Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 16
The Impact of Exacerbation History on the Safety and Efficacy of Aclidinium in Patients with Chronic Obstructive Pulmonary Disease and Increased Cardiovascular Risk: ASCENT-COPD Trial
Authors Wise RA , Chapman KR , Scirica BM, Daoud SZ, Lythgoe D , Garcia-Gil E
Received 22 October 2020
Accepted for publication 22 February 2021
Published 18 March 2021 Volume 2021:16 Pages 689—699
DOI https://doi.org/10.2147/COPD.S285068
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 5
Editor who approved publication: Dr Richard Russell
Robert A Wise,1 Kenneth R Chapman,2 Benjamin M Scirica,3,4 Sami Z Daoud,5 Dan Lythgoe,6 Esther Garcia-Gil7
1Medicine, Pulmonary and Critical Care, Johns Hopkins University School of Medicine, Baltimore, MD, USA; 2Department of Medicine, University of Toronto, Toronto, ON, Canada; 3Cardiovascular Division, Brigham and Women’s Hospital, Boston, MA, USA; 4Department of Medicine, Harvard Medical School, Boston, MA, USA; 5Late-Stage Respiratory and Immunology, BioPharmaceuticals R&D, AstraZeneca, Gaithersburg, MD, USA; 6Statistics, Phastar, Chiswick, London, UK; 7Respiratory & Immunology, BioPharmaceuticals Medical, AstraZeneca, Barcelona, Spain
Correspondence: Robert A Wise
Medicine, Pulmonary and Critical Care, Johns Hopkins University School of Medicine, 5501 Hopkins Bayview Circle, Baltimore, MD, 21224, USA
Email [email protected]
Purpose: Chronic obstructive pulmonary disease (COPD) exacerbations are associated with increased risk of major adverse cardiovascular events (MACE) and mortality. Here, we investigate whether the safety and efficacy of aclidinium bromide differ due to exacerbation history in patients with COPD and increased cardiovascular risk.
Patients and Methods: ASCENT-COPD was a Phase 4, multicenter, double-blind, randomized, placebo-controlled, parallel-group study of patients with moderate-to-very severe COPD and increased cardiovascular risk. Patients were randomized 1:1 to receive aclidinium or placebo twice daily for up to 3 years. Outcomes included time to first MACE and all-cause mortality over 3 years, exacerbation rate during the first year on-treatment, and change in baseline pre-dose forced expiratory volume in 1 second (FEV1) over 3 years. This pre-specified subgroup analysis compared outcomes in patients receiving aclidinium vs placebo. The comparison of patients with vs without an exacerbation history was added following a protocol amendment to increase enrollment in the primary study.
Results: Of 3589 patients, 2156 (60.1%) had ≥ 1 moderate or severe exacerbations in the prior year, compared with 1433 (39.9%) without prior exacerbations. Although patients with an exacerbation history had numerically higher rates of MACE and mortality regardless of treatment, aclidinium did not increase risk of MACE (≥ 1: hazard ratio [HR] 0.79, 95% confidence interval [CI]: 0.54– 1.16; none: HR 1.27, 95% CI: 0.65– 2.47; interaction P=0.233) or all-cause mortality (≥ 1: HR 1.08, 95% CI: 0.81– 1.43; none: HR 0.66, 95% CI: 0.36– 1.22; interaction P=0.154), regardless of exacerbation history. Aclidinium reduced the exacerbation rate vs placebo irrespective of exacerbation history (≥ 1: rate ratio [RR] 0.80, 95% CI: 0.68– 0.94; none: RR 0.69, 95% CI: 0.54– 0.89; interaction P=0.340) and improved FEV1 (interaction P=0.633).
Conclusion: In patients with moderate-to-very severe COPD and increased cardiovascular risk, aclidinium did not increase risk of MACE or mortality and reduced exacerbation rate vs placebo, regardless of exacerbation history.
Clinical Trial Registration: ClinicalTrials.gov Identifier: NCT01966107.
Keywords: COPD, COPD exacerbation, aclidinium, MACE, mortality
Introduction
Chronic obstructive pulmonary disease (COPD) is a heterogeneous disease characterized by persistent respiratory symptoms and airflow obstruction and is a leading cause of morbidity and mortality worldwide.1 In a review of five studies, over 70% of patients experienced ≥1 exacerbations within three years of study initiation,2 and these events play a substantial role in the disease burden for both patients and healthcare systems. Exacerbations can be characterized as mild (requiring an increase in dose of regular medication), moderate (requiring additional medication from a physician, such as corticosteroids and/or antibiotics), or severe (resulting in hospitalization and/or mortality).3 Exacerbations are associated with an accelerated decline in lung function4,5 and an increased risk of major adverse cardiovascular events (MACE; defined as cardiovascular mortality, non-fatal myocardial infarction, or non-fatal stroke)6–9 and mortality.10−12
Aclidinium bromide 400 µg twice daily is a long-acting muscarinic antagonist approved for use as maintenance treatment for patients with COPD, administered using a breath-actuated dry-powder inhaler (Genuair/Pressair; AstraZeneca).13,14 ASCENT-COPD was a Phase 4, multicenter, double-blind, randomized, placebo-controlled, parallel-group study that evaluated cardiovascular (CV) safety and COPD exacerbation rate in patients with moderate-to-very severe COPD and increased CV risk.15 Treatment with aclidinium did not increase risk of MACE vs placebo over 3 years and reduced the rate of COPD exacerbations vs placebo over one year.15
Most studies that aim to reduce COPD exacerbation risk enroll patients with a history of exacerbations and exclude patients with CV risk factors.3,16,17 ASCENT-COPD provided a unique population of patients with or without an exacerbation history and an increased CV risk. This pre-specified subgroup analysis aimed to compare the effect of aclidinium treatment on MACE, exacerbations, and lung function in ASCENT-COPD patients. The comparison of patients with vs without an exacerbation history was added following a protocol amendment to increase enrollment in the primary study. The hypothesis of this subgroup analysis was that a benefit in exacerbation prevention with aclidinium vs placebo would not be found in patients without an exacerbation history, but aclidinium would demonstrate improved lung function vs placebo. Moreover, it was hypothesized that patients with an exacerbation history would have more MACE and COPD exacerbations compared with patients without an exacerbation history.
Methods
Study Design
The study design for the ASCENT-COPD study has been reported in detail previously.18 In brief, ASCENT-COPD (NCT01966107) was a Phase 4, multicenter, double-blind, randomized, placebo-controlled, parallel-group study conducted at 522 sites in the USA and Canada.15 The study comprised a 2-week washout period, followed by a double-blind treatment phase, during which patients were randomized 1:1 to receive aclidinium 400 μg or matching placebo twice daily for up to 3 years, until ≥122 MACE events occurred. In this subgroup analysis, patients were categorized according to whether or not they had experienced ≥1 moderate or severe COPD exacerbations (requiring additional medication from a physician, such as corticosteroids and/or antibiotics, or resulting in hospitalization and/or mortality) in the year prior to the study.
Study Population
The study population for the ASCENT-COPD study has been previously reported.15 In brief, eligible patients were males or females aged ≥40 years with moderate-to-very severe COPD (forced expiratory volume in 1 second [FEV1]/forced vital capacity <70%, and FEV1 < 80% predicted) and a smoking history of ≥10 pack-years. Details of the CV risk factors can be found in the supplementary materials. When the ASCENT-COPD study was started, patients were required to have had ≥1 treated COPD exacerbations in the year prior to screening; however, this requirement was subsequently removed after approximately half of the patients were enrolled to increase accrual and allow for a broader patient population. At that time, the upper limit of FEV1 was also increased from 70% to 80% predicted.
Outcome Measures
Safety outcomes included time to first MACE over 3 years, as adjudicated by a clinical endpoint adjudication committee,15 and all-cause mortality. Efficacy outcomes were annual rate of moderate or severe COPD exacerbations during the first year on-treatment and change in baseline pre-dose (trough) FEV1 over 3 years.
Statistical Considerations
All statistical analyses were based on the full analysis set (all patients who took ≥1 dose of treatment), and patients were analyzed according to their randomized treatment. Safety analyses included “on-study” data, ie, all data collected during the follow-up period, irrespective of treatment discontinuation. Efficacy analyses included “on-treatment” data, ie, data up to discontinuation of randomized treatment, where applicable; MACE and moderate or severe COPD exacerbation rate analyses were pre-specified.
Time to first MACE was analyzed using subgroup-specific (ie, no or ≥1 exacerbations) Cox proportional hazards models with randomized treatment group (aclidinium/placebo), history of ≥1 exacerbation in the previous year (yes/no), baseline CV risk group (prior events and risk factors), and smoking status (current smoker, ex-smoker) as factors. To assess evidence of a differential treatment effect, an additional analysis was undertaken, including both subgroups and a treatment-by-exacerbation history interaction term. This approach was also undertaken for all-cause mortality. Moderate or severe COPD exacerbation rates were analyzed using negative binomial regression models with treatment group and exacerbation history, and their two-way interaction. Spirometry outcomes were analyzed on-treatment during the first year using mixed models for repeated measures adjusted for pre- and post-bronchodilator FEV1 at screening, baseline FEV1, smoking status, baseline inhaled corticosteroid use, exacerbation history, and visits. In addition, this included a three-way interaction between treatment, baseline exacerbation history, and study visit.
To compare the incidence of MACE and all-cause mortality between those with and without exacerbation history it was necessary to account for differential follow-up times between these subgroups. Cox regression models including randomized treatment group, history of ≥1 exacerbation in the previous year, baseline CV risk group, smoking status and the interaction between exacerbation history and treatment group were used. The overall effect of exacerbation history was obtained by averaging the treatment-specific effect estimates.
All reported outputs were produced using SAS version 9.3 (SAS Institute Inc). P values for treatment-by-exacerbation history interaction effects were considered statistically significant if P<0.10; otherwise P values less than 0.05 were considered statistically significant.
Results
Baseline Demographics and Characteristics
Of the 3589 patients included in this analysis, 2156 (60.1%) patients had a history of ≥1 moderate or severe COPD exacerbations in the year prior to randomization compared with 1433 (39.9%) patients without prior COPD exacerbations (Figure 1). Baseline demographics were generally comparable between patients with and without an exacerbation history; however, baseline COPD characteristics and CV risk differed (Table 1). Patients with an exacerbation history had worse airflow obstruction (14.9% very severe, 44.1% severe, 39.1% moderate, and 0.5% mild) vs patients without an exacerbation history (10.0% very severe, 35.2% severe, 53.1% moderate, and 0.4% mild). A higher percentage of patients with vs without an exacerbation history had one or more CV events, plus two or more atherothrombotic risk factors (47.3% vs 38.9%, respectively). Prior inhaled corticosteroid use was greater in patients with vs without an exacerbation history, both alone and in combination with a long-acting β2-agonists and/or long-acting muscarinic antagonist (60.0% vs 51.9%, respectively). COPD assessment test total and individual scores were similar between patients with and without an exacerbation history (total score, mean [standard deviation, SD]: 21.0 [7.3] vs 20.2 [7.1], respectively). Patients with an exacerbation history had lower lung function vs patients without an exacerbation history (post-bronchodilator FEV1% predicted, mean [SD] 45.7 [14.6] vs 50.7 [15.1], respectively).
 |
Table 1 Baseline Demographics and Characteristics |
Safety
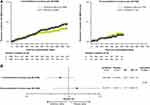
Although patients with an exacerbation history experienced numerically more MACE than patients without an exacerbation history (≥1 exacerbation: 5.1%; no exacerbations: 2.4%; hazard ratio [HR] 1.34, 95% confidence intervals [CI] 0.90–2.00; P=0.156), aclidinium did not increase risk of MACE, regardless of exacerbation history (≥1 exacerbation: HR 0.79, 95% CI: 0.54–1.16; no exacerbations: HR 1.27, 95% CI: 0.65–2.47; interaction P=0.233; Figure 2).
The rate of all-cause mortality was numerically higher in patients with an exacerbation history (≥1 exacerbation: 8.9%; no exacerbations: 2.9%; HR 1.11, 95% CI 0.76–1.62; P=0.580). However, aclidinium did not increase all-cause mortality risk, irrespective of COPD exacerbation (≥1 exacerbation: HR 1.08, 95% CI: 0.81–1.43; no exacerbations: HR 0.66, 95% CI: 0.36–1.22; interaction P=0.154; Figure 3).
Efficacy
The hazard ratios for time to first moderate or severe COPD exacerbations (Figure 4A) were similar for patients with or without an exacerbation history (interaction P=0.279). The annual exacerbation rate was numerically higher in patients who had a history of COPD exacerbations (≥1 exacerbation: aclidinium 0.65 vs placebo 0.82, absolute rate reduction: 0.17; no exacerbation: aclidinium 0.27 vs placebo 0.38, absolute rate reduction: 0.11; Figure 4B). Aclidinium reduced the annual exacerbation rate vs placebo for patients with or without an exacerbation history with a similar relative benefit (≥1 exacerbation: rate ratio [RR] 0.80, 95% CI: 0.68–0.94; no exacerbations: RR 0.69, 95% CI 0.54–0.89; interaction P=0.340). In addition, benefits of treatment with aclidinium in reducing exacerbation rate were irrespective of whether the exacerbation required systemic corticosteroid or antibiotic use (of note, patients could be counted in >1 category; Figure 4C); RRs were comparable between the two exacerbation treatment approaches (systemic corticosteroid: RR 0.81, 95% CI: 0.70–0.95; antibiotics: RR 0.75, 95% CI 0.65–0.87).
In terms of lung function, trough FEV1 was higher in patients with or without an exacerbation history treated with aclidinium vs placebo (Figure 5). Although treatment differences were numerically higher for patients with an exacerbation history vs those without (least square mean difference 93 mL, 95% CI: 66–120 vs 65 mL, 95% CI: 27–103), there was no evidence of a differential effect of treatment across subgroups (interaction P=0.633).
Discussion
In this subgroup analysis of the ASCENT-COPD study of patients with moderate-to-very severe COPD and CV risk factors, the risk of MACE, all-cause mortality, and rate of moderate-to-very severe COPD exacerbations were found to be numerically higher in patients with an exacerbation history vs those without an exacerbation history. Importantly, the safety of aclidinium with regards to MACE and all-cause mortality was similar to placebo, even in the higher risk population with a COPD exacerbation history. Although the relative reduction in rate of COPD exacerbations was similar in patients regardless of exacerbation history, the absolute reduction in exacerbation rate was greater in patients with an exacerbation history vs those without an exacerbation history. Improvements in pre-dose FEV1 were observed in all patients treated with aclidinium vs placebo, regardless of exacerbation history.
Overall and similar to previous observations,6–9,11,12 patients with a history of COPD exacerbation had a numerically increased risk of MACE and all-cause mortality vs those without an exacerbation history.
In a retrospective analysis of the UPLIFT trial, which evaluated symptoms, lung function, and exacerbation history,19 patients in GOLD Groups A and B, had exacerbations with tiotropium (RR 0.64 and 0.72, respectively) that were similar to the non-exacerbation subgroup in this analysis (RR 0.69) in this study; however, in GOLD Groups C and D, exacerbations with tiotropium (RR 0.91 and 0.89, respectively) were numerically higher than the prior-exacerbation subgroup reported here (RR 0.80). Rates of MACE were similar between tiotropium and placebo for GOLD Groups A-C in the UPLIFT trial; however, tiotropium significantly reduced the rate of MACE in GOLD Group D vs placebo. Because of the inclusion of patients with an increased CV risk in the ASCENT-COPD study, and subgroup definitions, it is not possible to say whether aclidinium is more effective than tiotropium in patients with more severe COPD (ie, patients in GOLD Groups C and D, and those with an exacerbation history). However, coupled with results from the UPLIFT trial, these findings support and extend those of the overall ASCENT-COPD study15 and increase the confidence that long-acting muscarinic antagonists do not confer increased risk of CV disease in patients with COPD.19
Strengths of the study include the use of prospective and uniform data collection and verified definitions of both exacerbations and MACE. Furthermore, in contrast to observational studies, the ASCENT-COPD study was designed to demonstrate the effects of aclidinium, including the rate of exacerbations, in patients with COPD and increased CV risk, and as such the treatment assignment to aclidinium was random, regardless of COPD exacerbation history.
Limitations of the study include the change in patient enrollment after the study had begun; although an exacerbation history was an inclusion factor at the beginning of the study, the enrollment of patients without an exacerbation history was permitted from approximately half-way through the study, therefore the two subpopulations were not completely concurrent. Together with study completion at 122 MACE events, this led to a longer follow-up time for patients with a COPD exacerbation history with respect to MACE and mortality; however, comparison of treatment effects between subgroups remain valid. In the ASCENT-COPD study, aclidinium was shown to be non-inferior to placebo for MACE risk. Finally, exacerbation history in the year prior to recruitment was ascertained via taking patient history, and therefore was subject to recall bias and uncertainty; COPD exacerbations are frequently under-reported20 and some overlap in exacerbation history between groups cannot be excluded.
Conclusion
In this pre-specified subgroup analysis of the ASCENT-COPD study of patients with moderate-to-very severe COPD and increased CV risk, patients with a history of COPD exacerbation were found to have increased CV risk, compared with patients who had no prior exacerbations. However, there was no safety signal to suggest increased risk of MACE or mortality due to aclidinium vs placebo, irrespective of exacerbation history. In addition, treatment with aclidinium reduced the rate of COPD exacerbations in patients, regardless of exacerbation history.
Aclidinium may be used to prevent future COPD exacerbations in patients with moderate-to-very severe COPD and increased CV risk without increased risk of MACE or mortality, regardless of exacerbation history.
Abbreviations
A, aclidinium; CAT, COPD assessment test; CI, confidence interval; COPD, chronic obstructive pulmonary disease; CV, cardiovascular; FEV1, forced expiratory volume in 1 second; HR, hazard ratio; MACE, major adverse cardiovascular event; N, total number of patients; n, number of patients with events; P, placebo; RR, rate ratio; SD, standard deviation.
Data Sharing Statement
Data underlying the findings described in this manuscript, including individual deidentified participant data, protocols and clinical trial documents, may be obtained in accordance with AstraZeneca’s data-sharing policy (described at https://astrazenecagrouptrials.pharmacm.com/ST/Submission/Disclosure) through Vivli (https://vivli.org/).
Ethics Approval and Consent to Participate
The study was performed in accordance with the Declaration of Helsinki and Good Clinical Practice Guidelines. The trial protocol and informed consent procedures were approved by the institutional review board with controlling authority at each study site (see Supplementary Table 1 for further details). All participants provided written informed consent.
Acknowledgments
Editorial support, under the direction of the authors, was provided by Richard Knight, PhD, and Sarah Hoyle, PhD, CMC Connect, McCann Health Medical Communications, and funded by AstraZeneca in accordance with Good Publication Practice (GPP3) guidelines (Ann Intern Med. 2015;163:461-464).
Author Contributions
RAW had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The ASCENT-COPD study was initially funded by Forest Laboratories and later funded by AstraZeneca and Circassia. AstraZeneca was involved in data collection and interpretation, and the development and review of this manuscript. The decision to submit the manuscript for publication was made by the authors.
Disclosure
RAW reports personal fees from AstraZeneca during the conduct of the study; personal fees from AbbVie, Anaptsys Bio, AstraZeneca/MedImmune, Bristol Myers Squibb, Chimerix, Circassia, ContraFect, Galderma, GlaxoSmithKline, Kamada, Kinevant, Kiniksa, Merck, Novartis, Pneuma, Propeller Health, Pulmonx, Roche, Sunovion, and Verona, outside the submitted work; and research grants from AstraZeneca/MedImmune, Boehringer Ingelheim, and Pearl Therapeutics, outside the submitted work. KRC reports personal fees from AstraZeneca, Boehringer Ingelheim, CIHR-GSK Research Chair in Respiratory Health Care Delivery (UHN), CSL Behring, Genentech, Grifols, Kamada, Merck, Novartis, Roche, and Sanofi; and grants from Amgen, AstraZeneca, Bayer, Baxter, Boehringer Ingelheim, CSL Behring, Genentech, GlaxoSmithKline, Grifols, Kamada, Mereo Biopharma, Novartis, Regeneron, Roche, Sanofi, Shire, and Vertex, during the conduct of the study. BMS is a member of the TIMI Study Group which has received institutional research grant support through Brigham and Women’s Hospital from Abbott, Amgen, Aralez, AstraZeneca, Bayer HealthCare Pharmaceuticals, Inc., BRAHMS, Daiichi-Sankyo, Eisai, GlaxoSmithKline, Intarcia, Janssen, MedImmune, Merck, Novartis, Pfizer, Poxel, Quark Pharmaceuticals, Roche, Takeda, The Medicines Company, and Zora Biosciences. He reports consulting fees from AbbVie, Allergan, AstraZeneca, Boehringer Ingelheim, Eisai, Elsevier Practice Update Cardiology, Esperion, Hamni, Lexicon, Medtronic, Merck, NovoNordisk, outside the submitted work; grants from Eisai, Merck, Novartis, NovoNordisk, and Pfizer Inc, outside the submitted work; and equity in Health[at]Scale. SZD and EG-G are employees of AstraZeneca. DL is an employee of PHASTAR and former consultant statistician to AstraZeneca. The authors report no other conflicts of interest in this work.
References
1. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. 2020. Available from: https://goldcopd.org/wp-content/uploads/2019/11/GOLD-2020-REPORT-ver1.0wms.pdf.
2. Hoogendoorn M, Feenstra TL, Boland M, et al. Prediction models for exacerbations in different COPD patient populations: comparing results of five large data sources. Int J Chron Obstruct Pulmon Dis. 2017;12:3183–3194.
3. Lipson DA, Barnhart F, Brealey N, et al. Once-daily single-inhaler triple versus dual therapy in patients with COPD. N Engl J Med. 2018;378(18):1671–1680.
4. Donaldson GC, Seemungal TA, Bhowmik A, Wedzicha JA. Relationship between exacerbation frequency and lung function decline in chronic obstructive pulmonary disease. Thorax. 2002;57(10):847–852.
5. Halpin DMG, Decramer M, Celli BR, Mueller A, Metzdorf N, Tashkin DP. Effect of a single exacerbation on decline in lung function in COPD. Respir Med. 2017;128:85–91.
6. Donaldson GC, Hurst JR, Smith CJ, Hubbard RB, Wedzicha JA. Increased risk of myocardial infarction and stroke following exacerbation of COPD. Chest. 2010;137(5):1091–1097.
7. Halpin DM, Decramer M, Celli B, Kesten S, Leimer I, Tashkin DP. Risk of nonlower respiratory serious adverse events following COPD exacerbations in the 4-year UPLIFT(R) trial. Lung. 2011;189(4):261–268.
8. Rothnie KJ, Yan R, Smeeth L, Quint JK. Risk of myocardial infarction (MI) and death following MI in people with chronic obstructive pulmonary disease (COPD): a systematic review and meta-analysis. BMJ Open. 2015;5(9):e007824.
9. Rothnie KJ, Connell O, Mullerova H, et al. Myocardial infarction and ischaemic stroke after exacerbations of chronic obstructive pulmonary disease. Ann Am Thorac Soc. 2018;15(8):935–946.
10. Suissa S, Dell’Aniello S, Ernst P. Long-term natural history of chronic obstructive pulmonary disease: severe exacerbations and mortality. Thorax. 2012;67(11):957–963. doi:10.1136/thoraxjnl-2011-201518
11. Soler-Cataluña JJ, Martínez-García MA, Román Sánchez P, Salcedo E, Navarro M, Ochando R. Severe acute exacerbations and mortality in patients with chronic obstructive pulmonary disease. Thorax. 2005;60(11):925–931. doi:10.1136/thx.2005.040527
12. Rothnie KJ, Müllerová H, Smeeth L, Quint JK. Natural history of chronic obstructive pulmonary disease exacerbations in a general practice–based population with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2018;198(4):464–471. doi:10.1164/rccm.201710-2029OC
13. AstraZeneca UK Ltd. Eklira Genuair Summary of Product Characteristics. 2017. Available from: https://www.ema.europa.eu/en/documents/product-information/eklira-genuair-epar-product-information_en.pdf.
14. AstraZeneca PLC. Prescribing information Tudorza® Pressair® (aclidinium bromide 400 µg inhalation powder).
15. Wise RA, Chapman KR, Scirica BM, et al. Effect of aclidinium bromide on major cardiovascular events and exacerbations in high-risk patients with chronic obstructive pulmonary disease: the ASCENT-COPD randomized clinical trial. JAMA. 2019;321(17):1693–1701. doi:10.1001/jama.2019.4973
16. Tashkin DP, Celli B, Senn S, et al. A 4-year trial of tiotropium in chronic obstructive pulmonary disease. N Engl J Med. 2008;359(15):1543–1554. doi:10.1056/NEJMoa0805800
17. Sethi S, Kerwin E, Watz H, et al. AMPLIFY: a randomized, Phase III study evaluating the efficacy and safety of aclidinium/formoterol vs monocomponents and tiotropium in patients with moderate-to-very severe symptomatic COPD. Int J Chron Obstruct Pulmon Dis. 2019;14:667–682.
18. Wise RA, Chapman KR, Scirica BM, et al. Long-term evaluation of the effects of aclidinium bromide on major adverse cardiovascular events and COPD exacerbations in patients with moderate to very severe COPD: rationale and design of the ASCENT COPD study. Chronic Obstr Pulm Dis. 2018;5(1):5–15.
19. Halpin DMG, Tashkin DP, Celli BR, Leimer I, Metzdorf N, Decramer M. Effect of tiotropium on outcomes in patients with COPD, categorized using the new GOLD Grading System: results of the UPLIFT(R) Randomized controlled trial. Chronic Obstr Pulm Dis. 2015;2(3):236–251.
20. Barnes N, Calverley PM, Kaplan A, Rabe KF. Chronic obstructive pulmonary disease and exacerbations: patient insights from the global Hidden Depths of COPD survey. BMC Pulm Med. 2013;13:54.
 © 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2021 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.