Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 18
Impact of Cardiovascular and Metabolic Comorbidities on Long-term Outcomes of Home-based Pulmonary Rehabilitation in COPD
Authors Grosbois JM, Détrée A, Pierache A , Bautin N, Pérez T, Wallaert B , Chenivesse C , Le Rouzic O
Received 11 July 2022
Accepted for publication 31 October 2022
Published 23 February 2023 Volume 2023:18 Pages 155—167
DOI https://doi.org/10.2147/COPD.S381744
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Russell
Jean-Marie Grosbois,1 Axelle Détrée,2 Adeline Pierache,3,4 Nathalie Bautin,5,6 Thierry Pérez,5,6 Benoit Wallaert,5,6 Cécile Chenivesse,5,6 Olivier Le Rouzic5,6
1FormAction Santé, Pérenchies, F-59840, France; 2Groupe Hospitalier Loos Haubourdin, Réhabilitation Respiratoire, Loos, F-59120, France; 3Université de Lille, CHU Lille, ULR 2694 - METRICS: Évaluation des technologies de santé et des pratiques médicales, Lille, F-59000, France; 4CHU Lille, Department of Biostatistics, Lille, F-59000, France; 5Université de Lille, CHU Lille, CNRS, Inserm, Institut Pasteur de Lille, U1019 - UMR 9017 - CIIL - Center for Infection and Immunity of Lille, Lille, F-59000, France; 6CHU Lille, Pneumologie et Immuno-Allergologie, Centre de référence constitutif pour les maladies pulmonaires rares, Lille, F-59000, France
Correspondence: Olivier Le Rouzic, Pneumologie et Immuno-Allergologie, Institut Cœur Poumon, 1 boulevard Jules Leclercq, CHU de Lille, Lille, 59037, France, Tel +33 3 20 44 59 48, Fax +33 3 20 44 57 68, Email [email protected]
Background: Cardiovascular and metabolic comorbidities in chronic obstructive pulmonary disease (COPD) are associated with higher symptoms burden. Few center-based studies have evaluated the impact of these comorbidities on short-term pulmonary rehabilitation outcomes with contrasting results.
Research Question: This study aimed to determine whether cardiovascular diseases and metabolic comorbidities impacted long-term outcomes of a home-based PR program in COPD patients.
Study Design and methods: Data of 419 consecutive COPD patients addressed to our pulmonary rehabilitation program between January 2010 and June 2016 were retrospectively analyzed. Our program consisted of once-weekly supervised home sessions, including therapeutic education and self-management support, with unsupervised retraining exercises and physical activities the other days for 8 weeks. Exercise capacity (6-min stepper test [6MST]), quality of life (visual simplified respiratory questionnaire), and anxiety and depression (hospital anxiety and depression scale) were assessed respectively, before (M0) and at the end (M2) of the pulmonary rehabilitation program, and at 6 (M8) and 12 months (M14) after its achievement.
Results: Patients (mean age 64.1± 11.2 years, 67% males, mean forced expiratory volume in one second (FEV1) 39.2± 17.0% predicted) were classified as having cardiovascular comorbidities (n=195), only metabolic disorders (n=122) or none of these comorbidities (n=102). After adjustment, all outcomes appeared similar between groups at baseline and improved after pulmonary rehabilitation with a greater effect at M14 for patients with only metabolic disorders on anxiety and depression score (− 5.0± 0.7 vs − 2.9± 0.8 and − 2.6± 0.6, p=0.021). Quality of life and exercise capacity improvements were not significantly different between the three groups at M2 and M14.
Conclusion: Cardiovascular and metabolic comorbidities do not preclude COPD patients from obtaining clinically meaningful improvements in exercise capacity, quality of life and anxiety-depression up to 1 year after a home-based pulmonary rehabilitation.
Keywords: anxiety, exercise tolerance, quality of life, comorbidities, home based pulmonary rehabilitation, COPD
Introduction
Chronic obstructive pulmonary disease (COPD) is a common disease characterized by persistent respiratory symptoms and airflow limitation due to airway and/or alveolar abnormalities. It is usually caused by significant exposure to noxious particles among which tobacco smoking is the main factor in France.1 Despite being preventable and treatable, COPD prevalence is still increasing and represents a major source of morbidity, mortality and a significant economic burden.2 Progression of the disease is associated with increased respiratory disability and health-related quality of life (HRQoL) alteration.
Pulmonary rehabilitation (PR) is an effective and comprehensive treatment for COPD patients combining retraining exercises, therapeutic education, nutritional and psychological supports but remains underused.3 Therefore, new models have emerge last years to improve access to PR such as home-based PR programs, which are useful for patients living far from PR centers and were also shown interesting for limiting contact during the SARS-CoV2 epidemic.4 However, impact of comorbidities on PR outcomes, particularly with these new PR modalities, is not well known.
Cardiovascular diseases such as ischemic heart disease, arrhythmia, heart failure, peripheral arterial diseases and metabolic disorders such as arterial hypertension and diabetes mellitus are frequently associated with COPD.5 These associations may be related to common underlying molecular mechanisms, but also to common risk factors such as smoking and decreased physical activity.6,7 These comorbidities were reported to be associated with higher symptoms burden and lower HRQoL in COPD.8 Moreover, cardiovascular diseases are associated with prolonged hospital length of stay after acute exacerbation of COPD and with increased mortality.9,10 However, it is proven that cardiac rehabilitation is effective in improving exercise capacity and HRQoL in patients with cardiovascular diseases.11 Only a few studies have evaluated the impact of cardiovascular comorbidities on PR-related outcomes in COPD patients and reported contrasting results.12–16 Furthermore, all of these studies were center-based and none evaluated benefits up to a year after the end of the PR program.
The aim of our study was to determine whether established cardiovascular diseases and metabolic comorbidities impacted long-term effects of a home-based PR program on exercise capacity, HRQoL and anxiety-depression in COPD patients.
Methods
Patients
Data of all consecutive COPD patients addressed for the FormAction home-based PR program between January 2010 and June 2016 were prospectively collected in the computerized medical record CARE ITOU® and retrospectively analyzed. All patients were addressed by a respiratory physician who confirmed the diagnosis of COPD according to GOLD definition and checked for absence of PR contraindications, ie active lung cancer, unstable cardiovascular disease, significant cognitive disorders, uncontrolled psychiatric illness, neurological sequelae or major osteoarticular restrictions.17 The choice of home-based vs center-based PR was determined according to patients’ wishes and/or lack of PR center close to their home. Adverse events and reasons for withdrawals were recorded with a systematic assessment of their relationship to the program. The study protocol was conducted in accordance with the Declaration of Helsinki and approved by the Observational Research Protocol Evaluation Committee of the French Society of Respiratory Disease (CEPRO 2017–007). All participants signed a written informed consent prior to the start of the program which included their approval to use the collected data for research purposes and the computerized medical record declared to the National Commission for Informatics and Liberties.
Cardiovascular and Metabolic Comorbidities
Comorbidities were self-reported by patients and then completed and corrected from medical reports provided by the patient and their respiratory physician. Comorbidities were then registered in the computerized medical record when patients entered the PR program. Patients with a diagnosis of ischemic heart disease, chronic heart failure, cardiac arrhythmias, pulmonary hypertension or peripheral arterial disease were classified as having at least one established cardiovascular disease (Cardiovascular group). Patients without previous cardiovascular comorbidities but with at least one comorbidity used to diagnose a metabolic syndrome, ie hypertension, hypercholesterolemia, diabetes mellitus, or obesity (defined by a body mass index [BMI] ≥30 kg/m2) were classified as having metabolic comorbidities (Metabolic group). Patients having both metabolic and cardiovascular comorbidities were classified in the Cardiovascular group. Finally, patients who were not classified in these two groups were considered with no cardiovascular and metabolic comorbidities and considered as the Reference group. Underweight was defined by a BMI ≤ 21 kg/m2.18
Pulmonary Rehabilitation Program
Our home-based PR program was described in previous studies.19 Briefly, this 8-week program included exercise training and physical activities, therapeutic education, nutritional support and behavioral and motivational approaches. Patients were supervised in-person by a member of the PR team during a weekly 90-min session and encouraged to continue exercises the rest of the week in autonomy and after the end of the PR program. Patients started with individual endurance exercises on a cycle ergometer at the target heart rate in 10-min sequences, at least 5 days per week, with the goal of reaching 30–45 min per sequence in one or several sessions. After the end of the program, the PR team performed home-visits at 6 and 12 months to assess encountered difficulties, find solutions and strengthen patients and caregivers’ motivation.
Study Design and Measurements
Assessments were performed at baseline before the PR program (M0), immediately at the end of the program (M2), and at 6 and 12 months after its end (M8 and M14, respectively). Exercise capacity was assessed using the 6-min stepper test (6MST) that measures the number of steps performed in 6 min on a stepper with a minimal clinically significant difference (MCID) of 40 steps.20,21 Health-related quality of life (HRQoL) was assessed using the visual simplified respiratory questionnaire (VSRQ) ranging for 0 (worse) to 80 (better) with a MCID of 3.4 points.22 Finally, anxiety and depression were assessed using the hospital anxiety and depression scale (HAD) distinguishing overall score, and anxiety and depression sub-scores. These scores increase with anxiety and depression with a MCID of 1.5 points for each score and sub-scores.23
Statistical Analysis
Quantitative variables are expressed as means ±standard deviation (SD) and categorical variables are expressed as frequencies (percentage). Among patients who initiated PR, differences in baseline characteristics between patients evaluated and those not evaluated at 12 months after end of PR (due to death or loss to follow-up) were assessed by calculating the absolute standardized difference (ASD); an ASD >20% was interpreted as a meaningful difference. Comparisons in baseline characteristics between the three groups were performed using one-way analysis of variance (ANOVA) for quantitative variables or chi-squared tests for categorical variables. Evolution of outcomes (HRQoL, exercise capacity, anxiety, and depression) from baseline (M0) to M2, M8 and M14 were analyzed using linear mixed models for repeated measures (an unstructured covariance pattern model to account the correlation between repeated measures) by including time as fixed effect. Comparisons in evolution of outcomes from baseline (M0) to M2, M8 and M14 between the three groups were also performed using linear mixed models including groups, time, interaction time*groups, baseline outcome values and predetermined confounding factors (age, sex, BMI, FEV1, and long-term oxygen therapy (LTOT) status) as fixed effects;24 post hoc comparisons of 2-, 8- and 14-month changes were done using linear contrasts. Comparisons in evolution of outcomes between the three groups were also done after excluding underweight patients as a sensitivity analysis. Normality of residuals of linear mixed models were checked using quantile-quantile (Q-Q) plots. All statistical tests were done at the two-tailed α level of 0.05 without correction for multiple comparisons. Data were analyzed using SAS software version 9.4 (SAS Institute, Cary, NC, USA).
Results
Population Description
Four hundred and nineteen consecutive COPD patients were addressed to the home-based PR program, among which 413 started the program and 380, 333, and 303 were evaluated at M2, M8 and M14, respectively (Figure 1). None of them had any contraindication to PR and no incident related to the PR program was reported. The population included 67% men. The mean age was 64.1±11.2 years. Most patients had severe COPD (mean FEV1 39.2±17% predicted, 66.3% GOLD stages III and IV) and were ex-smokers (80.9%) with cumulative smoking estimated at 48±30 pack-years (Table 1). Only 23.6% did not receive LTOT, noninvasive ventilation (NIV) or continuous positive airway pressure (CPAP). The most prevalent reported comorbidities were hypertension (40.8%), obesity (30.7%), underweight (22.8%), hypercholesterolemia (22.4%), ischemic heart disease (22.2%) and diabetes (21.7%) (Tables 1 and 2). Other self-reported comorbidities are detailed in Supplementary Table 1. One hundred and twenty-two patients (29.1%) were classified as having metabolic comorbidities without an established cardiovascular disease (Metabolic group) and 102 patients (24.3%) as having no cardiovascular nor metabolic comorbidities (Reference group). Therefore, 195 patients (46.5%) were classified as having at least one established cardiovascular disease (Cardiovascular group). Altogether, 83% had at least three reported comorbidities. The 110 patients who initiated the program and were lost to follow-up during the 14 months were more likely to have an established cardiovascular comorbidity, to be underweight, to present a very severe airflow limitation and to require LTOT or NIV (Supplementary Table 2).
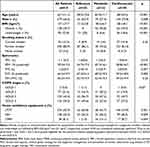 |
Table 1 Baseline Description of the Population |
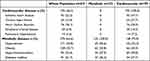 |
Table 2 Patients’ Reported Cardiovascular and Metabolic Comorbidities |
 |
Figure 1 Flowchart of the whole population. Abbreviation: PR, pulmonary rehabilitation. |
Baseline Assessment
At baseline, patients performed 309±9 steps during the 6MST and had an altered HRQoL reflected by a low VSRQ score (31.1±0.8) (Supplementary Table 3). They exhibited elevated anxiety and depression scores (9.7±0.2 and 8.0±0.2, respectively) with 52% and 34% of them showing anxiety and depression scores greater than or equal to 11, respectively. Patients from the Cardiovascular group were more often men (73.8%), were older (mean age 68.5±9.6 years) and more frequently treated with LTOT and NIV (Table 1). Patients from Metabolic and Cardiovascular groups had a higher BMI (30.5±6.7 and 28.1±8.1 kg/m2, respectively, vs 21.2±3.8 kg/m2 for the Reference group) and were more often treated with CPAP (13.1 and 8.7%, respectively, vs 1% for the Reference group). Proportion of GOLD stage IV COPD was higher in Reference group (45.6% vs 23.6% and 37.5% in Metabolic and Cardiovascular groups, respectively) while GOLD stages I and II COPD were more frequent in Metabolic group (29.2% vs 17.8% and 19.9% for Reference and Cardiovascular groups, respectively). At baseline, patients from Cardiovascular group performed significantly fewer steps on the 6MST (272±141 steps vs 343±161 and 339±164 for Reference and Metabolic groups, respectively), while VSRQ and HAD scores were similar between the three groups (Supplementary Table 4). Taking into account only patients evaluated at M2 and after adjustment to age, sex, BMI, FEV1 and LTOT status, the three groups were similar for all baseline assessments (Table 3).
 |
Table 3 Absolute Variations of Exercise Capacity, Quality of Life and Anxiety-depression for each Group of Patients |
Outcomes Improvement After PR
In the whole population, all outcomes significantly improved between baseline and the end of the program (M2), 6 months (M8) and 12 months after PR completion (M14) (Table 4). After adjustment on age, sex, BMI, FEV1, and LTOT status, changes in all outcomes remained significant for all three groups for all three assessments (M2, M8 and M14), except for the 6MST at M8 and M14 in Reference group (Table 5). The proportion of patients exceeding the MCID for at least one of the outcomes, ie HRQoL, anxiety-depression or exercise capacity, was 69.8%, 56.7%, and 50.7% at M2, M8 and M14, respectively (Figure 2). When comparing groups to each other, mean HAD global score was significantly more improved at M14 in patients from Metabolic group versus the two other groups and depression subscore at M14 between Metabolic and Cardiovascular groups (Table 3). There were no significant differences between groups for other time point and outcomes. Results were similar after exclusion of underweight patients (Supplementary Table 5).
 |
Table 4 Absolute Variations of Exercise Capacity, Quality of Life and Anxiety-depression for the Whole Population |
 |
Table 5 Comparisons to Baseline of Exercise Capacity, Quality of Life and Anxiety-depression Assessed at the End of the Rehabilitation Program and after 6 and 12 Months for each Group of Patients |
Discussion
This retrospective observational study evaluated the impact of cardiovascular and metabolic comorbidities on the outcomes of a home-based PR program in COPD patients over 1 year after the end of this program. COPD patients with metabolic comorbidities but no established cardiovascular disease exhibited a significant greater improvement in depression at 12 months after PR achievement compared to control group. No other outcome was significantly different between the three groups. To our knowledge, this is the first real-life study to evaluate impact of cardiovascular and metabolic comorbidities after 6 and 12 months of a home-based PR program.
Cardiovascular comorbidities are frequently associated with COPD and remain the most common causes of mortality in these patients.25 We confirm this strong association with only 24.3% of patients who had no cardiovascular disease nor cardiovascular risk-factors excluding smoking and by the observation that 81% of patients who died during the 14 month follow-up had at least one cardiovascular comorbidity. Moreover, at baseline, patients with established cardiovascular disease exhibited significant lower exercise capacity. Although in our study this group of patient was older than others, this is concordant with previous studies reporting decreased physical activity in COPD patients with concomitant cardiovascular disease, a diminished capacity partly mediated by deleterious cardiorespiratory interactions.26 Comprehensive care integrating all comorbidities is therefore essential to improve the prognosis of these patients.
We chose to group patients with established cardiovascular comorbidity regardless of metabolic comorbidity because only 24% of those patients did not have metabolic comorbidity and those cardiovascular comorbidity are associated with a significant exercise capacity limitation.27–29 The choice to categorize hypertension as a metabolic comorbidity and not as a cardiovascular comorbidity is questionable. However, definitions of metabolic syndrome consider hypertension as one of their diagnostic criteria and hypertension is clearly identified as a risk factor for adverse cardiovascular outcomes.30 In a cohort of healthy adults who underwent a cardiac health check-up, Kim et al reported that exercise capacity was more reduced, the level of coronary calcification more increased and the cardiac structure on echocardiography more altered when patients had more components of the metabolic syndrome including hypertension.31 This suggests that the impact of comorbidities defining the metabolic syndrome have a cumulative effect. Conversely these comorbidities are also improved and may be reversed to some extent by physical activity.32 Therefore, we chose to group these comorbidities including hypertension for their intermediate impact on exercise tolerance and their recovery potential.
Benefits of pulmonary rehabilitation for COPD patients are well described and our home-based PR program, as center-based programs, exhibit benefits on exercise capacity, quality of life and anxiety-depression, not only at the end of the program, but up to one year after its achievement in the whole population.19,33 Ninety percent of patients completed our home-based PR program. Compared to the British Thoracic Society objectives of achieving a 70% completion rate, this suggests that this modality would remove some of the obstacles to finalizing the PR program for some patients.34 Other effective PR models including telerehabilitation have emerged in recent years to improve access and uptake to PR and address issues related to the distance to rehabilitation centers or to constraints of the SARS-CoV2 epidemic.35 Cardiovascular comorbidities may be perceived as an obstacle to out-of-center PR, but our study demonstrates that home-based PR is feasible and effective for referred patients, provided that the prescriber first assesses the stability of these comorbidities.
Specific influence of cardiovascular and metabolic comorbidities on PR and results was evaluated by some studies immediately at the end of the PR program with contrasting effects. The association between having cardiovascular comorbidities and exhibiting a greater improvement of dyspnea after PR was not observed in all studies and only one retrospective study report an association between having cardiovascular comorbidities and exhibiting greater 6MWD improvements.12,14–16 In a retrospective study, Crisafulli et al reported a weaker improvement of SGRQ score in patients with cardiovascular comorbidities, but this negative association was not observed in their later prospective study nor in the Mesquita et al or Butler et al studies.13–15 Conversely, Tunsupon et al reported greater improvement of quality of life assessed with the chronic respiratory disease questionnaire in patients with cardiovascular diseases.12 None of these studies have evaluated the impact on anxiety-depression nor the persistence of benefits after the end of the PR. Considering metabolic comorbidities, to our knowledge no study reported an association between having a metabolic disorder and reporting a greater dyspnea improvement after PR.12,14–16 The impact of metabolic comorbidities on exercise capacity improvement after PR is more controversial. Thus, Walsh et al have reported a greater improvement associated with these metabolic comorbidities, as observed in our study, but there were no association in three other studies.13,15,16,36 Moreover, in two other studies, exercise capacity improvement was weaker in patients with metabolic comorbidities.12,14 Finally, as observed in our study, none reported an association between having metabolic comorbidities and exhibiting greater quality of life improvement. Altogether, these discrepancies may suggest that comorbidities did not impact PR outcomes per se except when they participate in the symptomatology and the impact of the disease. A more precise phenotyping of the mechanisms involved in patient’s symptoms may help to clarify condition when patients will benefit the most from a PR.
Our study is limited by its design as we included only patients addressed to our home-based PR program by their physicians who may have made the choice to address their patients to our home-based program based on criteria unknown to us. As our study included only patients managed in our home-based PR program, our results may not be extrapolated to a center-based program despite the fact that studies have reported that these two modalities could produce similar results and that characteristics of patients choosing one or the other of these modalities would not differ.4,37 As comorbidities were self-reported by patients, we cannot exclude that some comorbidities were misdiagnosed. While underdiagnosis of cardiovascular diseases was shown to be unlikely, overestimation is possible as hypertension or hypercholesterolemia underdiagnosis.38,39 Therefore, there is still a risk of misclassifying patients despite we systematically corrected self-reported comorbidities from medical reports provided by patients. Moreover, due to the retrospective design of our study, some information was not available including precise dyspnea evaluation, exacerbations rate, detailed evaluation of nutritional and muscular status, emphysema severity, distention level, and quantification of physical activity after PR discharge. A significant proportion of underweight patients were present in the reference group and their characteristics have similarities with the cachectic cluster described by Vanfleteren et al, a phenotype associated with poorer HRQoL, more frequent exacerbations and higher mortality.40 However, the sensitivity analysis performed after exclusion of these patients showed similar results to main analysis performed with adjustment for BMI demonstrating the modest impact of this heterogeneity in weight profile.
Conclusion
Stable cardiovascular and metabolic comorbidities are frequently associated with COPD and do not limit short- and long-term improvement of exercise capacity, quality of life and anxiety-depression after a home-based pulmonary rehabilitation. Whether specific personalization of the PR program is required to improve benefits for all patients according to their comorbidities remains to be determined.
Abbreviation
6MST, 6-min stepper test; 6MWD, distance in the 6-min walking test; BMI, body mass index; COPD, chronic obstructive pulmonary disease; CPAP, continuous positive airway pressure; FEV1, forced expiratory volume in one second; FVC, forced vital capacity; GOLD, global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease; HAD, hospital anxiety and depression scale; HRQoL, health-related quality of life; LTOT, long-term oxygen therapy; MCID, minimal clinically significant difference; NIV, noninvasive ventilation; PR, pulmonary rehabilitation; SGRQ, St George’s respiratory questionnaire; VSRQ, visual simplified respiratory questionnaire.
Acknowledgments
The authors would like to thank the rehabilitation team who managed the patients: G. Tywoniuk, S. Duriez, M Grosbois, V Opsomer, F. Urbain, V. Wauquier, and M. Lambinet. The authors would also like to thank Adair, Aeris Santé, Bastide, France Oxygène, Homeperf, LVL, Medopale, NorOx, Santélys, SOS Oxygène, Sysmed, VitalAire, and ARS Hauts-de-France for their support of the home-based PR program. They also thank Emeline Cailliau and Julien Labreuche who performed the new statistical analyses in response to reviewers’ comments.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
JMG received financial support from Adair, Aeris Santé, Bastide, Elivie, France Oxygène, Homeperf, LVL, Medopale, NorOx, Santélys, Santéo, SOS Oxygène, Sysmed, VentilHome, VitalAire, and ARS Hauts-de-France for the home-based PR program. JMG reports personal fees and nonfinancial support unrelated to the submitted work from AstraZeneca, Boehringer Ingelheim, Chiesi, CSL Behring, GlaxoSmithKlein, Novartis, Vitalaire, and Roche, unrelated to the submitted work. AD reports nonfinancial support from ALK-Abello, Amgen, AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKlein, LEO Pharma, Menarini, MSD, Novartis, Novo Nordisk, Pfizer, Resmed and Vitalaire, unrelated to the submitted work. AP reports no conflicts of interest related to the submitted work. NB reports personal fees from AstraZeneca, and nonfinancial support from AstraZeneca, Boehringer Ingelheim, GlaxoSmithKlein, Novartis, Santelys association, SOS Oxygène and TEVA, unrelated to the submitted work. TP reports grants from AstraZeneca, personal fees from AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKlein and Novartis, and congress support from AstraZeneca, GlaxoSmithKlein, Novartis and Chiesi, unrelated to the submitted work. BW reports personal fees from AstraZeneca, Boehringer Ingelheim, GlaxoSmithKlein, Roche and TEVA, and nonfinancial support from ALK-Abello, Aptalis pharma, AstraZeneca, Boehringer Ingelheim, Chiesi, Chugai pharma, France Oxygène, Kyowa Kirin, GlaxoSmithKlein, Mayoli, Mundipharma, Mylan, Novartis, Pfizer, Preciphar, Roche, SEFAM, SOS Oxygène, SYSMED, Vertex and Vitalaire, unrelated to the submitted work. CC reports grants from AstraZeneca and Santelys, personal fees from ALK-Abello, AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKlein, Novartis, Sanofi-Regeneron and TEVA, and congress support from ALK-Abello, AstraZeneca, GlaxoSmithKlein, Novartis, Pierre Fabre, Pfizer, Roche and TEVA, unrelated to the submitted work. OLR reports personal fees from AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKline and Novartis, and nonfinancial supports from AstraZeneca, Boehringer Ingelheim, Chiesi, Correvio, GlaxoSmithKlein, Mayoli, MSD, Mylan, Novartis, Pfizer, PulmonX, Santelys Association, Vertex, Vitalaire and Zambon, unrelated to the submitted work. OLR is the principal investigator in studies for Vertex and CSL Behring.
References
1. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease 2022 report. Available from: https://goldcopd.org/2022-gold-reports-2/#.
2. Khakban A, Sin DD, FitzGerald JM, et al. The projected epidemic of chronic obstructive pulmonary disease hospitalizations over the next 15 years. A population-based perspective. Am J Respir Crit Care Med. 2016;195(3):287–291. doi:10.1164/rccm.201606-1162PP
3. Holland AE, Cox NS, Houchen-Wolloff L, et al. Defining modern pulmonary rehabilitation. an official American thoracic society workshop report. Ann Am Thorac Soc. 2021;18(5):e12–e29. doi:10.1513/AnnalsATS.202102-146ST
4. Stafinski T, Nagase FI, Avdagovska M, Stickland MK, Menon D. Effectiveness of home-based pulmonary rehabilitation programs for patients with chronic obstructive pulmonary disease (COPD): systematic review. BMC Health Serv Res. 2022;22(1):557. doi:10.1186/s12913-022-07779-9
5. Gonçalves JMF, Bello MÁG, Martínez MDM, et al. The COPD comorbidome in the light of the degree of dyspnea and risk of exacerbation. J Chron Obstruct Pulmon Dis. 2019;16(1):104–107. doi:10.1080/15412555.2019.1592144
6. Faner R, Agustí A. Network analysis: a way forward for understanding COPD multimorbidity. Eur Respir J. 2015;46(3):591–592. doi:10.1183/09031936.00054815
7. Van Remoortel H, Hornikx M, Langer D, et al. Risk factors and comorbidities in the preclinical stages of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2014;189(1):30–38. doi:10.1164/rccm.201307-1240OC
8. Giezeman M, Hasselgren M, Lisspers K, et al. Influence of comorbid heart disease on dyspnea and health status in patients with COPD – a cohort study. Int J Chron Obstruct Pulmon Dis. 2018;13:3857–3865. doi:10.2147/COPD.S175641
9. Laforest L, Roche N, Devouassoux G, et al. Frequency of comorbidities in chronic obstructive pulmonary disease, and impact on all-cause mortality: a population-based cohort study. Respir Med. 2016;117:33–39. doi:10.1016/j.rmed.2016.05.019
10. Wang Y, Stavem K, Dahl FA, Humerfelt S, Haugen T. Factors associated with a prolonged length of stay after acute exacerbation of chronic obstructive pulmonary disease (AECOPD). Int J Chron Obstruct Pulmon Dis. 2014;9:99–105. doi:10.2147/COPD.S51467
11. Palmer K, Bowles KA, Paton M, Jepson M, Lane R. Chronic heart failure and exercise rehabilitation: a systematic review and meta-analysis. Arch Phys Med Rehabil. 2018;99(12):2570–2582. doi:10.1016/j.apmr.2018.03.015
12. Tunsupon P, Lal A, Abo Khamis M, Mador MJ. Comorbidities in patients with chronic obstructive pulmonary disease and pulmonary rehabilitation outcomes. J Cardiopulm Rehabil Prev. 2017;37(4):283–289. doi:10.1097/HCR.0000000000000236
13. Mesquita R, Vanfleteren LEGW, Franssen FME, et al. Objectively identified comorbidities in COPD: impact on pulmonary rehabilitation outcomes. Eur Respir J. 2015;46(2):545–548. doi:10.1183/09031936.00026215
14. Crisafulli E, Costi S, Luppi F, et al. Role of comorbidities in a cohort of patients with COPD undergoing pulmonary rehabilitation. Thorax. 2008;63(6):487–492. doi:10.1136/thx.2007.086371
15. Crisafulli E, Gorgone P, Vagaggini B, et al. Efficacy of standard rehabilitation in COPD outpatients with comorbidities. Eur Respir J. 2010;36(5):1042–1048. doi:10.1183/09031936.00203809
16. Butler SJ, Li LSK, Ellerton L, Gershon AS, Goldstein RS, Brooks D. Prevalence of comorbidities and impact on pulmonary rehabilitation outcomes. ERJ Open Res. 2019;5(4):00264–02019. doi:10.1183/23120541.00264-2019
17. Vogelmeier CF, Criner GJ, Martinez FJ, et al. Global strategy for the diagnosis, management, and prevention of chronic obstructive lung disease 2017 report: GOLD executive summary. Eur Respir J. 2017;49(3):1700214. doi:10.1183/13993003.00214-2017
18. Celli BR, Cote CG, Marin JM, et al. The body-mass index, airflow obstruction, dyspnea, and exercise capacity index in chronic obstructive pulmonary disease. N Engl J Med. 2004;350(10):1005–1012. doi:10.1056/NEJMoa021322
19. Grosbois JM, Gicquello A, Langlois C, et al. Long-term evaluation of home-based pulmonary rehabilitation in patients with COPD. Int J Chron Obstruct Pulmon Dis. 2015;10:2037–2044. doi:10.2147/COPD.S90534
20. Grosbois JM, Riquier C, Chehere B, et al. Six-minute stepper test: a valid clinical exercise tolerance test for COPD patients. Int J Chron Obstruct Pulmon Dis. 2016;11:657–663. doi:10.2147/COPD.S98635
21. Pichon R, Couturaud F, Mialon P, et al. Responsiveness and minimally important difference of the 6-minute stepper test in patients with chronic obstructive pulmonary disease. Respiration. 2016;91(5):367–373. doi:10.1159/000446517
22. Perez T, Arnould B, Grosbois JM, et al. Validity, reliability, and responsiveness of a new short Visual Simplified Respiratory Questionnaire (VSRQ) for health-related quality of life assessment in chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2009;4:9–18.
23. Puhan MA, Frey M, Büchi S, Schünemann HJ. The minimal important difference of the Hospital Anxiety and Depression Scale in patients with chronic obstructive pulmonary disease. Health Qual Life Outcomes. 2008;6:46. doi:10.1186/1477-7525-6-46
24. Lederer DJ, Bell SC, Branson RD, et al. Control of confounding and reporting of results in causal inference studies. Guidance for authors from editors of respiratory, sleep, and critical care journals. Ann ATS. 2019;16(1):22–28. doi:10.1513/AnnalsATS.201808-564PS
25. Agarwal S, Rokadia H, Senn T, Menon V. Burden of cardiovascular disease in chronic obstructive pulmonary disease. Am J Prev Med. 2014;47(2):105–114. doi:10.1016/j.amepre.2014.03.014
26. Mantoani LC, Dell’Era S, MacNee W, Rabinovich RA. Physical activity in patients with COPD: the impact of comorbidities. Expert Rev Respir Med. 2017;11(9):685–698. doi:10.1080/17476348.2017.1354699
27. Baloch ZQ, Abbas SA, Marone L, Ali A. Cardiopulmonary exercise testing limitation in peripheral arterial disease. Ann Vasc Surg. 2018;52:108–115. doi:10.1016/j.avsg.2018.03.014
28. Zweerink A, van der Lingen ALCJ, Handoko ML, van Rossum AC, Allaart CP. Chronotropic incompetence in chronic heart failure. Circ Heart Fail. 2018;11(8):e004969. doi:10.1161/CIRCHEARTFAILURE.118.004969
29. Paolillo S, Farina S, Bussotti M, et al. Exercise testing in the clinical management of patients affected by pulmonary arterial hypertension. Eur J Prev Cardiol. 2012;19(5):960–971. doi:10.1177/1741826711426635
30. Alberti KGMM, Eckel RH, Grundy SM, et al. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120(16):1640–1645. doi:10.1161/CIRCULATIONAHA.109.192644
31. Kim HJ, Kim JH, Joo MC. Association of exercise capacity, cardiac function, and coronary artery calcification with components for metabolic syndrome. Biomed Res Int. 2018;2018:4619867. doi:10.1155/2018/4619867
32. Thompson PD, Buchner D, Piña IL, et al. Exercise and physical activity in the prevention and treatment of atherosclerotic cardiovascular disease. Circulation. 2003;107(24):3109–3116. doi:10.1161/01.CIR.0000075572.40158.77
33. Grosbois JM, Le Rouzic O, Monge E, Bart F, Wallaert B. Comparison of home-based and outpatient, hospital-based, pulmonary rehabilitation in patients with chronic respiratory diseases. Rev Pneumol Clin. 2013;69(1):10–17. doi:10.1016/j.pneumo.2012.11.003
34. RCP London. Pulmonary rehabilitation: an exercise in improvement – combined clinical and organisational audit 2017; 2018. Available from: https://www.rcplondon.ac.uk/projects/outputs/pulmonary-rehabilitation-exercise-improvement-combined-clinical-and-organisational.
35. Cox NS, Dal Corso S, Hansen H, et al. Telerehabilitation for chronic respiratory disease. Cochrane Database Syst Rev. 2021;2021(1):CD013040. doi:10.1002/14651858.CD013040.pub2
36. Walsh JR, McKeough ZJ, Morris NR, et al. Metabolic disease and participant age are independent predictors of response to pulmonary rehabilitation. J Cardiopulm Rehabil Prev. 2013;33(4):249–256. doi:10.1097/HCR.0b013e31829501b7
37. Nolan CM, Kaliaraju D, Jones SE, et al. Home versus outpatient pulmonary rehabilitation in COPD: a propensity-matched cohort study. Thorax. 2019;74(10):996–998. doi:10.1136/thoraxjnl-2018-212765
38. Barr ELM, Tonkin AM, Welborn TA, Shaw JE. Validity of self-reported cardiovascular disease events in comparison to medical record adjudication and a statewide hospital morbidity database: the AusDiab study. Intern Med J. 2009;39(1):49–53. doi:10.1111/j.1445-5994.2008.01864.x
39. Burvill AJ, Murray K, Knuiman MW, Hung J. Comparing self-reported and measured hypertension and hypercholesterolaemia at standard and more stringent diagnostic thresholds: the cross-sectional 2010–2015 Busselton Healthy Ageing study. Clin Hypertens. 2022;28(1):16. doi:10.1186/s40885-022-00199-1
40. Vanfleteren LEGW, Spruit MA, Groenen M, et al. Clusters of comorbidities based on validated objective measurements and systemic inflammation in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2013;187(7):728–735. doi:10.1164/rccm.201209-1665OC
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

