Back to Journals » Journal of Pain Research » Volume 16
Veteran Perspectives on Phantom Limb Pain and Non-Drug Interventions
Authors Rich TL, Phelan HL, Gravely AA, Falbo KJ , Finn JA, Matsumoto ME, Muschler KJ, Olney CM , Kiecker JE, Hansen AH
Received 4 October 2022
Accepted for publication 13 April 2023
Published 25 April 2023 Volume 2023:16 Pages 1391—1400
DOI https://doi.org/10.2147/JPR.S390658
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Alaa Abd-Elsayed
Tonya L Rich,1,2 Hannah L Phelan,1,3 Amy A Gravely,1 Kierra J Falbo,1,2 Jacob A Finn,1,4 Mary E Matsumoto,1,5 Katherine J Muschler,1 Christine M Olney,1,2,6 Jessica E Kiecker,1 Andrew H Hansen1,2,7
1Minneapolis Veteran’s Affairs Health Care System, Minneapolis, MN, USA; 2Department of Rehabilitation Medicine, Division of Rehabilitation Science, University of Minnesota, Minneapolis, MN, USA; 3Medical College of Wisconsin, Milwaukee, WI, USA; 4Department of Psychiatry, University of Minnesota, Minneapolis, MN, USA; 5Department of Rehabilitation Medicine, University of Minnesota, Minneapolis, MN, USA; 6Department of Nursing, University of Minnesota, Minneapolis, MN, USA; 7Department of Biomedical Engineering, University of Minnesota, Minneapolis, MN, USA
Correspondence: Tonya L Rich, Tel +1 612-467-5463, Fax +1 612-725-2093, Email [email protected]
Background: Phantom limb pain (PLP) commonly occurs post-amputation and can negatively affect the daily functioning of persons with amputation. Best practices for medication and non-drug management remain unclear.
Objective: To better understand the PLP experience and patients’ familiarity with treatments, phone interviews were conducted at the Minneapolis Veterans Affairs Regional Amputation Center in Veterans with amputations.
Methods: Fifty Veteran participants (average age 66, 96% male) with lower limb amputation were recruited for phone-based data collection of patient-reported outcomes (ie, demographics using the Trinity Amputation and Prosthesis Experience Scales-Revised (TAPES-R) and pain experience using the Phantom Phenomena Questionnaire) to characterize the population and a semi-structured interview. Notes taken during interviews were analyzed using the Krueger and Casey constant comparison analysis method.
Results: Participants had an average of 15 years since amputation, and 80% reported PLP as identified with the Phantom Phenomena Questionnaire. Investigators identified several core themes from the qualitative interviews including 1) high variability in the experience of PLP, 2) acceptance and resilience, and 3) PLP treatment perceptions. The majority of participants reported trying common non-drug treatments with none endorsed consistently as highly effective.
Conclusion: More research is needed to inform identification and implementation of clinical best practices for non-drug interventions for PLP and understand the factors that influence engagement in non-drug interventions. The participants in this study were largely male, so these results may not be generalizable to females.
Keywords: amputation, phantom limb pain, rehabilitation, non-drug interventions, pain
Introduction
The population of those living with an amputation is growing with a prevalence expected to reach 3.6 million in the general US population by 2050.1 Of patients who survive an amputation, 48–85% experience phantom limb pain (PLP), a form of chronic neuropathic pain, where pain is perceived in the area where the limb has been amputated and is no longer there.2,3 Although some individuals with PLP respond to existing clinical treatments, when PLP is severe, limited effective treatments have been identified with sufficient evidence that can improve quality of life.4 Recent review papers cite preliminary evidence to support multi-modal approaches, imagery-based therapies (eg, graded motor imagery [GMI], mirror therapy, and virtual visual feedback) however at present, evidence is lacking for all non-drug treatments with rigorous studies needed.5–7
The Veterans Affairs (VA) Amputation System of Care (ASoC) serves Veterans with amputations nationally for comprehensive care including ongoing prosthetic and pain management. Given the complexity of the patient population and the lack of strong evidence for currently available non-drug treatments, new pain treatments are needed to effectively treat PLP. However, prior to further developing rehabilitation interventions for PLP in the Veteran population, gaining a greater understanding of how Veterans experience PLP in the context of daily life is essential. The purpose of this study is to qualitatively describe a sample of Veterans including their experience with PLP in daily life and their experiences with currently available clinical interventions.
Materials and Methods
The study was reviewed by the Minneapolis VA Institutional Review Board (IRB). The study received a determination of exempt from the requirements of 38 CFR 16/45 CFR 46, under category 2iii. As exempt human subjects research, written consent is not obtained. All data in this manuscript have been de-identified. The conduct of the study and publication of the results are compliant with the HIPAA Privacy Rule.
Study Design Overview and Setting
This study was a cross-sectional cohort study of Veteran participants from the Minneapolis VA Regional Amputation Center (RAC) that serves the Veterans Integrated Services Networks-23 Midwest region (ie, Minnesota, North Dakota, South Dakota, and portions of Wisconsin, Iowa, Nebraska, and Illinois). To learn more about Veterans’ perspectives, investigators conducted a semi-structured, open-ended interview and collected standardized patient-reported outcome measures by telephone in a sample of Veteran participants.
Inclusion Criteria and Recruitment Procedures
Eligible Veterans were at least 18 years old with lower limb amputation(s). We targeted those with lower limb amputation as this is the most common amputation location.1 Veterans were excluded if they had untreated mental health conditions, cognitive impairment, were living in a long-term care facility, or were receiving hospice care as verified by medical record review. The recruitment target was 50 Veterans as this interview was part of a larger study on patient-reported outcome measures. As we heard from clinicians about the variability of PLP, we sought to have a large enough sample to provide a meaningful contribution to the literature for this exploratory work. The clinicians in our Regional Amputation Center screened Veterans for this study based on a medical record review using the specified inclusion and exclusion criteria. All potential Veterans eligible for participation were mailed a recruitment letter with a follow up phone call to inquire about their interest in participating in the study.
Reflexivity Statement
Two female study team members completed the data collection (T.R. and H.P.) with training in the semi-structured interview guide and patient-reported outcome measures provided by the PI (T.R.). T.R. is an occupational therapist and PhD trained researcher and H.P. was a medical student. Neither T.R. nor H.P. had provided clinical care to the participants.
Data Collection
All Veterans interested in participating were mailed a paper copy of the patient-reported outcome measures (eg, Phantom Phenomena Questionnaire, TAPES-R, among others) prior to the phone interview. Participants were asked to review the measures beforehand for familiarity, and all questions were asked verbally at the time of the phone interview. The interviewer recorded the responses in real time during the interview. Individual interviews were completed in 45–60 minutes. Data collection was performed via phone, rather than via electronic surveys, in order to allow follow-up questions and further discussions with participants.
During the initial learning period, T.R. and H.P. met to discuss how the semi-structured interview guide was working during the interviews. To minimize the risk of error and investigator recall bias, the interviewers took real-time field notes with direct quotes to record subjective comments. Interviewers administered the entire questionnaires, asked follow-up questions as needed, and completed interview notes within 24 hours of the interview.
Measures
To establish trust with the participants, the semi-structured interviews began by discussing the purpose of the study and inviting participants to share a description of their amputation-related pain and how their pain affects daily life. We conducted a semi-structured interview using a guide that includes open-ended questions and follow-up probes (Supplemental Materials S1).
Investigators then transitioned to the Phantom Phenomena Questionnaire, previously developed for individuals with amputation and PLP.8 The Phantom Phenomena Questionnaire differentiates phantom sensation, phantom pain, and residual limb pain including rating the frequency, duration, and intensity. The Phantom Phenomena Questionnaire includes questions on medication use. Additionally, the measure includes questions on any other attempted strategies for the pain and their effectiveness as measured with an open-ended response. Although the Phantom Phenomena Questionnaire has limited published psychometric data, this questionnaire provided a standardized interview structure.
To characterize our population (eg, location of amputation, time since amputation, and presence of residual limb pain or PLP), participants orally completed Part II of the Trinity Amputation and Prosthesis Experience Scales-Revised(TAPES-R).9 The TAPES-R has acceptable person separation reliability of 0.72 and high item separation reliability of 0.91.9
Analysis
T.R. completed formal, in-person training with Krueger and Casey on the constant comparison analysis methodology prior to the commencement of the study.10 T.R. and H.P. analyzed the data. Once coded into themes, the interviewers evaluated the data using the constant comparison analysis methodology of Krueger and Casey.10 The qualitative analysis did not involve software for coding. The qualitative findings are reported using the Consolidation criteria for reporting qualitative studies (COREQ).11 Demographic variables are reported with use of frequency counts and descriptive statistics.
Results
Participants
Recruitment occurred from April 2020 to March 2021. A total of 187 Veterans were screened for eligibility. Of those, 43 were screened out for different reasons (eg, lives in a nursing home or is in hospice care, behavioral concerns, deceased, dementia, no phone number). A total of 144 were invited to participate with a recruitment letter and 94 did not participate for various reasons (eg, declined, declined as they do not experience PLP, no response, or contact information not up to date). Of those approached with a recruitment letter, the response rate was 35%. H.P. completed 12% of the interviews and T.R. completed the remainder of the interviews (88%). The proportion of interviews conducted by the two investigators was based on investigator availability. The telephone interviews were scheduled at the convenience of the participant lasting 45–60 minutes. The interviews were not audio recorded in attempt to offer anonymity and privacy for recruitment purposes. In the majority of cases (96%), only the interviewer and the participant were present. However, in two cases, the participant asked for their spouse to be present for the interview on speaker phone. In both cases, the participant provided all responses. One spouse affirmed the participant’s responses but did not contribute additional information. The investigators observed consistency in the participants’ descriptions and responses to the questions (eg, if they initially described PLP as mild, their description did not change throughout the interview).
This study included 50 participants, and their characteristics are described in Table 1. We did not verify self-report of medical history (eg, location of amputation, time since amputation, medications) with a medical record review. Many Veterans receive care outside the VA system, so a medical review of available VA records may be incomplete.
 |
Table 1 Participant Demographic Characteristics |
In our sample, 40 out of 50 participants (80%) reported PLP. Of the 10 Veterans without PLP, a small portion of participants (n=3, 30%) attributed the lack of PLP to their diminished sensation in the limb due to their personal history of neuropathy.
The TAPES-R includes a question about other medical issues separate from stump pain or PLP that also contribute to overall level of pain experienced. Of the 48 participants who responded to this question, 23 participants (48%) experience other medical issues that contribute to pain that participants consistently reported as distinct from PLP. We omitted this question in two participants due to time. The frequency of other contributing medical issues to pain is reported in Table 2.
 |
Table 2 Other Medical Issues Contributing to General Pain |
Themes
The investigators identified three themes in the qualitative responses of the semi-structured interviews and the Phantom Phenomena Questionnaire including 1) PLP is variable in nature, 2) acceptance and resilience, and 3) PLP treatment perceptions. Themes are described below using exemplar quotes.
PLP is Variable in Nature
There was between-individual variability in all features of PLP experienced by the participants in this study. Few participants described their PLP in the same way, with 32 different descriptions of PLP provided within the sample. Participants described pain and neuropathic qualities (eg, electric, shooting, tingling) as the most frequently used descriptors (n=26).
For example,
It’s [PLP is] like a pitchfork jammed through the foot. It [PLP] feels like glowing red-hot rebar that I stepped on or 100,000 needles or knives. It’s [PLP is] intense but momentary pain. [Interview 34]
PLP feels like you are running through a raspberry bush with thorns and shorts on. It [PLP] grabs, tearing, and embeds its thorns in you. It [PLP] happens when it happens… It’s like all of my nerves are firing all at once. [Interview 20]
Across our sample, participants described a range of pain severity, how often PLP is present, and how the PLP has changed since amputation.
Everyone with a leg cut off has it [PLP]…It’s like if you walked to a concrete wall and took your shoe off and kicked it as hard as you can. Over and over and over again. [Interview 43]
Some [PLP] are really painful but they go away fast and don’t last a long time. Some last longer but they are not as intense. I get them infrequently now, less often. [Interview 44]
It [PLP] feels like a pin sticking right in the end of the stump. It will happen every 10 seconds…wearing the leg can help but I have to be moving…When I overextend and my stump bumps the bottom of the socket it, it triggers phantom pains (like every 10 seconds). Then I can’t sleep for 24 hours. After that day is over, I will feel better the next day but have to sleep for like a day straight. [Interview 32]
For some participants (n=14, 28%), their PLP could be impacted by the addition or removal of their prosthesis.
The best way to describe it [PLP] is like you have the hiccups and you’re just sitting there waiting for the next hiccup to come. If I sit there or lie in my bed and wait for the next electrical shock to come…it just gets worse. That’s why I will get up and try walking on my prosthesis. But that doesn’t always work…it can shorten the duration. [Interview 30]
My brain still thinks it [leg] is there. All the same sensations are there. My brain has a blueprint of the nerves and it won’t give up on the leg that’s not there…If I get up and start doing something, it will relieve it [PLP]. Get up and walk around. [Interview 45]
For others, there was no reportable contributing factor that worsened or alleviated the pain. Some participants described that “a little” PLP does not exist. For example,
When it [PLP] attacks, it is a 10. [Interview 2]
There’s no such thing as a little PLP. It’s [PLP is] really intense every time. I can’t predict it [PLP]. [Interview 33]
Others described a lower intensity that causes minimal distress in their lives.
I have the pain once in a while. It’s [PLP] not serious. It comes and goes fast. It’s is not lingering…It [PLP] is irritating more than anything. [Interview 29]
I can’t call it [PLP] pain. Imagine pouring soda into a glass and watching it fizz. It [PLP] goes all the way down to the toes. It [PLP] starts at the lower end of the stump and goes to the toes that aren’t there. [Interview 27]
Acceptance and Resilience
A small number of participants (n=5, 10%) talked about their acceptance of the pain associated with their amputation. For example,
I’ve learned to live with it [PLP]. [Interview 34]
We live with pain and it becomes the norm…There’s always a little pain…you become numb to it. [Interview 37]
One participant said that they view PLP as part of the process of having an amputation. Another participant recalled that a physician described to them,
The problem with cutting your leg off is there are a billion nerves in there. It’s going to hurt. That’s just the way it is. [Interview 43]
A subset of participants (n=9) described how they view life with PLP from a perspective of resilience. These participants made statements about living their lives with pain and focusing on their desired activities or roles, regardless of the pain. For example,
I live with pain. I go ahead and function. You can’t just sit and give in to it. [Interview 33]
The busier I get, the less I concentrate on the pain…If you really want to do something, you have to push through it. I’ve got as long as I can to get up, move, and do stuff. I’m not going to let myself get in the way. It’s all about attitude. You have to have the right frame of mind. Look up, never down. [Interview 50]
PLP Treatment Perceptions
The participants reported trying a wide variety of medications and non-drug treatment methods to address their PLP (Supplemental Materials S2). In our sample, 48% (n=24) of participants noted that they were currently taking pain medication ranging from over-the-counter medications (eg, ibuprofen) to prescribed medications, and 78% (n=39) listed pain medications as a strategy in the past for PLP. Eighteen different medications were self-reported across participants, with varying reports of effectiveness. Regarding efficacy, some participants reported no PLP relief from pain medications and reported significant side effects (eg, itch, rash, ulcer, memory loss), while others found significant pain relief with prescription medications.
I tried them [pain medications] and they didn’t work. You just have to get used to it [PLP] and get over it [PLP]. [Interview 36]
One participant stated that they look forward to dental procedures as it was their only means to obtain opioids for pain relief. Other participants reported taking their pain medications as prescribed but were unsure if they had any influence on their PLP.
I don’t know. I just take them like I’m supposed to. [Interview 21]
Participants who reported trying non-drug strategies to address their PLP described 22 different strategies with inconsistent reports of usefulness. In this sample, 36 participants (72%) had tried at least one non-drug method with a range of one to eight strategies. The types of non-drug strategies and frequency reported by the sample is included in the Supplemental Materials S2. Fourteen participants (28%) reported no methods outside of medications to deal with their PLP (Figure 1).
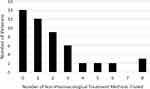 |
Figure 1 Self-reported number of non-drug phantom limb pain treatment methods tried in the sample of 50 Veteran participants per self-report. |
Sixteen participants (32%) utilized some form of metacognition with self-talk and/or attempted to distract themselves from the pain by engaging their mind in something else. For example,
I talk to my brain and say, ‘You’re not supposed to be feeling this. The leg ain’t there. Why are you sending signals to what doesn’t exist.’ That can help a little sometimes. [Interview 22]
It’s mind over matter for me. Nothing is hurting it. How can I have a sprained ankle and limb when it’s not there? [Interview 34]
If it [PLP] happens at night, I will get up and distract myself with TV or the computer. [Interview 38]
Summary of Findings
Participants vividly described PLP in different ways, and PLP is highly individualized with variability in intensity and overall experience. A subset of our sample described how a positive mindset can change the perception of PLP and minimize the impact. Participants identified several strategies for pain, but there was no endorsement for any one effective strategy across participants.
Discussion
The purpose of this study was to describe PLP and the use of PLP interventions in a sample of Veteran participants as there are few papers on the patient’s perspective of interventions provided clinically. In this sample, the participants’ reports regarding PLP are highly variable in nature (eg, frequency, duration, intensity), and for some, it can negatively influence function and quality of life. The participants specifically and vividly described their PLP, different from other potential sources of pain such as residual limb pain, back, hip, or knee pain. While the participants’ descriptions had some commonalities (eg, electrical sensation, sudden onset in nature, unpredictable), the experience was unique to each individual (eg, frequency, perceived contributing factors of PLP, methods for alleviating PLP, changing nature of PLP over time). Consistent with clinical practice, few consistencies were observed across the participants.
The Phantom Phenomena Questionnaire provided a standardized set of questions to guide the participant interviews starting with differentiating phantom sensations, PLP, and residual limb pain.8 Clinicians share with us that this differentiation can be challenging in the clinic as a patient may report all types of pain or sensations as “phantom pains” or PLP. Often subjective questions can guide the clinical differentiation; however, research-based methods are lacking. Having a standardized questionnaire used routinely during follow up visits allows for both consistency in pain reporting (eg, baseline and in response to intervention) and allows for building a clinical profile about the characteristics of the patient’s condition. Griffin et al identified telescoping sensations and pre-amputation pain as two characteristics associated with PLP.12 Incorporating standardized outcomes and/or questionnaires to build a clinical profile could result in early identification of changes in pain or activity.
We observed a variety of descriptions of the PLP experiences in our sample with some stating it was to be expected with the loss of the limb. The descriptions align with recent work and work conducted nearly 25 years ago.13–15 This suggests that although the variability of the PLP experience is acknowledged over the course of time in a limited body of qualitative evidence, innovation continues to be needed in this population. Exploration of novel techniques that are designed using a whole-health framework (eg, mindfulness, sleep, diet, activity) and service delivery models (eg, telehealth, home- and clinic-based intervention) could allow for personalized management that addresses both the amputation-related pain and general well-being given the presence of additional comorbidities that often accompanies an amputation. Whole-health frameworks are often implemented by a number of clinicians (eg, nursing, physical, occupational, recreation therapy, dieticians, among others). Using a whole-health framework could allow more clinicians to be involved the wellness and pain management thus increasing access to services.16
A subset of participants spoke of acceptance and resilience. They attributed their ability to remain engaged in desired daily activities to having this mindset. This supports prior findings that suggest the necessary tasks of daily life can still be completed during “bad” days.17,18 However, others in our sample described long durations of PLP and/or disruptions to sleep and activity. Many of the participants self-reported other comorbid pain conditions which could contribute to greater impact on daily tasks and confound the pain experience. Incorporating periodic psychological support into long-term amputation management is critical to supporting the individuals’ overall resilience and maintaining engagement in desired activities.
The participants self-identified several clinically and non-clinically available interventions (Supplemental Materials S2), however, there was a lack of preference for any particular intervention. This could relate in part to treatment expectations wherein if a treatment strategy is not found to be immediately effective, the strategy is not attempted again later or is assumed not to work from the start. We observed a distribution of non-pharmacological PLP treatments utilized by participants. Most participants reported use of zero to two strategies, while others employed up to eight strategies. Given all participants in this sample were served out of the Minneapolis RAC, treatment access should have been equal; however, we did not account for factors that influence equitable access to healthcare. Our findings on the lack of treatment preference and low report of trying non-drug interventions aligns with others.4,14 Routinely revisiting the use of non-drug strategies could provide an opportunity for the patient to re-engage with the clinician on treatment options.
Some interventions appear deceptively simple such as reports of wearing a prosthesis or walking with the prosthesis resulting in pain reduction yet few participants in our sample reported them. Future work focused on implementation science might help to identify the barriers and facilitators to utilizing these readily accessible, low-cost interventions. Consistent use of low-cost, accessible strategies would be worthwhile to also promote skin health, activity, pain management, and overall health. The Consolidated Framework for Implementation Research could be one approach to studying the provision, education, and uptake of non-pharmacological interventions for amputation-related pain with consideration for the patient’s needs and resources.19
Limitations
This study was an opportunity to gain perspectives of Veteran participants on the influence of PLP on daily life as well as pain management through interviews. We did not explore the participants’ perspective on the potential for improvement in their PLP condition. It is possible that long-standing beliefs exist in both providers and patients, predisposing both groups to the bias that non-drug treatments will be ineffective. It would be advantageous in future work to measure treatment expectations and preferences to understand the participant’s perspective and potential for change.20,21 This work could lead to further developments in clinician and patient education and potentially change the current direction of PLP treatment options. There were no repeat interviews, and the interviewers did not share the field notes with the participants for comment. Additionally, interview data are subject to recall bias. The amputation team may have discussed or even trialed a pain strategy with the participant, but if found to be ineffective, the participant may or may not have recalled trying the strategy.
As these data were completed in the context of a larger study on outcome measures, due to time limitations we did not ask additional questions about how long interventions were pursued and reasons for continuing or discontinuing interventions. Experiencing multiple factors of persistent pain could influence the response to treatment. We did not collect a list of comorbidities such as other persistent pain conditions (eg, low back or hip pain). The Phantom Phenomena Questionnaire was used to guide discussions and differentiation of the types of amputation-related pain. However, it can be difficult for some patients to distinguish between different types of pain, which may have influenced these self-reported results.
The participants in this study were largely male (96%) and white (92%), so these results may not be generalizable to females or people of diverse backgrounds. Future studies considering the unique needs of females with amputations is critically needed given there are known sex differences in pain influencing the biopsychosocial factors.22 Considering a multi-site study and/or standardization of clinical outcome data could allow for longitudinal examination of sex differences and potentially identification of additional intervention needs.
Conclusions
PLP can have a profound impact on daily functioning in some participants with lower limb amputations and continues to be a major clinical challenge without clear shared clinical practice guidelines or best practices. Few participants identified use of effective pain management strategies. Additional qualitative work to learn more about the aspects of intervention (eg, duration, reasons for continuing or discontinuing, routines around the intervention) is warranted. If the current strategies are ineffective for pain control, future work is needed on engaging end users in the development and design of novel non-drug interventions. To create practical pain management strategies, consideration must be given to the uniqueness of PLP as compared to treatment options for other sources of chronic pain. Altogether, this work would contribute to individualized treatment options and overarching clinical practice guidelines.
Abbreviations
ASoC, Amputation System of Care; COREQ, Consolidation criteria for reporting qualitative studies; PLP, Phantom limb pain; RAC, Regional Amputation Center; TAPES-R, Trinity Amputation and Prosthesis Experience Scales-Revised; VA, Veterans Affairs.
Acknowledgments
We thank the Veterans that participated in our study. We thank Julie Toth, RN, CCRC, CIP for her guidance on this study.
Funding
This work was supported in part by the US Department of Veterans Affairs Rehabilitation Research and Development Career Development Award 1IK1RX003216-01A2 and was conducted at the Minneapolis VA Health Care System. The materials presented here solely represent the views of the authors and do not represent the view of the US Department of Veterans Affairs or the United States Government.
Disclosure
The authors declare they have no competing interests.
References
1. Ziegler-Graham K, MacKenzie EJ, Ephraim PL, Travison TG, Brookmeyer R. Estimating the prevalence of limb loss in the United States: 2005 to 2050. Arch Phys Med Rehabil. 2008;89(3):422–429. doi:10.1016/j.apmr.2007.11.005
2. Sherman RA, Sherman CJ. Prevalence and characteristics of chronic phantom limb pain among American veterans. Results of a trial survey. Am J Phys Med. 1983;62(5):227–238.
3. Morgan SJ, Friedly JL, Amtmann D, Salem R, Hafner BJ. Cross-sectional assessment of factors related to pain intensity and pain interference in lower limb prosthesis users. Arch Phys Med Rehabil. 2017;98(1):105–113. doi:10.1016/j.apmr.2016.09.118
4. Trevelyan EG, Turner WA, Robinson N. Perceptions of phantom limb pain in lower limb amputees and its effect on quality of life: a qualitative study. Br J Pain. 2016;10(2):70–77. doi:10.1177/2049463715590884
5. Batsford S, Ryan CG, Martin DJ. Non-pharmacological conservative therapy for phantom limb pain: a systematic review of randomized controlled trials. Physiother Theory Pract. 2017;33(3):173–183. doi:10.1080/09593985.2017.1288283
6. Herrador Colmenero L, Perez Marmol JM, Martí-García C, et al. Effectiveness of mirror therapy, motor imagery, and virtual feedback on phantom limb pain following amputation: a systematic review. Prosthet Orthot Int. 2018;42(3):288–298. doi:10.1177/0309364617740230
7. Hyung B, Wiseman-Hakes C. A scoping review of current non-pharmacological treatment modalities for phantom limb pain in limb amputees. Disabil Rehabil. 2022;44(19):5719–5740. doi:10.1080/09638288.2021.1948116
8. Ehde DM, Czerniecki JM, Smith DG, et al. Chronic phantom sensations, phantom pain, residual limb pain, and other regional pain after lower limb amputation. Arch Phys Med Rehabil. 2000;81(8):1039–1044. doi:10.1053/apmr.2000.7583
9. Gallagher P, Franchignoni F, Giordano A, MacLachlan M. Trinity amputation and prosthesis experience scales: a psychometric assessment using classical test theory and rasch analysis. Am J Phys Med Rehabil. 2010;89(6):487–496. doi:10.1097/PHM.0b013e3181dd8cf1
10. Krueger RA, Casey MA. Focus Groups: A Practical Guide for Applied Research. SAGE; 2000.
11. Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual Health Care. 2007;19(6):349–357. doi:10.1093/intqhc/mzm042
12. Griffin SC, Alphonso AL, Tung M, et al. Characteristics of phantom limb pain in U.S. civilians and service members. Scand J Pain. 2022;22(1):125–132. doi:10.1515/sjpain-2021-0139
13. Björkman B, Arnér S, Lund I, Hydén LC. Adult limb and breast amputees’ experience and descriptions of phantom phenomena-A qualitative study. Scand J Pain. 2017;1(1):43–49. doi:10.1016/j.sjpain.2009.09.001
14. Horne CE, Paul J. Pain support for adults with a diabetes-related lower limb amputation: an empirical phenomenology study. Pain Manag Nurs. 2019;20(3):270–275. doi:10.1016/j.pmn.2018.09.007
15. Mortimer C, Steedman WM, McMillan IR, Ravey J. Phantom pain II: patients’ experiences, beliefs and knowledge. Br J Ther Rehabil. 1998;5(7):352–369. doi:10.12968/bjtr.1998.5.7.14062
16. Bokhour BG, Hyde J, Kligler B, et al. From patient outcomes to system change: evaluating the impact of VHA’s implementation of the whole health system of care. Health Serv Res. 2022;57(S1):53–65. doi:10.1111/1475-6773.13938
17. Camacho VM, Carlson AN, Bondoc S. Addressing phantom pain through occupational participation: a qualitative study of support group participants. OTJR. 2021;41(2):116–123. doi:10.1177/1539449220973950
18. Day MC, Wadey R, Strike S. Living with limb loss: everyday experiences of “good” and “bad” days in people with lower limb amputation. Disabil Rehabil. 2019;41(20):2433–2442. doi:10.1080/09638288.2018.1467502
19. Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4(1):50. doi:10.1186/1748-5908-4-50
20. Linde K, Witt CM, Streng A, et al. The impact of patient expectations on outcomes in four randomized controlled trials of acupuncture in patients with chronic pain. Pain. 2007;128(3):264–271. doi:10.1016/j.pain.2006.12.006
21. George SZ, Robinson ME. Preference, expectation, and satisfaction in a clinical trial of behavioral interventions for acute and sub-acute low back pain. J Pain. 2010;11(11):1074–1082. doi:10.1016/j.jpain.2010.02.016
22. Fillingim RB. Individual differences in pain: understanding the mosaic that makes pain personal. Pain. 2017;158(Suppl 1):S11–S18. doi:10.1097/j.pain.0000000000000775
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
