Back to Journals » Clinical Ophthalmology » Volume 17
Myopia Progression Among School-Aged Children in the COVID-19 Distance-Learning Era
Authors Althnayan YI, Almotairi NM, Alharbi MM, Alamer HB, Alqahtani HB , Alfreihi S
Received 28 August 2022
Accepted for publication 6 January 2023
Published 20 January 2023 Volume 2023:17 Pages 283—290
DOI https://doi.org/10.2147/OPTH.S381061
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Scott Fraser
Yasser I Althnayan,1,2 Nawal M Almotairi,2,3 Manal M Alharbi,2,3 Hadeel B Alamer,2,4 Hanan B Alqahtani,2– 4 Shatha Alfreihi2,4,5
1Ophthalmology Division, Department of Surgery, King Faisal Specialist Hospital and Research Center, Riyadh, Saudi Arabia; 2King Abdullah International Medical Research Centre, Riyadh, Saudi Arabia; 3Department of Optometry, College of Applied Medical Science, King Saud University, Riyadh, Riyadh Province, Saudi Arabia; 4Paediatric Ophthalmology Division, Paediatric Surgery Department, Ministry of National Guard - Health Affairs, Riyadh, Saudi Arabia; 5College of Medicine, King Saud Bin Abdulaziz University for Health Sciences, Riyadh, Saudi Arabia
Correspondence: Shatha Alfreihi, King Abdullah Specialist Children’s Hospital, P.O. Box 22490, Riyadh, 11426, Saudi Arabia, Tel +966-11-8011111, Fax +966-11-8011000 EXT 53273, 53320, Email [email protected]
Objective: To investigate the effect of online learning and other environmental factors on myopia progression during the Coronavirus pandemic (COVID-19).
Methods: A retrospective cohort study from 2018 to 2021. Data from children aged 6– 14 were gathered during three visits: pre-pandemic, at the beginning, and during the pandemic. Demographics (hours spent on screens for educational, recreational purposes, outdoors, and type of screen), best-corrected distance visual acuity (BCDVA), uncorrected distance visual acuity (UCDVA), and cycloplegic refraction were gathered.
Results: Of 150 patients, 70 [47%] were boys. The mean age was 11 (2.4) years. Participants mainly used mobile phones (62%) and had insufficient outdoor play (88%). Of the 300 eyes, 221 (74%) showed myopia progression. A significant difference in spherical equivalent (SE) was found between pre-pandemic and post-pandemic periods (− 0.29 (0.23) D vs − 0.40 (0.11) D; p =0.023). Additionally, UCDVA showed a difference between the initial and 1st follow-up visits (0.57 (0.37) vs 0.64 (0.36), p =0.001), and the first and 2nd follow-up visits (0.64 (0.36) vs 0.70 (0.36), p =0.001). Significant hazard ratio for change in SE in patients with higher age (> 9 years), (HR [95% confidence interval (CI)], 0.71 [0.51– 0.84]), greater recreational screen usage (HR [95% CI], 1.26 [1.15– 1.66]), and insufficient outdoor time (HR [95% CI], 1.45 [1.35– 1.67]).
Conclusion: Myopia progression was accelerated during the COVID-19 pandemic. Younger age, prolonged screen use, and insufficient outdoor time contributed to increased myopia progression. However, the type of device used had no significant effect.
Keywords: myopia, distance-learning, COVID-19, pandemic, school, children
Plain Language Summary
What is Already Known on This Topic
- Myopia is a progressive condition with a complex origin.
- A considerable myopic shift in school-aged youngsters has been found in studies, generating several concerns.
- It is critical to research the impact of online learning and environmental variables on myopia advancement during the COVID-19 pandemic since it may go unnoticed.
What This Study Adds
- This is one of few studies that show the acceleration of myopia in the same individual with cycloplegic refraction during the pandemic.
- Home confinement, extended screen time, and decreased outdoor time have all contributed to the acceleration of myopia in school-aged children, regardless of the type of device used.
How This Study Might Affect Research, Practice or Policy
- When policymakers outlined the overall class time for learning during home confinement or regular remote learning outside the pandemic, the influence of distant learning on myopia advancement had to be taken into consideration.
Introduction
The coronavirus disease (COVID-19) spread rapidly worldwide. The pandemic posed a critical challenge to the health system, economy, and education.1 Examples of its effects on education include the introduction of online learning and virtual classes to compensate for school closures during the lockdown.2 Globally, studies have reported a significant myopic shift in school-aged children during the pandemic, raising many concerns.3
Myopia is a global health problem therefore; the World Health Organization listed it as one of the five immediate priorities of the “Vision 2020” initiative.4 Myopia has a multifactorial etiology5 and is progressive in nature. Moreover, early-onset myopia is expected to progress to high myopia in adult life.6 The world is trending towards an increase in the prevalence of myopia, and the number of myopic individuals is expected to reach 5 billion by 2050. Therefore, 50% of the world’s population is likely to be affected.7
A cross-sectional study reported that near-work activities increased the prevalence of myopia.8 Particularly, online learning increases the prevalence of myopia at higher-grade levels due to the extended use of electronic devices.9 Previous studies have not looked into the progression using cycloplegic refraction, which is crucial in children.2,3 Our study aimed to investigate the effect of prolonged screen time on myopia progression in school-aged children during the pandemic of COVID-19.
Methods
This retrospective cohort study was conducted on children aged 6–14 years who visited the pediatric ophthalmology clinic at King Abdullah Specialist Children’s Hospital. The research was approved by the Institutional review board (IRB) at King Abdullah International Medical Research Center (KAIMRC) prospectively. The guidelines of the Declaration of Helsinki were followed.
All participants underwent a comprehensive ocular examination, including an assessment of uncorrected distance visual acuity (UCDVA), best-corrected distance visual acuity (BCDVA), and cycloplegic refraction. The sample size was calculated by sample size formula depending on the current population of Riyadh, Saudi Arabia.10
Patients with myopia with two previous visits to the pediatric ophthalmology clinic were included in the study. Myopia was defined as visual acuity <1.0 or spherical equivalent (SE) < −0.5 Diopters (D) in either eye.11 Patients using contact lenses, OrthoK lenses, or low-dose atropine for myopia control, and patients with developmental delay, systemic diseases, or a history of previous ocular surgery were excluded.
Data from three visits were compared: pre-pandemic visits (between 2018 and 2019), early pandemic visits (between 2019 and May 2020), and visits during the pandemic (between June 2020 and November 2021). Patients were enrolled in the study at the last follow-up based on the availability of the two previous visits and meeting the study criteria. June 2020 was chosen to ensure that enough time had passed for meaningful changes in progression. Parents were interviewed to collect the demographic data. The examination started with the determination of UCDVA and BCDVA in both eyes. Visual acuity was measured using tumbling E-charts and LogMAR units were utilized. Cycloplegic refraction was used to measure SE objectively, without subjective refinement. Cyclopentolate 1% (Bausch & Lomb Incorporated Tampa, FL USA) was applied twice 5 minutes apart in both eyes and repeated once if necessary. Cycloplegic refraction was performed at least 40 minutes after the first dose by a pediatric ophthalmologist or an optometrist, The event rates at 36 months were calculated for changes in BCDVA, UCDVA, and SE. Myopia progression was calculated as the difference between visits 1 and 2 and then compared to the difference between visits 2 and 3. With regard to the baseline age, patients were categorized into 6–9 years (group 1) and 10–14 years (group 2).
The screen time was categorized as low (30 min to 2 h), average (> 2 h to 4 h), and high (>4 h). The time spent outdoors was categorized as insufficient (<2 h) and sufficient (≥ 2 h) per day.12 Data regarding the type of device used during learning, including televisions, computers, tablets, and phones were collected.
Ethical Consideration
Informed consent was obtained from the parents or guardian at the time of data collection, and the patients’ confidentiality was ensured.
Statistical Analysis
Demographic and clinical characteristics are expressed as mean (standard deviation) or percentage (%). Continuous data with normal distribution were compared using Student’s t-test; the Mann–Whitney U-test was used for non-normally distributed data. Normality was checked using the Shapiro–Wilk test under the null hypothesis that the variable is normally distributed. The paired sample t-test was used to determine whether the mean difference between paired observations was statistically significant. The chi-square test was used for comparisons of categorical variables.
The primary outcome of our study was the change in SE. Secondary outcomes included changes in BCDVA and UCDVA. The events were considered and adjusted for age based on a previously published study.12 An event was recorded for each patient based on OS or OD. Cox proportional hazard analysis was performed to determine the predictability of baseline characteristics for changes in BCDVA, UCDVA, and SE events for the entire study cohort.
Univariate models were constructed based on age (Group 1 vs Group 2), sex (male vs female), educational screen time, recreational screen time, outdoor time, and device use. Hazard ratios (HRs) with 95% confidence intervals (CIs) were calculated for each model.
For the Kaplan–Meier curves, event-free curves were computed, and event-free survival was compared between subgroups using the Log rank test. Statistical significance was set at p < 0.05 (2-sided). IBM SPSS Statistics for Windows, version 23.0 (IBM Corp., Armonk, NY., USA) was used for data entry and statistical analysis. Microsoft Excel was used for graphical illustrations.
Patient and Public Involvement
This research was completed without patient involvement. Patients were not invited to comment on the study design and were not consulted to develop patient-relevant outcomes or interpret the results. Patients were not invited to contribute to the writing or editing of this document for readability or accuracy.
Results
Baseline characteristics of the 150 patients included in the final analysis are shown in Table 1. The mean age was 11 (2.4) years, and 47% (70) of the participants were males. Noticeably, the majority of the study cohort had an insufficient outdoor play (88%), and mainly used mobile phones (62%) at baseline.
 |
Table 1 Patient Characteristics |
In all 300 eyes, the difference in the mean SE between initial and first follow-up visit (−2.62 (0.78) D vs −2.91 (0.68) D, p-value = 0.001), and first follow-up visit and second follow-up visit (−2.91 (0.68) vs −3.35 (0.34), p = 0.001) was statistically significant. Similarly, there was a significant difference in the mean UCDVA between the initial and first follow-up visits (0.57 (0.37) vs 0.64 (0.36), p =0.001) and the first and second follow-up visits (0.64 (0.36) vs 0.70 (0.36), p =0.001). In contrast, the difference in BCDVA between baseline and follow-up visits was not statistically significant (Supplementary Table 1).
Clinical Outcomes at the Three-Year Follow Up
The mean follow-up period was 27.2 (6.90) months. Out of 300 eyes, 221 (74%) showed myopia progression, measured as a change in SE. Significantly fewer events were reported in the higher age group than in the lower age group (69% vs 85%, p =0.031). Additionally, participants with prolonged recreational screen use had significantly higher event rates compared to those with average and low screen use (95% vs 68% vs 51%, p = 0.003). Finally, insufficient outdoor time contributed to significantly higher event rates than sufficient outdoor time (79% vs 33%, p = 0.001) (Supplementary Table 2).
Pre- and Post-Pandemic
Myopia progression was calculated by summarizing the differences in BCDVA, UCDVA, and SE between the initial and first follow-up visits (pre-pandemic) and first and second follow-up visits (early pandemic and during pandemic). A significant difference was found in SE between the pre-pandemic and post-pandemic periods (−0.29 (0.23) D vs −0.40 (0.11) D, p= 0.023). In contrast, the difference between pre-and post-pandemic BCDVA (−0.01 (0.03) vs −0.01 (0.02), p = 0.601) and UCDVA (0.06 (0.12) vs 0.07 (0.13), p = 0.297) was not statistically significant (Table 2).
 |
Table 2 Comparison of Myopia Progression Between Pre-and Post-COVID Times |
Survival Analysis
The results of the univariate model analysis showed a significant HR for myopia progression (SE event) in the older age group (HR [95% CI], 0.71 [0.51–0.84]). In addition, recreational screen usage and outdoor time were strong predictors of change in SE (HR [95% CI], 1.26 [1.15–1.66], and 1.45 [1.35–1.67], respectively) (Table 3).
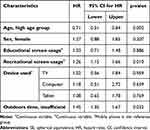 |
Table 3 Hazard Ratios for SE Events for Study Characteristics |
The Kaplan–Meier analysis demonstrated that age and outdoor time were reliable parameters to stratify patients with regard to changes in SE (p = 0.004 and p = 0.001, respectively) (Figures 1 and 2A). Regarding recreational screen use, prolonged usage demonstrated a significant difference in cumulative survival with regard to change in SE relative to low and average screen usage (p = 0.018 and p = 0.026, respectively) (Figure 2B).
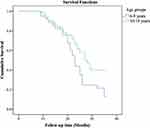 |
Figure 1 Kaplan–Meier curves showing cumulative survival rates of SE events for the study age groups. |
 |
Figure 2 Kaplan–Meier curves showing cumulative survival rates of SE events for the study recreational screen hours groups (A) and outdoor time groups (B). |
The 1-, 2-, and 3-year event-free survival rates in the lower and higher age groups were 90%, 43%, and 13% and 94%, 62%, and 40%, respectively. Furthermore, the 1, 2, and 3-year event-free survivals in the insufficient and sufficient outdoor time groups were 91%, 58%, and 21% and 100%, 91%, and 49%, respectively. Finally, the 1-, 2-, and 3-year event-free survival rates for the high recreational screen time group were 100%, 64%, and 22%, respectively, compared to 100%, 80%, and 45% and 100%, 78%, and 46%, in the average and low recreational screen time groups, respectively.
Discussion
The increased utilization of distance learning during the COVID-19 pandemic raised concerns regarding its effect on myopia. Especially, children in Saudi Arabia had extended hours of distance learning reaching 4–6 h daily at the elementary school level. This is one of the longest durations worldwide.3,9,12–16 Moreover, we had one of the longest periods of distance learning in the world (22 months). To the best of our knowledge, our study is the first to highlight important factors, such as insufficient time spent outdoors, increased recreational screen time, and younger age, that contributed to myopia progression during the pandemic based on changes in cycloplegic refraction over a three-year period in a sample with a large age range from 6 to 14 years.
In this study, SE measured using cycloplegic refraction by trained ophthalmologists or optometrists, provided a realistic measure of the extent of myopia, with a statistically significant difference between the pre-and post-pandemic values. The mean change in SE of −0.11 D indicated accelerated myopia progression during the post-pandemic period. Wang et al reported a mean change of −0.30 D in non-cycloplegic SE refraction in children aged 6–8 years.3 Although Hu et al reported a −0.35 D shift in SE cycloplegic refraction, their sample was limited to children from grades 2 and 3.13 Compared to other studies, our sample size included a wider range of age group, and utilized cycloplegic refraction, which may explain the lower mean change in SE. Picotti et al showed an increase in myopia progression compared to pre-pandemic median values, however, risk factors were not studied.17
In this study, 88% of children with daily outdoor activity ≤2 h had a 45% higher risk of myopia worsening compared to patients who spent adequate time outdoors. The findings are comparable to those in another study in which children who had 2 h of daily outdoor activity had a 33% lower risk of myopia progression.12 In addition, in a study by He et al, 40 min spent outdoors was found to reduce the incidence of myopia over 3 years.14 Another study showed an increase in myopia progression among children aged between 7 and 12 years during the COVID-19-associated lockdown; although outdoor time decreased significantly during the pandemic, the authors found no association between myopia progression and outdoor time.15 To explain the effect of outdoor activities on myopia, two hypotheses have been proposed: first, in contrast to sunlight, interior illumination focuses behind the retina owing to its longer wavelengths, encouraging axial growth; second, axial myopia is controlled by light-induced dopamine release.18
Patients who spent > 4 h per day in front of screens for recreational purposes had a 26% higher risk of myopia worsening than those who spent less time in front of screens. In some reports, increased screen time > 5 h per day accelerated myopia progression.15,16 In addition, in a cross-sectional study, Chen et al found a higher prevalence of myopia in children who used electronic devices for extended periods.11 A substitution effect was proposed to explain the increased use of digital devices at the expense of spending time outside, which results in more near work and myopia.19 However, Aslan and Sahinoglu-Keskek found no statistically significant correlation between screen time and myopia during home confinement.12 Interestingly, in this study, educational screen time did contribute to myopia progression.
In our 3-year follow-up, the effect of myopia was less noticeable in the older age groups; survival analysis showed that the older age group had a 29% lower risk of myopia progression than the lower age group. In a study conducted in Shanghai, China, older age was found to have a similar protective effect.15 French et al20 compared the prevalence of myopia in younger (6–8 years old) and older (9–13 years old) children. Despite the older group taking longer online courses, they reported a higher increase among the younger group. Thus, younger children are more vulnerable to environmental factors.3,20
Due to the low socioeconomic status of our study sample, most patients used mobile phones (62%). A significant progression was expected. However, due to the lack of sufficient comparison groups, we used the mobile phone group as a reference group for comparison with other device groups, and the differences in myopia progression were not statistically significant, which is similar to the findings in other studies.12 Ma et al showed that patients using televisions and projectors had slower myopia progression than those using other near-distance devices such as phones and tablets.15 Moreover, the low socioeconomic status could be a risk factor for myopia incidence and progression. Philip et al noted that myopia is more prevalent in children with poor socioeconomic status.21,22 However, family income was not one of the demographics studied in our cohort.
Over a three year period during the pandemic, our study looked at the progression and risk factors of myopia in school aged children using cycloplegic refraction. The findings of this study should be interpreted in light of its limitations. As this was a retrospective study, the time spent in front of the screen and outside were reported by parents, which may have influenced the accuracy of the actual number of hours spent daily on those activities. We did not include ocular biometry, such as corneal keratometry and axial length, because relevant data were not collected in this study. Most patients in this study had a low socioeconomic status and did not own a laptop or any other tablet besides their parent’s phone. Further research that includes ocular biometry, bigger sample size, wider range of age group, different socioeconomic backgrounds and ethnic groups may provide additional information about myopia progression.
Conclusion
Myopia progression, assessed based on changes in SE, was accelerated during the COVID-19 pandemic compared to pre-pandemic times. Younger age, prolonged screen use, and lack of outdoor time contributed to an increase in myopia. However, the type of device had no statistically significant effect on myopia progression.
Synopsis/Precis
Regardless of the type of device used, home confinement, prolonged screen time, and decrease outdoor activity have led to the acceleration of myopia in school-aged children during the COVID-19 pandemic.
Acknowledgment
The abstract of this paper was presented as a poster presentation with interim findings at the ARVO annual meeting, May 1–4 2022, at Denver, Colorado. The poster’s abstract was published in Investigative Ophthalmology & Visual Science (IOVS) an ARVO journal, June 2022. Volume 63, Issue 7.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Sohrabi C, Alsafi Z, O’Neill N, et al. World Health Organization declares global emergency: a review of the 2019 novel coronavirus (COVID-19). Int J Surg. 2020;76(1):71–76. doi:10.1016/j.ijsu.2020.02.034
2. Nguyen NV. The impact of COVID-19 on education activity at Tra Vinh University – Vietnam. J Res Lepid. 2020;51(3):109–122. doi:10.36872/LEPI/V51I3/301173
3. Wang J, Li Y, Musch DC, et al. Progression of myopia in school-aged children after COVID-19 home confinement. JAMA Ophthalmol. 2021;139(3):293. doi:10.1001/jamaophthalmol.2020.6239
4. Pizzarello L, Abiose A, Ffytche T, et al. The right to sight: a global initiative to eliminate avoidable blindness. Arch Ophthalmol. 2004;122(4):615–620. doi:10.1001/archopht.122.4.615
5. Morgan I, Rose K. How genetic is school myopia? Prog Retin Eye Res. 2005;24(1):1–38. doi:10.1016/j.preteyeres.2004.06.004
6. Liang C-L, Yen E, Su J-Y, et al. Impact of family history of high myopia on level and onset of myopia. Invest Ophthalmol Vis Sci. 2004;45(10):3446. doi:10.1167/iovs.03-1058
7. Holden BA, Fricke TR, Wilson DA, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036–1042. doi:10.1016/j.ophtha.2016.01.006
8. Mutti DO, Mitchell GL, Moeschberger ML, Jones LA, Zadnik K. Parental page 7 of 9 myopia, near work, school achievement, and children’s refractive error. Invest Ophthalmol Vis Sci. 2002;43(12):3633–3640.
9. Chen F, He X, Tang J, et al. Prevalence of myopia and associated risk factors among primary students in the period of online study during COVID-19: a cross-sectional study in Guangzhou. Int J Ophthalmolo Vis Sci. 2020;5(4):84–89. doi:10.11648/j.ijovs.20200504.11
10. 2021 world population by country. 2021 world population by country; n.d. Available from: http://www.worldpopulationreview.com./.
11. Robaei D, Rose K, Ojaimi E, Kifley A, Huynh S, Mitchell P. Visual acuity and the causes of visual loss in a population-based sample of 6-year-old Australian children. Ophthalmology. 2005;112(7):1275–1282. PMID: 15921756. doi:10.1016/j.ophtha.2005.01.052
12. Aslan F, Sahinoglu-Keskek N. The effect of home education on myopia progression in children during the COVID-19 pandemic. Eye. 2021:1–6. doi:10.1038/s41433-021-01655-2
13. Hu Y, Zhao F, Ding X, et al. Rates of myopia development in young Chinese schoolchildren during the outbreak of COVID-19. JAMA Ophthalmol. 2021;139(10):1115–1121. doi:10.1001/JAMAOPHTHALMOL.2021.3563
14. He M, Xiang F, Zeng Y, et al. Effect of time spent outdoors at school on the development of myopia among children in China a randomized clinical trial. J Am Med Assoc. 2015;314(11):1142–1148. doi:10.1001/jama.2015.10803
15. Ma M, Xiong S, Zhao S, Zheng Z, Sun T, Li C. COVID-19 home quarantine accelerated the progression of myopia in children aged 7 to 12 years in China. Invest Ophthalmol Vis Sci. 2021;62(10):37. doi:10.1167/IOVS.62.10.37
16. Zhang X, Cheung SSL, Chan HN, et al. Myopia incidence and lifestyle changes among school children during the COVID-19 pandemic: a population-based prospective study. Br J Ophthalmol. 2021. doi:10.1136/bjophthalmol-2021-319307
17. Picotti C, Sanchez V, Fernandez IL, et al. Myopia progression in children during COVID-19 home confinement in Argentina acknowledgments group of ophthalmologists in pandemia (by order of enrolment). SSRN. n.d.;14(3):1.
18. Cao K, Wan Y, Yusufu M, Wang N. Significance of outdoor time for myopia prevention: a systematic review and meta-analysis based on randomized controlled trials. Ophthalmic Res. 2020;63(2):97–105. doi:10.1159/000501937
19. Lanca C, Saw SM. The association between digital screen time and myopia: a systematic review. In: Ophthalmic and Physiological Optics. Vol. 40. John Wiley & Sons, Ltd.; 2020:216–229. doi:10.1111/opo.12657
20. French AN, Morgan IG, Mitchell P, Rose KA. Risk factors for incident myopia in Australian school children. Ophthalmology. 2013;120(10):2100–2108. doi:10.1016/j.ophtha.2013.02.035
21. Enthoven CA, Mölenberg FJM, Tideman JWL, et al. Physical activity spaces not effective against socioeconomic inequalities in myopia incidence: the generation R study. Optom Vis Sci. 2021;98(12):1371–1378. PMID: 34759237; PMCID: PMC8677612. doi:10.1097/OPX.0000000000001809
22. Nouraeinejad A. Urban inequality: a hypothetic risk factor for myopia. Med Hypothesis Discov Innov Ophthalmol. 2022;2(4):146–149. doi:10.51329/mehdioptometry139
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The
full terms of this license are available at https://www.dovepress.com/terms.php
and incorporate the Creative Commons Attribution
- Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted
without any further permission from Dove Medical Press Limited, provided the work is properly
attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
Recommended articles
Suicide and Suicide Attempts Among Patients Attending Primary Health Care Facilities in Uganda: A Medical Records Review
Kaggwa MM, Rukundo GZ, Wakida EK, Maling S, Sserumaga BM, Atim LM, Obua C
Risk Management and Healthcare Policy 2022, 15:703-711
Published Date: 19 April 2022
COVID-19 Pandemic and Physician Burnout: Ramifications for Healthcare Workforce in the United States
Bhardwaj A
Journal of Healthcare Leadership 2022, 14:91-97
Published Date: 13 June 2022
Behavioural Response To Self-Medication Practice Before and During Covid-19 Pandemic in Western Uganda
Dare SS, Eze ED, Echoru I, Usman IM, Ssempijja F, Bukenya EE, Ssebuufu R
Patient Preference and Adherence 2022, 16:2247-2257
Published Date: 20 August 2022
The Need for Speed: A Qualitative Study on Nurse Recruitment and Management Amidst the COVID-19 Pandemic in Indonesia
Efendi F, Aurizki GE, Auwalin I, McKenna L
Journal of Multidisciplinary Healthcare 2022, 15:1809-1817
Published Date: 27 August 2022
Factors Associated with Anxiety During COVID-19 Pandemic and Its Association with Hypertension in Saudi Arabia
Said B, Gharawi MO, Dallak FH, Maashi AQ, Hurissi E, Gharawi SO, Tarshi MM, Hayyan AI, Faqihi SA, AlMusawa HI, Hakami GM, Alhazmi AH
Patient Preference and Adherence 2023, 17:905-912
Published Date: 29 March 2023
