Back to Journals » International Journal of General Medicine » Volume 16
Correlation Between IL-8, C-Reactive Proteins (CRP) and Neutrophil to Lymphocyte Ratio (NLR) as Predictor of Mortality in COVID-19 Patients with Diabetes Mellitus Comorbidity
Authors Iskandar A , Mayashinta DK , Robert R, Samsu N , Endharti AT , Widjajanto E
Received 11 March 2023
Accepted for publication 16 May 2023
Published 8 June 2023 Volume 2023:16 Pages 2349—2354
DOI https://doi.org/10.2147/IJGM.S412070
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Agustin Iskandar,1– 3 Dearikha K Mayashinta,2,3 Robert Robert,3 Nur Samsu,4 Agustina Tri Endharti,2 Edy Widjajanto3
1Doctoral Program in Medical Science, Faculty of Medicine, Universitas Brawijaya/Saiful Anwar General Hospital, Malang, Indonesia; 2Department of Parasitology, Faculty of Medicine, Universitas Brawijaya/Saiful Anwar General Hospital, Malang, Indonesia; 3Department of Clinical Pathology, Faculty of Medicine, Universitas Brawijaya/Saiful Anwar General Hospital, Malang, Indonesia; 4Department of Internal Medicine, Faculty of Medicine, Universitas Brawijaya/ Saiful Anwar General Hospital, Malang, Indonesia
Correspondence: Agustin Iskandar, Faculty of Medicine, Universitas Brawijaya/Saiful Anwar General Hospital, Malang, Indonesia, Email [email protected]
Background: COVID-19 is caused by SARS-CoV-2 and has a wide range of symptoms. While Diabetes Mellitus (DM) is a common comorbidity in COVID-19 patients, it is the main comorbidity in non-surviving COVID-19 patients. Interleukin-8 (IL-8) is a cytokine that has been correlated with severity and mortality in COVID-19 patients, but its role in COVID-19 patients with DM comorbidity and its relationship with NLR and CRP as markers of inflammation are not yet fully understood.
Objective: To investigate the correlation between IL-8, NLR, and CRP in COVID-19 patients with DM comorbidity.
Methods: A cross-sectional study was conducted at the Integrated Infectious Disease Installation of Dr. Saiful Anwar Malang Hospital from June to November 2021 using consecutive sampling. IL-8 was measured using the ELISA method with Legendmax® Human IL-8. NLR was measured using flow cytometry, while CRP was measured using the immunoturbidimetric method with Cobas C6000®. Patient outcomes were obtained from medical records.
Results: A total of 124 research subjects participated in the study. IL-8 and CRP levels were significantly higher (p < 0.05) in COVID-19 patients with DM comorbidity, and were also significantly higher (p < 0.05) in non-surviving COVID-19 patients. Overall, there was a positive correlation between IL-8 and CRP (r = 0.58, p < 0.05). There was also a positive correlation between IL-8 (r = 0.58; p < 0.05), NLR (r = 0.45, p < 0.05), CRP (r = 0.54, p < 0.05) and mortality in COVID-19 patients with DM comorbidity. The presence of DM comorbidity increased IL-8 levels and aggravated inflammation in COVID-19 patients, thereby increasing the risk of mortality.
Conclusion: IL-8, CRP and NLR levels were higher in non-surviving COVID-19 patients with DM comorbidity, indicating that they could serve as good predictors of poor outcomes in this patient population.
Keywords: interleukin-8, CRP, NLR, COVID-19
Background
COVID-19 has been a significant challenge for people with diabetes mellitus (DM), as they are at higher risk of severe illness, hospitalization, and death. Research has shown that DM is the second most common comorbidity in COVID-19 patients, and it is the main comorbidity in non-survivor COVID-19 patients.1
The co-occurrence of COVID-19 and DM is a significant health issue in Indonesia, as both conditions have a high prevalence in the population. According to data from the Indonesian Ministry of Health, as of January 2023, there were over 6.5 million confirmed COVID-19 cases and Case Fatality Rate (CFR) of 3.9%. Indonesia is ranked at eight places of the country with the most cases of COVID-19 in Asia. In addition, DM is also highly prevalent in this country, affecting approximately 10% of the adult population.1,2
Studies have shown that COVID-19 patients with DM are at higher risk of severe illness, hospitalization, and death. In Indonesia, a study conducted in Jakarta found that among COVID-19 patients, those with DM had a higher risk of severe illness and were more likely to require hospitalization compared to those without DM. The study also found that the presence of DM was associated with a higher risk of mortality among COVID-19 patients.3–5
Diabetes, and complications that accompany them, can increase the risk of morbidity and mortality, due to decreased immune function, endothelial and alveolar dysfunction, hyperglycemia and also hypercoagulable state.3 In COVID-19 patients with diabetes, there are also reports of more severe pneumonia, increased levels of enzymes related to tissue damage, uncontrolled inflammation, and hypercoagulable conditions associated with abnormal glucose metabolism. These factors can contribute to a higher risk of morbidity and mortality in COVID-19 patients with diabetes. Recent studies reported that COVID-19 patients with diabetes comorbidity have been found to be three times more likely to require ICU admissions compared to non-diabetes patients.6–9 It is crucial to develop biomarkers that could manage diabetes effectively in COVID-19 patients to minimize the risk of severe illness and to prevent complications that can worsen outcomes. Development of biomarkers in COVID-19 patients with DM could help predict mortality and identify high-risk patients who may benefit from early intervention. These biomarkers could also aid in monitoring disease progression and response to treatment.
Several biomarkers related to severity of COVID-19 have been reported, including NLR, CRP and IL-8. Interleukin-8, also known as CXCL8, is a pro-inflammatory chemokine that recruits neutrophils to the site of infection. The increased production of IL-8 is associated with increased infiltration of neutrophils in the lung tissue, which contributes to the development of acute respiratory distress syndrome (ARDS) in severe COVID-19 cases. In individuals with DM, the levels of IL-8 may be higher compared to those without DM due to impaired immune function and chronic inflammation associated with diabetes. Therefore, IL-8 may be a useful biomarker for predicting disease severity in COVID-19 patients with DM.10
NLR, which is the ratio of neutrophils to lymphocytes in the blood, is another biomarker that is associated with disease severity in COVID-19. An increased NLR has been reported in severe COVID-19 cases, indicating a higher degree of inflammation and a more severe immune response. In individuals with DM, the levels of NLR may be higher due to the underlying chronic inflammation associated with diabetes.11 Therefore, NLR may also be a useful biomarker for predicting disease severity in COVID-19 patients with DM.
CRP, a protein produced by the liver in response to inflammation, is another biomarker that is elevated in COVID-19 patients. Elevated CRP levels have been associated with increased mortality in COVID-19 patients. In individuals with DM, CRP levels may be higher due to underlying chronic inflammation associated with diabetes.10,11 Overall, IL-8, NLR, and CRP are important biomarkers for predicting disease severity and mortality in COVID-19 patients with DM. Further research is needed to determine the optimal cut-off values for these biomarkers in this population and to explore potential therapeutic strategies targeting these biomarkers to improve outcomes in COVID-19 patients with DM comorbidity.
Methods
Study Design and Data Collection
This is a cross-sectional study conducted at Dr. Saiful Anwar Hospital, a tertiary hospital in Malang, from June to November 2021. One hundred and twenty-four subjects in the study who were diagnosed as confirmed COVID-19, proven by a Reverse-Transcriptase–Polymerase-Chain-Reaction (RT-PCR) method. The inclusion criteria for subjects in this research are: patients who have been confirmed to have COVID-19 through RT-PCR testing of nasopharyngeal or oropharyngeal swabs, aged 17 years or older and have experienced symptom onset within 14 days prior to being diagnosed as a COVID-19 patient. Meanwhile, DM patients were diagnosed according to the Indonesian Association of Endocrinology, based on fasting and 2 hours post prandial blood glucose level, and/or HbA1C level. This study’s subject exclusion criteria are pregnant or breastfeeding women, having a coagulation disorder before being diagnosed as COVID-19, and co-morbidities such as cancer, hepatitis, or HIV/AIDS.
Cytokine levels of IL-8 were measured from serum subjects using the Enzyme-Linked Immunosorbent Assay (ELISA) examination procedure. The ELISA procedure was carried out according to the manual protocol of the Human IL-8 Bioassay Technology Laboratory (BT-Lab) ELISA kit (Cat. No. E0143Hu).
CRP and IL-8 were examined on the same day the patients confirmed positive for COVID-19.
NLR was examined using automatic flow cytometry analyzer Sysmex XN-1000®, while CRP was carried out by using a Nanopia CRP kit (Sekisui Medical, Japan) using an automatic chemistry analyzer Cobas 6000®. An antigen-antibody reaction occurs between CRP in heparin serum or plasma samples and latex particles which have been coated with mouse anti-CRP in glycine buffer. This reaction will form an aggregate of latex particles that are measured turbidimetrically.
Ethical Clearance
Ethical Clearance of this study was approved by ethics committee of Saiful Anwar General Hospital (No. 400/161/K.3/102.7/2022). All of the patients participating in this study provided informed consent that has been in accordance with the Declaration of Helsinki.
Statistical Analysis
Statistical analysis was carried out using the SPSS 25.0 (IBM Inc., USA). Because the distribution of the data is abnormal, the results are presented in the form of the median (min:max), while difference test was performed by Mann–Whitney test.
Results
During the study period, there were 124 research subjects, consisting of 60 subjects with comorbid DM and 64 subjects without comorbid DM. Table 1 shows the laboratory parameters of COVID-19 patients. There were no significant differences in the level of Hb, leukocytes, platelets, NLR and IL-8 between DM and non-DM COVID-19 patients, but there was a significant difference (p < 0.05) in Random Blood Glucose (RBG) and CRP between DM and non-DM COVID-19 patients. COVID-19 patients with comorbid DM were found to have higher RBG and CRP compared to patients without comorbid DM.
 |
Table 1 Laboratory Parameters Between DM and Non-DM COVID-19 Patients |
Table 2 shows the laboratory parameters of COVID-19 patients with DM comorbidity based on outcome. In the Mann–Whitney statistical test, there were no significant differences in Hb, platelet, and RBG levels between survivor and non-survivor patients, but there were significant differences (p < 0.05) in the leukocyte count, NLR, CRP, and IL-8 between DM and non-DM COVID-19 patients. Non survivor patients had higher leukocyte counts, NLRs, CRP and IL-8 levels compared to survivors.
 |
Table 2 Laboratory Parameters in COVID-19 Patients with DM Comorbidity Based on Mortality |
Table 3 shows the Pearson correlation of IL-8, NLR and CRP with mortality in all COVID-19 patients, compared to only COVID-19 patients with DM comorbidity. The result showed significant correlation between both IL-8, CRP and NLR with mortality, either in COVID-19 patients or COVID-19 patients with DM comorbidity. The result also showed that DM have moderate correlation with mortality. According to correlation analysis, among these three biomarkers, CRP has the best performance in determining mortality compared to IL-8 and CRP.
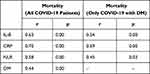 |
Table 3 The Result of Pearson Correlation Between IL-8, NLR and CRP with Mortality |
Discussion
The pathogenesis of SARS-CoV-2 infection is classified into two phases: the early and late phases. During the initial phase of COVID-19, viral replication occurs, resulting in direct virus-mediated tissue damage. In the later phase, infected host cells trigger an immune response by recruiting T lymphocytes, monocytes, and neutrophils that release cytokines, such as Tumor Necrosis Factor- (TNF-α), Granulocyte-Macrophage Colony-Stimulating factor (GM-CSF), Interleukin-1 (IL-1), Interleukin-6 (IL-6), IL-1β, IL-8, IL-12, and interferon (IFN)-γ. In severe COVID-19 patients, the immune system can become over-activated, resulting in a “cytokine storm”. This is characterized by the excessive release of cytokines into the circulation, causing a local and systemic inflammatory response. Numerous studies have confirmed an increase in various inflammatory cytokines in patients with severe COVID-19 who are admitted to the intensive care unit, providing evidence for a cytokine storm.12
The study’s results align with Harbuwono et al’s findings, demonstrating that COVID-19 patients with comorbid DM had a considerably higher mortality rate (21.28%) compared to non-DM COVID-19 patients (2.77%). Additionally, the study’s findings are consistent with Nurshad Ali’s meta-analysis, which revealed a significant increase in CRP in COVID-19 patients compared to controls, with increases ranging from 20 to 50 mg/L. Patients with severe COVID-19 (86%) had elevated CRP more frequently than those with mild and moderate COVID-19, and the increase was significantly higher than in mild and moderate COVID-19 patients. Elevated CRP levels are a common marker of inflammation and have been linked to worse outcomes in COVID-19 patients, including higher mortality rates. Therefore, monitoring CRP levels in COVID-19 patients with comorbid DM could be essential to identifying those at increased risk of mortality.7,9
The findings of this study are in line with the findings of Li et al, who found that there was an increase in IL-8 in severe COVID-19 patients. Interleukin-8 acts as an activation factor for neutrophils, and neutrophils are a major source of chemokines and cytokines. In patients with severe COVID-19, increased neutrophil numbers and neutrophil-to-lymphocyte ratio (NLR) are associated with higher disease severity and poorer clinical outcomes. Interleukin-8 has also been found to be a prognostic factor in in-hospital death in patients with severe COVID-19.13
COVID-19 patients with comorbid DM are also susceptible to systemic hyperinflammation, which is an uncontrolled systemic inflammatory condition caused by increased cytokines and results in multiple organ failure. The condition of systemic hyperinflammation in one of them is characterized by an increase in IL-8.14 CRP was also found to be elevated in COVID-19 patients with comorbid DM. This occurs because of the inflammatory reaction and tissue damage that occurs, and the increase in CRP is closely related to the severity of the DM condition that accompanies COVID-19 patients.15 These two things are related, where Xiao et al found that an increase in IL-8 in COVID-19 patients was positively correlated with an increase in CRP.16 Both increased of IL-8 and CRP were associated with poorer clinical outcomes and increased mortality compared to COVID-19 patients with lower IL-8 and/or CRP.13
Several studies have investigated the correlation between NLR (neutrophil to lymphocyte ratio), CRP, IL-8, and mortality in COVID-19 patients with DM comorbidity. One study found that higher NLR values were significantly associated with increased mortality in COVID-19 patients with DM, aligning with the study, and showed that NLR was also higher in COVID-19 patients with DM, and also higher in non-survivor COVID-19 patients with DM. NLR also has a moderate correlation with mortality, even though this biomarker has lowest correlation compared to IL-8 and CRP. Additionally, elevated levels of CRP and IL-8 were found to be predictive of mortality in these patients. Another study found that higher levels of IL-8 were associated with increased mortality risk in COVID-19 patients with DM.15,16
Overall, these studies suggest that monitoring NLR, CRP, and IL-8 levels could be useful in predicting mortality risk in COVID-19 patients with DM comorbidity. However, further research is needed to confirm these findings and determine the optimal cutoff values for these biomarkers in predicting mortality risk in this patient population. Interleukin-8 can also be used as a biomarker that should be examined as an early warning marker in COVID-19 patients, especially in moderate to severe COVID-19 patients. This is based on the fact that IL-8 is more able to show progression of COVID-19 disease in patients with severe degrees. The use of IL-8 combined with IL-6 can be used as a biomarker of the severity of COVID-19, especially in COVID-19 patients with DM comorbidity.
Conclusion
Based on the findings, we can conclude that IL-8, NLR, and CRP have a positive correlation with mortality and can be used as predictors of poor outcomes in COVID-19 patients with DM comorbidity. Non-survivor COVID-19 patients with DM comorbidity had higher levels of IL-8, NLR, and CRP compared to survivors. Of the three biomarkers, CRP demonstrated the best performance in predicting mortality when compared to IL-8 and NLR.
Ackowledgements
The authors would like to thank to the Dean of Medical Faculty of Universitas Brawijaya for giving partially funding for this research under Professor’s Grant contract no 2371/ 4/ UN10.F08/ PN/ 2022.
Disclosure
The authors report no conflicts of interest in this work.
References
1. WHO. COVID-19 weekly epidemiological update [WWW document]; 2021. Available from: https://covid19.who.int/.
2. Indonesian Ministry of Health. COVID-19 spread map; 2023. Available from: https://covid19.go.id/peta-sebaran.
3. Cascella M, Rajnik M, Cuomo A, Dulebohn SC, Di Napoli R. Features, Evaluation, and Treatment of Coronavirus (COVID-19). StatPearls; 2022.
4. Ilma U, Kun’ain A, Rahardjo SS, Tamtomo G. Meta-analysis: the effect of diabetes mellitus comorbidity on the risk of death in Covid-19 patients. Indones J Med. 2021;5(4):368–377.
5. Singh AK, Gupta R, Ghosh A, Misra A. Diabetes in COVID-19: prevalence, pathophysiology, prognosis and practical considerations. Diabetes Metab Syndr. 2020;14(4):303. doi:10.1016/j.dsx.2020.04.004
6. Du M, Lin YX, Yan WX, Tao LY, Liu M, Liu J. Prevalence and impact of diabetes in patients with COVID-19 in China. World J Diabetes. 2020;11(10):468. doi:10.4239/wjd.v11.i10.468
7. Harbuwono DS, Handayani DO, Wahyuningsih ES, et al. Impact of diabetes mellitus on COVID-19 clinical symptoms and mortality: Jakarta’s COVID-19 epidemiological registry. Prim Care Diabetes. 2022;16(1):65. doi:10.1016/j.pcd.2021.11.002
8. Stringer D, Braude P, Myint PK, et al. The role of C-reactive protein as a prognostic marker in COVID-19. Int J Epidemiol. 2021;50(2):420. doi:10.1093/ije/dyab012
9. Ali N. Elevated level of C‐reactive protein may be an early marker to predict risk for severity of COVID‐19. J Med Virol. 2020;92(11):2409. doi:10.1002/jmv.26097
10. Gonzalez-Aparicio M, Alfaro C. Influence of interleukin-8 and neutrophil extracellular trap (NET) formation in the tumor microenvironment: is there a pathogenic role? J Immunol Res. 2019;2019:1–7. doi:10.1155/2019/6252138
11. Ma A, Zhang L, Ye X, et al. High levels of circulating IL-8 and soluble IL-2R are associated with prolonged illness in patients with severe COVID-19. Front Immunol. 2021;12:12.
12. Ketut Wardika I, Putu G, Sikesa H. Pengukuran Interleukin-6 (IL-6), C-Reactive Protein (CRP) dan D-Dimer sebagai prediktor prognosis pada pasien COVID-19 gejala berat: sebuah tinjauan pustaka. Intisari Sains Medis. 2021;12(3):901–907. doi:10.15562/ism.v12i3.1158
13. Li H, Zhang J, Fang C, et al. The prognostic value of IL-8 for the death of severe or critical patients with COVID-19. Medicine. 2021;100(11):e23656. doi:10.1097/MD.0000000000023656
14. Gęca T, Wojtowicz K, Guzik P, Góra T. Increased risk of COVID-19 in patients with diabetes mellitus-current challenges in pathophysiology, treatment and prevention. Int J Environ Res Public Health. 2022;19(11):6555. doi:10.3390/ijerph19116555
15. Debi H, Itu ZT, Amin MT, Hussain F, Hossain MS. Association of serum C-reactive protein (CRP) and D-dimer concentration on the severity of COVID-19 cases with or without diabetes: a systematic review and meta-analysis. Expert Rev Endocrinol Metab. 2022;17(1):83–93. doi:10.1080/17446651.2022.2002146
16. Xiao LN, Ran X, Zhong YX, Li SS. Clinical value of blood markers to assess the severity of coronavirus disease 2019. BMC Infect Dis. 2021;21(1). doi:10.1186/s12879-021-06623-5
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
