Back to Journals » Clinical Ophthalmology » Volume 16
Visual and Refractive Efficacy of Panoptix Toric Intraocular Lens in a Clinical Setting
Authors Ackerman M, Lawless M, Levitz L , Bhatt U, Reich JA, Sutton G, Roberts TV, Tenen A, Kaur A, Hodge C
Received 23 September 2022
Accepted for publication 16 November 2022
Published 19 December 2022 Volume 2022:16 Pages 4227—4237
DOI https://doi.org/10.2147/OPTH.S390980
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Scott Fraser
Mariska Ackerman,1 Michael Lawless,2,3 Lewis Levitz,4 Uday Bhatt,4 Joseph A Reich,4 Gerard Sutton,2,3 Timothy V Roberts,2,3 Abi Tenen,4 Amanpreet Kaur,4 Chris Hodge2,3,5,6
1Sydney Medical School, The University of Sydney, Sydney, New South Wales, Australia; 2Vision Eye Institute, Sydney, New South Wales, Australia; 3Save Sight Institute, Faculty of Medicine and Health, The University of Sydney, Sydney, New South Wales, Australia; 4Vision Eye Institute, Melbourne, Victoria, Australia; 5Graduate School of Health, University of Technology Sydney, Sydney, New South Wales, Australia; 6Macquarie University, Sydney, Australia
Correspondence: Michael Lawless, Vision Eye Institute, Level 3 270 Victoria Avenue, Chatswood, Sydney, NSW, 2067, Australia, Tel +61 2 9424 9999, Fax +61 2 9410 3000, Email [email protected]
Purpose: Trifocal Intraocular Lenses (IOLs) were developed to provide patients with effective near, intermediate and distance vision, thus minimizing spectacle dependency. Residual astigmatism has previously been shown to impact unaided visual acuity across all distances; therefore, to optimise the expected outcomes, consideration of preoperative corneal astigmatism is essential. The purpose of this study was to provide a real-world, multi-site review of visual and refractive outcomes in eyes undergoing implantation with the Panoptix Trifocal toric IOL platform.
Patients and Methods: This study represents a two-fold approach. Patients who had previously undergone routine cataract removal and IOL insertion with the Panoptix Toric IOL were retrospectively analysed for routine efficacy and safety endpoints (“Retrospective Cohort”). Data was retrieved from the preoperative, surgical and postoperative visits (range 2– 6 weeks). A further subset of patients undergoing lens removal and bilateral Panoptix Toric IOL insertion were identified at surgery (“Qualitative Cohort”). These patients underwent additional testing inclusive of quality of vision questionnaire and bilateral defocus curve.
Results: A total of 466 eyes of 254 patients were included in the retrospective cohort. Between 91% and 98% of eyes, respectively, were within 0.50D and 1.00D of target. Mean absolute difference from Spherical Equivalent (SE) target was 0.22 ± 0.24Ds. Following surgery, 94% of eyes demonstrated a refractive astigmatism of 0.50D or less. Further, 61% eyes achieved uncorrected distance visual acuity (UDVA) of 20/20 or better, increasing to 94% achieving 20/32 or better. Seventy percent of eyes unilaterally achieved N5 unaided and 66.0% achieved N8 or better at intermediate. In the qualitative cohort, no patient described any symptom as significant or requested explant.
Conclusion: In a real-world setting, the PanOptix toric trifocal IOL continues to demonstrate refractive accuracy and good visual performance at all focal distances. This IOL also exhibited good quality of vision, with minimally bothersome visual disturbances or photic phenomena.
Keywords: cataract surgery, IOL, trifocal, lens extraction, visual acuity
Introduction
Cataract surgery is one of the most common surgical procedures.1 Cumulative experience and continued technological advances have succeeded in making cataract surgery a highly efficacious procedure with excellent refractive and visual outcomes.2 Accordingly, patient expectations have increased with many patients now expecting spectacle independence following surgery. Monofocal intraocular lenses (IOL) provide excellent visual quality at a fixed focal length, however patients routinely require reading prescription for near activities.3,4 Comparatively, the trifocal IOL was developed to provide patients with effective near, intermediate and distance vision, thus minimizing spectacle dependency.3,5
To achieve the best possible visual outcomes postoperatively regardless of IOL technology, correction of preoperative refractive error, including corneal astigmatism is essential. Corneal astigmatism is common in patients undergoing cataract surgery, and residual postoperative astigmatism will impact unaided visual acuity at all distances and lead to suboptimal outcomes.6,7 Postoperative refractive astigmatism is poorly tolerated when multi or trifocal IOLs are used. Astigmatism may be corrected through limbal relaxing incisions or with the aid of a toric IOL.8 With the introduction of toric trifocal IOLs, surgeons are now able to restore a patient’s vision at a range of focal distances, whilst also treating any pre-existing astigmatism.
The aim of our study was to retrospectively investigate the visual and refractive outcomes of the Alcon PanOptix toric trifocal lens in a large, multi-surgeon cohort. A secondary aim in a smaller targeted cohort, was to assess the range of unaided vision and the quality of vision using the toric IOL.
Materials and Methods
This study represents a two-fold approach. Data from patients who had previously undergone routine cataract removal and IOL insertion with the Panoptix Toric IOL (Alcon Labs, Ft. Worth TX, USA) were retrospectively collected and analysed for routine efficacy and safety endpoints (“Retrospective Cohort”). Data was retrieved from the preoperative, surgical and 1-month postoperative visits (range 2–6 weeks). A further subset of patients undergoing lens removal and bilateral Panoptix Toric IOL insertion were identified at surgery (“Qualitative Cohort”). Following consent, these patients underwent additional testing at 3 months post-surgery including quality of vision questionnaire and bilateral defocus assessment. Standard visual and refraction outcomes were also measured.
Inclusion criteria for both studies were the use of a Panoptix Trifocal IOL. Exclusion criteria were not applied to limit the cohort; however, each surgeon applied their own criteria to initially selecting the IOL as appropriate to the patient. The presence of mild-to-moderate ocular pathology, limiting potential postoperative corrected visual acuity, represented a general exclusion criterion for Panoptix IOL insertion. This may have excluded patients with prior refractive surgery, significant dry eye and concurrent ocular disease such as macular degeneration or glaucoma. The VERION system (Alcon, Fort Worth, TX) was used for eye registration and used to guide toric IOL alignment. Postoperatively, unaided near vision was routinely measured at 33cm across all sites; however, intermediate vision distance varied according to patient working distance (between 40cm to 80cm).
The prospective cohort study was assessed and approved by an external Human Research Ethics Committee (University of Sydney HREC No. 2019/517). The retrospective study was approved by the institutional Low and Negligible Risk committee. All patient information remained deidentified and the study complied with the Tenets of the Declaration of Helsinki.
Deidentified data was collected and stored in an Excel spreadsheet prior to analysis with SPSS (V24. IBM, Chicago IL, USA). Standard demographic variables were collated (mean, standard deviation and range) for visual and refractive parameters. Vector analysis as described by Thibos was used to understand the impact on the retrospective cohort.9
Results
Four hundred and sixty-six eyes of 254 consecutive patients undergoing Panoptix Toric IOL insertion were analysed. Overall, the mean age of patients was 67.9 ± 10.4 years (range 36 to 101 years) with 53.9% of the cohort female. The preoperative demographic data is listed in Table 1. With respect to astigmatic orientation, 73.5% of eyes exhibited “with the rule” astigmatism, 13.8% “against the rule” astigmatism and 12.7% considered “oblique”. The majority of eyes received a lower power toric IOL (TFNT2, 68.3%).
 |
Table 1 Preoperative Demographics |
The postoperative refractive outcomes of the retrospective cohort are listed in Table 2. Reflecting these values, 91% and 98% of eyes, respectively, were within 0.50D and 1.00D of the spherical equivalent (SE) target refraction (Figure 1). The mean arithmetic difference from SE target was 0.02 ± 0.32Ds (range −1.91 to 1.37Ds) and mean absolute difference from SE target was 0.22 ± 0.24Ds.
 |
Table 2 Postoperative Outcomes |
 |
Figure 1 Spherical equivalent refractive accuracy. |
Refractive astigmatism was recorded preoperatively and at 1-month post-surgery (Figure 2). Preoperatively, the majority of eyes (80%) had 1.00D or less of refractive astigmatism. Following surgery, 94% of all eyes demonstrated a refractive astigmatism of 0.50D or less (Figure 2). There was no statistically significant difference in terms of astigmatism direction and final magnitude of refractive cylinder. Vector analysis was undertaken and reported (Figure 3). The increased concentration of data points around the origin reflect an overall improvement following surgery. The difference between J0 Vectors between surgery was not clinically significant; however, the reduction in J45 values from pre- to post-surgery reached statistical significance (p = 0.043). Vector analysis values are listed in Table 3. Figure 4 identifies the visual acuity outcomes. Almost half (47%) of eyes in the retrospective cohort had preoperative corrected distance visual acuity of 20/20 highlighting a broader refractive group (Figure 4). Postoperatively, 61% of patients achieved an uncorrected distance visual acuity (UDVA) of 20/20 or better, increasing to 94% achieving 20/32 or better. Seventy percent of eyes unilaterally achieved N5 unaided at near whilst 66.0% achieved N8 or better at intermediate distance (Figure 5).
 |
Table 3 Mean Preoperative and Postoperative Astigmatic Outcomes |
 |
Figure 2 Refractive astigmatism pre- and post-surgery. |
 |
Figure 4 Cumulative visual acuity. Abbreviations: CDVA, corrected distance visual acuity; UDVA, uncorrected distance visual acuity. |
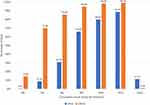 |
Figure 5 Cumulative intermediate and near visual acuity. Abbreviations: UIVA, uncorrected intermediate visual acuity, UNVA, uncorrected near visual acuity. |
No intraoperative complications were recorded and at follow-up (1 month), no patient had undergone secondary procedures including laser refractive surgery, IOL removal or rotation, nor YAG laser for posterior capsular opacification. No cystoid macular edema was reported.
Qualitative Cohort
Preoperative and postoperative refractive data for the qualitative cohort are demonstrated in Table 4. These outcomes match the broader retrospective data at both timepoints.
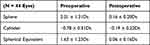 |
Table 4 Qualitative Cohort Refractive Outcomes (N = 22 Patients) |
Figure 6 demonstrates the percentage of patients that experienced photic conditions following the PanOptix toric IOL procedure within this cohort. Practically, patients were required to identify the frequency and severity of photic occurrences, as well as how bothersome they were in nature. The respective answers are listed in Figure 7. Two (9.1%) and four patients (18.2%), respectively, described haloes and glare as severe; however, only two of these patients were “bothered quite a bit” by these symptoms. Neither patient requested explant of the IOL. No patient described any symptoms as significant (“very much bothersome”).
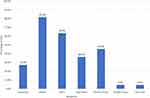 |
Figure 6 Postoperative photic symptom breakdown. |
 |
Figure 7 Symptom breakdown by intensity ((A) = Frequency; (B) = Severity; (C) = Bothersome). |
Additional Symptoms
One patient within the qualitative cohort commented that they felt they had to “refocus” at distance. The patient was 20/20 unaided in each eye at the final postoperative visit and achieved N6 and N4 unaided at intermediate and near, respectively. A further patient described “a film over the eye”, “flickering lights” and a “shadow”. This patient had a prior central retinal vein occlusion (CRVO) and the symptoms were unchanged from prior to surgery.
Bilateral Defocus Curve
Binocular corrected visual acuity for each defocus step is demonstrated in Figure 8. The Panoptix lens achieved good visual acuity across all distances. Mean visual acuity was greater than 0.1 LogMar were observed for defocus levels between −2.50D to +1.00D with the exception of −1.00D and −0.50D steps.
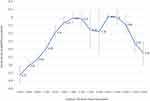 |
Figure 8 Defocus curve for qualitative cohort. Optimal peaks occurred at −2.00Ds and 0.00Ds points. |
Discussion
IOL choice at surgery will be dependent on a range of considerations including general ocular health, predicted postoperative visual acuity and both patient lifestyle and expectations. Monofocal IOLs provide excellent visual acuity and quality for the desired focal length; however, patients will require optical aids to assist vision at other distances. Extended depth of focus (EDOF) IOLs expand the range of good uncorrected vision to include practical intermediate vision and trifocal IOLs, such as the PanOptix IOL, aim to provide unaided visual acuity at all distances and give the best opportunity for spectacle independence across all activities.10 Regardless of IOL type, the presence of residual refractive astigmatism will impact unaided visual acuity and therefore reduce both quality of vision and patient satisfaction.11,12 Accordingly, incorporating a toric component to the respective IOLs to minimise astigmatic error following surgery has been shown to increase efficacy and satisfaction of surgery.13
This retrospective analysis represents the largest current, real-world cohort of patients undergoing PanOptix Trifocal IOL implantation with the toric platform. The mean residual astigmatic error in the broader study was −0.16 ± 0.27D with 94% indicating cylinder ≤0.5D. In 50 eyes, Kohnen et al found 96% of eyes achieving similar outcomes.14 Of interest, in a comparison between 200 toric and 500 non-toric PanOptix IOL eyes, Curreno and co-authors found a significant difference in residual mean error (0.28 ± 0.23D vs 0.42 ± 0.29D in toric and non-toric eyes, respectively) and subsequent percentage of eyes achieving residual error less than 0.5D (94% vs 81%).15 This study highlights the potential improvement in refractive astigmatic outcomes for toric IOLs against non-toric IOLs; however, the study did not mention preoperative mean or range values for both cohorts. Of note, the majority of eyes (68.2%) in the retrospective study required low power (T2) toric correction reflecting larger demographic cohort studies which suggest approximately 80% of eyes will have refractive astigmatism less than 1D. This may further be reflected in the relatively minimal change in astigmatic vectors pre- and post-surgery, albeit there maintained a reduction in all parameters.
The visual outcomes match current literature in smaller, targeted cohorts with 61% of all eyes achieving an UDVA of 20/20 or better increasing to 94.2% achieving 20/30 or better. Kohnen et al described 68% of 50 eyes with the PanOptix toric IOL achieving 20/20.14 Similarly, Carreno and co-authors in 200 Panoptix Toric eyes did not report unilateral unaided visual acuity breakdown however the authors did show mean uncorrected binocular vision at 4 meters of −0.08 LogMAR (approximately 20/16) indicating excellent summation of unaided vision in their cohort. Further, 94.8% and 66% of eyes achieved N8 (approximately 20/40) or better at near and intermediate respectively.15 Donmez et al in 79 eyes indicated all eyes achieving 20/40 or better for both near and intermediate distances.16 Kohnen et al similarly describe all eyes achieving this level of uncorrected near and intermediate visual acuity in their small cohort.14 In the absence of significant differences in residual refractive error between cohorts, the difference at intermediate for our retrospective study is likely to reflect the variation across postoperative visit and assessment distance within the practices. Rosa et al previously highlighted the neuroadaptation process for multifocal IOLs.17 Our findings may suggest that extending the postoperative review visit to minimum 4 weeks may provide an opportunity for better unaided near vision, a finding supported through the smaller prospective study which assessed patients at 3 months and found comparatively improved outcomes for both near and intermediate vision. The assessment distance for intermediate visual acuity was variable across the retrospective study and appeared to reflect a combination of patient habits or preference and work-related distances. The variation represents a limitation of our retrospective study but does likely reflect routine practice. Although not identified in the broader study, understanding spectacle independence provides a practical measure of IOL functionality and therefore most reflective of functional surgery outcomes. Notably, existing Panoptix Toric IOL cohort studies identify between 80% and 94.8% of patients achieving spectacle independence following surgery.14–19 All findings within the retrospective study reflect a unilateral outcome. Given bilateral summation, it would be reasonably expected that binocular outcomes will also result in improved outcomes at all distances and would reflect real-world practice.
Defocus curves simulate visual performance at a range of distances and provide a further analysis of functionality of the trifocal IOL. Albeit in a smaller cohort, the prospective PanOptix Toric study achieved good vision at near, intermediate and distance intervals, exceeding 20/30 at all distances which remains broadly comparable to findings in other PanOptix Toric cohorts and confirms the extended range of the IOL.20–22
One commonly reported issue with the trifocal IOL is the presence of photic phenomena, which varies with different trifocal IOL designs.22,23 Based on our questionnaire, the most frequent and severe phenomena were starbursts, haloes and glare. The impact of the phenomena on daily activities is of equal importance however and the responses indicated only glare was described to be “quite a bit” bothersome (2 patients), suggesting that phenomena is not a debilitating issue in the motivated, Panoptix IOL patient. As previous studies have highlighted the incidence of photic phenomena will decrease over time, likely due to the neuroadaptation process, we expect this to continue to resolve further matching the anecdotal findings of the larger retrospective cohort.14,24
The main component of the study was retrospective in nature which limits the investigation of the findings, in particular toric IOL axis alignment was not recorded which may have provided greater awareness of findings of residual astigmatism. The group does, however, currently represent the largest combined cohort of Toric Panoptix patients within the literature. Our qualitative sub-group outcomes do support the anecdotal findings of the retrospective cohort and together provide a helpful snapshot for surgeons considering treating patients with pre-existing astigmatism who may be interested in achieving full independence from optical aids.
Conclusion
To conclude, the PanOptix toric trifocal IOL demonstrated precision to target good visual performance at all focal distances. Although the majority of patients noticed photic phenomena through the postoperative period, the IOL appeared to exhibit good quality of vision, with minimally bothersome visual disturbances.
Funding
The study was supported by an investigator-initiated trial grant (Alcon Inc).
Disclosure
Dr Lewis Levitz reports grants from Alcon, during the conduct of the study. Dr Uday Bhatt reports grants from Alcon, non-financial support from Acufocus, during the conduct of the study; grants, non-financial support from Alcon, grants from Acufocus, outside the submitted work. Professor Timothy V Roberts reports grants from Alcon, during the conduct of the study. Dr Chris Hodge reports grants from Alcon, during the conduct of the study. The authors report no other conflicts of interest in this work.
References
1. Park SJ, Lee JH, Kang SW, Hyon JY, Park KH. Cataract and cataract surgery: nationwide prevalence and clinical determinants. J Korean Med Sci. 2016;31(6):963–971. doi:10.3346/jkms.2016.31.6.963
2. Zaidi FH, Corbett MC, Burton BJL, Bloom PA. Raising the benchmark for the 21st century—the 1000 cataract operations audit and survey: outcomes, Consultant-supervised training and sourcing NHS choice. Br J Ophthalmol. 2007;91:731–736. doi:10.1136/bjo.2006.104216
3. Wang SY, Stem MS, Oren G, Shtein R, Lichter PR. Patient-centered and visual quality outcomes of premium cataract surgery: a systematic review. Eur J Ophthalmol. 2017;27:387–401. doi:10.5301/ejo.5000978
4. Leyland M, Zinicola E. Multifocal versus monofocal intraocular lenses in cataract surgery: a systematic review. Ophthalmology. 2003;110:1789–1798. doi:10.1016/S0161-6420(03)00722-X
5. Wilkins MR, Allan BD, Rubin GS, et al. Randomized trial of multifocal intraocular lenses versus monovision after bilateral cataract surgery. Ophthalmology. 2013;120(12):2449–2455. doi:10.1016/j.ophtha.2013.07.048
6. Ferrer-Blasco T, Montés-Micó R, Peixoto-de-Matos SC, González-Méijome JM, Cerviño A. Prevalence of corneal astigmatism before cataract surgery. J Cat Refract Surg. 2009;35:70–75. doi:10.1016/j.jcrs.2008.09.027
7. De Bernardo M, Zeppa L, Cennamo M, Iaccarino S, Zeppa L, Rosa N. Prevalence of corneal astigmatism before cataract surgery in Caucasian patients. Eur J Ophthalmol. 2014;24:494–500. doi:10.5301/ejo.5000415
8. Kessel L, Andresen J, Tendal B, Erngaard D, Flesner P, Hjortdal J. Toric intraocular lenses in the correction of astigmatism during cataract surgery: a systematic review and meta-analysis. Ophthalmology. 2016;123:275–286. doi:10.1016/j.ophtha.2015.10.002
9. Thibos LN, Horner D. Power vector analysis of the optical outcome of refractive surgery. J Cataract Refract Surg. 2001;27(1):80–85. doi:10.1016/S0886-3350(00)00797-5
10. Vasavada AR, Nath V, Raj S, Vasavada V, Vasavada S. Technology and intraocular lenses to enhance cataract surgery outcomes-annual review (January 2013 to January 2014). Asia Pac J Ophthalmol. 2014;3:308–321. doi:10.1097/APO.0000000000000092
11. Hayashi K, Manabe S-I, Yoshida M, Hayashi H. Effect of astigmatism on visual acuity in eyes with a diffractive multifocal intraocular lens. J Cat Refract Surg. 2010;36:1323–1329. doi:10.1016/j.jcrs.2010.02.016
12. Hayashi K, Yoshida M, Igarashi C, Hirata A. Effect of refractive astigmatism on all-distance visual acuity in eyes with a trifocal intraocular lens. Am J Ophthalmol. 2021;221:279–286. doi:10.1016/j.ajo.2020.07.051
13. Mojzis P, Majerova K, Plaza-Puche AB, Hrckova L, Alio JL. Visual outcomes of a new toric trifocal diffractive intraocular lens. J Cat Refract Surg. 2015;41:2695–2706. doi:10.1016/j.jcrs.2015.07.033
14. Kohnen T, Lwowski C, Hinzelmann L, et al. Presbyopia correction in astigmatic eyes using a toric trifocal intraocular lens with quadrifocal technology. J Refract Surg. 2020;36(10):638–644. doi:10.3928/1081597X-20200729-04
15. Carreño E, Carreño EA, Carreño R, Carreño M, López V, Potvin R. Refractive and visual outcomes after bilateral implantation of a trifocal intraocular lens in a large population. Clin Ophthalmol. 2020;7(14):369–376. doi:10.2147/OPTH.S238841
16. Donmez O, Asena BS, Aydin Akova Y. Subjective and objective clinical outcomes of a new trifocal toric intraocular lens and effect of femtosecond laser cataract surgery. Eur J Ophthalmol. 2021;16:11206721211046496.
17. Rosa AM, Miranda ÂC, Patrício M, et al. Functional magnetic resonance imaging to assess the neurobehavioral impact of dysphotopsia with multifocal intraocular lenses. Ophthalmology. 2017;124(9):1280–1289. doi:10.1016/j.ophtha.2017.03.033
18. Hovanesian JA, Jones M, Allen Q. The PanOptix Trifocal IOL vs the ReSTOR 2.5 Active Focus and ReSTOR 3.0-add multifocal lenses: a study of patient satisfaction, visual disturbances, and uncorrected visual performance. Clin Ophthalmol. 2021;15:983–990. doi:10.2147/OPTH.S285628
19. Blehm C, Potvin R. Reported patient satisfaction and spectacle independence following bilateral implantation of the PanOptix(®) trifocal intraocular lens. Clin Ophthalmol. 2021;15:2907–2912. doi:10.2147/OPTH.S323337
20. de Medeiros AL, de Araújo Rolim AG, Motta AFP, et al. Comparison of visual outcomes after bilateral implantation of a diffractive trifocal intraocular lens and blended implantation of an extended depth of focus intraocular lens with a diffractive bifocal intraocular lens. Clin Ophthalmol. 2017;11:1911–1916. doi:10.2147/OPTH.S145945
21. Yeu EM, Petznick A, Gu X. The landscape of presbyopia correction with IOLs. Available from: https://us.alconscience.com/sites/g/files/rbvwei1736/files/pdf/The-Landscape-of-Presbyopia-Correction-with-IOLs-US-ACP-1900033.pdf.
22. Ribeiro FJ, Ferreira TB. Comparison of visual and refractive outcomes of 2 trifocal intraocular lenses. J Cat Refract Surg. 2020;46:694–699. doi:10.1097/j.jcrs.0000000000000118
23. Ukai Y, Okemoto H, Seki Y, et al. Quantitative assessment of photic phenomena in the presbyopia-correcting intraocular lens. PLoS One. 2021;16(12):e0260406. doi:10.1371/journal.pone.0260406
24. Lawless M, Hodge C, Reich J, et al. Visual and refractive outcomes following implantation of a new trifocal intraocular lens. Eye Vis. 2017;4:10. doi:10.1186/s40662-017-0076-8
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.