. Epilepsy Behav. 2016;60:218–224. doi:10.1016/j.yebeh.2016.04.004
51. Alzhrani SH, AlSufyani MH, Abdullah RI, Almalki S. School teacher's knowledge, attitudes, and practice toward student with epilepsy in Taif, Saudi Arabia: cross-sectional study. J Family Med Prim Care. 2021;10(7):2668–2678. doi:10.4103/jfmpc.jfmpc_2087_20
52. Berhe T, Yihun B, Abebe E, Abera H. Knowledge, attitude, and practice about epilepsy among teachers at Ethio-National School, Addis Ababa, Ethiopia. Epilepsy Behav. 2017;70(Pt A):150–153. doi:10.1016/j.yebeh.2017.02.009
53. Al-Harbi AF, Alsaid LA, Parameaswari PJ. Primary school female teachers’ knowledge, attitude, and practice toward students with epilepsy in Riyadh, Saudi Arabia. J Family Med Prim Care. 2018;7(2):331–336. doi:10.4103/jfmpc.jfmpc_58_18
54. Birbeck GL, Chomba E, Atadzhanov M, Mbewe E, Haworth A. Zambian teachers: what do they know about epilepsy and how can we work with them to decrease stigma? Epilepsy Behav. 2006;9(2):275–280. doi:10.1016/j.yebeh.2006.06.005
55. Asindi AA, Eyong KI. Stigma on Nigerian children living with epilepsy. J Pediatr Neurol. 2012;10(02):105–109. doi:10.3233/JPN-2012-0554
56. Kolahi AA, Abbasi-Kangevari M, Bakhshaei P, Mahvelati-Shamsabadi F, Tonekaboni SH, Farsar AR. Knowledge, attitudes, and practices among mothers of children with epilepsy: a study in a teaching hospital. Epilepsy Behav. 2017;69:147–152. doi:10.1016/j.yebeh.2016.10.018
57. Gzirishvili N, Kasradze S, Lomidze G, et al. Knowledge, attitudes, and stigma towards epilepsy in different walks of life: a study in Georgia. Epilepsy Behav. 2013;27(2):315–318. doi:10.1016/j.yebeh.2013.02.011
58. Barennes H, Sengkhamyong K, Sambany EM, et al. Children’s access to treatment for epilepsy: experience from the Lao People’s Democratic Republic. Arch Dis Child. 2011;96(3):309–313. doi:10.1136/adc.2009.181255
59. El Sharkawy G, Newton C, Hartley S. Attitudes and practices of families and health care personnel toward children with epilepsy in Kilifi, Kenya. Epilepsy Behav. 2006;8(1):201–212. doi:10.1016/j.yebeh.2005.09.011
60. Hirfanoglu T, Serdaroglu A, Cansu A, Soysal AS, Derle E, Gucuyener K. Do knowledge of, perception of, and attitudes toward epilepsy affect the quality of life of Turkish children with epilepsy and their parents? Epilepsy Behav. 2009;14(1):71–77. doi:10.1016/j.yebeh.2008.08.011
61. Baker GA, Spector S, McGrath Y, Soteriou H. Impact of epilepsy in adolescence: a UK controlled study. Epilepsy Behav. 2005;6(4):556–562. doi:10.1016/j.yebeh.2005.03.011
62. Elafros MA, Mulenga J, Mbewe E, et al. Peer support groups as an intervention to decrease epilepsy-associated stigma. Epilepsy Behav. 2013;27(1):188–192. doi:10.1016/j.yebeh.2013.01.005
63. Maya Kaye A. Pediatric epilepsy and psychoeducational interventions: a review of the literature. Epilepsy Behav. 2021;121(Pt A):108084. doi:10.1016/j.yebeh.2021.108084
64. Lewis MA, Hatton CL, Salas I, Leake B, Chiofalo N. Impact of the Children’s Epilepsy Program on parents. Epilepsia. 1991;32(3):365–374. doi:10.1111/j.1528-1157.1991.tb04665.x
65. Brabcova D, Lovasova V, Kohout J, Zarubova J, Komarek V. Improving the knowledge of epilepsy and reducing epilepsy-related stigma among children using educational video and educational drama--a comparison of the effectiveness of both interventions. Seizure. 2013;22(3):179–184. doi:10.1016/j.seizure.2012.11.017
66. Brabcová D, Kohout J, Weberová V, Komárek V. Educational video and story as effective interventions reducing epilepsy-related stigma among children. Epilepsy Behav. 2017;69:12–17. doi:10.1016/j.yebeh.2017.01.019
67. Brabcova DB, Belohlavkova A, Kohout J, Ebel M, Rokytova J, Krsek P. Psychometric properties of the Czech versions of the Impact of Pediatric Epilepsy Scale (IPES) and quality of life in epilepsy inventory for adolescents (QOLIE-AD-48). Epilepsy Behav. 2021;114(PtA):107629. doi:10.1016/j.yebeh.2020.107629
68. Gebrewold MA, Enquselassie F, Teklehaimanot R, Gugssa SA. Ethiopian teachers: their knowledge, attitude and practice towards epilepsy. BMC Neurol. 2016;16(1):167. doi:10.1186/s12883-016-0690-4
69. Martiniuk AL, Speechley KN, Secco M, Campbell MK, Donner A. Evaluation of an epilepsy education program for Grade 5 students: a cluster randomized trial. Epilepsy Behav. 2007;10(4):604–610. doi:10.1016/j.yebeh.2007.03.009
70. Roberts RM, Farhana HS. Effectiveness of a first aid information video in reducing epilepsy-related stigma. Epilepsy Behav. 2010;18(4):474–480. doi:10.1016/j.yebeh.2010.06.004
71. Cicero CE, Giuliano L, Todaro V, et al. Comic book-based educational program on epilepsy for high-school students: results from a pilot study in the Gran Chaco region, Bolivia. Epilepsy Behav. 2020;107:107076. doi:10.1016/j.yebeh.2020.107076
72. Bozkaya IO, Arhan E, Serdaroglu A, Soysal AS, Ozkan S, Gucuyener K. Knowledge of, perception of, and attitudes toward epilepsy of schoolchildren in Ankara and the effect of an educational program. Epilepsy Behav. 2010;17(1):56–63. doi:10.1016/j.yebeh.2009.10.011
73. Mecarelli O, Messina P, Capovilla G, et al. An educational campaign about epilepsy among Italian primary school teachers. 2. The results of a focused training program. Epilepsy Behav. 2015;42:93–97. doi:10.1016/j.yebeh.2014.07.022
74. Giuliano L, Cicero CE, Padilla S, et al. Knowledge, stigma, and quality of life in epilepsy: results before and after a community-based epilepsy awareness program in rural Bolivia. Epilepsy Behav. 2019;92:90–97. doi:10.1016/j.yebeh.2018.11.036
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
