Back to Journals » Patient Preference and Adherence » Volume 16
Prevalence and Determinants of Antibiotic Self-Administration Among Adult Antibiotic Users: A Cross-Sectional Study
Authors Kabir H , Hasan MK , Tutul AH, Islam MS , Jamil S , Das BC, Islam MF , Jannat H , Ara R, Akter O, Biswas L, Miah ME, Mitra DK
Received 4 May 2022
Accepted for publication 29 July 2022
Published 1 September 2022 Volume 2022:16 Pages 2409—2421
DOI https://doi.org/10.2147/PPA.S372501
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Johnny Chen
Humayun Kabir,1,* Md Kamrul Hasan,1,2,* Ariful Haque Tutul,3,* Mohammad Shahidul Islam,3,* Safayet Jamil,4 Bikash Chandra Das,1 Md Fakrul Islam,1 Hasina Jannat,1 Rawshan Ara,5 Ojifa Akter,6 Lila Biswas,7 Md Ebrahim Miah,6,8 Dipak Kumar Mitra1
1Department of Public Health, North South University, Dhaka, 1229, Bangladesh; 2Department of Biochemistry and Molecular Biology, Tejgaon College, Dhaka, 1215, Bangladesh; 3Dhaka Medical College and Hospital, Dhaka, 1000, Bangladesh; 4Department of Pharmacy, Khwaja Yunus Ali University, Sirajganj, 6751, Bangladesh; 5Prime College of Nursing, Dhaka, 1229, Bangladesh; 6School of Medical Sciences, Shahjalal University of Science & Technology, Sylhet, 3114, Bangladesh; 7Department of Nursing, CRP Nursing College, Savar, 1343, Bangladesh; 8Institute of Social Welfare and Research, University of Dhaka, Dhaka, 1000, Bangladesh
*These authors contributed equally to this work
Correspondence: Humayun Kabir; Md Kamrul Hasan, Department of Public Health, North South University, Dhaka, 1229, Bangladesh, Tel +880 1785811449; +880 1684867565, Email [email protected]; [email protected]
Introduction: Each year, antibiotics save hundreds of thousands of lives; nonetheless, antibiotic self-administration is a major concern all over the world. This study aimed to investigate the prevalence of antibiotic self-administration among two-month adult antibiotic users as well as the factors contributing to this prevalence.
Method and Participants: This cross-sectional study was conducted among 295 Bangladeshi adults between May 22nd and June 15th, 2021, during the COVID-19 pandemic. Descriptive statistics included frequency distribution, while inferential statistics included the Pearson chi-square test. For data analysis, the statistical software STATA-16 was used.
Results: In this study, the prevalence of antibiotic self-administration was 17.97%. Antibiotic self-administration was found to be significantly more prevalent among those who were unable to take antibiotic on time, incomplete doses, did not know over prescriptions may cause antibiotic resistance, and could not correctly recognize amoxicillin and azithromycin are antibiotics.
Conclusion: Due to the increased rate of antibiotic self-administration among adults in Bangladesh, the responsible authority should give more attention towards the factors responsible for antibiotic self-administration and revise their current policy to ensure the safe and effective use of antibiotics.
Keywords: antibiotic, self-administration, antibiotic resistance, Bangladesh
Introduction
When people use medicines to alleviate illnesses or symptoms that they have recognized on their own, or when they use a prescribed drug consistently or long-term to treat chronic or recurring diseases or symptoms, this phenomenon is referred to as self-medication.1 Obtaining pharmaceuticals without a prescription, resubmitting old prescriptions to purchase medications, exchanging medication information with friends or family members, and using unnecessary pills kept at home are all common examples of self-medication.2 Nowadays, self-medication is becoming more common in developing countries, and antibiotic along with other drugs, are more widely self-administering.3
Antibiotic self-administration is a significant concern for people all around the world. Since their discovery, antibiotic saved and continue to save hundreds of thousands of lives each year.4 Nowadays, numerous consumers utilize antibiotics, and the demand is constantly rising nearly every day.4 According to a systematic review and meta-analysis, between 26.2% and 92% of people self-administered antibiotic.5 The figure was 38.5% among the Ethiopian university students.6 In Southwestern Nigeria, antibiotic self-administration was 53.8% among students.6 A recent study in Jordan, which indicated that 67.1% adults thought antibiotics could help them with common cold and cough symptoms.7 Gillani et al, reported that in developing countries, the rate of antibiotic self-use was higher in developed countries, with 3% in Europe and 4–75% in Asia.8 It was widespread in neighboring countries, India and Nepal.3 Disparities in socioeconomic status and cultural factors were reported as responsible determinants for the outcome.
Antibiotic self-administration poses a severe health hazard in various ways, and it may raise the burden of healthcare disparity. The issues surrounding self-medication with antibiotics are exacerbated in the developing world because they are combined with other problems such as poverty, lack of access to medications and knowledge about prescription medications, poor quality of health care facilities, and ineffective enforcement of medicine-related legislation.9–11 According to a previous survey conducted in Italy, merely 9.8% of the general population recognized antibiotic, while 21.3% comprehended how to use them efficiently.8
Antibiotic resistance, however, has emerged as a global problem as the use of antibiotic among citizens has increased substantially. Antibiotic resistance acquires if antibiotic are consistently self-administered.12 Antibiotic resistance has resulted in a terrible spike in the medical sector and the burden of the disease that is currently difficult to cope with in developing countries.1 Besides, O’Neill predicted that antibiotic-resistant bacteria are supposed to induce around 10 million deaths each year by 2050.13
In Bangladesh, the antibiotic resistance was only familiar to 56.1% of population, while 20.5% was self-administrated.10 There may be a lack of awareness and concerns regarding the harmful consequences of antibiotic self-administering and associated complications such as antibiotic resistance. Even though the government prohibits antibiotic without prescription, due to the lack of enforcement of anti-antibiotic legislation, non-prescription antibiotic use is rampant.14
As a developing country, the vast majority of the population is still inaccessible to compact healthcare facilities in Bangladesh.15 Besides, patients are urged to purchase antibiotic from unlicensed suppliers because many medicines are not always available at official facilities.4 According to Hoque et al, the extensive purchase of antimicrobials without a prescription in Bangladesh resulted in increased irrational overuse, degradation of the ecology, and the propagation of resistance.14 Furthermore, many individuals, particularly the impoverished, rely heavily on unlicensed healthcare practitioners, many of whom may be unprepared to deliver professional, high-quality health care to the general population.16 On the other hand, the rural people of Bangladesh have uncontrolled access to non-prescribed pharmaceuticals and nutritional supplements.4
Despite the fact that antibiotic self-administration in Bangladesh may escalate, there has not been enough study conducted to determine the factors responsible for the phenomenon. As a result of antibiotic self-administration activities, several unanswered questions have arisen, including association with demography, knowledge of antibiotic, and antibiotic resistance. This study intended to investigate the prevalence of antibiotic self-administration within two-month adults antibiotic users and identify the determinants of antibiotic self-administration.
Methods and Materials
Study Design, Setting, and Participants
This cross-sectional study was conducted during the COVID-19 pandemic by using available online platforms in Bangladesh between 22nd May 2021 and 15th June 2021 among 295 adult antibiotic users. The criteria of the study participants were explained in the first page of the questionnaire. The inclusion criteria include (a) took antibiotic within the last two months of study participation, (b) age was at least 18 years, and (c) willing to participate. The exclusion criteria include (a) provided incomplete responses and (b) not provided online consent.
Required Sample Size
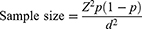
In 2018, Tasnuva Ferdous conducted a descriptive study among students in Dhaka and Gazipur district, Bangladesh and reported the prevalence of antibiotic self-administration within one year was 83.98%.17 Based on following formula18 and the recent prevalence, our required sample size was 207 at 80% power, 95% CI of 0.05 to 1.96, and an effect size of 5%. As we intended to include more samples to minimize the effect size, an additional 88 sample was included.
[Here: p = recent prevalence, Z= Z-score, d = effect size].
Questionnaire Development, Sampling, and Data Collection
Trained research assistants were assigned for data collection, and the notable name of the research assistants can be found in the Supplementary Table S1. However, a structured questionnaire was developed for data collection based on the literature review.1,8,19–29 For content validity, the questionnaire was reviewed by two public health experts in Bangladesh. Based on their suggested modifications, the questionnaire was developed. Besides, the questionnaire was pretested among 15 participants prior to data collection, and these 15 participants were not included in the final study. After minor modifications, the final questionnaire was transferred to “Google Form” to develop an online version. By using the online questionnaire, data was collected based on convenient and snowball sampling strategies. The research assistants shared the link of the online version questionnaire on the following social media sites: Facebook, LinkedIn, WhatsApp, and Twitter. In addition, the assistants requested their friends, relatives, and followers connected by social media to provide data before checking their eligibility criteria. 295 completed responses were accepted for data analysis after excluding 26 incomplete responses from the total of 321 responses.
Study Variables
The outcome variable of the study was antibiotic self-administration within the last two months, measured by responding to “Yes” or “No”. The exploratory variables included sociodemographic variables (age, sex, marital status, residence, and educational level), antibiotic administration related variables (antibiotic taking frequency, whether they took antibiotic at the proper time, whether they completed the doses, and whether their problem has been resolved), antibiotic resistance related variables (ever heard of antibiotic resistance, either antibiotic resistance may occur due to incomplete dose, over-prescription, use in livestock and fish, and overuse of sanitizers), and antibiotic specification related variables (either they could correctly specify antibiotic from list of anti-microbials such as Amoxicillin, Cefixime, Azithromycin, Remdesivir, and Abendazole).
Bias
Due to the application of convenient and snowball sampling strategies, and the utilization of the online data collection technique, the selection bias might have occurred in this study. Moreover, because the self-reported questionnaire was used, the response bias was also possible to happen.
Data Analysis and Software
As the nature of data collection for this study, data were automatically entered into an online Excel spreadsheet. The data was then cleaned in an Excel file, with only the completed responses were kept and entered into the statistical software. The statistical software STATA-16 was used for data analysis, and Prism 8.0 was used to draw the figures. The descriptive and inferential statistics were performed, whereas descriptive statistics include frequency distribution and the inferential statistics include the Pearson chi-square test. At the 95% confidence interval, the p-value <0.05 was considered statistically significant.
Ethical Issue
The confidentiality of the participants and the objectives of the study were outlined on the first page of the questionnaire. The first item on the questionnaire (“Yes” or “No”) asked participants whether they were willing to participate or not. Those who chose “Yes” were permitted to receive the questionnaire and submit it along with their self-responses. Those who chose “No” were automatically sent out questionnaire with no responses. The Ethical Review Committee of the Tejgaon College, Dhaka-1215, Bangladesh, approved the study. The reference number is 2021/OR-TGC/0201. The research was carried out in compliance with the Helsinki Declaration.30
Results
Background Characteristics of the Study Participants
The study participants’ background characteristics are presented in Table 1. The majority (57.97%) were between the ages of 20 and 29 years, and nearly half (52.20%) were female. In more than half of the cases (58.64%), their marital status was unmarried. From the urban area, 85.76% participated, and nearly 80% of them were higher secondary passed to graduated. In this study, the prevalence of antibiotic self-administration was 17.97%.
 |
Table 1 Background Characteristics of the Study Participants (n = 295) |
Background Characteristics by Antibiotic Self-Administration
The participants’ background characteristics by antibiotic self-administration are presented in Table 2. Self-administration of antibiotic was found to be the highest among the youngest (20 years old) (34.78%). Self-administration was higher among females than males (21.43% vs 14.18%). Unmarried participants (20.23% vs 14.75%) were more likely to self-administer antibiotic, and so were the rural residents (23.81% vs 17.00%).
 |
Table 2 Background Characteristics by Antibiotic Self-Administration (n = 295) |
Antibiotic Administration Related Variables and Antibiotic Self-Administration
In this study population, 27% took antibiotic within two months more than once, 85.08% took antibiotic timely, 80% completed the doses, and 12.20% of their problem was reported to be unsolved. The overall distribution of the antibiotic administration related variables is illustrated in Figures 1 and 2. The antibiotic administration related variables by antibiotic self-administration are presented in Table 3. When participants took antibiotic more than once, self-administration was found to be greater (22.37% vs 16.34%). Self-administration was found to be significantly more prevalent in those who were unable to take antibiotic at proper time (38.64% vs 14.34%, p <0.001). Self-administration was also significantly more frequent among failures to doses (35.59% vs 13.56%, p <0.001). Antibiotic self-administration was higher in those whose problem was unsolved (18.15% vs 16.67%).
 |
Table 3 Antibiotic Administration Related Variables by Antibiotic Self-Administration (n = 295) |
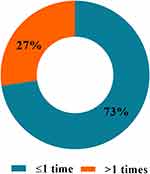 |
Figure 1 Distributions of antibiotic use within last two months (n = 295). |
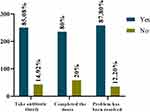 |
Figure 2 Distributions of antibiotic administration related variables (n = 295). |
Antibiotic Resistance Related Variables and Antibiotic Self-Administration
In the total sample, 38.64% did not ever hear of antibiotic resistance. Incomplete dose, antibiotic over-prescription, use in livestock and fish, and overuse of sanitizers are possible reasons for antibiotic resistance reported by 61.36%, 78.31%, 54.92%, 50.51%, and 72.88%, respectively of the respondents. Moreover, Figure 3 shows the overall distribution of the antibiotic resistance related variables. The antibiotic resistance related variables by self-administration are presented in Table 4. Self-administration of antibiotic was found to be higher among those who had not heard of antibiotic resistance (21.05% vs 16.02%) previously. Similarly, self-administration of antibiotic was more frequent (20.31% vs 17.32%) among those who were unaware that doses could lead to resistance. Self-administration was significantly greater (24.81% vs 12.35%, p = 0.006) among those who did not know that antibiotic over prescriptions may attribute to antibiotic resistance. Antibiotic were self-administered at a higher rate (18.60% vs 16.25%) among those uninformed that overusing sanitizer could contribute to antibiotic resistance.
 |
Table 4 Antibiotic Resistance Related Variables by Antibiotic Self-Administration (n = 295) |
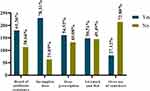 |
Figure 3 Distributions of antibiotic resistance related variables (n = 295). |
Antibiotic Specification Related Variables and Antibiotic Self-Administration
Penicillin, Amoxicillin, and Cefixime were correctly specified as antibiotic by 63.39%, 68.81%, and 70.17%, participants, respectively. On the other hand, 66.78% and 59.66% reported that Remdesivir, and Albendazole are also antibiotic. Furthermore, Figure 4 demonstrates the overall distribution of the antibiotic specification related variables. Table 5 presents the antibiotic specification related variables by antibiotic self-administration. Self-administration was significantly higher among those who could not correctly recognize Amoxicillin as an antibiotic (26.09% vs 14.29%, p = 0.014). Self-administration was higher in those who could not correctly distinguish Cefixime as an antibiotic (22.73% vs 15.94%). Similarly, among those who could not specify Azithromycin as an antibiotic, the prevalence of self-administration was significantly higher (28.00% vs 14.55%, p = 0.009). Antibiotic self-administration was higher among those who recognized Remdesivir as an antibiotic (23.47% vs 15.23%). Similarly, the self-administration rate was higher among those who identified Albendazole as an antibiotic (21.85% vs 15.34%).
 |
Table 5 Antibiotic Specification Related Variables by Antibiotic Self-Administration (n = 295) |
 |
Figure 4 Distributions of antibiotic specification related variables (n = 295). |
Discussion
To the best of the authors’ knowledge, this is the first study that attempted to investigate the prevalence of antibiotic self-administration among the Bangladeshi population within two months of administration. A high prevalence of antibiotic self-administration was found, and several factors were also found to be significantly associated with the self-administration. This study might contribute to the antibiotic drug regulatory authority re-thinking the existing policy to minimize the possible impact of antibiotic self-administration on the community.
In this study, the prevalence of antibiotic self-administration was 17.97%. A survey conducted in UAE conducted by Abasaeed et al, found the prevalence of self-administration of antibiotic was 44%.25 According to a systematic review on antibiotic self-administration in Asia, the prevalence varied from 4% to 75%.31 Another systematic review conducted by Ocan et al, found that the overall prevalence of antibiotic self-administration in underdeveloped countries was 38.8%.5 Shah et al, reported that the prevalence of antibiotic self-administration in Karachi was 47.6%.27 The antibiotic self-administration among Nigerian students was 53.8%.6 However, a higher prevalence of antibiotic self-administration was found in several studies conducted in the Czech Republic (31.1%), Jordan (20.0%), and Lithuania (39.9%) compared to our study.25 Besides, Shah et al, revealed that the prevalence of self-administration of antibiotic was 47.8% in Southern China, 79.5% in Sudan, and 48% in Iran.27
In Lithuania, women were more likely to self-administered antibiotic than males.25 We found that 21.43% of the females self-administrated antibiotic, whereas males were only 14.18%. However, sex varies with the prevalence of antibiotic self-administration in numerous studies in several countries. In Malaysia, the rate of antibiotic self-administration among females and males was 51.5% and 48.5%, respectively.32 Besides, in their study, Sharma et al, showed that most of the respondents were male, which was 65.64%.3 In Pakistan, there was a high prevalence of antibiotic self-administration among females (57%) than males (43%).8 There might be numerous reasons for females to self-administrate antibiotics. Females may be more prone to stay at home. Moreover, the female respondents might perceive that self-administration of antibiotic may reduce their time and decrease the hassle of visiting a doctor.8
In our study, it was found that the most prevalent age group in antibiotic self-administration (34.78%) was the youngest (<20 years). Similarly, the youngest respondents of India (18–20 years) were reported as the highest prevalent (60.7%) group.3 Albeit, in turkey, the highest rate of antibiotic self-administration (23%) was found among the middle (40–49) years age group.33 According to Mitra et al, the youngest people were more prone to self-administration with antibiotic as they perceived less willingness and trust to visit doctors while going through minor health issues.28
This study found that the prevalence of antibiotic self-administration among rural residents was higher (23.81% vs 17.00%) than the urban dwellers. A study conducted in Pakistan by Bilal et al, found that 81.25% of the rural people self-administered antibiotic.34 Another study also reported that 44.6% of Greek rural people were self-administered with antibiotic.26 Rural people were mainly more self-administrated with antibiotic than urban people, possibly because they have fewer health-related facilities. Besides, they might not clearly understand antibiotic resistance, and they might become prone to improper dispensing of antibiotic in local pharmacies.34,35
For the respondents of this study, who took antibiotic more than once within two months, their prevalence of self-administration was higher (22.37%). 50% of the Sri Lankan adults used any antibiotic once in the previous 3 months; among them, 11% reported being antibiotic self-administered.36 In Pakistan, 45% of the respondents administered antibiotic at least once in the last six months.8 In Kuwait, 10.8% of the respondents self-administered antibiotic once a year.28 A study in Bangladesh found that 30.3% of students self-administered antibiotic more than two times in the past 12 months.37 Most of the respondents assumed their health issue was minor and less concerning, and they were prone to choose the self-administration of antibiotic.37
In this study, of those who did not take antibiotic at the proper time, among them 38.64% were self-administered. Antibiotic therapy was not taken by maintaining proper time and not completed doses contribute to the development of antibiotic resistance.11 However, an incomplete antibiotic course is another crucial factor contributing to the development of antibiotic resistance.38 A considerable portion who self-administered, 35.59%, did not complete the doses in our research. Therefore, people seem unaware of the impacts of antibiotic dose incompletion. This might be because they were less concerned about their diseases or health issues.39 Thus, when they get rid of their sickness with seasonal or common diseases, they do not prioritize completing the doses.5 Sometimes people might feel it often occurred in their body, like flu and fever; therefore, their approach to completing the antibiotic course is less-concerned.9,32
In our study, 21.05% of antibiotic self-administered participants had not heard about antibiotic resistance, and of them, 20.31% did not know that antibiotic resistance may occur due to incomplete doses. This study’s findings might be indicated the poor knowledge of the participants on antibiotic resistance. Gillani et al, reported that 30% were aware that the inconsistent administration of antibiotic would attribute antibiotic resistance.8 However, 24.81% of the self-administered participants did not know resistance might occur due to over-prescription in this study. Besides, the prevalence of self-administration was only 12.35% among the knowing group. Zawahir et al, reported that overall knowledge related to antibiotic resistance in Sri Lanka was poor.36 Zawahir et al, also found that the general people in Sri Lanka had a limited understanding of antibiotic, reasons for antibiotic resistance, and their usability.36 In our study, who had not heard that antibiotic resistance might occur due to the overuse of sanitizers, 18.60% of them were self-administered. Pidot et al, demonstrated that the resistant bacterium Enterococcus faecium became growingly tolerant to alcohol antiseptics such as hand rub alternatives and they warn that a comprehensive approach to antimicrobial resistance will need to consider its adaptive responses not just to antimicrobials but to other active agents in sanitizer remedies.40 Besides, according to Albawani et al, antibiotic resistance was unknown to nearly half of the study group, and their chance of self-administration was high.19
Yusef et al, reported that Amoxicillin and Clavulanic acid combination was the most commonly used antibiotic (31%), second by Amoxicillin alone (15%), Azithromycin (5%), and Cefixime (4%) among adults in North Jordan.41 Our research explored the knowledge of antibiotic specification on several commonly used antimicrobials (Amoxicillin, Cefixime, Azithromycin, Remdesivir, and Albendazole) those were widely used during COVOD-19 in Bangladesh and their prevalence of self-administration. We found a considerable knowledge gap in the specification of antibiotic-related drugs, and the prevalence of self-administration was higher who could not specify the antibiotic accurately from the given list. Nevertheless, 26.09% of the respondents in our study were self-administered and could not identify Amoxicillin as an antibiotic. Besides, 22.73% and 28% of respondents were self-administered who failed to identify Cefixime and Azithromycin as antibiotic. Moreover, respondents who thought Remdesivir and Albendazole are antibiotic, their prevalence of self-administration was also high (23.47% and 21.85%, respectively). Based on our study findings, it can be concluded that adequate knowledge of correctly identifying antibiotic may reduce a higher prevalence of antibiotic self-administration.
Conclusion and Recommendation
This study revealed higher prevalence of antibiotic self-administration and the respondents’ understandings toward administration of antibiotic, antibiotics resistance, and antibiotic specification substantially influenced the concern. As a consequence of the rising rate of antibiotic self-administration, the authority should respond by reforming the prevailing policy to ensure antibiotics’ safe and effective use. Government legislation should be enacted to restrict the sale of prescription-only antibiotic that can only be obtained with the proper prescription. The government, the media, and healthcare organizations need to express their roles in educating and persuading consumers about antibiotic administration. Furthermore, local authorities may require to arrange community-level campaigning to limit antibiotic self-administration by promoting the significance of proper antibiotic adminstration and rising awareness.
Strength and Limitation
The strength of this study is that we explored the prevalence and the determinants of antibiotic self-administration within two months. This study is the first time in Bangladesh investigating the relationship of the variables related to sociodemographic, antibiotic administration, antibiotic resistance, and antibiotic specification with antibiotic self-administration. However, as the nature of the cross-sectional design, the relationship could not be considered a causality between the variables. Due to the online self-responses, only the participants having internet access participated, and the response bias was unavoidable. Moreover, as the participants were selected from the urban area, and therefore, the generalizability for of the whole population might be compromised. Thus, further in-depth and rigorous research on antibiotic self-administration considering numerous independent variables is recommended.
Data Sharing Statement
Data of the study can be found by the correspondent author’s request upon the reason for use.
Acknowledgments
We cordially accolade the contributions of the research assistants (names provided in Supplementary Table S1) for their valuable contribution to data collection for this study. Humayun Kabir and Md Kamrul Hasan contributed equally as co-first authors. Ariful Haque Tutul and Mohammad Shahidul Islam contributed equally as co-second authors.
Funding
The authors confirm no financial support for conducting the study.
Disclosure
The authors report no conflicts of interest in relation to this work and no potential conflicts of interest concerning study, authorship, and publication.
References
1. Biswas M, Roy MN, Manik MIN, et al. Self medicated antibiotics in Bangladesh: a cross-sectional health survey conducted in the Rajshahi city. BMC Public Health. 2014;14(1):1–7. doi:10.1186/1471-2458-14-847/FIGURES/5
2. Alam N, Saffoon N, Uddin R. Self-medication among medical and pharmacy students in Bangladesh. BMC Res Notes. 2015;8(1):763. doi:10.1186/s13104-015-1737-0
3. Sharma N, Jain M, Sharma P, et al. Prevalence of self-medication of antibiotics among 2nd year medical students and their knowledge about antibiotic resistance. Int J Acad Med. 2020;6(3):203. doi:10.4103/IJAM.IJAM_13_20
4. Sutradhar K. Irrational use of antibiotics and antibiotic resistance in Southern rural Bangladesh: perspectives from both the physicians and patients. Annu Res Rev Biol. 2014;4(9):1421–1430. doi:10.9734/arrb/2014/8184
5. Ocan M, Obuku EA, Bwanga F, et al. Household antimicrobial self-medication: a systematic review and meta-analysis of the burden, risk factors and outcomes in developing countries. BMC Public Health. 2015;15(1):742. doi:10.1186/s12889-015-2109-3
6. Osemene K, Lamikanra A. A study of the prevalence of self-medication practice among university students in southwestern Nigeria. Trop J Pharm Res. 2012;11(4):683–689. doi:10.4314/tjpr.v11i4.21
7. Shehadeh M, Suaifan G, Darwish RM, Wazaify M, Zaru L, Alja’fari S. Knowledge, attitudes and behavior regarding antibiotics use and misuse among adults in the community of Jordan. A pilot study. Saudi Pharm J. 2012;20(2):125–133. doi:10.1016/j.jsps.2011.11.005
8. Gillani AH, Ji W, Hussain W, et al. Antibiotic self-medication among non-medical university students in Punjab, Pakistan: a cross-sectional survey. Int J Environ Res Public Health. 2017;14:10. doi:10.3390/ijerph14101152
9. Widayati A, Suryawati S, de Crespigny C, Hiller JE. Self medication with antibiotics in Yogyakarta city Indonesia: a cross sectional population-based survey. BMC Res Notes. 2011;4(1):491. doi:10.1186/1756-0500-4-491
10. Ahmed I, Rabbi MB, Rahman M, et al. Knowledge of antibiotics and antibiotic usage behavior among the people of Dhaka, Bangladesh. Asian J Med Biol Res. 2020;6(3):519–524. doi:10.3329/ajmbr.v6i3.49803
11. Islam MS, Sikdar KY, Hossain AM, Faroque A. Study on the pattern of antibiotic use including the resistance episodes in Bangladesh. Dhaka Univ J Pharm Sci. 2019;18(2):135–143. doi:10.3329/dujps.v18i2.43255
12. Abduelkarem AR, Othman AM, Abuelkhair ZR, Ghazal MM, Alzouobi SB, El Zowalaty ME. Prevalence of self-medication with antibiotics among residents in United Arab Emirates. Infect Drug Resist. 2019;12:3445–3453. doi:10.2147/IDR.S224720
13. O’Neill J. Antimicrobial resistance: tackling a crisis for the health and wealth of nations; 2014.
14. Hoque R, Ahmed SM, Naher N, et al. Tackling antimicrobial resistance in Bangladesh: a scoping review of policy and practice in human, animal and environment sectors. PLoS One. 2020;15(1):e0227947. doi:10.1371/JOURNAL.PONE.0227947
15. Joarder T, Chaudhury TZ, Mannan I. Universal health coverage in Bangladesh: activities, challenges, and suggestions. Adv Public Heal. 2019;2019:4954095. doi:10.1155/2019/4954095
16. Wester CW, Durairaj L, Evans AT, Schwartz DN, Husain S, Martinez E. Antibiotic resistance: a survey of physician perceptions. Arch Intern Med. 2002;162(19):2210–2216. doi:10.1001/ARCHINTE.162.19.2210
17. Tasnuva Ferdous P. Prevalence of self medication practice with antibiotics among the students of some educational institutions of Dhaka and Gazipur district. Bioresearch Commun. 2018;4(2):555–564.
18. Pourhoseingholi MA, Vahedi M, Rahimzadeh M. Sample size calculation in medical studies. Gastroenterol Hepatol from Bed to Bench. 2013;6(1):14–17.
19. Albawani SM, Bin hassan Y, Abd-Aziz N, Gnanasan S. Self-medication with antibiotics in Sana’a City, Yemen. Trop J Pharm Res. 2017;16(5):1195. doi:10.4314/tjpr.v16i5.30
20. Chapot L, Sarker MS, Begum R, et al. Knowledge, attitudes and practices regarding antibiotic use and resistance among veterinary students in Bangladesh. Antibiotics. 2021;10(3):332. doi:10.3390/antibiotics10030332
21. Rathish D, Wijerathne B, Bandara S, et al. Pharmacology education and antibiotic self-medication among medical students: a cross-sectional study. BMC Res Notes. 2017;10(1):337. doi:10.1186/s13104-017-2688-4
22. Jairoun A, Hassan N, Ali A, Jairoun O, Shahwan M, Hassali M. University students’ knowledge, attitudes, and practice regarding antibiotic use and associated factors: a cross-sectional study in the United Arab Emirates. Int J Gen Med. 2019;12:235–246. doi:10.2147/IJGM.S200641
23. Ayele Y, Jifar A. Assessment of knowledge, attitude and practice toward antibiotic use among Harar city and its surrounding community, Eastern Ethiopia. Interdiscip Perspect Infect Dis. 2018;2018:1–6. doi:10.1155/2018/8492740
24. Voidăzan S, Moldovan G, Voidăzan L, Zazgyva A, Moldovan H. Knowledge, attitudes and practices regarding the use of antibiotics: study on the general population of Mureş County, Romania. Infect Drug Resist. 2019;12:3385–3396. doi:10.2147/IDR.S214574
25. Abasaeed A, Vlcek J, Abuelkhair M, Kubena A. Self-medication with antibiotics by the community of Abu Dhabi Emirate, United Arab Emirates. J Infect Dev Ctries. 2009;3(07):491–497. doi:10.3855/jidc.466
26. Skliros E, Merkouris P, Papazafiropoulou A, et al. Self-medication with antibiotics in rural population in Greece: a cross-sectional multicenter study. BMC Fam Pract. 2010;11(1):58. doi:10.1186/1471-2296-11-58
27. Shah SJ, Ahmad H, Rehan RB, et al. Self-medication with antibiotics among non-medical university students of Karachi: a cross-sectional study. BMC Pharmacol Toxicol. 2014;15(1):74. doi:10.1186/2050-6511-15-74
28. Mitra AK, Imtiaz A, Al Ibrahim YA, Bulbanat MB, Al Mutairi MF, Al Musaileem SF. Factors influencing knowledge and practice of self-medication among college students of health and non-health professions. IMC J Med Sci. 2019;12(2):57–68. doi:10.3329/imcjms.v12i2.39662
29. Gunawardhana C, Sakeena M, Sivayoganthan C. Awareness of rational medication use and antibiotic self-medication practices among undergraduate students in a university in Sri Lanka. Trop J Pharm Res. 2015;14(4):723. doi:10.4314/tjpr.v14i4.23
30. Association WM. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310(20):2191–2194. doi:10.1001/JAMA.2013.281053
31. Rathish D, Wickramasinghe ND. Prevalence, associated factors and reasons for antibiotic self-medication among dwellers in Anuradhapura: a community-based study. Int J Clin Pharm. 2020;42(4):1139–1144. doi:10.1007/s11096-020-01065-6
32. Haque M, Rahman NAA, McKimm J, et al. Self-medication of antibiotics: investigating practice among university students at the Malaysian National Defence University. Infect Drug Resist. 2019;12:1333–1351. doi:10.2147/IDR.S203364
33. Ilhan MN, Durukan E, Ilhan SÖ, Aksakal FN, Özkan S, Bumin MA. Self-medication with antibiotics: questionnaire survey among primary care center attendants. Pharmacoepidemiol Drug Saf. 2009;18(12):1150–1157. doi:10.1002/pds.1829
34. Bilal M. Self-medication with antibiotics among people dwelling in rural areas of Sindh. J Clin Diagnostic Res. 2016. doi:10.7860/JCDR/2016/18294.7730
35. Torres NF, Solomon VP, Middleton LE. Patterns of self-medication with antibiotics in Maputo city: a qualitative study. Antimicrob Resist Infect Control. 2019;8(1):161. doi:10.1186/s13756-019-0618-z
36. Zawahir S, Lekamwasam S, Halvorsen KH, Rose G, Aslani P. Self-medication behavior with antibiotics: a national cross-sectional survey in Sri Lanka. Expert Rev Anti Infect Ther. 2021;19(10):1341–1352. doi:10.1080/14787210.2021.1911647
37. Siam MHB, Imran A, Limon MBH, et al. Antibiotic abuse: a cross-sectional study on knowledge, attitude, and behavior among the university students in Dhaka, Bangladesh. Electron J Gen Med. 2021;18(3):em289. doi:10.29333/ejgm/10836
38. Langford BJ, Morris AM. Is it time to stop counselling patients to “finish the course of antibiotics”? Can Pharm J. 2017;150(6):349–350. doi:10.1177/1715163517735549
39. Torres NF, Chibi B, Middleton LE, Solomon VP, Mashamba-Thompson TP. Evidence of factors influencing self-medication with antibiotics in low and middle-income countries: a systematic scoping review. Public Health. 2019;168:92–101. doi:10.1016/j.puhe.2018.11.018
40. Pidot SJ, Gao W, Buultjens AH, et al. Increasing tolerance of hospital Enterococcus faecium to handwash alcohols. Sci Transl Med. 2018;10(452):eaar6115. doi:10.1126/scitranslmed.aar6115
41. Yusef D, Babaa AI, Bashaireh AZ, et al. Knowledge, practices & attitude toward antibiotics use and bacterial resistance in Jordan: a cross-sectional study. Infect Dis Heal. 2018;23(1):33–40. doi:10.1016/j.idh.2017.11.001
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.