Back to Journals » Open Access Emergency Medicine » Volume 14
Perioperative Management for Emergency Surgery in Pediatric Patients with COVID-19: Retrospective Observational Study
Authors Giwangkancana G , Oktaliansah E, Ramlan AAW, Utariani A, Kurniyanta P, Arifin H, Widyastuti Y , Pratiwi A, Syukur R
Received 2 June 2022
Accepted for publication 31 August 2022
Published 20 September 2022 Volume 2022:14 Pages 515—524
DOI https://doi.org/10.2147/OAEM.S377201
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Hans-Christoph Pape
Gezy Giwangkancana,1 Ezra Oktaliansah,1 Andi Ade W Ramlan,2 Arie Utariani,3 Putu Kurniyanta,4 Hasanul Arifin,5 Yunita Widyastuti,6 Astrid Pratiwi,7 Rusmin Syukur8
1Department of Anesthesia and Intensive Care, Faculty of Medicine Universitas Padjadjaran/Dr. Hasan Sadikin National Referral and Teaching Hospital, Bandung, Indonesia; 2Department of Anesthesia and Intensive Care, Faculty of Medicine Universitas Indonesia/Dr. Cipto Mangunkusumo National Referral and Teaching Hospital, Jakarta, Indonesia; 3Department of Anesthesia and Intensive Care, Faculty of Medicine Universitas Airlangga/Dr. Soetomo Provincial Referral and Teaching Hospital, Surabaya, Indonesia; 4Department of Anesthesia and Intensive Care, Faculty of Medicine Universitas Udayana/ Prof Dr. I.G.N.G Ngoerah National Referral and Teaching Hospital, Bali, Indonesia; 5Department of Anesthesia and Intensive Care, Faculty of Medicine Universitas Sumatera Utara/Dr. Adam Malik National Referral and Teaching Hospital, Medan, Indonesia; 6Department of Anesthesia and Intensive Therapy, Faculty of Medicine, Public Health and Nursing Universitas Gajah Mada/Dr. Sardjito National Referral and Teaching Hospital, Yogyakarta, Indonesia; 7Department of Anesthesia and Intensive Care, Harapan Kita Mother and Child Hospital, Jakarta, Indonesia; 8Department of Anesthesia and Intensive Care Faculty of Medicine Universitas Hassanudin/ Dr. Wahidin Sudirohusodo National Referal and Teaching Hospital, Makassar, Indonesia
Correspondence: Gezy Giwangkancana, Department of Anesthesia and Intensive Care, Faculty of Medicine Universitas Padjadjaran/Dr. Hasan Sadikin National Referral and Teaching Hospital, RSUP Dr Hasan Sadikin, Bandung, Pasteur Street No. 38, Bandung, 40161, Indonesia, Tel +628122005952, Email [email protected]
Background: The first wave of COVID-19 in 2020 created massive challenges in providing safe surgery for pediatric patients with COVID-19. Inevitably, emergency surgery and the unknown nature of the disease place a burden on the heavily challenged surgical services for pediatrics in a developing country. Lessons from the pandemic are important for future disaster planning.
Aim: To describe the characteristics of pediatric surgical patients with COVID-19 undergoing emergency surgery during the first wave and its perioperative narrative in a developing country.
Methods: The study was a multicenter retrospective descriptive study in eight Indonesian government-owned referral and teaching hospitals. The authors reviewed confirmed COVID-19 pediatric patients (≤ 18 years old) who underwent surgery. Institutional review board clearances were acquired, and data were evaluated in proportion and percentages. The writing of this paper follows the STROBE guidelines.
Results: About 7791 pediatric surgical cases were collected, 73 matched the study criteria and 24 confirmed cases were found. Cases were more common in females (58.3%), who were above 12 years old (37.5%) and who were asymptomatic (62.5%). Laparotomy (33.3%), general anesthesia (90.4%) and intubation (80.8%) were common, while use of video laryngoscopy (40%) and rapid sequence intubation (28.8%) were rare. The mean length of stay was 12 ± 13.3 days, and in-hospital mortality was 8.3%.
Discussions: Lockdown and school closure were successful in protecting children, hence the low incidence of pediatric surgical cases with COVID-19 during the first wave. Many hospitals were unprepared to perform surgery for a droplet or airborne infectious disease, and COVID-19 testing was not available nationally in the early pandemic, hence the use of protective protection equipment during these early pandemic times are often not efficient.
Conclusion: The incidence of COVID-19 in pediatric surgical patients is low. The rapidity and availability of preoperative testing for a new emerging disease are essential in a pandemic.
Keywords: COVID-19, emergency surgery, operating room, pandemic, pediatric anesthesia, pediatric surgery, perioperative
Introduction
The COVID-19 pandemic had emerged in Indonesia by January 2020; by the end of 2021, reports concluded four million cases with 150,000 deaths.1,2 The spread of the severe acute respiratory syndrome coronavirus type 2 (SARS-CoV-2) virus, the pathogen behind COVID-19, affected the provision of emergency and elective pediatric surgery services globally. Official reports stated that children represented 1.8–14.5% of global cases – highest among older adolescents and young adults – with a case fatality of 0.1–0.4% or around 72,000–58,000 cases in Indonesia alone.3,4 Owing to the high number of pediatric patients during the COVID-19 pandemic, which had not been seen during previous flu pandemics, some pediatric surgical patients are highly likely to be infected with the virus during their preoperative period. Furthermore, pediatric patients are asymptomatic and may unknowingly transmit the virus to others, including health care workers.3,5–7
Although pediatric surgeries were generally postponed at the beginning of the pandemic owing to lockdowns and the preservation of medical resources to manage the pandemic, emergency surgery continued.8,9 Alarmingly, multicenter studies reported that adult patients with COVID-19 had higher rates of mortality and morbidity than those without COVID-19.9–14 However, there is a dearth of studies on pediatric emergency surgery epidemiology or outcomes of COVID-19 in developing countries and its perioperative management. These outlooks and studies are essential in pediatric surgery as the pandemic moves to a chronic state globally in 2022, and there are predictions of another pandemic in the future. At the time of writing this paper, the World Health Organization (WHO) has declared monkeypox as a new pandemic, while COVID-19 is still present.1 Hence, first-stage reports of reaction to a pandemic are essential for better disaster planning in the future, especially that related to the safety of patients and health care personnel.
Firstly, we aim to describe the characteristics of pediatric surgical patients with COVID-19 undergoing emergency surgery during the first wave of the pandemic. Second, we aim to provide a narrative of the perioperative management of emergency pediatric surgery for pediatric patients with COVID-19 in a developing country.
Methods
Study Setting, Study Design and Data Collection
This study was a multicenter retrospective descriptive study involving eight government-owned hospitals. Six centers were a national referral and teaching hospital, one was a provincial referral and teaching hospital, and one was a specialized provincial referral mother and child hospital. All of the centers were COVID-19 referral centers.
The study reviews subjects undergoing emergency surgery with a suspected or confirmed COVID-19 infection in the preoperative period. Data were collected from the Indonesian Pediatric Surgery (I-PASS) registry from May 1 2020 to December 31, 2020, with the age limit for the subjects being 18 years old. A confirmed or positive COVID-19 case was defined when a nasal or nasopharyngeal swab test was positive for severe acute respiratory syndrome coronavirus type 2 (SARS-CoV-2) using the real-time (RT) polymerase chain reaction (PCR) test.2
Mortality was defined as whether the patient was discharged alive or dead. Preoperative, intraoperative and postoperative data were collected. The preoperative data collected included the patient’s origin, sex, age, contact history, symptoms, laboratory results, immunological results, coexisting disease, body mass index and vital signs. Intraoperative data collected were personal protective equipment, negative pressure operating room, intubation technique, type of surgery and type of anesthesia. Postoperative data collected were postoperative inpatient facility, length of stay and discharged condition. Patients were excluded if their RT-PCR results were unavailable.
Preliminary institutional board review (IRB) clearance was obtained first in the primary center (Dr. Hasan Sadikin National Referral and Teaching Hospital), number LB.02.01/X.6.5/14/2021, and each participating center completed its internal IRB clearance. The IRBs waived patient consent since data were taken from medical records and complied with the Declaration of Helsinki. Data were collected using a Microsoft Excel form in each center and pooled in a primary center database. The writing of this paper follows the STROBE guidelines. All subjects that matched the inclusion and exclusion criteria were included, and no minimal sample was measured; hence, a descriptive approach using simple proportions and percentages was used.
Results
Of the 7791 pediatric patients in the registry, 84 subjects matching the searched criteria of cases with suspected COVID-19 during the preoperative period were included. Eleven cases were excluded since nine did not have RT-PCR results, and two had incomplete anesthetic and surgical records (Figure 1).
 |
Figure 1 Strengthening the reporting of observational studies in epidemiology (STROBE) diagram. Adapted by permission from Springer Nature, Aging Clinical and Experimental Research Bolignano D, Mattace-Raso F, Torino C, et al. The quality of reporting in clinical research: the CONSORT and STROBE initiatives. Aging Clin Exp Res. 2013;25(1):9-15, COPYRIGHT 2013.24 |
Most of the suspected cases came from Java Island (91.8%), with a center in East Java reporting the most cases (n=28 cases), and secondly the capital, Jakarta (Figure 2).
 |
Figure 2 Indonesian area distribution of pediatric surgical cases with suspected COVID-19 infection. |
Most cases were managed using general anesthesia (90.4%), and patients were intubated (80.8%). The use of video laryngoscope was at 40%, and 28.8% of intubation was done using the rapid sequence protocol. Most cases were done using level 3 personal protective equipment (PPE) (74%). RT-PCR results were available within 24 hours in 50.6% of the cases, and 61.6% of the patients were done in a negative chamber operating room (Table 1).
 |
Table 1 Pediatric Anesthesia Services for Suspected and Confirmed COVID-19 Patients in Indonesian Referral Hospitals |
This study recorded 24 confirmed COVID-19 cases in the preoperative period with an incidence of 0.3% (24 patients/7791 pediatric surgical cases). Most cases were female (58.3%), over 12 years old (37.5%) and asymptomatic (62.5%). A positive antibody test for SARS-CoV-2 was found in 50% of the cases, and most radiological imaging was normal (70.8%). Clinically, 33.3% of the patients required oxygen supplementation, with the lowest saturation recorded (92–98%) at 58.3%, and 12.5% of the patients required mechanical ventilation. General pediatric laparotomy surgery was the most common type of surgical procedure (33.3%), and most procedures were emergency or urgent surgery (50%; 33.3%). Most patients were discharged to the COVID-19 inpatient ward, with a mean length of stay of 12 ±13.3 days. In-hospital mortality was 8.3% among COVID-19-positive pediatric patients undergoing surgery (Table 2).
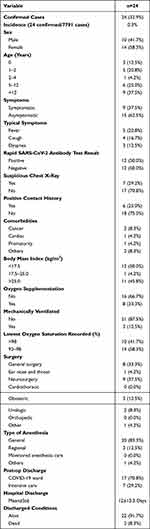 |
Table 2 Characteristics of Confirmed COVID-19 Pediatric Patients Undergoing Surgery in Indonesia |
A comparison was made between the two groups of patients: patients with positive SARS-CoV-2 results (confirmed) and patients with negative SARS-CoV-2 results (discarded). More patients in the negative group had more pneumonia in chest radiological examinations (29.2% vs 69.4%), more oxygen requirements (33.3% vs 61.2%), lower saturation (58.3% vs 85.7%), more admission to ICU (29.2% vs 57.1%) and higher mortality (8.3% vs 24.5%) (Table 3).
 |
Table 3 Comparison of Pediatric Patients with Positive SARS-CoV-2 Results (Confirmed) and Patients with Negative SARS-CoV-2 Results (Discarded) Undergoing Surgery |
Discussion
Our multicenter study was the first to describe the prevalence of pediatric COVID-19 among general pediatric surgical patients in a low-middle-income country (LMIC), which would be relevant to surgeons and anesthesiologists in other LMICs, especially in regards to mitigating the possibility of another emerging disease in the future. There are some limitations in our study. Although this was a multicenter study, we did not include all 12 COVID-19 referral hospitals in Indonesia. Secondly, there is the possibility of bias in data entry; hence, not all pediatric surgical patients with or without suspected COVID-19 were included in the database. Thirdly, there is a possibility that there are patients who were operated in private hospitals, which is beyond the scope of this paper. Hence, this study’s 0.3% incidence of pediatric surgical patients with COVID-19 cannot be generalized.
Our results are compared with a similar multicenter registry in a similar time frame in early 2020 in several countries. This study included three United children’s hospitals that resulted in 12 COVID-19-positive patients from 1295 pediatric surgical patients with an incidence of 0.22%.16 Another single-center study in Texas from April to August 2020 found one of the highest records of 66 confirmed pediatric surgical patients with COVID-19. However, this study did not provide the total of pediatric surgical performed during that period, so the incidence was not calculated.17 Although WHO data show that during early 2020 infection rates in the US were three times higher than in Indonesia during the same period, our comparison shows that the incidence is somewhat similar.1,2 It is to be noted that the incidence of cases in our study and other comparative studies was small. There are several possible reasons why the incidence is low. One is that COVID-19 is more commonly found in adults, there are higher false-negative results owing to technical difficulties in performing swab tests, and a more deficient expression enzyme angiotensin-converting enzyme (ACE2) cell surface serves as the SARS-CoV-2 entry point in the nasal epithelium of children.4–6,15–17 Another possibility is the success of the lockdown protocols worldwide during the early phase of the pandemic, where schools were closed quickly so that infection transmissions were stopped. Hence, lockdowns in pandemic are essential to protect high-risk populations such as children and to slow down infection rates, in order to provide a timeframe for health services to start disaster protocols including surgery disaster protocols and planning.3–6,16–18
Another finding in our study was that most COVID-19-positive patients were asymptomatic, and negative COVID-19 patients had more symptoms and higher severity and had worse outcomes. This description should be interpreted carefully since our study has some limitations. First, there were insufficient data to perform a statistical analysis of the differences in symptoms and outcomes. Since there were fewer pediatric patients in general in early 2020, a future study should include a multinational study to gather more patients. Second, although there were changes in workflow in each hospital to face the pandemic, the Indonesian Ministry of Health has issued guidelines on the management of COVID-19.15 However, each participating center in our study used different sets of clinical criteria to triage patients during the first wave of the pandemic. This triage generally consisted of a standardized triage questionnaire and assessment by a specific infection assessment team appointed by each hospital and known nationally as the tim penyakit infeksi new-emerging dan reemerging (Pinere).
Screening consisted mainly of positive contact history, presence of symptoms such as fever and cough, suspicious laboratory results, suspicious chest radiological examination, or a positive SARS-CoV-2 antibody or antigen test. In the early stages of the pandemic, COVID-19 patients were symptomatic, and those with respiratory symptoms that appeared during admission to the emergency room were quickly triaged as suspected COVID-19 patients. Only recent studies and understanding show that most pediatric patients were asymptomatic and that the sensitivity and specificity of many questionnaire-based triages are weak compared to RT-PCR.5,6,10,16,17 Further study is needed on whether asymptomatic children transmit COVID-19; hence, preoperative SARS-CoV-2 PCR testing is still deemed necessary for the time being.10,18
The general impression of emergency surgery for pediatric patients with COVID-19, during the first wave of the pandemic, was alarming. Many surgeries were not performed in the recommended negative pressure operating room, guided intubation using the recommended video laryngoscope and rapid sequence was not common, and some surgeries were done without the recommended level 3 PPE.19–21 Possible reasons for this finding could primarily relate to the preparedness of a country’s general healthcare system to face a pandemic. Studies have shown that national and hospital preparedness in many countries around the world, including Indonesia, is inadequate, with general issues such as the provision of onsite testing for SARS-CoV-2, availability of PPE, regulations in protection for health care workers, availability of isolation facilities and conflicting roles of agencies.22,23
Since symptoms, radiological and laboratory results are not adequate to screen for COVID-19 in the perioperative period, there is an urgent requirement for general and rapid sensitive and specific testing for hospitals that provide emergency screening in the preoperative period if another emerging disease appears. When rapid point-of-care antigen testing with high specificity and sensitivity is not available, it is inevitable that PPE and infectious disease operating rooms will be overused owing to false-positive screening. If such a pandemic should happen again in the future, a strategy that seems to protect children is an early lockdown. However, as the pandemic continues to evolve through 2022, with new variants of the SARS-CoV-2 virus emerging and vaccinations in children being carried out, it will be interesting to continue observing the dynamics between the COVID-19 pandemic and pediatric surgery.
Conclusion
The incidence of COVID-19 in pediatric surgical patients is below, and most patients are asymptomatic. Provision of rapid point-of-care antigen testing with high specificity and sensitivity for perioperative screening for emergency surgery is critical during a pandemic.
Acknowledgments
The research team would like to thank Muhammad Ramadhan Hasibuan MD, Fidkya Alisha MD and Lusianawati MD for their contributions to each local center, Ms Emma Nurhasanah for her secretarial and administrative work and Ms Vita for statistical analysis. We dedicate this paper to all health care workers and essential workers for their hard work during the COVID-19 pandemic; we salute you for your bravery and dedication. Finally, we dedicate this paper to all parents and children affected by COVID-19.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research did not receive any specific grant from funding agencies in public, commercial or not-for-profit sectors.
Disclosure
The authors declare no conflict of interest.
References
1. World COVID-19 Dashboard. World Health Organization. Available from: https://covid19.who.int/region/searo/country/id.
2. Indonesia COVID-19 Dashboard. Indonesian Ministry of Health. Available from: https://infeksiemerging.kemkes.go.id/.
3. World Health Organization. COVID-19 disease in children and adolescents: scientific brief. World Health Organization; 2021. Available from; WHO/2019CoV/Sci_Brief/Children_and_adolescents/2021.1.
4. Central for Disease Control USA. Children and COVID-19: State-Level Data Report. Available from: https://www.aap.org/en/pages/2019-novel-coronavirus-COVID-19-infections/children-and-COVID-19-state-level-data-report/.
5. Wu L, Zhang XF, Yang Y, et al. Clinical characteristics of pediatric cases of COVID-19 in Hunan, China: a retrospective, multi-center case series. Front Pediatr. 2021:995. doi:10.3389/fped.2021.665377
6. Soebandrio A, Kusumaningrum T, Yudhaputri FA, Oktavianthi S, Malik SG, Myint KSA. Characteristics of children with confirmed SARS-CoV-2 infection in Indonesia. J Clin Virol Plus. 2021;1:100027. doi:10.1016/j.jcvp.2021.100027
7. Surendra H, Elyazar IR, Djaafara BA, et al. Clinical characteristics and mortality associated with COVID-19 in Jakarta, Indonesia: a hospital-based retrospective cohort study. Lancet Reg Health West Pac. 2021;9:100108. doi:10.1016/j.lanwpc.2021.100108
8. Qazi SH, Saleem A, Pirzada AN, Hamid LR, Dogar SA, Das JK. Challenges to delivering pediatric surgery services in the midst of COVID 19 crisis: experience from a tertiary care hospital of Pakistan. Pediatr Surg Int. 2020;36:1–7. doi:10.1007/s00383-019-04581-3
9. Gunadi YI, Paramita VMW, Fauzi AR, Makhmudi A, Makhmudi A, Makhmudi A. The Impact of COVID-19 pandemic on pediatric surgery practice: a cross-sectional study. Ann Med Surg. 2020;59:96. doi:10.1016/j.amsu.2020.09.020
10. Nahshon C, Bitterman A, Haddad R, Hazzan D, Lavie O. Hazardous postoperative outcomes of unexpected COVID-19 infected patients: a call for global consideration of sampling all asymptomatic patients before surgical treatment. World J Surg. 2020;44:2477–2481. doi:10.1007/s00268-020-05575-2
11. Haffner MR, Le HV, Saiz AM, et al. Postoperative In-hospital morbidity and mortality of patients with COVID-19 infection compared with patients without COVID-19 infection. JAMA Netw Open. 2021;4(4):e215697–e215697. doi:10.1001/jamanetworkopen.2021.5697
12. COVIDSurg Collaborative. Mortality and pulmonary complications in patients undergoing surgery with perioperative SARS-CoV-2 infection: an international cohort study. Lancet. 2020;396:10243.
13. COVIDSurg Collaborative, & GlobalSurg Collaborative. Timing of surgery following SARS‐CoV‐2 infection: an international prospective cohort study. Anaesthesia. 2021;76(6):748–758.
14. Indonesia Development Indicators. The World Bank. Available from: https://data.worldbank.org/indicator/SP.POP.TOTL?locations=ID.
15. Indonesian Ministry of health. Pedoman pengendalian dan pencegahan coronavirus disease. Indonesian Ministry of health. Available from: https://infeksiemerging.kemkes.go.id/document/download/KpvOAX9r3j.
16. Lin EE, Blumberg TJ, Adler AC, et al. Incidence of COVID-19 in pediatric surgical patients among 3 US children’s hospitals. JAMA Surg. 2020;155(8):775–777. doi:10.1001/jamasurg.2020.2588
17. Mehl SC, Loera JM, Shah SR, et al. Favorable postoperative outcomes for children with COVID-19 infection undergoing surgical intervention: experience at a free-standing children’s hospital. J Pediatr Surg. 2021;56:2078–2085. doi:10.1016/j.jpedsurg.2021.01.033
18. Ladhani SN, Amin-Chowdhury Z, Davies HG, et al. COVID-19 in children: analysis of the first pandemic peak in England. Arch Dis Child. 2020;105(12):1180–1185. doi:10.1136/archdischild-2020-320042
19. Matava CT, Kovatsis PG, Summers JL, et al. Pediatric airway management in Coronavirus disease 2019 patients: consensus guidelines from the society for pediatric anesthesia’s pediatric difficult intubation collaborative and the Canadian pediatric anesthesia society. Anesth Analg. 2020;131:61–73. doi:10.1213/ANE.0000000000004872
20. Wen X, Li Y. Anesthesia procedure of emergency operation for patients with suspected or confirmed COVID-19. Surg Infect. 2020;21(3):299. doi:10.1089/sur.2020.040
21. Gai N, Maynes JT, Aoyama K. Unique challenges in pediatric anesthesia created by COVID-19. J Anesth. 2021;35(3):345–350. doi:10.1007/s00540-020-02837-0
22. Griffin KM, Karas MG, Ivascu NS, Lief L. Hospital preparedness for COVID-19: a practical guide from a critical care perspective. Am J Respir Crit Care Med. 2020;201(11):1337–1344. doi:10.1164/rccm.202004-1037CP
23. Djalante R, Lassa J, Setiamarga D, et al. Review and analysis of current responses to COVID-19 in Indonesia: period of January to March 2020. Prog Disaster Sci. 2020;6:100091. doi:10.1016/j.pdisas.2020.100091
24. Bolignano D, Mattace-Raso F, Torino C, et al. The quality of reporting in clinical research: the CONSORT and STROBE initiatives. Aging Clin Exp Res. 2013;25(1):9-15.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
