Back to Journals » Clinical Ophthalmology » Volume 16
Optical Biometry and Lens Power Calculations in 500 Phakic Patients: Axial Length and Corneal Curvature in the Fellow Eye
Authors Kristianslund O , Hassaf SE, Drolsum L
Received 28 May 2022
Accepted for publication 14 July 2022
Published 23 August 2022 Volume 2022:16 Pages 2775—2780
DOI https://doi.org/10.2147/OPTH.S375743
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Scott Fraser
Olav Kristianslund,1,2 Safia Esmail Hassaf,1 Liv Drolsum1,2
1Department of Ophthalmology, Oslo University Hospital, Oslo, Norway; 2Institute of Clinical Medicine, University of Oslo, Oslo, Norway
Correspondence: Olav Kristianslund, Department of Ophthalmology, Oslo University Hospital, Mailbox 4956, Nydalen, Oslo, 0424, Norway, Tel +47 22 11 85 45, Email [email protected]
Objective: In eyes with severe corneal pathology, biometric measurements of the corneal curvature (K) can be challenging. The aims of this study were to test whether K mean values from the fellow eye can be used as substitute in lens power calculations and to determine if similarity in axial length (AL) in a patient’s two eyes implies similarity also in the corneal curvature.
Methods and Analysis: A retrospective study of optical biometry measurements in 500 adults (1000 phakic eyes) that was scheduled for cataract surgery. Inclusion criteria were complete recordings of all parameters in both eyes and a signal-to-noise ratio of at least 10. Similar AL was defined as less than 0.3 mm difference between the patient’s two eyes.
Results: The IOL power calculated with K mean from the fellow eye was 0.39 D (standard deviation (SD) 0.57) different from the calculation with both AL and K mean from the correct eye. The difference was larger than 1.0 D in 26 (5%) eyes. In patients with similar AL in their two eyes (n = 372), the interocular difference in K mean was 0.43 D (SD 0.67 D), compared to 0.45 D (SD 0.49 D) for the patients with an AL difference of 0.3 mm or more (n = 128) (p = 0.81).
Conclusion: Lens calculations with keratometry values from the fellow eye as substitute yielded quite similar results as calculations with the correct values. Hence, this seems to be an acceptable approach in patients with incomplete keratometry recordings. Similarity in AL between a person’s two eyes did not imply more similar corneal curvatures.
Keywords: optical biometry, cataract surgery, axial length, corneal curvature, intraocular lens, IOL, IOL power calculation
Introduction
Cataract surgery is one of the most common surgical procedures in the health care system, with an estimated 20–30 millions of operations performed globally each year.1 The risk of complications is generally low, and most patients expect a successful outcome with marked vision improvement and a satisfactory refractive result.2,3 To achieve a predictable postoperative refraction, the intraocular lens (IOL) power calculation requires accurate optical biometry.4 In most patients with cataract, such measurements are feasible in both eyes. However, adequate keratometry recordings may be difficult to obtain in some eyes with serious corneal pathologies, such as traumatic perforation, previous keratitis, trachoma or advanced corneal dystrophy.
In case of preoperative measurement errors in one eye, some would consider to use the IOL calculation in the fellow eye, based on the assumption that the two eyes are similar in terms of refraction. The scientific basis and clinical effectiveness of this approach does not seem to be well documented,5 although normal biometry measures have been studied to some extent6,7 and a high degree of interocular symmetry has been shown.5,8–10 Still, exact similarity between a person’s two eyes is often not present,5,6 and the difference can be quite considerable in some patients. If the correlation between the prediction error in the first eye versus the second eye was consistent, it could be incorporated into the lens calculation prior to second eye surgery to improve the refractive outcome.8,11,12 However, several authors have discussed that partial adjustment may be better than full adjustment,11,12 likely related to varying degrees of similarity between patients’ two eyes in terms of optical biometry measures.11
Based on the anatomy of the human eye, one might hypothesize that axial length (AL) and corneal curvature are highly correlated parameters. If this was true, one would expect that patients with similar ALs in their two eyes would also have similar corneal curvatures. We have not identified any studies specifically addressing this question, and we wanted to test this hypothesis by analyzing optical biometry measurements from a high number of eyes. The aims of the present study were thus to test whether K mean values from the fellow eye can be used as substitute in lens power calculations and to determine if similarity in AL in a patient’s two eyes can predict similarity also in corneal curvature.
Materials and Methods
This retrospective study analyzed optical biometry measurements of 1000 phakic eyes in 500 adult patients scheduled for cataract surgery in the first half of 2020 in the Department of Ophthalmology at Oslo University Hospital. Inclusion criteria were complete optical biometry recordings of AL, corneal curvature and anterior chamber depth (ACD) in both eyes and a signal-to-noise ratio (SNR) of at least 10. Examinations were performed with NIDEK optical biometer (NIDEK Biometer AL-scan, NIDEK Co., Ltd, Gamagori, Japan). For corneal curvature, we used the K mean measured in the 2.4 mm central zone of the cornea. Similarity in AL in the two eyes of a patient was defined as a difference of less than 0.3 mm, in accordance with the alert threshold of the optical biometer. The main analysis was also performed using a more restrictive inclusion criterion, requiring an SNR above 15 in both eyes. In addition, we performed a subgroup analysis of interocular differences for patients with normal biometry measures, defined as AL of 22–26 mm and K mean of 40–48 D in both eyes, as compared to the patients with abnormal biometry measures (outside these limits) in one or both eyes.
Since this was a retrospective quality study, data were registered without any personally identifiable information, and no additional information was obtained from medical records. The study and the publication of the results were approved by the Oslo University Hospital Data Protection Office/local Ethics Committee, which waived the need for approval by the Regional Ethical Committee or written informed consent. The study adhered to the tenets of the Declaration of Helsinki and is reported in accordance with the SQUIRE guidelines (Standards for QUality Improvement Reporting Excellence).13 Data may be considered for sharing upon reasonable request.
Statistics
The statistical analysis was performed with SPSS, version 25.0 (IBM Corp., Armonk, USA). The results have been presented as mean (SD) unless otherwise noted. Additional IOL power calculations with corneal curvature values from the fellow eye as substitute were performed using the SRK II formula, which is easily available for calculations in large datasets. The differences in AL, ACD and K mean between the patients’ two eyes were calculated as absolute values (ie either 0 or a positive value) to determine the mean interocular difference for each parameter. In addition, each parameter was compared statistically between the eyes with a paired-samples t-test, in which the interocular differences were consequently calculated as the value in the right eye minus the value in the left eye, which could be either 0, a negative or a positive value for each patient.
Results
Optical biometry measurements were obtained from 500 adult patients (1000 eyes) with a mean age of 70.1 (SD 12.7) years, and 53% women.
Intraocular Lens Power Calculations
The mean difference in IOL power for emmetropia between each patient’s two eyes, calculated as absolute (positive) values, was 0.79 D (SD 1.14 D). The interocular difference was larger than 0.5 D in 228 (46%) patients and larger than 1.0 D in 114 (23%) patients. The mean IOL power for emmetropia in right eyes versus left eyes is shown in Table 1.
 |
Table 1 Optical Biometry in 500 Patients (1000 Eyes): Axial Length, Anterior Chamber Depth (ACD), and Corneal Curvature (K Mean). Results are Presented as Mean (Standard Deviation) |
The IOL power calculated by using the K mean from the fellow eye (left) as substitute differed by 0.39 D (SD 0.57 D) compared to the calculation with both AL and K mean from the correct eye (right). This difference was larger than 0.5 D in 121 (24%) patients and larger than 1.0 D in 26 (5%) patients. Similar results were found when calculating the IOL power for the left eye by using K mean values from the right eye as substitute. Substituting the K mean value from the fellow eye yielded a significantly better result than simply using the IOL power for emmetropia from the fellow eye (p < 0.001).
Symmetry in Axial Length and Corneal Curvature
The mean differences in optical biometry measures between each patient’s two eyes in absolute (positive) values were 0.27 mm (SD 0.41 mm) for AL, 0.43 D (SD 0.63 D) for K mean and 0.11 mm (SD 0.16 mm) for ACD. A total of 372 (74%) patients had similar AL in their two eyes (<0.3 mm difference), and these patients had an interocular difference in K mean of 0.43 D (SD 0.67 D), compared to 0.45 D (SD 0.49 D) for the 128 patients with a larger difference in AL (p = 0.81). When the analysis only included measurements with an SNR above 15 (n = 351 altogether), the corresponding results were 0.44 D (SD 0.68 D) and 0.43 D (SD 0.40 D), respectively (p = 0.95).
Furthermore, the same comparison was performed within the group of 404 patients defined as having normal biometry measures in both eyes and within the group of 96 patients with abnormal measures in one or both eyes. In neither group was the interocular difference in K mean significantly different between patients with similar AL versus patients with a larger variation in AL. However, the interocular difference in K mean was smaller in the group of normal eyes compared to the group of abnormal eyes; 0.38 (SD 0.42) D versus 0.66 (SD 1.13) D, respectively (p = 0.02), as were also the interocular differences in AL in these two groups; 0.23 (SD 0.29) mm versus 0.47 (SD 0.70) mm, respectively (p = 0.001).
Comparison Between Left and Right Eyes
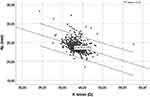
Differences in AL, ACD and K mean between right and left eyes calculated as part of a paired-samples t-test (consequently, the right minus the left eye) are shown in Table 1. The difference was not statistically significant for AL (p = 0.22), borderline significant for ACD (p = 0.05) and significant for K mean (p = 0.02) with a slightly higher value for left eyes compared to right eyes. Each of these parameters was highly correlated between the two eyes (Table 1). Furthermore, AL and K mean were found to be significantly correlated measures, with r = −0.378 (p < 0.001) in right eyes (Figure 1), and r = −0.378 (p < 0.001) in left eyes.
Discussion
In eyes with serious corneal pathology, it can be challenging to perform optical biometry examinations. In such cases, one may consider to use the values from the fellow eye as substitute in the IOL power calculations. In the present study, we analyzed optical biometry measurements of 1000 phakic eyes in 500 patients scheduled for cataract surgery in a university hospital. The results showed that IOL power calculations with the K mean from the fellow eye as substitute yielded acceptable results. However, patients with similar AL in their two eyes did not necessarily have more similar corneal curvatures than others; hence, similarity in AL did not seem to be a reliable predictor of full interocular symmetry.
In today’s cataract surgery, patients’ expectations are high and seem to be increasing, not least regarding refractive outcomes. Implantation of an IOL with suboptimal lens power has been identified as one of the largest groups of malpractice claims after cataract surgery and one of the main reasons for IOL explantation.2 Even in cases of apparently good biometry measurements, prediction errors may occur, and various calculation formulas and adjustments for second eye surgery have been suggested for improvement.11 Still, in some eyes, it is challenging to obtain any biometry measures at all, and in particular for some ocular conditions it can be difficult to measure the corneal curvature, such as in eyes with corneal perforation, prior keratitis, or in cases of pronounced corneal oedema, eg, due to Fuch’s dystrophy.
In planning for cataract surgery in such eyes, one may consider to use the biometry measurements of the fellow eye to compensate for missing values, based on the assumption that the two eyes of a person are symmetric and almost similar. Since this assumption is not always true, we wanted to test the approach by performing IOL power calculations with the value from the fellow eye as substitute. Further, we wanted to determine if we can predict when interocular symmetry is present by analyzing high-quality optical biometry measurements of 500 patients (1000 phakic eyes) scheduled for cataract surgery. The results showed that using the K mean from the fellow eye as substitute yielded a mean difference in lens power of 0.39 D compared to calculations with the correct values, with only 5% of the patients having a difference larger than 1.0 D. This result was better than simply using the calculated lens power from the fellow eye, which yielded a mean difference of 0.79 D, and a difference larger than 1.0 D in 23% of the patients. Further, the results showed that patients with similar AL in their eyes did not have more equal corneal curvatures than patients with a larger difference in AL. Nevertheless, it seems that we can expect a smaller interocular difference for AL and corneal curvature in patients with ocular biometry measures within the normal range.
We have not identified other publications specifically addressing these same research questions. However, some previous studies have examined correlations of ocular biometry measures between a patient’s two eyes, and reported a quite high5,8–11 or modest6 degree of correlation for the same parameter. In the present study, each of the parameters AL, corneal curvature and ACD had highly correlated values in the two eyes of each patient. The mean values for right and left eyes were similar for AL, while they were borderline significantly different for ACD, and significantly different for K mean with slightly higher values for left eyes (Table 1). The clinical significance of this latter finding is questionable, although it is consistent with a previous study that included a high number of patients.5 It should be mentioned that the present study was performed in a tertiary referral clinic with a diversified patient population, and thus with a possibly larger variation between the two eyes than in the general population. Still, the average biometry values were mostly consistent with previous reports5,6 with an AL of 24.0 mm, K mean of 43.6 D and ACD of 3.1 mm.
The hypothesis of the present study was based on the assumption that the two eyes of a patient are almost similar, and further the assumption that the AL and the corneal curvature in an eye are correlated measures. A few previous studies have reported some degree of correlation between the AL and the corneal curvature, demonstrating that a longer eye is often associated with a slightly flatter cornea.6,14 One study even investigated the genetic scaling of the eye anatomy and its symmetry, particularly in relation to AL and corneal curvature.15 However, in a congress abstract, Cayette et al16 reported no statistically significant correlation between these parameters. In the present study, we found a significant correlation between AL and K mean in the same eye; however, the correlation was far from 1. This is in accordance with our finding that similar AL in the two eyes of a patient was not necessarily associated with similarity also in corneal curvature. Another factor to consider in eyes with severe corneal pathology, is possible changes in AL due to scarring causing excessive flattening or ectasia causing excessive steepening. It should also be mentioned that even ALs defined as similar (less than 0.3 mm difference) may result in clinically significant differences in IOL power calculations.
The main clinical implications of the present study are that in patients with inadequate keratometry recordings in one eye, we cannot assume that the values in the other eye are equal even if there is interocular similarity in AL. Great efforts should therefore be taken to perform adequate recordings of both eyes. However, sometimes this is not achievable. It seemed that using the keratometry values from the fellow eye in the lens power calculations resulted in quite small differences compared to the correct values, and it was better than simply choosing the calculated lens power from the fellow eye. Consistent with others5,8–10 we found a quite high degree of symmetry between the eyes. Furthermore, it seems that in patients with optical biometry measurements within the normal range, one can assume less interocular difference. In preoperative evaluations of eyes with corneal pathology, also other clinical information is helpful to evaluate the likelihood of similarity in refraction between the eyes, including use of glasses, known anisometropia, and previous keratometry recordings.
A main strength of the present study is the high number of included eyes. As the study only evaluated anonymous data, other medical information was not available. For this reason, we did not analyze refractive outcomes and prediction errors, and hence, could not determine the likelihood of measurement errors, which is a limitation. However, we excluded low-quality measurements that did not meet the inclusion criteria with complete recordings of AL, K mean and ACD in both eyes and an SNR of at least 10, or even higher in the additional analysis. Conditions or previous treatment that may affect the AL or corneal curvature were expected to have little influence on the mean values, and we also performed additional analyses after excluding eyes with abnormal biometry values. The biometry measurements were performed in a cataract clinic with a diversified patient population, which is important to consider in the interpretation of the result, as the number of patients with interocular differences were possibly higher than normal. The IOL power calculations were performed with the SRK II formula, as this is publicly available for calculations in large data sets.
In conclusion, the present study showed that IOL power calculations with the keratometry values from the fellow eye yielded quite similar results as with the correct values. Hence, it seems that in eyes with serious corneal pathology, this approach is better than simply using the IOL power from the fellow eye. The study further revealed that similar AL in the two eyes of a patient did not predict similarity also in corneal curvature. Still, a quite high degree of correlation between the two eyes was found, and patients with ocular biometry measures within the normal range had less interocular differences for AL and corneal curvature.
Ethics Approval Statement
This study was approved by an Ethics Committee/Data Protection Officer.
Funding
There is no funding to report.
Disclosure
No competing interests for any author. Outside the submitted work: Olav Kristianslund has received a small fee for a presentation about intraocular lens dislocation at a seminar by Bausch&Lomb.
References
1. Shah SP, Gilbert CE, Razavi H, Turner EL, Lindfield RJ; International Eye Research N. Preoperative visual acuity among cataract surgery patients and countries’ state of development: a global study. Bull World Health Organ. 2011;89(10):749–756. doi:10.2471/BLT.10.080366
2. Brick DC. Risk management lessons from a review of 168 cataract surgery claims. Surv Ophthalmol. 1999;43(4):356–360. doi:10.1016/S0039-6257(98)00052-6
3. Mollazadegan K, Lundstrom M. A study of the correlation between patient-reported outcomes and clinical outcomes after cataract surgery in ophthalmic clinics. Acta Ophthalmol. 2015;93(3):293–298. doi:10.1111/aos.12490
4. Melles RB, Kane JX, Olsen T, Chang WJ. Update on intraocular lens calculation formulas. Ophthalmology. 2019;126(9):1334–1335. doi:10.1016/j.ophtha.2019.04.011
5. De Bernardo M, Zeppa L, Forte R, et al. Can we use the fellow eye biometric data to predict IOL power? Semin Ophthalmol. 2017;32(3):363–370. doi:10.3109/08820538.2015.1096400
6. Hoffer KJ. Biometry of 7500 cataractous eyes. Am J Ophthalmol. 1980;90(3):360–368. doi:10.1016/S0002-9394(14)74917-7
7. Olsen T, Arnarsson A, Sasaki H, Sasaki K, Jonasson F. On the ocular refractive components: the Reykjavik Eye Study. Acta Ophthalmol Scand. 2007;85(4):361–366. doi:10.1111/j.1600-0420.2006.00847.x
8. Jabbour J, Irwig L, Macaskill P, Hennessy MP. Intraocular lens power in bilateral cataract surgery: whether adjusting for error of predicted refraction in the first eye improves prediction in the second eye. J Cataract Refract Surg. 2006;32(12):2091–2097. doi:10.1016/j.jcrs.2006.08.030
9. Li Y, Bao FJ. Interocular symmetry analysis of bilateral eyes. J Med Eng Technol. 2014;38(4):179–187. doi:10.3109/03091902.2014.899401
10. Muthappan V, Paskowitz D, Kazimierczak A, Jun AS, Ladas J, Kuo IC. Measurement and use of postoperative anterior chamber depth of fellow eye in refractive outcomes. J Cataract Refract Surg. 2015;41(4):778–784. doi:10.1016/j.jcrs.2014.08.034
11. Covert DJ, Henry CR, Koenig SB. Intraocular lens power selection in the second eye of patients undergoing bilateral, sequential cataract extraction. Ophthalmology. 2010;117(1):49–54. doi:10.1016/j.ophtha.2009.06.020
12. Olsen T. Use of fellow eye data in the calculation of intraocular lens power for the second eye. Ophthalmology. 2011;118(9):1710–1715. doi:10.1016/j.ophtha.2011.04.030
13. Ogrinc G, Davies L, Goodman D, Batalden P, Davidoff F, Stevens D. SQUIRE 2.0 (Standards for QUality Improvement Reporting Excellence): revised publication guidelines from a detailed consensus process. BMJ Qual Saf. 2016;25(12):986–992. doi:10.1136/bmjqs-2015-004411
14. Fledelius HC, Goldschmidt E. Oculometry findings in high myopia at adult age: considerations based on oculometric follow-up data over 28 years in a cohort-based Danish high-myopia series. Acta Ophthalmol. 2010;88(4):472–478. doi:10.1111/j.1755-3768.2008.01472.x
15. Guggenheim JA, Zhou X, Evans DM, et al. Coordinated genetic scaling of the human eye: shared determination of axial eye length and corneal curvature. Invest Ophthalmol Vis Sci. 2013;54(3):1715–1721. doi:10.1167/iovs.12-10560
16. Cayette S, Touzeau O, Rodallec FT, et al. Correlation between eye axial length and corneal biometric parameters. Invest Ophthalmol Vis Sci. 2011;52:5187.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.