Back to Journals » Cancer Management and Research » Volume 14
The Potential Role of Genomic Signature in Stage II Relapsed Colorectal Cancer (CRC) Patients: A Mono-Institutional Study
Authors Roberto M, Arrivi G, Pilozzi E, Montori A, Balducci G, Mercantini P, Laghi A, Ierinò D, Panebianco M, Marinelli D, Tomao S, Marchetti P, Mazzuca F
Received 22 December 2021
Accepted for publication 21 February 2022
Published 7 April 2022 Volume 2022:14 Pages 1353—1369
DOI https://doi.org/10.2147/CMAR.S342612
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Harikrishna Nakshatri
Michela Roberto,1 Giulia Arrivi,2 Emanuela Pilozzi,3 Andrea Montori,3 Genoveffa Balducci,4 Paolo Mercantini,4 Andrea Laghi,5 Debora Ierinò,2 Martina Panebianco,2 Daniele Marinelli,6 Silverio Tomao,1 Paolo Marchetti,2 Federica Mazzuca2
1Department of Radiological, Oncological and Anatomo-Pathological Sciences, Medical Oncology Unit A, Policlinico Umberto I, “Sapienza” University of Rome, Rome, Italy; 2Department of Clinical and Molecular Medicine, Sapienza University of Rome, Oncology Unit, Sant’ Andrea University Hospital, Rome, Italy; 3Department of Clinical and Molecular Medicine, Sapienza University of Rome, Anatomia Patologica Unit, Sant’ Andrea University Hospital, Rome, Italy; 4Department of Medical-Surgical Sciences and Translation Medicine, Sapienza University of Rome, Gastro-intestinal Surgery Unit, Sant’ Andrea University Hospital, Rome, Italy; 5Department of Medical-Surgical Sciences and Translation Medicine, Sapienza University of Rome, Radiology Unit, Sant’ Andrea University Hospital, Rome, Italy; 6Medical Oncology Unit B, Policlinico Umberto I, Sapienza University, Rome, Italy
Correspondence: Giulia Arrivi, Department of Clinical and Molecular Medicine, Sapienza University of Rome, Oncology Unit, Sant’ Andrea University Hospital, Via di Grottarossa 1035-1039, Rome, 00189, Italy, Tel +39 3387231524, Fax +39 0633776629, Email [email protected]
Purpose: The absolute benefit of adjuvant chemotherapy in stage II CRC is only 3– 4%. The identification of biomarkers through molecular profiling could identify patients who will more benefit from adjuvant chemotherapy.
Patients and Methods: This retrospective analysis examined tissue blocks from 17 patients affected by relapsed stage II CRC, whose comprehensive genomic profiling of tumors was conducted through next-generation sequencing (NGS) via Roche-FoundationOne®.
Results: Mutations were found in APC (76.5%), TP53 (58.8%) and KRAS (52.9%). Only KRAS wild-type samples showed FBXW7. APC frameshift mutations and MLH1 splice variant were conversely significant correlated (7% v 93%, P = 0.014). The median number of gene mutations reported was 6 (range 2– 14). The TP53 mutation was associated most frequently with lung metastasis (P = 0.07) and high tumor budding (P = 0.03). Despite no statistical significance, lung recurrence, LVI/Pni, MSI and more than 6 genetic mutations were correlated to worse DFS and OS. Patients carried co-mutations of TP53-FBXW7 reported the worse DFS (4 v 14 months) and OS (4 v 65 months) compared to the other patients.
Conclusion: According to the present analysis, the setting of relapsed CRC emerges as one of the fields of greatest utility for NGS, looking at personalized cancer care.
Keywords: next-generation sequencing, NGS, colon cancer, stage II, biomarkers
Introduction
Colorectal tumorigenesis is a multistep process that involves an accumulation of multiple, successive genetic alterations like chromosomal abnormalities, gene mutations, and epigenetic changes, that induces neoplastic transformation of the colic epithelium.1 The most commonly genetic aberrations in colorectal cancer (CRC) are reported in APC (Adenomatous Polyposis Coli), TP53, RAS (rat sarcoma viral oncogene homolog) and PIK3CA (Phosphatidylinositol-4,5-bisphosphate 3-kinase catalytic subunit alpha) genes.2–6 Some of these alterations, whose prognostic and predictive role is well established, are routinely used to make personalized treatment decisions in CRC.7
Approximately 80% of CRC presents as a localized or regional disease at diagnosis, but 35% of these patients develop a disease relapse, which in most cases (80%) occurs within the first 3 years of surgery.8 The use of adjuvant chemotherapy, of which fluoropyrimidines are still the backbone, is associated with reduction of recurrence in 25% of patients with stage III CRC;9 while the absolute benefit in stage II CRC is only 3–4%.10–12 In retrospective analyses, different genes were involved in the prognosis and prediction of response to chemotherapy in early-stage CRC, especially KRAS, BRAF, PIK3CA and p53.13–19 A recent analysis of 130 patients with stage II–III CRC revealed that TYMS/KRAS/BRAF molecular profiling predicts survival after adjuvant chemotherapy.20 The loss of heterozygosity at the TYMS locus on chromosome 18 showed a role in the genesis of resistance to fluoropyrimidine-based therapy.21 APC mutations, associated with poor prognosis in 5-fluorouracil treated stage III colon cancers, have shown no correlation with disease-free survival in stage II colon cancers.22 A role of the axis fibroblast growth factor 1/fibroblast growth factor receptor 3 (FGF1/FGFR-3) and overexpression of FGFR was recognized in tumour growth and metastatization.23,24 Negative prognostic characteristics like right-sided tumors, microsatellite instability, BRAF mutations, lymph node metastases, and a higher tumor stage seem to be more frequently correlated with PTEN alterations that may lead to poor prognosis.25,26 The predictive and prognostic role of PI3K/AKT pathway27,28 and ERBB4 gene29–31 in CRC is still debated. In this complex context, the identification of biomarkers through extensive molecular profiling of stage II CRC could provide more information about diagnosis, prognosis, but especially to identify those patients who will receive more benefit from 5-Fluorouracil (5FU)-based adjuvant chemotherapy.
On this basis, the aim of our study was to investigate comprehensive genomic profile of relapsed stage II CRC patients treated at our hospital. The secondary aim was to evaluate the possible association between these molecular alterations in respect to both survival outcomes and clinicopathological characteristics.
Materials and Methods
Study Design
This is a mono-institutional retrospective analysis that has examined formalin-fixed paraffin-embedded (FFPE) tissue blocks retrieved from surgical resection, from patients affected by r stage II CRC, who underwent surgery at Sant’ Andrea Hospital in Rome from 2009 to 2015 and whose comprehensive genomic profiling of tumors was conducted through next-generation sequencing (NGS) via FoundationOne®.32,33 The study enrolled 17 patients, who reported a relapse of disease, out of those 174 patients included in a previous analysis of stage II CRC34 (Figure 1). Out of those 17 patients, 6 were affected by stage II CRC high risk according to NCCN guidelines definition.35 All patients included in our study received follow up in our center, six of these received also adjuvant 5-fluorouracil-based chemotherapy due to the high risk of the tumor. Patient demographics and clinical characteristics were also examined.
 |
Figure 1 CONSORT 2010 flow diagram. |
To compare our results with validate literature data, we assumed data from cBioPortal for Cancer Genomics, that converts molecular profiling data from cancer tissues and cell lines in-to highly accessible genetic, epigenetic, gene expression, and proteomic events (https://www.cbioportal.org). Oncoprints (Figures 2–4) show mutational frequency of selected genes on The Cancer Genome Atlas colon adenocarcinoma (COAD TCGA) Cohorts, respectively in all population stage II CRCs, non-recurred and recurred CRCs. The first objective of our study was to explore genetic mutations, amplifications, or alterations in patients with relapsed stage II CRC. The secondary objectives were to correlate genomic profile to survival outcomes and clinicopathological characteristics.
 |
Figure 2 The Cancer Genome Atlas Colon Adenocarcinoma Cohorts (TCGA COAD) stage II CRCs. |
 |
Figure 3 The Cancer Genome Atlas Colon Adenocarcinoma Cohorts (TCGA COAD) stage II non recurred CRCs. |
 |
Figure 4 The Cancer Genome Atlas Colon Adenocarcinoma Cohorts (TCGA COAD) stage II recurred CRCs. |
All patients signed an informed consent for scientific research purpose at the first oncological visit. The study was conducted in accordance with the Declaration of Helsinki and the protocol approved by the institutional (Sant’ Andrea Hospital, Sapienza University) ethical committee (N.3874_2015).
Determination of Gene Mutations/Next Generation Sequencing
Comprehensive genomic profiling was performed on DNA extracted from 17 formalin-fixed paraffin-embedded (FFPE) tissue sections from one block representative of the tumor using the FoundationOne (Foundation Medicine, Cambridge, USA). Foundation Medicine is a next-generation sequencing based in vitro diagnostic test that uses targeted high throughput hybridization-based capture technology for detection of substitutions, insertion and deletion alterations, and copy number alterations in 315 cancer-related genes plus introns from 28 genes often rearranged or altered in solid tumors. Furthermore, the assay provides information about Microsatellite status and tumor mutation burden (https://www.foundationmedicine.com). All NGS-results are also listed in Supplementary Table. The gene panel list is listed in Supplementary Table.
Statistical Analysis
Patient characteristics and gene mutation frequencies were described using descriptive analysis. Data are presented as number, number and percentage, or median and range. Pearson’s χ2 test or Fisher’s exact test was used to evaluate associations between TP53, KRAS, PIK3CA, and FBXW7 mutations, and dMMR, CDX2, tumor budding and other clinicopathologic variables such us sidedness of primary tumor (right vs left), sites of metastases. Kaplan-Meier method was used for survival analysis. Correlation between clinicopathological characteristics and survival was done by Cox regression. Statistical calculations were performed using SPSS Statistics version 24 (SPSS, Inc., Chicago, IL, USA). P-values less than 0.05 were considered statistically significant.
Results
Clinicopathological Characteristics
A total of 174 consecutive patients with stage II colon cancer were screened, and those 17 (10%) patients with a relapse of disease within the first 5 years of follow up for colon cancer, were included in this study. Tissue blocks of primary tumor were available for all included patients. The median age of subjects was 71 years (range:43–84), most of them (14, 82%) were male, and affected with right-side colon cancer rather than left-side colon cancer (71% and 29%, respectively). Fourteen (82%) tumors were pT3, and only one case reported <12 lymph-nodes retrieval. The majority of cases were moderately differentiated tumors (65%), without lymphovascular invasion (67%) and with a low stage risk according to international clinical guidelines (65% and 35% was low and high stage risk, respectively). Out of 1 patient who reported a local recurrence, 15 patients experienced a distant recurrence, especially in liver (35%) and lung (35%). Other patient and tumor characteristics are summarized in Table 1.
 |
Table 1 Clinicopathologic Features of Patients |
Comparison with Clinical Factors
NGS analysis was carried out in all patients and median exon coverage is >500x for all samples. All NGS-results are also listed in Supplementary Table. Genomic profile was different and heterogenous among the study patients (Table 2). Most of the patients reported mutations in the following genes: APC (76.5%), TP53 (58.8%) and KRAS (52.9%). Gene mutations frequency was represented in Figure 2. Among the KRAS gene mutations, 8 (88%) had mutation in exon 2 (G12D, G13D), 1 (12%) in exon 3 (K117N). PIK3CA mutations were identified in 5 (29.4%) tumors. All of these had mutation in exon 9 (E545K, E542Q, R88Q, and R849*). FBXW7 as well as MLH1 were both reported in 3 cases (17.6%). FBXW7 were found only in KRAS wild-type samples. MLH1 splice variant and APC frameshift mutations were conversely significant reported (7% v 93%, P = 0.014). No other significant relationship was found. However, TP53-KRAS, TP53-PIK3CA and TP53-FBXW7 mutations were co-occurrent in 5 (29%), 3 (18%) and 2 (12%) patients, respectively. Only 1 patient carried KRAS-PIK3CA co-mutations.
 |
Table 2 Genomic Profile and Clinicopathological Characteristics of Relapsed CRC Patients |
Additional mutations were also detected in 11.8% of cases (ARID2, BRAF, CIC, KMT2C (MLL3), LRP1B, NRAS, PTEN, RNF43, SMAD4 and SOX9TNNB1, NRAS, and SMAD4) and other 42 genes at lesser frequency. Overall, the median number of gene mutations reported was 6 (range 2–14).
Patients who carried a TP53 mutation, developed disease recurrence more frequently in the lung than liver or other metastatic sites. (55% v 27% v 18%, P = 0.07). No other significant correlation was found between genetic mutations and clinicopathological factors.
In order to integrate the gene mutations panel with the potential molecular and biological consequences involved in CRC relapse, we performed a STRING network analysis. STRING is a database of known and predicted protein-protein interactions that includes direct and indirect associations.36 We included in STRING analysis, both genes that presented mutation incidence > 18% in our analysis - APC, TP53, KRAS, PIK3CA, FBXW7, MLH1 – (Figure 5), and the others most important genes involved in colorectal cancer process including BRAF and NRAS. On the basis of this analysis, we can hypothesize that other gene mutations in addition to those we usually use in CRC management (KRAS, NRAS, BRAF), could figure out as novel target to improve the landscape of relapsed CRC treatment (Figure 6). These possible future targets are represented by genes involved in mechanisms of cellular senescence and aging, immune response, intracellular signal transduction mediated by members of the RAS superfamily of proteins. Several are the evidence of a role of tumor microenvironment in treatment response and relapse such us the interplay between cancer cells and cancer-associated fibroblasts (CAFs) that has been proven to promote colorectal carcinogenesis.
 |
Figure 5 Frequency and representation of gene mutations in cohort study. Vertical axis: frequency of mutations. Horizontal axis: genes. |
Prevalence of dMMR/MSI-H, CDX2 and Tumor Budding
Microsatellite instability was reported in 4 (18%) patients, 3 (67%) of whom carrying MLH1 mutation. Only 1 patient was CDX2 negative. This single patient was carrier of FBXW7 mutation (P = 0.02) Tumor budding was equally represented: high and low was both reported in 8 (50%) patients, and it was not examined in 1 case. Tumor budding high was frequently associated with TP53 mutation (88% v 12%, P= 0.03). Contrary, MLH1 mutation was present only in samples with tumor budding low (P = 0.05). Accordingly, tumor budding high was not reported in MSI tumors (P = 0.05).
Survival Analysis
With a median follow up of 53 months (range 4–107), median DFS and OS were 14 and 65 months, respectively. None of variables analyzed were significantly associated to survival. However, patients with high stage risk, lung recurrence, pT4 tumor, LVI/Pni, MSI, FBXW7 mutant carriers and with more than 6 genetic mutations showed the worse DFS (Table 3). Patients with age >70, right colon cancer, lung recurrence, LVI/Pni, grade G3, MSI, carriers of PIK3CA, FBXW7 or MLH1 mutations and with more than 6 genetic mutations showed the worse OS. Moreover, patients carried co-mutations of TP53-FBXW7 reported the worse DFS and OS compared to the other patients studied (DFS: 4 v 14 months; DFS: 4 v 65 months).
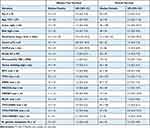 |
Table 3 Univariate Analysis for Disease Free Survival (DFS) and Overall Survival (OS) |
Discussion
Stage II CRC is characterized by a good prognosis, with 5-year overall survival of 70–80% after surgery;37 but about 20% of these patients develop a tumor relapse.10,38 The adjunct of a 5-fluorouracil-based adjuvant chemotherapy provide an absolute benefit of 3–4% only10–12,39 and the current international clinical guidelines (https://www.nccn.org/professionals/physician_gls/pdf/colon.pdf) seems to be insufficient to identify the “real” high risk stage II CRC. The identification of biomarkers through molecular profiling of tumors, could help clinicians mostly to identify those patients who will receive more benefit from adjuvant chemotherapy. With this aim, we conducted a mono-institutional retrospective analysis of 174 patients affected by stage II CRC who underwent surgery at Sant’ Andrea Hospital. We enrolled only those seventeen (10%) patients who reported a relapse of disease, whose comprehensive genomic profiling of tumor through NGS (FoundationOne®) was conducted. The possible association in respect to clinicopathological characteristics and survival outcomes was explored.
According to literature data the recurrence rate of our population was about 10%.8 Lymphovascular and perineural invasion by cancer cells, although very promising as prognostic variables, have proved difficult to standardize due to technical problems inherent in the visual analysis and the subjective definition of these features.40 Nevertheless, there are data in literature about association between poor histological differentiation and advanced T stage and the presence of lymph node involvement:41 according to this knowledge, the pathological characteristics of stage II CRC of our study, showed that 65% of cases were moderately differentiated tumors, and 33% showed lymphovascular invasion.
Six patients received adjuvant 5-fluorouracil-based chemotherapy in relation to the risk. As previously reported, stage II CRC receive a small benefit with adjuvant chemotherapy in QUASAR trial32 and in the MOSAIC trial, there was no difference in DFS in stage II patients who received chemotherapy and those who did not.42 Nowadays, guidelines recommended adjuvant chemotherapy in “high-risk” stage II patients, which include (exclusive for those cancer that are MSI-H) poorly differentiated/undifferentiated histology, lymphatic/vascular invasion, bowel obstruction, <12 lymph node sampling, peri-neural invasion, perforation, or positive margins (https://www.nccn.org/professionals/physician_gls/pdf/colon.pdf).
In literature, there is the evidence of a predictive value of several mutant genes, but most previous studies combined all stages of CRC.43 With the aim of clarifying the molecular effects, we conducted a study only in relapsed stage II CRC, with the small sample size limitation, compared to more than 300 genes explored by NGS.
Complete spectrum of gene mutations is represented in Supplementary Table and their percentages distribution in our cohort of patients in Figure 2. The most of mutations involves genes whose prognostic and predictive role is widely reported in the literature:13,14,17,18 76.5% of our patients showed APC mutations, 58.8% TP53, 52.9% KRAS and 29.4% PIK3CA. The involving of these genes is in line with the Cancer Genome Atlas colon adenocarcinoma (TCGA COAD) cohort. Mutations in APC, a tumor suppressor gene with an important role in the WNT signaling pathway, intercellular adhesion, cytoskeleton stabilization, cell cycle regulation, and apoptosis,44–48 appear to play a role in promoting tumorigenesis;49,50 while mutations of p53 tumor suppressor gene are among the commonest genetic alterations in all cancers. As we know KRAS and BRAF mutations, especially for left-sided and rectal tumors were associated with poor prognosis13–16 while PIK3CA mutations was associated with increased risk of local recurrence.17
FBXW7 is a critical tumor suppressor gene that encodes the substrate recognition components of SKP1-Cullin1-F-box protein ubiquitin E3 ligase complexes,51,52 that negatively regulate the intracellular abundance of various key oncogenic proteins. Therefore, the loss of FBXW7 function results in accumulation of its substrates, which leads to oncogenesis and progression of multiple cancers, including CRC.53 Clinical studies reported that the low expression level of FBXW7 was related to a poor prognosis.54,55 The frequency of this alterations (17.6%) in our study is slightly higher than the previously reported rates.56–59 Noteworthy, we found FBXW7 mutations only in KRAS wild-type samples while in previous reports KRAS was frequently found as a concomitant mutation, especially in patients with colorectal cancer (until 86%).60,61
About co-occurring mutations, we reported TP53-PIK3CA, TP53-FBXW7 and TP53-KRAS in 3 (18%), 2 (12%) and 5 (29%) patients, respectively. The last one is an uncommon combination: TP53 and KRAS mutations were rarely found together in the same tumor, suggesting different genetic pathways leading to tumor formation. The low number of tumors containing mutations in both genes could suggest that this phenotype may have arisen by chance.62,63 Indeed, we excluded by our analysis, patients with familiar history of CRC. Moreover, co-altered RAS/BRAF/TP53 resulted as an independent factor for mortality and was associated with worse OS in patients with liver and lung metastases. These tumors were significantly more likely to involve extrahepatic metastatic sites:64 to confirm this, four of our five total patients harboring this co-alteration, have metastasized in lung (3 patients) and abdominal wall (1 patient), although no significant correlation was found between these genetic mutations and clinicopathological factors.
An early event in colorectal carcinogenesis65,66 is the promoter hypermethylation of the mismatch repair gene Human Mut-L Homologue 1 (MLH1), frequently associated with microsatellite instability and BRAF mutations in CRC.67–71 Previous studies observed that microsatellite instable tumors may harbor less aberrations in KRAS, TP53 or APC, suggesting that these tumors develop through a distinct pathway.72–75 Vogel et al76 confirmed that MLH1 hypermethylation was less common in tumors with APC mutations or KRAS mutations; and our data showed that MLH1 splice variant and APC frameshift mutations were conversely significant correlated (7% v 93%). Instead, microsatellite instability was reported in 4 (18%) patients, 3 (67%) of whom carrying MLH1 mutation. This is in line with the observed high correlation between MLH1 methylation and microsatellite instability in the colorectum68–70 and its inverse relationship with mutations in other key genes involved in colorectal carcinogenesis.72–75
The idea that the tumor biology and key mutations might differ between various sites of metastatic manifestation is well established:77 p53 mutations promoted CRC metastasis, including lymphatic and distant metastases, in European and American populations.78 A complete mutational status of CRC lung metastases and corresponding primary tumors by NGS, with a concordance of 83.5%, founded mutations in TP53 in 57.4% of both primary tumors and corresponding lung metastasis.79 In our work patients who carried a TP53 mutation, developed disease recurrence more frequently in the lung (55% v 27 v 18, P = 0.07).
In addition to the effects of single gene mutations, the median number of gene mutations, which we know to be related with the stage,80 was also evaluated, and we reported a median number of 6 mutations (range 2–14) in our population.
Previous studies indicated that CDX2 negative tumors are often associated with several adverse prognostic variables such as advanced stage, poor differentiation, vascular invasion, BRAF mutation, and CIMP-positive status.81–84 Loss of CDX2 expression has been reported in several colorectal cancers and cancer cell lines with a potential inverse correlation between CDX2 levels and tumor stage;85 actually, the combination of the T stage with the CDX2 expression status seems to have better prognostic prediction value in CRC from stage I to stage III.86 Only one patient affected by stage II CRC was CDX2 negative, moreover was carrier of FBXW7 mutation (P = 0.02) and MSI. These reports indicated the involvement of FBXW7 in the development and regulation of cellular differentiation by targeting multiple substrates for degradation and can be explained by the FBXW7-mediated inhibition of CDX2 expression, that also could lead to reduced CDX2 transactivation and growth arrest of colon cancer cells.85 Indeed, overexpression of FBXW7 in colon cancer cells led to a reduction of CDX2 protein levels.
MSI-H, common among stage II (20%) and III (12%)87 confers a favorable prognosis in patients with localized disease88,89 and results associated with CDX2 negative status (P < 0.001) and vice versa.34
In MSI patients, tumor budding high was not reported (P = 0.05) and accordingly MLH1 mutation was present only in samples with tumor budding low (P = 0.05). Tumors with high-level MSI, seem to have very low rates or no tumor budding:90 indeed, the invasive front of colorectal cancers can be thought as a dynamic interface of pro- and anti- tumor factors composed primarily of cytotoxic T lymphocytes, to protect vascular and lymphatic channels from invasion by tumor buds91 and MSI-H colorectal cancers exemplify this attacker/defender model and highlight a pro-immunogenic phenotype.92 Accordingly, in the study by Romiti et al, only 16% of populations with high tumor budding presented microsatellite instability.34
With a median follow up of 53 months (range 4–107), median DFS and OS were 14 and 65 months, respectively. Despite none of variables analyzed resulted significantly correlated to survival, patients with high stage risk, lung recurrence, pT4 tumor, LVI/Pni, MSI, FBXW7 mutant carriers showed worse DFS. (Table 3) Many of these features are reported in literature as prognostic factors in term of recurrence after surgery.93–96 Perineural invasion, because of its correlation with depth of tumor invasion and lymphovascular invasion, was defined as a prognostic factor for the survival of patients with stage II CRC.97 In a recent work by Shinto et al98 pT4 appeared as an independent poor prognostic factor, specifically in stage II CRC. The substantiation of MSI status determination in stage II CRC patients may be controversial: on one side we have NCCN recommendations, but on the other side we should consider the results of the meta-analysis by Des Guetz et al99 that observed no statistically significant difference in patient survival in terms of Regression-Free Survival or OS irrespective of adjuvant chemotherapy implementation for the MSI-H patients.
In terms of OS, worse outcome was demonstrated by patients harboring these characteristics: age >70, right colon cancer, lung recurrence, LVI/Pni, grade G3, MSI, carriers of PIK3CA, FBXW7 or MLH1 mutations. In patients with pulmonary metastasis, the frequency of KRAS mutations was significantly higher,100 along with those of APC and TP53,101 mutations that we could define as signatures associated with poor prognosis. As reported above, the role of the MSI status as a predictive marker remains controversial,102 so this molecular signature could allow for stage II dismemberment, more precisely identifying patients at high and low risk of relapse.
A retrospective analysis of 93 CRC cases has showed in patients with low FBXW7 expression, a worse 5‐year OS than those in the high expression group, to demonstrate the prognostic role of FBXW7.47 Furthermore, FBXW7 missense mutations are associated with PIK3CA mutations and with a shorter OS.52 Loss of function of this gene seems to be implicated in anti-EGFR resistance,103 in increased resistance to paclitaxel,104 regorafenib,105 5-fluorouracil,106 or oxaliplatin.107 This implication of FBXW7 status in chemoresistance, could suggest the potential of FBXW7-targeted therapy, as demonstrated in other field of tumor disease.108
Patients with more than 6 genetic mutations and carried co-mutations of TP53-FBXW7 reported the worse DFS and OS compared to the other patients studied. Co-deletion of both FBXW7 and p53 causes highly penetrant, aggressive, and metastatic adenocarcinomas that frequently metastasized to lymph nodes and liver and often exhibited chromosomal instability,109 (Supplementary Figures 1 and 2).
There are several limitations to this study. First, the retrospective nature of this analysis, the small sample size of our populations and the lack of a control group of patients affected by stage II CRC not relapsed. Furthermore, NGS was conducted only in formalin-fixed paraffin-embedded (FFPE) tissue blocks retrieved from surgical resection; we did not provide a complete mutational status of corresponding metastases however in colon cancer the concordance between primary tumors and metastases was near to 90%.64 Nevertheless, we recognize that the characteristics of our study do not allow to draw strict conclusion, but we can make speculative assessments about gene mutations involved in relapse of CRC. Our study showed how targeting specific molecular pathways and gene mutations has become a critical step in improving treatment options and increasing patient survival. Hence, the use of NGS in relapsed CRC should be widespread in clinical practice since the early stage of disease.
Conclusion
Our retrospective work supports a deep molecular characterization of stage II CRC as a key element for optimal patient’s management. Uniform guidelines to detect and classify variants, to interpret and report results should be recommended and adopted.110 According to our analysis, the setting of relapsed CRC emerges like one of the fields of greatest utility for NGS, in clinical practice. Although the clinical implications of many genetic aberrations in CRC are still unclear, despite the extensive scientific research that has been conducted, the aim of this study is to emphasize the inclusion of genomic data into daily patient care and clinical guidelines. However, further researches are required to clarify the methodology to identify novel and reliable biomarkers and to help clinicians in treatment decisions in early stage CRC.
Disclosure
Prof. Dr. Andrea Laghi reports speaker’s fee from Bracco, from Bayer, from GE Healthcare, and from Guerbet, outside the submitted work. Prof. Dr. Paolo Marchetti reports grants, personal fees from ROCHE, grants, personal fees from MSD, grants, personal fees from BMS, grants from ASTRA ZENECA, grants from BOEHRINGER INGELHEIM, personal fees from LILLY, grants, personal fees from NOVARTIS, grants, personal fees from PFIZER, outside the submitted work. The authors report no other conflicts of interest in this work.
References
1. Vogelstein B, Fearon ER, Hamilton SR, et al. Genetic alterations during colorectal-tumor development. N Engl J Med. 1988;319:525–532. doi:10.1056/NEJM198809013190901
2. Dinu D, Dobre M, Panaitescu E, et al. Prognostic significance of KRAS gene mutations in colorectal cancer–preliminary study. J Med Life. 2014;7(4):581–587.
3. Davies H, Bignell GR, Cox C, et al. Mutations of the BRAF gene in human cancer. Nature. 2002;417(6892):949–954. doi:10.1038/nature00766
4. Cathomas G. PIK3CA in Colorectal Cancer. Front Oncol. 2014;4:35. doi:10.3389/fonc.2014.00035
5. Soussi T, Béroud C. Significance of TP53 mutations in human cancer: a critical analysis of mutations at CpG dinucleotides. Hum Mutat. 2003;21(3):192–200. doi:10.1002/humu.10189
6. Smith G, Carey FA, Beattie J, et al. Mutations in APC, Kirsten-ras, and p53–alternative genetic pathways to colorectal cancer. Proc Natl Acad Sci U S A. 2002;99(14):9433–9438.
7. Therkildsen C, Bergmann TK, Henrichsen-Schnack T, Ladelund S, Nilbert M. The predictive value of KRAS, NRAS, BRAF, PIK3CA and PTEN for anti-EGFR treatment in metastatic colorectal cancer: a systematic review and meta-analysis. Acta Oncol. 2014;53(7):852–864. doi:10.3109/0284186X.2014.895036
8. Sargent D, Sobrero A, Grothey A, et al. Evidence for cure by adjuvant therapy in colon cancer: observations based on individual patient data from 20,898 patients on 18 randomized trials. J Clin Oncol. 2009;27(6):872–877. doi:10.1200/JCO.2008.19.5362
9. Longley DB, Harkin DP, Johnston PG. 5-Fluorouracil: mechanisms of action and clinical strategies. Nat Rev Cancer. 2003;3(5):330–338. doi:10.1038/nrc1074
10. Benson AB, Schrag D, Somerfield MR, et al. American society of clinical oncology recommendations on adjuvant chemotherapy for Stage II colon cancer. J Clin Oncol. 2004;22(16):3408–3419. doi:10.1200/JCO.2004.05.063
11. Köhne CH. Should adjuvant chemotherapy become standard treatment for patients with Stage II colon cancer? Against the proposal. Lancet Oncol. 2006;7(6):516–517.
12. Sobrero A, Köhne CH. Should adjuvant chemotherapy become standard treatment for patients with Stage II colon cancer? Lancet Oncol. 2006;7(6):515–516. doi:10.1016/S1470-2045(06)70727-6
13. Hutchins G, Southward K, Handley K, et al. Value of mismatch repair, KRAS, and BRAF mutations in predicting recurrence and benefits from chemotherapy in colorectal cancer. J Clin Oncol. 2011;29(10):1261–1270. doi:10.1200/JCO.2010.30.1366
14. Sinicrope FA, Mahoney MR, Yoon HH, et al. Analysis of molecular markers by anatomic tumor site in Stage III colon carcinomas from adjuvant chemotherapy trial NCCTG N0147 (Alliance). Clin Cancer Res. 2015;21(23):5294–5304. doi:10.1158/1078-0432.CCR-15-0527
15. Sinicrope FA, Mahoney MR, Smyrk TC, et al. Prognostic impact of deficient DNA mismatch repair in patients with Stage III colon cancer from a randomized trial of FOLFOX-based adjuvant chemotherapy. I J Clin Oncol. 2013;31(29):3664–3672. doi:10.1200/JCO.2013.48.9591
16. Taieb J, Le Malicot K, Shi Q, et al. Prognostic value of BRAF and KRAS mutations in MSI and MSS Stage III colon cancer. J Natl Cancer Inst. 2016;109(5):djw272. doi:10.1093/jnci/djw272
17. He Y, Van’t Veer LJ, Mikolajewska-Hanclich I, et al. PIK3CA mutations predict local recurrences in rectal cancer patients. Clin Cancer Res. 2009;15(22):6956–6962. doi:10.1158/1078-0432.CCR-09-1165
18. Oh HJ, Bae JM, Wen X, et al. P53 expression status is associated with cancer-specific survival in Stage III and high-risk Stage II colorectal cancer patients treated with oxaliplatin-based adjuvant chemotherapy. Br J Cancer. 2019;120(8):797–805. doi:10.1038/s41416-019-0429-2
19. Zaanan A, Cuilliere-Dartigues P, Guilloux A, et al. Impact of P53 expression and microsatellite instability on Stage III colon cancer disease-free survival in patients treated by 5-Fluorouracil and leucovorin with or without oxaliplatin. Ann Oncol. 2010;21(4):772–780. doi:10.1093/annonc/mdp383
20. Ntavatzikos A, Spathis A, Patapis P, et al. TYMS/KRAS/BRAF molecular profiling predicts survival following adjuvant chemotherapy in colorectal cancer. World J Gastrointest Oncol. 2019;11(7):551–566. doi:10.4251/wjgo.v11.i7.551
21. Uchida K, Hayashi K, Kawakami K, et al. Loss of heterozygosity at the thymidylate synthase (TS) locus on chromosome 18 affects tumor response and survival in individuals heterozygous for a 28-bp polymorphism in the TS gene. Clin Cancer Res. 2004;10(2):433–439. doi:10.1158/1078-0432.CCR-0200-03
22. Van den Broek E, Krijgsman O, Sie D, et al. Genomic profiling of stage II and III colon cancers reveals APC mutations to be associated with survival in Stage III colon cancer patients. Oncotarget. 2016;7(45):73876–73887. doi:10.18632/oncotarget.12510
23. Henriksson ML, Edin S, Dahlin AM, et al. Colorectal cancer cells activate adjacent fibroblasts resulting in FGF1/FGFR3 signaling and increased invasion. Am J Pathol. 2011;178(3):1387–1394. doi:10.1016/j.ajpath.2010.12.008
24. Takayama T, Miyanishi K, Hayashi T, Sato Y, Niitsu Y. Colorectal cancer: genetics of development and metastasis. J Gastroenterol. 2006;41(3):185–192. doi:10.1007/s00535-006-1801-6
25. Day FL, Jorissen RN, Lipton L, et al. PIK3CA and PTEN gene and exon mutation-specific clinicopathologic and molecular associations in colorectal cancer. Clin Cancer Res. 2013;19(12):3285–3296. doi:10.1158/1078-0432.CCR-12-3614
26. Chung Y, Wi YC, Kim Y, et al. The Smad4/PTEN expression pattern predicts clinical outcomes in colorectal adenocarcinoma. J Pathol Transl Med. 2018;52(1):37–44. doi:10.4132/jptm.2017.10.20
27. Danielsen SA, Eide PW, Nesbakken A, et al. Portrait of the PI3K/AKT pathway in colorectal cancer. Biochimica Et Biophysica Acta - Rev Cancer. 2015;1855:104–121.
28. Johnson SM, Gulhati P, Rampy BA, et al. Novel expression patterns of PI3K/Akt/MTOR signaling pathway components in colorectal cancer. J Am Coll Surg. 2010;210(5):
29. Cerami E, Gao J, Dogrusoz U, et al. The cbio cancer genomics portal: an open platform for exploring multidimensional cancer genomics data. Cancer Discov. 2012;2(5):401–404. doi:10.1158/2159-8290.CD-12-0095
30. Gao J, Aksoy BA, Dogrusoz U, et al. Integrative analysis of complex cancer genomics and clinical profiles using the CBioPortal. Sci Signal. 2013;6(269):pl1. doi:10.1126/scisignal.2004088
31. Williams CS, Bernard JK, Beckler MD, et al. ERBB4 is over-expressed in human colon cancer and enhances cellular transformation. Carcinogenesis. 2015;36(7):710–718.
32. Frampton GM, Fichtenholtz A, Otto GA, et al. Development and validation of a clinical cancer genomic profiling test based on massively parallel DNA sequencing. Nat Biotechnol. 2013;31(11):1023–1031. doi:10.1038/nbt.2696
33. Uzilov AV, Ding W, Fink MY, et al. Development and clinical application of an integrative genomic approach to personalized cancer therapy. Genome Med. 2016;8(1):62. doi:10.1186/s13073-016-0313-0
34. Romiti A, Roberto M, Marchetti P, et al. Study of histopathologic parameters to define the prognosis of Stage II colon cancer. Colorectal Dis. 2019;34(5):905–913. doi:10.1007/s00384-019-03279-1
35. Benson AB, Venook AP, Al-Hawary MM, et al. NCCN guidelines insights: colon cancer, Version 2.2018. J Natl Compr Canc Netw. 2018;16(4):359–369. doi:10.6004/jnccn.2018.0021
36. Szklarczyk D, Gable AL, Lyon D, et al. STRING v11: protein-protein association networks with increased coverage, supporting functional discovery in genome-wide experimental datasets. Nucleic Acids Res. 2019;47(D1):D607–D613. doi:10.1093/nar/gky1131
37. American Cancer Society. Facts & figures 2019. Am Cancer Soc. 2019;4:e478.
38. Dotan E, Cohen SJ. Challenges in the management of stage II colon cancer. Semin Oncol. 2011;38(4):511–520. doi:10.1053/j.seminoncol.2011.05.005
39. Gray R, Barnwell J, McConkey C, et al; Quasar Collaborative Group. Adjuvant chemotherapy versus observation in patients with colorectal cancer: a Randomised Study. Lancet. 2007;370(9604):2020–2029. doi:10.1016/S0140-6736(07)61866-2
40. Compton C, Fenoglio-Preiser CM, Pettigrew N, Fielding LP. American joint committee on cancer prognostic factors consensus conference: colorectal Working Group. Cancer. 2000;88(7):1739–1757. doi:10.1002/(SICI)1097-0142(20000401)88:7<1739::AID-CNCR30>3.0.CO;2-T
41. Compton CC, Fielding LP, Burgart LJ, et al. Prognostic factors in colorectal cancer: College of American pathologists consensus statement 1999. Arch Pathol Lab Med. 2000;124(7):979–994. doi:10.5858/2000-124-0979-PFICC
42. André T, Boni C, Mounedji-Boudiaf L, et al. Oxaliplatin, fluorouracil, and leucovorin as adjuvant treatment for colon cancer. N Engl J Med. 2004;350(23):2343–2351. doi:10.1056/NEJMoa032709
43. Kuan TC, Chang SC, Lin JK, et al. Prognosticators of long-term outcomes of TNM stage II colorectal cancer: molecular patterns or clinicopathological features. World J Surg. 2019;43(12):3207–3215. doi:10.1007/s00268-019-05158-w
44. Miller JR, Hocking AM, Brown JD, Moon RT. Mechanism and function of signal transduction by the Wnt/beta-catenin and Wnt/Ca2+ pathways. Oncogene. 1999;18(55):7860–7872. doi:10.1038/sj.onc.1203245
45. Jou TS, Stewart DB, Stappert J, Nelson WJ, Marrs JA. Genetic and biochemical dissection of protein linkages in the cadherin-catenin complex. Proc Natl Acad Sci U S A. 1995;92(11):5067–5071. doi:10.1073/pnas.92.11.5067
46. Kawasaki Y, Senda T, Ishidate T, et al. Asef, a link between the tumor suppressor APC and G-protein signaling. Science. 2000;289(5482):1194–1197. doi:10.1126/science.289.5482.1194
47. Morrison EE, Wardleworth BN, Askham JM, et al. EB1, a protein which interacts with the APC tumour suppressor, is associated with the microtubule cytoskeleton throughout the cell cycle. Oncogene. 1998;17(26):3471–3477. doi:10.1038/sj.onc.1202247
48. Morin PJ, Vogelstein B, Kinzler KW. Apoptosis and APC in colorectal tumorigenesis. Proc Natl Acad Sci U S A. 1996;93(15):7950–7954. doi:10.1073/pnas.93.15.7950
49. He TC, Sparks AB, Rago C, et al. Identification of C-MYC as a target of the APC pathway. Science. 1998;281(5382):1509–1512. doi:10.1126/science.281.5382.1509
50. Tetsu O, McCormick F. Beta-catenin regulates expression of cyclin D1 in colon carcinoma cells. Nature. 1999;398(6726):422–426. doi:10.1038/18884
51. Spruck CH, Strohmaier H, Sangfelt O, et al. HCDC4 gene mutations in endometrial cancer. Cancer Res. 2002;62(16):4535–4539.
52. Yeh CH, Bellon M, Nicot C. FBXW7: a critical tumor suppressor of human cancers. Mol Cancer. 2018;17(1):115. doi:10.1186/s12943-018-0857-2
53. Cao J, Ge MH, Ling ZQ. Fbxw7 tumor suppressor: a vital regulator contributes to human tumorigenesis. Medicine. 2016;95(7):e2496. doi:10.1097/MD.0000000000002496
54. Iwatsuki M, Mimori K, Ishii H, et al. Loss of FBXW7, a cell cycle regulating gene, in colorectal cancer: clinical significance. Int J Cancer. 2010;126(8):1828–1837. doi:10.1002/ijc.24879
55. Babaei-Jadidi R, Li N, Saadeddin A, et al. FBXW7 influences murine intestinal homeostasis and cancer, targeting Notch, Jun, and DEK for degradation. J Exp Med. 2011;208(2):295–312. doi:10.1084/jem.20100830
56. Kemp Z, Rowan A, Chambers W, et al. CDC4 mutations occur in a subset of colorectal cancers but are not predicted to cause loss of function and are not associated with chromosomal instability. Cancer Res. 2005;65(24):11361–11366. doi:10.1158/0008-5472.CAN-05-2565
57. Akhoondi S, Sun D, von der Lehr N, et al. FBXW7/HCDC4 is a general tumor suppressor in human cancer. Cancer Res. 2007;67(19):9006–9012. doi:10.1158/0008-5472.CAN-07-1320
58. Malapelle U, Pisapia P, Sgariglia R, et al. Less frequently mutated genes in colorectal cancer: evidences from next-generation sequencing of 653 routine cases. J Clin Pathol. 2016;69(9):767–771. doi:10.1136/jclinpath-2015-203403
59. Korphaisarn K, Morris VK, Overman MJ, et al. FBXW7 missense mutation: a novel negative prognostic factor in metastatic colorectal adenocarcinoma. Oncotarget. 2017;8(24):39268–39279. doi:10.18632/oncotarget.16848
60. Bai J, Gao J, Mao Z, et al. Genetic mutations in human rectal cancers detected by targeted sequencing. J Hum Genet. 2015;60(10):589–596.
61. Jardim DL, Wheler JJ, Hess K, et al. FBXW7 mutations in patients with advanced cancers: clinical and molecular characteristics and outcomes with MTOR inhibitors. P PLoS One. 2014;9(2):e89388. doi:10.1371/journal.pone.0089388
62. Smith G, Carey FA, Beattie J, et al. Mutations in APC, Kirsten-Ras, and P53 - Alternative Genetic Pathways to Colorectal Cancer. Proc Natl Acad Sci U S A. 2002 Jul 9;99(14):9433–8
63. Conlin A, Smith G, Carey FA, Wolf CR, Steele RJ. The prognostic significance of K-ras, p53, and APC mutations in colorectal carcinoma. Gut. 2005;54(9):1283–1286. doi:10.1136/gut.2005.066514
64. Datta J, Smith JJ, Chatila WK, et al. Coaltered Ras/B-Raf and TP53 is associated with extremes of survivorship and distinct patterns of metastasis in patients with metastatic colorectal cancer. Clin Cancer Res. 2020;26(5):1077–1085.
65. Esteller M. Epigenetic lesions causing genetic lesions in human cancer: promoter hypermethylation of DNA repair genes. Eur J Cancer. 2000;36(18):2294–2300. doi:10.1016/S0959-8049(00)00303-8
66. Kawakami K, Ruszkiewicz A, Bennett G, et al. DNA hypermethylation in the normal colonic mucosa of patients with colorectal cancer. Br J Cancer. 2006;94(4):593–598. doi:10.1038/sj.bjc.6602940
67. Weisenberger DJ, Siegmund KD, Campan M, et al. CpG island methylator phenotype underlies sporadic microsatellite instability and is tightly associated with BRAF mutation in colorectal cancer. Nat Genet. 2006;38(7):787–793. doi:10.1038/ng1834
68. Arnold CN, Goel A, Compton C, et al. Evaluation of microsatellite instability, HMLH1 expression and HMLH1 promoter hypermethylation in defining the MSI phenotype of colorectal cancer. Cancer Biol Ther. 2004;3(1):73–78. doi:10.4161/cbt.3.1.590
69. Herman JG, Umar A, Polyak K, et al. Incidence and functional consequences of HMLH1 promoter hypermethylation in colorectal carcinoma. Proc Natl Acad Sci U S A. 1998;95(12):6870–6875. doi:10.1073/pnas.95.12.6870
70. Kuismanen SA, Holmberg MT, Salovaara R, de la Chapelle A, Peltomäki P. Genetic and epigenetic modification of MLH1 accounts for a major share of microsatellite-unstable colorectal cancers. Am J Pathol. 2000;156(5):1773–1779. doi:10.1016/S0002-9440(10)65048-1
71. de Vogel S, Bongaerts BW, Wouters KA, et al. Associations of dietary methyl donor intake with MLH1 promoter hypermethylation and related molecular phenotypes in sporadic colorectal cancer. Carcinogenesis. 2008;29(9):1765–1773. doi:10.1093/carcin/bgn074
72. Ogino S, Brahmandam M, Kawasaki T, Kirkner GJ, Loda M, Fuchs CS. Combined analysis of COX-2 and p53 expressions reveals synergistic inverse correlations with microsatellite instability and CpG island methylator phenotype in colorectal cancer. Neoplasia. 2006;8(6):458–464. doi:10.1593/neo.06247
73. Salahshor S, Kressner U, Pâhlman L, Glimelius B, Lindmark G, Lindblom A. Colorectal cancer with and without microsatellite instability involves different genes. Genes Chromosomes Cancer. 1999;26(3):247–252. doi:10.1002/(SICI)1098-2264(199911)26:3<247::AID-GCC9>3.0.CO;2-H
74. Samowitz WS, Albertsen H, Herrick J, et al. Evaluation of a large, population-based sample supports a CpG island methylator phenotype in colon cancer. Gastroenterology. 2005;129(3):837–845. doi:10.1053/j.gastro.2005.06.020
75. van Rijnsoever M, Grieu F, Elsaleh H, Joseph D, Iacopetta B. Characterisation of colorectal cancers showing hypermethylation at multiple CpG islands. Gut. 2002;51(6):797–802. doi:10.1136/gut.51.6.797
76. de Vogel S, Weijenberg MP, Herman JG, et al. MGMT and MLH1 promoter methylation versus APC, KRAS and BRAF gene mutations in colorectal cancer: indications for distinct pathways and sequence of events. Ann Oncol. 2009;20(7):1216–1222. doi:10.1093/annonc/mdn782
77. Tie J, Lipton L, Desai J, et al. KRAS mutation is associated with lung metastasis in patients with curatively resected colorectal cancer. Clin Cancer Res. 2011;17(5):1122–1130. doi:10.1158/1078-0432.CCR-10-1720
78. Huang D, Sun W, Zhou Y, et al. Mutations of key driver genes in colorectal cancer progression and metastasis. Cancer Metastasis Rev. 2018;37(1):173–187. doi:10.1007/s10555-017-9726-5
79. Schweiger T, Liebmann-Reindl S, Glueck O, et al. Mutational profile of colorectal cancer lung metastases and paired primary tumors by targeted next generation sequencing: implications on clinical outcome after surgery. J Thorac Dis. 2018;10(11):6147–6157. doi:10.21037/jtd.2018.10.72
80. Cai ZX, Tang XD, Gao HL, et al. APC, FBXW7, KRAS, PIK3CA, and TP53 gene mutations in human colorectal cancer tumors frequently detected by next-generation DNA sequencing [abstract]. J Mol Genet Med. 2014;8:4.
81. Lugli A, Tzankov A, Zlobec I, Terracciano LM. Differential diagnostic and functional role of the multi-marker phenotype CDX2/CK20/CK7 in colorectal cancer stratified by mismatch repair status. Mod Pathol. 2008;21(11):1403–1412. doi:10.1038/modpathol.2008.117
82. Baba Y, Nosho K, Shima K, et al. Relationship of CDX2 loss with molecular features and prognosis in colorectal cancer. Clin Cancer Res. 2009;15(14):4665–4673. doi:10.1158/1078-0432.CCR-09-0401
83. Zlobec I, Bihl MP, Schwarb H, Terracciano L, Lugli A. Clinicopathological and protein characterization of BRAF- and K-RAS-mutated colorectal cancer and implications for prognosis. Int J Cancer. 2010;127(2):367–380. doi:10.1002/ijc.25042
84. Bae JM, Lee TH, Cho NY, Kim TY, Kang GH. Loss of CDX2 expression is associated with poor prognosis in colorectal cancer patients. World J Gastroenterol. 2015;21(5):1457–1467. doi:10.3748/wjg.v21.i5.1457
85. Kumar Y, Shukla N, Thacker G, et al. Ubiquitin ligase, Fbxw7, targets CDX2 for degradation via two phosphodegron motifs in a GSK3b-dependent manner. Mol Cancer Res. 2016;14(11):1097–1109. doi:10.1158/1541-7786.MCR-16-0138
86. Xu W, Zhu Y, Shen W, et al. Combination of CDX2 expression and T stage improves prognostic prediction of colorectal cancer. J Int Med Res. 2019;47(5):1829–1842. doi:10.1177/0300060518819620
87. Koopman M, Kortman GA, Mekenkamp L, et al. Deficient mismatch repair system in patients with sporadic advanced colorectal cancer. Br J Cancer. 2009;100(2):266–73.7. doi:10.1038/sj.bjc.6604867
88. Lothe RA, Peltomäki P, Meling GI, et al. Genomic instability in colorectal cancer: relationship to clinicopathological variables and family history. Cancer Res. 1993;53(24):5849–5852.
89. Thibodeau SN, Bren G, Schaid D. Microsatellite instability in cancer of the proximal colon. Science. 1993;260(5109):816–819. doi:10.1126/science.8484122
90. Jass JR, Barker M, Fraser L, et al. APC mutation and tumour budding in colorectal cancer. J Clin Pathol. 2003;56(1):69–73. doi:10.1136/jcp.56.1.69
91. Zlobec I, Lugli A. Invasive front of colorectal cancer: dynamic interface of pro-/anti-tumor factors. World J Gastroenterol. 2009;15(47):5898–5906. doi:10.3748/wjg.15.5898
92. Zlobec I, Lugli A. Epithelial mesenchymal transition and tumor budding in aggressive colorectal cancer: tumor budding as oncotarget. Oncotarget. 2010;1(7):651–661. doi:10.18632/oncotarget.199
93. Koyama M, Morita T, Hashizume T, et al. Prognostic risk factors associated with recurrence after curative resection in patients with stage II colorectal cancer. Gan To Kagaku Ryoho. 2013;40(12):1650–1652.
94. Nissan A, Stojadinovic A, Shia J, et al. Predictors of recurrence in patients with T2 and early T3, N0 adenocarcinoma of the rectum treated by surgery alone. J Clin Oncol. 2006;24(25):4078–4084. doi:10.1200/JCO.2006.06.2968
95. Fujita S, Shimoda T, Yoshimura K, Yamamoto S, Akasu T, Moriya Y. Prospective evaluation of prognostic factors in patients with colorectal cancer undergoing curative resection. J Surg Oncol. 2003;84(3):127–131. doi:10.1002/jso.10308
96. Quah HM, Chou JF, Gonen M, et al. Identification of patients with high-risk stage II colon cancer for adjuvant therapy. Dis Colon Rectum. 2008;51(5):503–507. doi:10.1007/s10350-008-9246-z
97. Huh JW, Kim HR, Kim YJ. Prognostic value of perineural invasion in patients with stage II colorectal cancer. Ann Surg Oncol. 2010;17(8):2066–2072. doi:10.1245/s10434-010-0982-7
98. Shinto E, Oki E, Shimokawa M, et al. A validation study for recurrence risk stratification of stage II colon cancer using the 55-gene classifier. Oncology. 2020;98(8):534–541. doi:10.1159/000506369
99. Des Guetz G, Schischmanoff O, Nicolas P, Perret GY, Morere JF, Uzzan B. Does microsatellite instability predict the efficacy of adjuvant chemotherapy in colorectal cancer? A systematic review with meta-analysis. Eur J Cancer. 2009;45(10):1890–1896. doi:10.1016/j.ejca.2009.04.018
100. Ghidini M, Personeni N, Bozzarelli S, et al. KRAS mutation in lung metastases from colorectal cancer: prognostic implications. Cancer Med. 2016;5(2):256–264. doi:10.1002/cam4.592
101. Li W, Qiu T, Guo L, Ying J, Zhou A. NGS-based oncogenic mutations analysis in advanced colorectal cancer patients improves targeted therapy prediction. Pathol Res Pract. 2019;215(3):483–489. doi:10.1016/j.prp.2018.12.037
102. Copija A, Waniczek D, Witkoś A, Walkiewicz K, Nowakowska-Zajdel E. Clinical significance and prognostic relevance of microsatellite instability in sporadic colorectal cancer patients. Int J Mol Sci. 2017;18(1):107. doi:10.3390/ijms18010107
103. Guinney J, Ferté C, Dry J, et al. Modeling RAS phenotype in colorectal cancer uncovers novel molecular traits of RAS dependency and improves prediction of response to targeted agents in patients. Clin Cancer Res. 2014;20(1):265–272. doi:10.1158/1078-0432.CCR-13-1943
104. Wertz IE, Kusam S, Lam C, et al. Sensitivity to antitubulin chemotherapeutics is regulated by MCL1 and FBW7. Nature. 2011;471(7336):110–114. doi:10.1038/nature09779
105. Tong J, Tan S, Zou F, Yu J, Zhang L. FBW7 mutations mediate resistance of colorectal cancer to targeted therapies by blocking Mcl-1 degradation. Oncogene. 2017;36(6):787–796. doi:10.1038/onc.2016.247
106. Lorenzi F, Babaei-Jadidi R, Sheard J, Spencer-Dene B, Nateri AS. Fbxw7-associated drug resistance is reversed by induction of terminal differentiation in murine intestinal organoid culture. Mol Ther Methods Clin Dev. 2016;3:16024. doi:10.1038/mtm.2016.24
107. Li N, Babaei-Jadidi R, Lorenzi F, et al. An FBXW7-ZEB2 axis links EMT and tumour microenvironment to promote colorectal cancer stem cells and chemoresistance. Oncogenesis. 2019;8(3):13. doi:10.1038/s41389-019-0125-3
108. Ye M, Zhang Y, Zhang X, et al. Targeting FBW7 as a strategy to overcome resistance to targeted therapy in non–small cell lung cancer. Cancer Res. 2017;77(13):3527–3539. doi:10.1158/0008-5472.CAN-16-3470
109. Grim JE, Knoblaugh SE, Guthrie KA, et al. Fbw7 and P53 cooperatively suppress advanced and chromosomally unstable intestinal cancer. Mol Cell Biol. 2012;32(11):2160–2167. doi:10.1128/MCB.00305-12
110. Li MM, Datto M, Duncavage EJ, et al. Standards and guidelines for the interpretation and reporting of sequence variants in cancer: a joint consensus recommendation of the Association for Molecular Pathology, American Society of Clinical Oncology, and College of American Pathologists. J Mol Diagn. 2017;19(1):4–23. doi:10.1016/j.jmoldx.2016.10.002
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

