Back to Journals » Patient Related Outcome Measures » Volume 14
Incidence and Associated Factors of Postoperative Undesirable Anesthetic Outcomes Among Surgical Patients at Referral Hospitals in Amhara Region, Ethiopia: A Multi-Center Study
Authors Admassie BM , Admass BA , Yaregal Melesse D
Received 23 February 2023
Accepted for publication 12 May 2023
Published 16 May 2023 Volume 2023:14 Pages 137—152
DOI https://doi.org/10.2147/PROM.S403697
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Robert Howland
Belete Muluadam Admassie, Biruk Adie Admass, Debas Yaregal Melesse
Department of Anesthesia, School of Medicine, College of Medicine and Health Science, University of Gondar, Gondar, Ethiopia
Correspondence: Biruk Adie Admass, Email [email protected]
Background: Patients undergoing surgery frequently experience unfavorable anesthetic outcomes. They may have an impact on body systems and result in more serious postoperative morbidities. This study was conducted to determine the incidence of postoperative undesirable anesthetic outcomes among surgical patients at referral hospitals in Amhara region, Ethiopia.
Methods: A total of 412 patients, who underwent surgical procedures between August 1 and October 30 of 2022, were included in this study. The Leiden Perioperative Care Patient Satisfaction Questionnaire’s (LPPSq) dimension “discomfort and needs” was used to collect data on the first postoperative day. Data entry and analysis were performed using SPSS version 20. To assess how risk factors affected the outcome variable, logistic regression analysis was utilized. In multivariable logistic regression analysis, a variable with a P-value of less than 0.05 was statistically considered as significant.
Results: The proportion of those who had “at least a little bit” of unfavorable outcomes was calculated to estimate their overall prevalence, and the prevalence of those who had “more than moderate” levels of unfavorable outcomes was determined to appreciate how severe these outcomes were. The percentages of postoperative pain, the most common undesired result, for “at least a little bit” and “more than moderate” were 87.7% and 32.3%, respectively. In this study, postoperative cold was the least prevalent (51.4%) undesirable anesthetic outcome. The remaining undesirable postoperative outcomes were reported less frequently.
Conclusion and Recommendation: Undesirable postoperative anesthetic outcomes were still common. The most frequent unfavorable result was postoperative pain. Adequate postoperative patient follow-up and quality service are paramount.
Keywords: undesired anesthetic outcome, postoperative complication, postoperative outcome, surgery, anesthesia
Introduction
Undesirable postoperative anesthetic outcomes are common after surgery. Unfavorable anesthetic outcomes are adverse events that can affect all of the patient’s body systems.1,2
Most postoperative complications occur at a post anesthesia care unit (PACU). These may arise from the squeal of operations, anesthetic and analgesic agents, worsening co-morbidities.1
Postoperative pain is a regular occurrence and is a major issue that anesthesia professionals face on a daily basis.3,4 One of the reasons for various medical difficulties is inadequate care of immediate postoperative pain. This results in longer hospital stays and slower recovery times, which raises the postoperative morbidity rate.5,6
Postoperative nausea, vomiting, sore throat, thirst, hunger, and cold were frequently reported unwanted anesthetic outcomes.1 In most cases, postoperative complications that are more severe and persistent are linked to failure to prevent these unwanted outcomes.7 These have also been delineated as avoidable causes of patient’s dissatisfaction.8 Through accurate and prompt identification of the symptoms and use of the right medication, these unwanted events can be managed as effectively as possible.9 The provision of high-quality care depends on the diagnosis and treatment of these unwanted post-anesthetic outcomes.7,9
Patients in our facility have been seen to experience these issues during their recovery periods. Although most studies had reported a high prevalence of postoperatively undesirable anesthesia outcomes, no studies were conducted in Ethiopia. As a result, determining the magnitude of unfavorable postoperative anesthesia outcomes and the factors is critical for taking early and appropriate intervention.
Methods and Materials
Study Design and Period
A multicentre institution-based cross-sectional study was performed on 412 surgical patients at referral hospitals in Amhara regional state in Ethiopia from April 1, 2022, to October 30, 2022, to determine the magnitude and contributing factors of undesirable anesthetic outcomes after surgery. The study was conducted in University of Gondar comprehensive specialized referral hospital, Tibebe Gihon referral hospital, Debre Tabore referral hospital, and Debre Markos referral hospital. Following approval of the ethical concern, the ethical review committee of the college of medicine and health sciences provided ethical clearance. Letter of permission was obtained from each hospital’s medical director.
All patients age 18 and older who were able to express their condition and operated under anesthesia were included. Patients who were uncooperative, had decreased cognitive function, were unconscious after surgery, were released before 24 hours of the postoperative period, and had upper respiratory tract infections prior to surgery were excluded from the study.
Sample Size Determination
Single population proportion formula was applied to estimate the sample size. The number of study participants was calculated with a 95% level of confidence and a 5% margin of error. In Ethiopia, no similar study was conducted to determine the magnitude of postoperatively undesirable outcomes. As a result, the 0.5 proportion assumption was applied. The ultimate sample size was 424, with a 10% non-response rate. Patients who met the inclusion criteria were consecutively selected in the study until the required sample is reached.
Data Collection Procedure
Prior to their operation, patients were recruited. Patients provided written consent after receiving a clear description of the study’s objective and assurances of confidentiality and anonymity. After confirming them that they felt at ease to provide information, the study was conducted in their respective postoperative wards. A chart review and a structured questionnaire-based patient interview were used to collect data. The components of the patients’ socio-demographic and medical characteristics were recorded in the data collecting form. From the chart, patient-related, surgical-related, and anesthesia-related factors were recorded.
Patients were interviewed 24 hours following the procedure to identify if they had any unfavorable anesthetic outcomes, using the dimension “discomfort and needs” of the Leiden Perioperative Care Patient Satisfaction Questionnaire (LPPSq). Translation of the dimension of leiden perioperative care patient satisfaction questionnaire from English language to Amharic, the local spoken language, was performed. Questions in the dimension were standardized and measured using a five-point likert scale from “not at all” to “extremely”. An expert opinion from the anesthesiology department was used to assess the content validity of the items in the dimension, as well as the internal consistency of the dimension (Cronbach = 0.66).1
Data Quality Control
A pre-test was conducted on 10% of participants. The data have been checked for completeness, accuracy, and clarity by the lead investigator. Training was provided to data collectors on how to use the data collection tools and how to collect data. Finally, data had been cleaned up and cross-checked prior to analysis.
Data Analysis
Data were coded, entered, and checked for errors using SPSS software (version 20). SPSS version 20 was used to analyze data. The Shapiro–Wilk normality test was applied to check the data distribution. Bivariate logistic regression was used to assess predictor factors that influence the result, and variables with a p-value less than 0.2 in bivariate logistic regression were fitted for multivariate logistic regression. Normally distributed data were displayed as mean and standard deviation, whereas categorical data were presented as frequency and percentage. In multivariable logistic regression, p-values less than 0.05 are considered statistically significant.
Operational Definition
Undesired anesthesia outcomes are complications that commonly affect all body systems and occur after surgery.1
Ethical Consideration
The ethical consideration was approved by the ethical committee of college of medicine and health sciences at University of Gondar. Referral hospitals, where the study was conducted, in the Amhara region provided a letter of permission. The study’s objectives and significance were described, and each participant provided written consent. During all stages of the investigation, confidentiality was maintained. The study was conducted in compliance with the declaration of Helsinki.
Results
Socio-Demographic and Clinical Characteristics
Four hundred and twenty-four patients with a 97.2% response rate participated. Four hundred and twelve patients were included in the data analysis. Age of the patients was in between 18 and 70 years with mean and standard deviation of (Mean±SD) 33.8±11.8. The majority of the participants, 238 (57.8%), were men, with 256 (62.1%) having a normal BMI. About 211 (51.2%) were ASA I physical status, 187 (45.4%) underwent general surgery, and most of the remaining 240 (58.3%) received general anesthesia (Table 1 and Table 2).
 |
Table 1 Demographic and Medical Characteristics of the Patients with Continuous Variables (N = 412) |
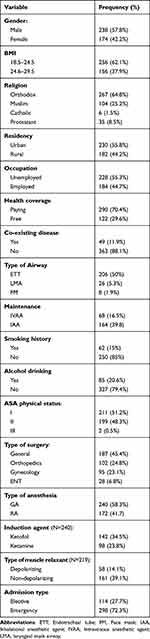 |
Table 2 Frequency Distribution of Socio-Demographic and Medical Characteristics of the Patients (N = 412) |
Prevalence of Undesirable Postoperative Anesthetic Outcomes
The frequency distribution of undesirable anesthetic outcomes and the prevalence with “at least a little bit” and “more than moderate” were reported (Table 3 and Table 4). The most prevalent undesirable postoperative anesthetic outcome was pain, followed by nausea, thirst, headache, back pain, sore throat, vomiting, hunger, and a cold. The proportion of “at least a little bit” and “more than moderate” for the most observed undesirable anesthetic outcome, pain, was 362 (87.7%) and 133 (32.35%), respectively. The percentage of “at least a little bit” and “more than moderate” for the least prevalent variable, cold, was 212 (51.4%) and 138 (34.4%), respectively (Table 4).
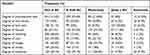 |
Table 3 Frequency Distribution of Undesirable Postoperative Anesthetic Outcomes (N = 412) |
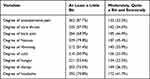 |
Table 4 Prevalence of Undesirable Postoperative Anesthetic Outcomes (N = 412) |
Undesirable Postoperative Anesthetic Outcomes Among Surgical Patients and Associated Factors
The associations of undesirable postoperative anesthesia outcomes with the independent variables were computed. Postoperative pain was three times [AOR: 2.96, 95% CI: 0.01, 3] higher in patients who underwent orthopedic surgery compared to other types of surgery. When compared to patients who received general anesthesia, patients who underwent surgery under regional anesthesia were less likely [AOR: 0.26, 95% CI: 0.008, 0.8] to develop postoperative pain. Patients induced with ketofol were thirteen times [AOR: 13, 95% CI: 2.95, 60] high likely to develop postoperative pain compared to those induced with ketamine. Patients who received a depolarizing muscle relaxant were greater than four times [AOR: 4.4, 95% CI: 1.1, 18] more likely to develop postoperative pain (Table 5).
 |
Table 5 Multivariate Logistic Regression Analysis of Undesirable Postoperative Anesthesia Outcomes with Independent Variables |
The odds of having post operative sore throat were more than eleven folds [AOR: 11.4, 95% CI: 2.2, 58.9] higher among smoker patients compared to non smoker. Patients who underwent general surgery were two times [AOR: 2, 95% CI: 0.2, 19.9] more likely to develop a postoperative sore throat. Patients who underwent surgery under general anesthesia were more likely [AOR: 1.5, 95% CI: 0.67, 3.44] to develop a postoperative sore throat compared to those who underwent RA. Compared to other types of airway maintenance, using a face mask decreased the risk of postoperative sore throat by 0.4 times [AOR: 0.4, 95% CI: 0.3, 1.7] (Table 5).
The odds of having postoperative back pain were more than twice [AOR: 2.3, 95% CI: 1.2, 4.5] higher among farmers compared to non-farmers. Those patients who had an age below the mean were 0.4 times [AOR: 0.4, 95% CI: 0.23, 0.76] less likely to develop postoperative back pain, and patients who received regional anesthesia were 1.5 times [AOR: 1.5, 95% CI: 0.88, 2.8] more likely to develop postoperative back pain compared to those who received GA (Table 5).
Males were 0.2 times [AOR: 0.2, 95% CI: 0.09, 0.3] less likely than females to develop postoperative nausea. Non-smokers have 1.3 times [AOR: 1.3, 95% CI: 0.2, 8.13] higher odds of postoperative nausea than smokers. Patients who received RA 0.2 times [AOR: 0.2, 95% CI: 0.07, 0.64] had a lower risk of developing postoperative nausea than those who received GA. Postoperative nausea occurs 17 times [AOR: 17, 95% CI: 1.89, 59.8] and 1.83 times [AOR: 1.83, 95% CI: 0.65, 5] when ketamine is used as an induction agent and IAA is used as a maintenance agent (Table 5).
The odds of having postoperative vomiting 0.14 times [AOR: 0.14, 95% CI: 0.03, 0.55] were less likely to occur in non-smokers compared to smokers. Patients who received GA had a 10-fold [AOR: 10, 95% CI: 3.1, 35] higher risk of postoperative vomiting than those who received RA. Using ketamine as an induction agent 1.9 times [AOR: 11.9, 95% CI: 3.9, 6.3] more likely develops postoperative vomiting, and being female 2.8 times [AOR: 2.8, 95% CI: 1.12, 7.33] more likely develops postoperative vomiting (Table 5).
The risk of developing a postoperative cold was about three times [AOR: 2.8, 95% CI: 1.12, 7.33] higher in females compared to males. When IAA was used as anesthesia maintenance, the odds of having postoperative hunger were about three times [AOR: 2.8, 95% CI: 1.12, 7.33] higher than when IVAA was used as maintenance (Table 5).
Postoperative thirst was 0.2 times [AOR: 0.2, 95% CI: 0.05, 0.45], 0.16 times [AOR: 0.16, 95% CI: 0.04, 0.6], 0.1 times [AOR: 0.1, 95% CI: 0.009, 0.36], and 0.3 times [AOR: 0.3, 95% CI: 0.7, 1] less likely in patients who were younger, male, and had no coexisting conditions. Having general anesthesia increased the risk of postoperative thirst by three times [AOR: 3, 95% CI: 1.17, 12.7] (Table 5).
Postoperative headache among females was 2.8 times [AOR: 2.8, 95% CI: 6.4, 92.8] more likely to develop compared to males. Postoperative headache occurred more than eight times [AOR: 8.3, 95% CI: 2.2, 31.5], 3 times [AOR: 3, 95% CI: 1.17, 12.7], and two times [AOR: 2, 95% CI: 0.99, 8.4] more likely in ENT surgery; the patient received GA and IAA as maintenance anesthesia, respectively (Table 5).
Discussion
This study focuses on common undesirable postoperative anesthetic outcomes reported by patients. Similar to previous studies done in Eritrea,1 and Singapore4 the most frequent unwanted postoperative anesthetic outcome was pain (87.7%). Despite the fact that postoperative optimal pain control is a crucial part of providing high-quality postoperative patient care,10 our findings indicate that postoperative pain prevalence was still high. This is supported by a study conducted in Kilimanjaro, Africa, which reported that a high prevalence of postoperative pain (73%).11 This could be because the anesthetist’s work does not extend beyond the operating room, and the management of these events is left to either the surgeon or the ward nurses. It has been suggested that nurses’ lack of knowledge and attitude toward pain management were variables influencing effective pain management.12
Similar to a study done in Tanzania10 patients underwent orthopedics surgery had significant association with postoperative pain. This might be due to the generally known fact that bone surgeries are associated with more severe pain and poor postoperative pain control.13,14
In this study, using ketamine significantly decreased the occurrence of postoperative pain. This might be explained by the use of N-methyl-D-aspartate (NMDA) receptor antagonists effective for the control of postoperative pain and, therefore, ketamine exerts its main analgesic effect by antagonizing NMDA receptors.15 In addition, depolarizing muscle relaxants have a high likelihood of postoperative pain that might be related to suxamethonium-induced myalgia.
In this study, the proportion of undesirable postoperative thirst was 73.5%. It is higher compared to previous study done in University of Gondar comprehensive and specialized hospital (59.4%),16 Eritrea (27.7%),1 China (58.7%)17 and Taiwan University Hospital (55.8%).18 This disparity could be attributable to an underestimation of the condition, since the quality of postoperative care varies by nation. Also, most professionals do not want to examine their patients’ thirst. Patients in the postoperative period face the most merciless part of their thirst after fasting for overly long durations, sometimes due to the surgical staff’s lack of expertise about managing thirst safely in the perioperative phase.19
This study revealed that the type of anesthesia used was significantly related to the proportion of thirst after surgery. Patients who received general anesthesia have a higher probability of developing postoperative thirst than those who had regional anesthesia. This result is in line with studies conducted in Ethiopia, Taiwan, and Brazil.16,19,20 This association could be due to the fact that we used different drugs and airway equipment during general anesthesia. The effects of the different anesthetic agents, endotracheal intubation, and a prolonged NPO time may increase the risk of postoperative thirst.
Postoperative nausea and vomiting are unpleasant and commonly occurring phenomena after surgical procedures. The magnitude of nausea and vomiting in this study was 79.8% and 51.4%, respectively. It was higher compared to previous studies in Ethiopia (35.2% and 20%),21 Eritrea (40.6% and 37.7%)1 and Iran (31.4% and 16.8%).22 This could be explained by the current practice of nausea and vomiting prophylaxis in this clinical setting was suboptimal.23 This large disparity in prevalence may be related to changes in surgery and anesthetic practices, study designs, and tools used to assess nausea.
The finding of this study revealed that being female and a nonsmoker increased the likelihood of postoperative nausea and vomiting. Even though the risk of postoperative nausea and vomiting is a multidimensional phenomenon, female gender, nonsmoker, and increased age were the main predictors of postoperative nausea and vomiting (PONV).24–26
In our study, patients receiving general anesthesia with ketofol as an induction agent and IAA for maintenance anesthesia had a higher likelihood of postoperative nausea and vomiting. This is supported by a study conducted in Uganda, in which the incidence of PONV was low due to propofol’s antiemetic effect.27 Another possibility is that because most inhalation anesthetics are circulatory depressants and vasodilators, they create hypotension, which leads to intestinal hypoperfusion. Intestinal hypoperfusion can produce serotonin release, which can lead to PONV via vagal afferent activation in the GI tract.
Postoperative sore throat was the most reported patients’ most undesirable outcome.28 The percentage of postoperative sore throat was 57.0%. This was higher than previous studies in China (16%)29 and Eritrea (18.5%).1 This discrepancy might be due to differences in airway equipment and assessment tools, and there may also be clinical setting differences. On the contrary, the proportion of postoperative sore throat was lower than a study in Gondar (80%).28 This difference could be attributed to a variation in the description of the problem and the techniques utilized to assess the prevalence of sore throats.
One of the most common negative postoperative anesthesia outcomes in patients who had surgery under general anesthesia versus regional anesthesia was a postoperative sore throat. This might be explained by the fact that during general anesthesia technique, the insertion of airway equipment is an inherent risk factor of a postoperative sore throat.30
The occurrence of sore throat was higher in patients who underwent surgery under ETT anesthesia versus LMA and FM anesthesia, according to our findings. This report was in agreement with a previous study showing that the incidence of postoperative sore throat during LMA anesthesia is lower compared with tracheal tube insertion.31 When inserting a tracheal tube, postoperative throat complications are, intuitively, more likely.32 This may be due to coughing or movement due to inadequate anesthesia or neuromuscular blockade; glottis exposure may be difficult; and airway trauma during insertion, tracheal lumen irritation, and ischemia due to cuff pressure are more common during ETT anesthesia. Furthermore, similar to previous study in Ethiopia,28 patients underwent general surgery had high risk compared to other type of surgery. This could be because most general surgery performed under general anesthesia in our setting necessitates the insertion of airway equipment.
In this study, the prevalence of postoperative back pain was 68.9%. It was higher than studies done in Eritrea (26.6%)1 and Gondar, Ethiopia.33 This disparity may be due to differences in sample size, anesthesia type, and clinical setting. In adults, the incidence of back discomfort following neuraxial anesthesia is comparable to that following general anesthesia.34 However, patients who got regional anaesthetic had a higher incidence of postoperative back pain than those who received general anesthesia, according to this study. Postoperative back pain is frequently reported after RA.35 It could be related to soft tissue damage during lumbar puncture.36
Hunger is a complex process involving neuronal and systemic components.17 Early initiation of postoperative feeding accelerates bowel function recovery and decreases paralytic illus.37,38 The prevalence of postoperative hunger was 50.9%. This result was higher than an Eritrean (18.3%)1 and Chinese studies (47.47%).17 This disparity could be attributed to the technique used to assess postoperative hunger and the quality of postoperative patient care, which varies by setting. Another possible explanation may be a difference between clinical practice and feeding protocols.39,40
In this study, using an inhalational anesthetic agent (IAA) as anesthesia maintenance had a significant relation with the occurrence of postoperative hunger compared to using an IVAA. This might be due to the fact that anesthetic drugs alter feeding behavior. Unlike isoflurane, propofol induces feeding behavior in mice for at least six hours.37,41 Previous study done in France has shown that, compared with sevoflurane, propofol did not accelerate the recovery of appetite after outpatient minor surgery.42 Furthermore, propofol had no influence on other clinical or biological markers connected with food intake.
Postoperative headache is a minor postoperative morbidity. It significantly increases postoperative morbidity by necessitating higher pain medication doses, lowering overall patient satisfaction, and even delaying patients’ discharge.43 In this study, the prevalence of postoperative headache was 70.8%. This finding was higher compared to studies done in University of Athens, Greece (28.3%)44 and Eritrea (25.1%).1 This might be due to differences in the assessment tool and clinical setting.
Similar to a previous study done in Greece,44 female gender, nonsmoker status, and patients who underwent ENT surgery, received GA, and used IAA as maintenance of anesthesia were found to be strongly linked with the occurrence of postoperative headache, whereas alcohol consumption and ketamine use were found to be unrelated. In contrast to our finding, patients have co-existing diseases, and the anesthetic and adjuvant drugs administered [N-methyl-d-aspartate (NMDA) receptors] contribute to the occurrence of postoperative headache.45,46
Being female increases the risk of postoperative headache43 and this could be hormonal or psychological differences in females. Smokers have a higher likelihood of experiencing postoperative headaches. The possible explanation might be that smoking is strongly related with vascular disease or withdrawal from tobacco. In our findings, alcohol consumption did not have any effect on the incidence of postoperative headache. In contrast to our finding in a previous study, which stated that alcohol consumption is an independent factor for perioperative headache occurrence.47
Limitation of the Study
This study was conducted after 24 hr of completion of surgery. Patients may experience undesirable anesthetic outcomes immediately within 24 hours of end of surgical procedures. As a result, patients may be missed and not included in the study.
Conclusion and Recommendation
Undesirable postoperative anesthetic outcomes were still common. The most frequent unfavorable result was postoperative pain, whereas postoperative cold was the least frequent postoperative anesthetic outcome. Appropriate postoperative patient follow-up and quality service are paramount. Furthermore, reliable and valid monitoring of anesthetic outcomes is crucial for improving postoperative anesthetic care.
Data Sharing Statement
At reasonable request, the corresponding author will release the data sets used and analyzed during the study.
Ethical Approval
The study gained ethical clearance and approval from the College of Medicine and Health Sciences’ ethical review committee at the University of Gondar. Letter of permission was obtained from each referral hospitals in Amhara region. Each study participant completed a written informed consent form after receiving a full explanation. Confidentiality was protected by preventing personal identification and locking the completed questionnaires.
Acknowledgment
The department of anesthesia and the department of surgery provided excellent cooperation, which the authors appreciate for their contributions.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study received no financing from public, private, or non-profit organizations.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Andemeskel YM, Elsholz T, Gebreyohannes G, Tesfamariam EH. Undesirable postoperative anesthesia outcomes at two national referral hospitals: a cross-sectional study in Eritrea. Anesthesiol Res Pract. 2020;2020:1.
2. Kellner DB, Urman RD, Greenberg P, Brovman EY. Analysis of adverse outcomes in the post-anesthesia care unit based on anesthesia liability data. J Clin Anesth. 2018;50:48–56. doi:10.1016/j.jclinane.2018.06.038
3. Abdalrahim MS. Postoperative pain assessment and management: the effects of an educational program on Jordanian nurses’ practice, knowledge, and attitudes. Int J Health Sci. 2009;2009:1.
4. Look X, Mok MUS, Tay YS, Abdullah HR. How do Singapore patients view post-anaesthesia adverse outcomes? A single-centre willingness-to-pay study. Singapore Med J. 2018;59(5):264. doi:10.11622/smedj.2017078
5. Fletcher D, Fermanian C, Mardaye A, Aegerter P. A patient-based national survey on postoperative pain management in France reveals significant achievements and persistent challenges. PAIN. 2008;137(2):441–451. doi:10.1016/j.pain.2008.02.026
6. Dumolard P, Gök M, Le N. Nurses’ responsibilities in postoperative pain management following total Hip arthroplasty; 2017.
7. Paavolainen L, Wallstedt J. Post-operative complications of general anesthesia: a recorded video presentation; 2016.
8. Falco D. Patient satisfaction with anesthesia care what do we know? AANA J. 2017;85:4.
9. Malczyk D, Marczak K, Miśtal A, Solga K, Borodzicz AM, Krzemińska SA. Are there any unwanted anesthesia symptoms in patients undergoing anesthesia?. J Edu Health Sport. 2018;8(9):77–89.
10. Mwashambwa MY, Yongolo IM, Kapalata SNW, Meremo AJ. Post-operative pain prevalence, predictors, management practices and satisfaction among operated cases at a regional referral hospital in Dar es Salaam, Tanzania. Tanzan J Health Res. 2018;20:2. doi:10.4314/thrb.v20i2.10
11. Ndebea AS, van den Heuvel SA, Temu R, Kaino MM, van Boekel RL, Steegers MA. Prevalence and risk factors for acute postoperative pain after elective orthopedic and general surgery at a tertiary referral hospital in Tanzania. J Pain Res. 2020;13:3005. doi:10.2147/JPR.S258954
12. Admassie BM, Lema GF, Ferede YA, Tegegne BA. Emergency nurses perceived barriers to effective pain management at emergency department in Amhara region referral hospitals, Northwest Ethiopia, 2021. Multi-center cross sectional study. Ann Med Surg. 2022;81:104338. doi:10.1016/j.amsu.2022.104338
13. Apfelbaum JL, Chen C, Mehta SS, Gan TJ. Postoperative pain experience: results from a national survey suggest postoperative pain continues to be undermanaged. Anesth Analg. 2003;97(2):534–540. doi:10.1213/01.ANE.0000068822.10113.9E
14. Arendt-Nielsen L, Fernández-de-Las-Peñas C, Graven-Nielsen T. Basic aspects of musculoskeletal pain: from acute to chronic pain. J Man Manip Ther. 2011;19(4):186–193. doi:10.1179/106698111X13129729551903
15. Kaur S, Saroa R, Aggarwal S. Effect of intraoperative infusion of low-dose ketamine on management of postoperative analgesia. J Nat Sci Biol Med. 2015;6(2):378. doi:10.4103/0976-9668.160012
16. Belete KG, Ashagrie HE, Workie MM, Ahmed SA. Prevalence and factors associated with thirst among postsurgical patients at University of Gondar comprehensive specialized hospital. Institution-based cross-sectional study. J Patient Rep Outcomes. 2022;6(1):1–8. doi:10.1186/s41687-022-00476-5
17. Lai L, Zeng L, Yang Z, Zheng Y, Zhu Q. Current practice of postoperative fasting: results from a multicentre survey in China. BMJ open. 2022;12(7):e060716. doi:10.1136/bmjopen-2021-060716
18. Lee C-W, Liu S-T, Cheng Y-J, Chiu C-T, Hsu Y-F, Chao A. Prevalence, risk factors, and optimized management of moderate-to-severe thirst in the post-anesthesia care unit. Sci Rep. 2020;10(1):1–10. doi:10.1038/s41598-019-56847-4
19. Pierotti I, Nakaya T, Garcia A, Nascimento L, Conchon M, Fonseca L. Thirst and fasting time assessment in surgical patients. Rev BaianaEnferm. 2018;32:e27679.
20. Gulia S, Kumari V, Khatri N. Effectiveness of an intervention bundle on thirst intensity and dry mouth among patients admitted in ICU. Int J Health Sci Res. 2019;9:397–408.
21. Hoyle J, Reddi D, Belayneh T. Prevalence and factors associated with postoperative nausea and vomiting at the University of Gondar teaching hospital, Northwest Ethiopia, 2012: a cross-sectional study. Ethiop J Health Bio Sci. 2014;6(1):49–57.
22. Amirshahi M, Behnamfar N, Badakhsh M, et al. Prevalence of postoperative nausea and vomiting: a systematic review and meta-analysis. Saudi J Anaesth. 2020;14(1):48. doi:10.4103/sja.SJA_401_19
23. Admass BA, Tawye HY, Endalew NS, et al. Assessment of post-operative nausea and vomiting prophylaxis usage for cesarean section, 2021: a cross sectional study. Ann Med Surg. 2022;75:103399. doi:10.1016/j.amsu.2022.103399
24. Doubravska L, Dostalova K, Fritscherova S, Zapletalova J, Adamus M. Incidence of postoperative nausea and vomiting in patients at a university hospital. Where are we today. Biomed Pap Med Fac Univ Palacky Olomouc Czech Repub. 2010;154(1):69–76. doi:10.5507/bp.2010.012
25. Stadler M, Bardiau F, Seidel L, Albert A, Boogaerts JG. Difference in risk factors for postoperative nausea and vomiting. J Am Soc Anesthesiolog. 2003;98(1):46–52.
26. Van den Bosch J, Kalkman C, Vergouwe Y, et al. Assessing the applicability of scoring systems for predicting postoperative nausea and vomiting. Anaesthesia. 2005;60(4):323–331. doi:10.1111/j.1365-2044.2005.04121.x
27. Ssebuufu R, Kakande I, Okello M. Post-operative nausea and vomiting at Mulago Hospital. East Cent Afr J Surg. 2009;14(2):50–57.
28. Gemechu BM, Gebremedhn EG, Melkie TB. Risk factors for postoperative throat pain after general anaesthesia with endotracheal intubation at the University of Gondar Teaching Hospital, Northwest Ethiopia, 2014. Pan Afr Med J. 2017;27:1.
29. Li X, Wang X, Zhao Y, et al. Incidence of postoperative sore throat after using a new technique of insertion of a second generation Laryngeal Mask Airway: a randomised controlled trial. Eur J Anaesthesiol. 2021;38(3):285. doi:10.1097/EJA.0000000000001378
30. El‐Boghdadly K, Bailey C, Wiles M. Postoperative sore throat: a systematic review. Anaesthesia. 2016;71(6):706–717. doi:10.1111/anae.13438
31. Banihashem N, Alijanpour E, Hasannasab B, Zarei A. Prophylactic effects of lidocaine or beclomethasone spray on post-operative sore throat and cough after orotracheal intubation. Iran J Otorhinolaryngol. 2015;27(80):179.
32. Calder A, Hegarty M, Erb TO, von Ungern‐Sternberg BS. Predictors of postoperative sore throat in intubated children. Paediatr Anaesth. 2012;22(3):239–243. doi:10.1111/j.1460-9592.2011.03727.x
33. Zeleke TG, Mersha AT, Endalew NS, Ferede YA. Prevalence and factors associated with back pain among patients undergoing spinal anesthesia at the University of Gondar Comprehensive and Specialized Hospital, North West Ethiopia: an institutional based cross-sectional study. Adv Med. 2021;2021:1.
34. Benzon HT, Asher YG, Hartrick CT. Back pain and neuraxial anesthesia. Anesth Analg. 2016;122(6):2047–2058. doi:10.1213/ANE.0000000000001270
35. Salam AA, Afshan G. Patient refusal for regional anesthesia in elderly orthopedic population: a cross-sectional survey at a tertiary care hospital. J Anaesthesiol Clin Pharmacol. 2016;32(1):94. doi:10.4103/0970-9185.173372
36. Tekgül ZT, Pektaş S, Turan M, Karaman Y, Çakmak M, Gönüllü M. Acute back pain following surgery under spinal anesthesia. Pain Pract. 2015;15(8):706–711. doi:10.1111/papr.12260
37. Nematihonar B, Salimi S, Noorian V, Samsami M. Early versus delayed (traditional) postoperative oral feeding in patients undergoing colorectal anastomosis. Adv Biomed Res. 2018;7. doi:10.4103/abr.abr_290_16
38. Charoenkwan K, Matovinovic E. Early versus delayed oral fluids and food for reducing complications after major abdominal gynaecologic surgery. Cochrane Database Syst Rev. 2014;12:1.
39. Le Pape S, Boisson M, Loupec T, Vigneau F, Debaene B, Frasca D. Postoperative fasting after general anaesthesia: a survey of French anaesthesiology practices. Anaesth Crit Care Pain Med. 2018;37(3):245–250. doi:10.1016/j.accpm.2017.11.012
40. Rattray M, Roberts S, Marshall A, Desbrow B. A systematic review of feeding practices among postoperative patients: is practice in‐line with evidenced‐based guidelines? J Hum Nutr Diet. 2018;31(2):151–167. doi:10.1111/jhn.12486
41. Besnier E, Clavier T, Tonon M-C, et al. Anesthetic drugs modulate feeding behavior and hypothalamic expression of the POMC polypeptide precursor and the NPY neuropeptide. BMC Anesthesiol. 2018;18(1):1–7. doi:10.1186/s12871-018-0557-x
42. Besnier E, Perdrix A, Gillibert A, et al. Postoperative hunger after outpatient surgery in patients anesthetized with propofol vs sevoflurane: a randomized-controlled trial. Can J Anaesth. 2020;67(5):550–559. doi:10.1007/s12630-020-01584-w
43. Myles P, Hunt J, Moloney J. Postoperative ‘minor’complications: comparison between men and women. Anaesthesia. 1997;52(4):300–306. doi:10.1111/j.1365-2044.1997.89-az0091.x
44. Matsota PK, Christodoulopoulou TC, Batistaki CZ, Arvaniti CC, Voumvourakis KI, Kostopanagiotou GG. Factors associated with the presence of postoperative headache in elective surgery patients: a prospective single center cohort study. J Anesth. 2017;31(2):225–236. doi:10.1007/s00540-016-2285-z
45. Ashkenazi A, Silberstein SD. Headache management for the pain specialist. Reg Anesth Pain Med. 2004;29(5):462–475. doi:10.1016/j.rapm.2004.05.008
46. Lipton R, Bigal M, Steiner T, Silberstein S, Olesen J. Classification of primary headaches. Neurology. 2004;63(3):427–435. doi:10.1212/01.WNL.0000133301.66364.9B
47. Gill P, Guest C, Rabey P, Buggy D. Perioperative headache and day case surgery. Eur J Anaesthesiol. 2003;20(5):401–403. doi:10.1097/00003643-200305000-00009
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
