Back to Journals » Biologics: Targets and Therapy » Volume 17
Treating Alpelisib-Induced Hyperinsulinemia in Patients with Advanced Breast Cancer – A Real-Life Experience
Authors Percik R , Oedegaard Smith C, Leibovici A, Shai A
Received 2 November 2022
Accepted for publication 28 February 2023
Published 3 May 2023 Volume 2023:17 Pages 61—67
DOI https://doi.org/10.2147/BTT.S395817
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Doris Benbrook
Ruth Percik,1– 3 Cecilie Oedegaard Smith,3,4 Anca Leibovici,5,6 Ayelet Shai7
1Division of Endocrinology, Diabetes and Metabolism, Sheba Medical Center, Ramat Gan, Israel; 2Endo-Oncology Clinic, Sheba Medical Center, Ramat Gan, Israel; 3Sackler Faculty of Medicine, Tel Aviv University, Tel-Aviv, Israel; 4Oncology Institute, Sheba Medical Center, Ramat Gan, Israel; 5Oncology Department, Galilee Medical Center, Nahariya, Israel; 6Azrielly Faculty of Medicine, Bar-Ilan University, Zafed, Israel; 7Breast Cancer Unit, Division of Oncology, RAMBAM Health Care Campus, Haifa, Israel
Correspondence: Ayelet Shai, Oncology Department, Rambam Health Care Campus, Ha’alia Hashnia 8, Haifa, 3109601, Israel, Tel +972507887731, Email [email protected]
Abstract: PIK3CA activating mutations are found in 40% of advanced breast cancer and are associated with worse prognosis. PI3K blockage is associated with insulin resistance, leading to hyperglycemia and hyperinsulinemia. Alpelisib is the first PI3K inhibitor used in cancer treatment. Laboratory evidence indicated that alpelisib-induced hyperinsulinemia offsets the drug’s efficacy, but insulin levels were not tested in the clinical trials that evaluated alpelisib for breast cancer. Hyperglycemia could also interfere with anti-tumor effects of PI3K inhibitors by inducing Immune tolerance and altered mitochondrial metabolism. We have monitored insulin levels in 4 breast cancer patients with concomitant metabolic syndrome treated with alpelisib, and pre-treated patients with baseline increased insulin levels with pioglitazone, a potent insulin sensitizer, to target both hyperinsulinemia and hyperglycemia, and we report the treatment course of these patients. All patients achieved glycemic control and were able to maintain alpelisib dose intensity. Duration of response to alpelisib was longer than anticipated in this treatment setting. Insulin dynamics confirmed the efficacy of pioglitazone as a specific on-target hypoglycemic and hypo-insulinemic agent in the unique setting of PI3K blockade. Our experience suggests that targeting hyperinsulinemia in patients with is safe and feasible and results in good metabolic and oncologic outcomes.
Keywords: alpelisib, hyperglycemia, insulin, pioglitazone, hyperinsulinemia, diabetes mellitus
Introduction
Alterations in the PI3K pathway are drivers in several types of cancer including breast cancer, colorectal cancer, endometrial cancer, prostate cancer, glioblastoma and other solid tumors.1 Drugs targeting this pathway are being developed and tested in different disease settings.2 Alpelisib is an oral PI3K inhibitor, active in patients with advanced ER positive HER2 negative breast cancer harboring a PIK3CA activating mutation in combination with fulvestrant,3 and is the first PI3K inhibitor that is used in routine clinical practice. However, since the PI3K pathway also mediates downstream effects of insulin, PI3K blockage is associated with insulin resistance, leading to hyperglycemia in most patients.3
Obesity, metabolic syndrome and diabetes mellitus increase the risk of breast cancer, other common cancers4 and cancer mortality.5 In patients treated for early-stage breast cancer, obesity and diabetes are associated with increased risk of recurrence.6 Insulin resistance, the hallmark of the metabolic syndrome and type 2 diabetes, results in hyperinsulinemia and elevated levels of IGF1, that result in enhanced signaling via the insulin receptor and IGF1-R. Activation of these receptors by increased levels and bioavailability of their ligands is one of the mechanisms linking the metabolic syndrome and breast cancer progression.7,8 IGF1R downstream effects include activating the PI3K pathway and transactivating the estrogen receptor.9 The mechanisms linking IGF1R with breast cancer initiation and progression are complex,7 however it has been shown that IGF1R activation10 is associated with breast cancer prognosis and that its sub-cellular localization to the nucleus to act as a transcription factor is an important mechanism of tumorigenesis.11 IGF1R is involved in cancer cell migration and invasion.12 Other mechanisms linking the insulin resistance and IGF1R activation with cancer, such as enhancement of epithelial–mesenchymal transition13 and stemness of breast cancer cells14 have also been suggested.
In a study with a mouse model of PIK3CA mutated breast cancer, hyperinsulinemia interfered with the therapeutic effects of alpelisib,15 while pharmacological suppression of hyperinsulinemia enhanced the efficacy of alpelisib. The association between hyperinsulinemia and alpelisib’s efficacy has not been tested in breast cancer patients.
Pioglitazone is a potent insulin sensitizer that reduces the risk of cardiovascular and hepatic complications of diabetes mellitus, with beneficial effects on blood pressure and serum lipids.16,17 Its use has declined during the last decades due to concerns regarding adverse events, specifically edema and increased fracture risk.18 Due to its insulin-sensitizing properties, pioglitazone might be beneficial for treatment of alpelisib-induced hyperglycemia, which is caused by insulin resistance. Pioglitazone is an inexpensive and easily available medication, and its adverse effects might be acceptable among patients with advanced cancer.
We describe the treatment course of 4 patients in whom insulin levels were monitored alongside glucose levels and pioglitazone was used to control hyperinsulinemia.
Patients and Methods
This report is based on a collaborative database of the Sheba and Galilee medical centers that included all consecutive patients who were treated with alpelisib for estrogen-receptor positive metastatic breast cancer during the years 2017–2020. We analyzed in detail the treatment course of 4 consecutive patients for whom insulin levels were monitored. The institutional ethical boards of both institutes approved the study.
Results
Patient 1
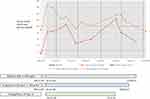
A 67-year-old female treated for metastatic estrogen receptor (ER) positive, HER2 negative breast cancer. Her cancer recurred with bone metastases 4 years after surgery for localized disease, during adjuvant aromatase inhibitor. Her medical history consisted of localized transitional cell carcinoma, which was excised and treated with BCG washes. Previous treatment lines included fulvestrant and a CDK 4/6 inhibitor for 4 months and capecitabine for 3 months. After progression on capecitabine, a PIK3CA mutation was detected, and treatments with Alpelisib 300 mg/d and exemestane 25 mg/d was initiated, with fexofenadine 180 mg once daily as skin rash prophylaxis. Metabolic background consisted of past gestational diabetes and obesity, with a body mass index (BMI) of 28.5 kg/m2. One week following treatment initiation her glucose levels rose to 400 mg/dL and insulin level was 265mU/l (upper normal range 25mU/l). Anti-diabetic treatment with empagliflozin 12.5 mg per day, metformin 850 mg twice daily and pioglitazone 30 mg once daily was initiated. In addition, to optimize glycemic control, the patient initiated a strict ketogenic diet. Subsequently, the patient developed a grade 3 maculopapular rash and treated with topical and systemic steroids and antihistamines. Alpelisib was halted for a week, during which her glucose had dropped to 154 mg/dL and insulin to 36 mU/l. Because of the delayed pharmacodynamics of pioglitazone, known to achieve maximal insulin-sensitizing effect after 5–6 weeks of treatment, it was administered continuously until treatment with alpelisib was resumed. Upon resolution of rash, alpelisib was resumed at 300 mg/d with the concomitant diabetic regimen. Four months later, significant improvement in the liver and bone lesions was noted on PET-CT scan. The patient continued treatment with blood glucose levels remaining stable around 150 mg/dl and insulin levels within normal range and without further significant adverse events. Response was maintained for 10 months, when progressive liver disease was diagnosed. Serum glucose and insulin dynamics over the time course of treatment with alpelisib are depicted in Figure 1, alongside a medication panel deploying chronologically administration of all agents affecting glycemic control.
Patient 2
A 64-year-old female was treated for ER positive, HER2 negative breast cancer metastatic to the liver. Her cancer recurred 8 years after completion of treatment for localized disease and she was treated with letrozole and a CDK 4/6 inhibitor for 4 years. Following disease progression, she received 3 additional lines of therapy. Genomic profiling of a biopsy from a liver metastasis detected an activating PIK3CA mutation and alpelisib with fulvestrant were started as her 5th treatment line.
Relevant medical history included overweight (BMI 28.5 kg/m2), impaired fasting glucose and past gestational diabetes, which indicated she had insulin resistance. To moderate hyperinsulinemia and hyperglycemia with alpelisib, she commenced treatment with Pioglitazone 30 mg/d a week prior to alpelisib initiation. In addition, she started a low-carbohydrate diet, aiming for consumption of 60–90 grams of carbohydrates per day. Alpelisib was initiated at a dose of 200 mg once daily with antihistamines as rash prophylaxis and gradually increased to 250 mg per day a week later. With this regimen, blood glucose and insulin levels were elevated to 170 mg/dl and 83mU/l respectively. At this point, empagliflozin, an SGLT2 inhibitor, at a dose of 10mg/d was added to her antidiabetic regimen. Three weeks later, blood glucose measurements declined to 110–130 mg/dl with parallel decrease in insulin levels to 43mU/l. Trajectories of glucose and insulin levels are depicted in Figure 2. Imaging studies showed a partial response, which was maintained for 5 months, after which her cancer progressed in the liver.
Patient 3
A 57-year-old female experienced metastatic recurrence of ER positive HER2 negative breast cancer, with bone and liver metastases, while on adjuvant exemestane. Her disease progressed four months after she began first-line fulvestrant and a CDK 4/6 inhibitor, and genomic studies revealed a PIK3CA mutation, thus alpelisib at a dose of 300 mg/d with letrozole 2.5 mg/d were initiated. Her past medical history was unremarkable. During the first two weeks of therapy, she developed a grade 2 rash that was successfully treated with oral prednisone and oral antihistamines, and alpelisib was continued at a reduced dose of 250 mg/day. Additionally, mild hyperglycemia of 135 mg/dl was documented, and she started taking 850 mg metformin once daily. Shortly thereafter, daily pioglitazone 30 mg/d was added to the regimen. Two months later, her fasting glucose levels were 120 mg/dl, post prandial glucose levels were 160 mg/dl and fasting insulin levels were slightly increased at 30 mU/l. Thus, pioglitazone dose was increased to 30 mg twice daily. Afterwards, blood glucose was well-controlled, and further anti-glycemic measures were not necessary. Seven months after treatment initiation, alpelisib dose was reduced to 200 mg/d due to grade 3 elevations in serum lipase levels. Imaging studies confirmed a partial response that was maintained for 1 year, when she experienced radiological progression of liver metastases and was taken off therapy.
Patient 4
A 64-year-old woman treated for ER positive, HER2 negative breast cancer with bone and liver metastases 7 years after completion of adjuvant therapy. Treatment lines included letrozole, fulvestrant and a CDK 4/6 inhibitor and capecitabine. Four years after diagnosis of metastatic disease, a PIK3CA mutation was detected.
Her metabolic background included obesity with a BMI of 36 kg/m2, diabetes mellitus controlled by diet with baseline fasting glucose 110 mg/dl, insulin levels 39 mU/l (upper normal range 25 mU/l) and hemoglobin A1c 5.9%. Pioglitazone 30 mg/d and metformin 850 mg once daily were initiated with fulvestrant and after 3 weeks alpelisib at a dose of 300 mg/d was added. Ten days later she developed a grade 3 rash and diarrhea treated with antihistamines and glucocorticoids.
After resolution of the rash, alpelisib was resumed at a dose of 200 mg/d, however fasting glucose levels rose to 180 mg/dl and insulin levels rose to 204 mU/l. Pioglitazone dose was increased to 45 mg/d, metformin increased to 850 mg X3/D and she was put on a low carbohydrate diet. PET scans performed 2 and 6 months after treatment initiation showed a partial response and she currently continues treatment.
Discussion
We present real-life experience of approaching alpelisib-induced hyperglycemia and hyperinsulinemia. Patients with prior metabolic syndrome are known to be at increased risk of severe hyperglycemia that may necessitate discontinuation of alpelisib19 and may become, in rare cases, life threatening.20 Moreover, the evidence from animal models regarding hyperinsulinemia potentially offsetting the efficacy of PI3K blockade15 suggests our treatment should target the efficacy aspect of hyperinsulinemia in addition to the safety aspect of hyperglycemia. We have endorsed a proactive approach towards minimizing hyperinsulinemia: preemptive metabolic screening is recommended to all patients prior to initiation of therapy, aiming to allocate patients who are prone to develop severe insulin resistance to proactive treatment and intense monitoring.
We chose to describe the treatment course of 4 patients for whom insulin levels were monitored meticulously and available for presentation. Three of these patients had prior metabolic syndrome or diabetes mellitus. All patients achieved glycemic control and were able to continue alpelisib and maintain dose intensity. Testing for insulin confirmed the efficacy of pioglitazone in reducing insulin levels, with full hypoglycemic effect expressed 5–6 weeks after initiation of therapy, correlating with its known effects.16 Thus, pioglitazone may be an optimal drug to treat alpelisib-induced hyperglycemia, and can be started several days before alpelisib in patients with metabolic risk factors, to minimize acute hyperglycemic events. Pioglitazone is an inexpensive drug, whose use declined due to concerns of increased risk of urinary tract malignancies, edema, and bone fragility. However, recent meta-analyses have shown that rates of urinary tract cancers are in fact unaffected by pioglitazone use21 and fracture risk increases only with prolonged use.18 Thus, it seems that its safety profile is acceptable in the setting of advanced breast cancer.
Our patients were treated in the 3rd, 4th and 5th line setting, and were pre-treated with a CDK 4/6 inhibitor. All had a partial treatment response which was maintained for 5–12 months, which is longer than reported in this population.22 Patient #1 had a very short PFS of 3–4 months on Fulvestrant and a CDK 4/6 inhibitor and a short PFS on chemotherapy as well, but nevertheless achieved a prolonged response to alpelisib, lasting 10 months. Patient #3 had a similar treatment course, with progression after 4 months from initiating fulvestrant and a CDK 4/6 inhibitor and a response to letrozole and alpelisib that lasted for 1 year. These favorable results might be explained by selection of highly motivated and compliant patients for monitoring insulin levels; however, the results of animal models suggest that controlling insulin levels supports to the anti-tumor effects of alpelisib15 and thus controlling hyperinsulinemia might have contributed to the beneficial oncological outcomes of our patients. A recent study suggested that hyperglycemia suppresses T cell anti- tumor effects23 and PI3K inhibition increased anti- tumor immune response in a study using mouse models of metastatic breast cancer.24 Recent evidence highlights the role of mitochondrial metabolism in tumor progression.25 PI3K signaling is central to mitochondrial upregulation, and PI3K pathway inhibition could inhibit mitochondrial function, leading to cancer growth arrest.26 It is thus plausible that immune activation and mitochondrial metabolism downregulation are additional mechanisms that contribute to the synergism between improved glycemic control and anti-tumor effects of alpelisib. Moreover, better glycemic control enables maintaining alpelisib dose intensity, which may also contribute to the beneficial oncological outcomes.
Our cohort is small, and data was retrospectively collected. However, addressing the management of the metabolic adverse events of PI3K inhibitors and of additional drugs targeting the PI3K pathway could become a pivotal issue in the fore coming years, since these agents are tested for the treatment of several malignancies. Our experience suggests that targeting hyperinsulinemia is feasible and associated with favorable metabolic and oncologic outcomes.
Conclusions
Our experience supports the approach of monitoring insulin levels in patients treated with alpelisib and aiming treatment to control both hyperglycemia and hyperinsulinemia. We suggest that pioglitazone be used as treatment for alpelisib-induced hyperglycemia not controlled by metformin. Patients with pre-existing metabolic syndrome or diabetes may benefit from pre-treatment with pioglitazone before starting alpelisib.
Data Sharing Statement
The datasets used and/or analyzed during the current study are available from Dr. Ruth Percik on reasonable request.
Ethics Approval
The protocol was approved by the Sheba Medical Center Institutional Review Board (SMC-21-8549) and by the Galilee Medical Center Institutional Review Board (NHR-21-0135). Patients gave their informed consent to publication of the cases.
Author Contributions
All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
This study was carried out without funding.
Disclosure
Dr Ayelet Shai reports personal fees from Novartis, during the conduct of the study; personal fees from Pfizer, outside the submitted work. The authors declare that they have no other competing interests.
References
1. Noorolyai S, Shajari N, Baghbani E, Sadreddini S, Baradaran B. The relation between PI3K/AKT signalling pathway and cancer. Gene. 2019;698:120–128. doi:10.1016/j.gene.2019.02.076
2. Mishra R, Patel H, Alanazi S, Kilroy MK, Garrett JT. PI3K inhibitors in cancer: clinical implications and adverse effects. Int J Mol Sci. 2021;22(7):3464. doi:10.3390/ijms22073464
3. André F, Ciruelos E, Rubovszky G, et al. Alpelisib for PIK3CA -mutated, hormone receptor–positive advanced breast cancer. N Engl J Med. 2019;380(20):1929–1940. doi:10.1056/NEJMoa1813904
4. Ballotari P, Vicentini M, Manicardi V, et al. Diabetes and risk of cancer incidence: results from a population-based cohort study in northern Italy. BMC Cancer. 2017;17(1):1–8. doi:10.1186/s12885-017-3696-4
5. Emerging Risk Factors Collaboration. Diabetes mellitus, fasting glucose, and risk of cause-specific death. N Engl J Med. 2011;364(9):829–841. doi:10.1056/NEJMoa1008862
6. Jiralerspong S, Kim ES, Dong W, Feng L, Hortobagyi GN, Giordano SH. Obesity, diabetes, and survival outcomes in a large cohort of early-stage breast cancer patients. Ann Oncol. 2013;24(10):2506–2514. doi:10.1093/annonc/mdt224
7. Lee J-S, Tocheny CE, Shaw LM. The insulin-like growth factor signaling pathway in breast cancer: an elusive therapeutic target. Life. 2022;12(12):1992. doi:10.3390/life12121992
8. Werner H, LeRoith D. Hallmarks of cancer: the insulin-like growth factors perspective. Front Oncol. 2022;12:1055589. doi:10.3389/fonc.2022.1055589
9. Farabaugh SM, Boone DN, Lee AV. Role of IGF1R in breast cancer subtypes, stemness, and lineage differentiation. Front Endocrinol. 2015;6(APR):1–12. doi:10.3389/fendo.2015.00059
10. Law JH, Habibi G, Hu K, et al. Phosphorylated insulin-like growth factor-i/insulin receptor is present in all breast cancer subtypes and is related to poor survival. Cancer Res. 2008;68(24):10238–10246. doi:10.1158/0008-5472.CAN-08-2755
11. Sarfstein R, Pasmanik-Chor M, Yeheskel A, et al. Insulin-like growth factor-I receptor (IGF-IR) translocates to nucleus and autoregulates IGF-IR gene expression in breast cancer cells. J Biol Chem. 2012;287(4):2766–2776. doi:10.1074/jbc.M111.281782
12. Guvakova MA, Adams JC, Boettiger D. Functional role of alpha-actinin, PI 3-kinase and MEK1/2 in insulin-like growth factor I receptor kinase regulated motility of human breast carcinoma cells. J Cell Sci. 2002;115(Pt 21):4149–4165. doi:10.1242/jcs.00104
13. Matà R, Palladino C, Nicolosi ML, et al. IGF-I induces upregulation of DDR1 collagen receptor in breast cancer cells by suppressing MIR-199a-5p through the PI3K/AKT pathway. Oncotarget. 2016;7(7):7683–7700. doi:10.18632/oncotarget.6524
14. Chang WW, Lin RJ, Yu J, et al. The expression and significance of insulin-like growth factor-1 receptor and its pathway on breast cancer stem/progenitors. Breast Cancer Res. 2013;15(3):R39. doi:10.1186/bcr3423
15. Hopkins BD, Pauli C, Xing D, et al. Suppression of insulin feedback enhances the efficacy of PI3K inhibitors. Nature. 2018;560(7719):499–503. doi:10.1038/s41586-018-0343-4
16. Miyazaki Y, Mahankali A, Matsuda M, et al. Improved glycemic control and enhanced insulin sensitivity in type 2 diabetic subjects treated with pioglitazone. Diabetes Care. 2001;24(4):710–719. doi:10.2337/diacare.24.4.710
17. DeFronzo RA, Inzucchi S, Abdul-Ghani M, Nissen SE. Pioglitazone: the forgotten, cost-effective cardioprotective drug for type 2 diabetes. Diabetes Vasc Dis Res. 2019;16(2):133–143. doi:10.1177/1479164118825376
18. Bazelier MT, de Vries F, Vestergaard P, et al. Risk of fracture with thiazolidinediones: an individual patient data meta-analysis. Front Endocrinol. 2013;4(FEB):1–9.
19. Rugo HS, André F, Yamashita T, et al. Time course and management of key adverse events during the randomized Phase III SOLAR-1 study of PI3K inhibitor alpelisib plus fulvestrant in patients with HR-positive advanced breast cancer. Ann Oncol. 2020;31(8):1001–1010. doi:10.1016/j.annonc.2020.05.001
20. Carrillo M, Rodriguez RM, Walsh CL, Mcgarvey M. Alpelisib-induced diabetic ketoacidosis: a case report and review of literature. AACE Clin Case Rep. 2021;7(2):127–131. doi:10.1016/j.aace.2020.11.028
21. Filipova E, Uzunova K, Kalinov K, Vekov T. Pioglitazone and the risk of bladder cancer: a meta-analysis. Diabetes Ther. 2017;8(4):705–726. doi:10.1007/s13300-017-0273-4
22. Rugo HS, Lerebours F, Ciruelos E, et al. Alpelisib plus fulvestrant in PIK3CA-mutated, hormone receptor-positive advanced breast cancer after a CDK4/6 inhibitor (BYLieve): one cohort of a Phase 2, multicentre, open-label, non-comparative study. Lancet Oncol. 2021;22(4):489–498. doi:10.1016/S1470-2045(21)00034-6
23. Mu X, Xiang Z, Xu Y, et al. Glucose metabolism controls human γδ T-cell-mediated tumor immunosurveillance in diabetes. Cell Mol Immunol. 2022;19(8):944–956. doi:10.1038/s41423-022-00894-x
24. Sai J, Owens P, Novitskiy SV, et al. PI3K inhibition reduces mammary tumor growth and facilitates antitumor immunity and anti-PD1 responses. Clin Cancer Res. 2017;23(13):3371–3384. doi:10.1158/1078-0432.CCR-16-2142
25. Taghizadeh-Hesary F, Akbari H, Bahadori M, Behnam B. Targeted anti-mitochondrial therapy: the future of oncology. Genes. 2022;13(10):1728. doi:10.3390/genes13101728
26. Gao M, Wang J, Wang W, Liu J, Wong C-W. Phosphatidylinositol 3-kinase affects mitochondrial function in part through inducing peroxisome proliferator-activated receptor γ coactivator-1β expression. Br J Pharmacol. 2011;162(4):1000–1008. doi:10.1111/j.1476-5381.2010.01105.x
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.