Back to Journals » Infection and Drug Resistance » Volume 15
Talaromyces marneffei is the Persistent Overwhelming Bloodstream Infection Pathogen Among HIV Inpatients in Fujian, China
Authors Lai J, Liu Y, Ye H, Chen Y
Received 28 June 2022
Accepted for publication 25 August 2022
Published 5 September 2022 Volume 2022:15 Pages 5207—5214
DOI https://doi.org/10.2147/IDR.S379100
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Suresh Antony
Jinglan Lai,1 Yuming Liu,2 Hanhui Ye,1 Yahong Chen1
1Department of Infectious Diseases, Mengchao Hepatobiliary Hospital of Fujian Medical University, Fuzhou, People’s Republic of China; 2Department of Anesthesiology, MengChao Hepatobiliary Hospital of Fujian Medical University, Fuzhou, People’s Republic of China
Correspondence: Yahong Chen; Hanhui Ye, Department of Infectious Diseases, Mengchao Hepatobiliary Hospital of Fujian Medical University, No. 312, Xihong Road, Fuzhou, Fujian, People’s Republic of China, Tel +86 591 88116119, Fax +86 591 88116105, Email [email protected]; [email protected]
Purpose: This study aimed to investigate the epidemiology and etiological spectrums of BSI in Fujian over the past 6 years in the post antiretroviral treatment (ART) era.
Methods: A retrospective, observational study was conducted to include positive BSI inpatients with HIV between September 2015 and August 2021 in Mengchao Hepatobiliary Hospital of Fujian Medical University, the largest designated HIV/AIDS care hospital in Fujian, China. Demographic data and laboratory data including gender, age, blood cell counts, biochemistry results, CD4 and CD8 cell counts, HIV-RNA loads, pathogen isolates, procalcitonin (PCT) levels and c-reactive protein (CRP) levels were collected. Continuous variables were expressed as median (range) and Kruskal–Wallis or Mann–Whitney test was used to analyze the differences between groups. Categorical data were expressed as numbers (percentage) and the differences between groups were analyzed by Pearson’s chi-squared test.
Results: In total, 3681 HIV inpatients with blood culture data were included and 683 strains identified from 646 inpatients were further analyzed. The median age of patients was 38 years and male accounted for 86.84%. The pooled prevalence of BSI was 18.55% (12.01%– 22.36% during the six-year period). The overall isolated rate of Talaromyces marneffei (TM) in blood culture was 12.42% (8.3%– 15.00% during the study period). TM was the persistent dominant BSI pathogen from 2015 to 2021 (accounting for 63.04% to 71.43%), followed by Cryptococcus neoformans (responsible for 10.00% to 20.83%). Compared to patients with other organisms BSI, those with TM BSI were younger and had lower CD4 counts, WBC counts, HB and CRP level, but higher HIVRNA loads.
Conclusion: BSI is still a major problem in the post ART era in hospitalized patients with HIV/AIDS in Fujian, China. TM is the predominant pathogen. This underlines the importance of an early diagnosis of opportunistic pathogen to avoid BSI in HIV-infected populations with a low immune status.
Keywords: HIV, bloodstream infection, epidemiology, etiology, Talaromyces marneffei
Introduction
The occurrence rate and patterns of BSI in HIV patients heavily depend on geographical areas and ART.1 The positive rate of BSI is usually higher in Africa where Mycobacterium tuberculosis, Cryptococcus neoformans and Salmonella spp. are important pathogens in HIV patients.2,3 The incidence rate of BSI is moderate in Southeast Asia such as Thailand, Vietnam and South China where TM and Mycobacteria have been becoming more common.4–6 Bacteremia is the leading BSI, while fungemia and mycobacteremia are less frequent in developed regions, where Staphylococci spp. and Streptococcus spp. are the prevalent isolates.7–9
In addition, many HIV patients have become older in the post ART era, and comorbidities such as diabetes, hypertension, cardiovascular disease, chronic kidney disease, and non-AIDS defining tumors are increasing in these patients.10,11 The etiological spectrums of BSI will also be anticipated to change over time. Some studies show important changes in the etiology and prognosis of BSI in recent years.1,5
What is more important, BSI still remains severe disease with a heavy burden in terms of morbidity and mortality in HIV-infected individuals.9,11–13 And reports available on BSI are usually restricted to small sample size and short-period of time.
There is no study on the incidence and patterns of BSI over time using large sample size of patients with HIV in Fujian, China. To describe the epidemiology and etiology of BSI in local region is crucial to manage and treat patients successfully. This study aimed to investigate whether there are any specific patterns in the incidence and etiology of BSI among HIV hospitalized patients in Fujian.
Methods
Ethical Consideration
The study was approved by the ethics committee of Mengchao Hepatobiliary Hospital of Fujian Medical University (The Ethics approval reference number: 2022_015_01). This study was performed retrospectively and data were anonymously used through electronic medical records. All information about the patients was kept confidential. All procedures were carried out in compliance with the Helsinki Declaration. Thus, patient informed consent was waived.
Study Design and Population
HIV inpatients with blood culture data were retrospectively included in Mengchao Hepatobiliary Hospital of Fujian Medical University, in China, from September 2015 to August 2021. The patients with positive blood isolates were further analyzed.
Data Collection
Data including age, gender, HIVRNA loads, CD4 counts, CD8 counts, complete blood counts, blood chemistry results, PCT levels, CRP levels and organism isolates were carefully collected from medical records for each individual. All data were carefully checked after abstraction.
Laboratory Methods
Clinical signs such as temperature >38°or <36 ◦C, white cell count >12,000 cells/mm3 or <4000 cells/mm3, tachycardia, tachypnea were evidence of suspected BSI. Venous blood samples were collected from each patient (2 sites, 2x10mL for aerobic bacteria, 10mL for fungus and 10mL for mycobacteria). Specimens for bacterial culture were incubated in the BACT/ALERT® 3D system (bioMérieux, USA) for 7 days, fungal culture in the BACTECTM FX system (BD, USA) for 14 days and mycobacterium culture in the BACTEC MGIT 960 system (BD, USA) for 42 days, or until the instrument automatically reported organisms growth. Positive bacterial cultures were Gram stained and subcultured onto plates with blood, then identified by the VITEK MS system (bioMerieux, USA). TM was inoculated onto Sabouraud′s dextrose agar plates and identified by its dimorphic character (cell shape from mycelium at 25°C to yeast-like form at 37°C). Candida was inoculated onto chromogenic agars and identified by different colors and biochemical tests. Cryptococcus neoformans and Aspergillus were also subcultured onto Sabouraud′s dextrose agar plates, further identified by biochemical tests and automatic identification systems. Mycobacterium were subcultured onto Roche culture media and then detected by an MPB64-based immunochromatographic assay. Isolates expressing the protein MPB64 were defined as MTB, otherwise regarded as NTM.
Definition
BSI diagnosis criteria were as follows: blood cultures positive for bacteria, mycobacteria, or fungi with clinically apparent signs and symptoms of sepsis. Unless isolated from more than one separate blood culture with the same antibiogram and obviously clinical symptoms, Corynebacterium spp., Bacillus spp., Micrococcus spp., coagulase negative Staphylococcus (CoNS), Sphingomonas paucimobilis, Propionibacterium spp. and Kocuria spp. were considered as contaminants, or if doctors did not initiate treatment, believing that they were not true pathogenic strains. Repeated positive blood cultures for the same pathogen were regarded as one in this study. Polymicrobial BSI was defined as isolation of more than one species from the same blood culture sets.
Data Analysis
We used SPSS16.0 software (SPSS Inc., Chicago, USA) to analyze data. Continuous variables expressed as median (ranges) were compared using Kruskal–Wallis or Mann–Whitney test. Categorical data were expressed as numbers (percentages) and the differences between groups were analyzed by Pearson’s chi-squared or Fisher’s exact test. A P-value less than 0.05 was considered to be of statistical significance (two sides).
Results
A total of 4282 HIV/AIDS patients were admitted to Mengchao Hepatobiliary Hospital of Fujian Medical University between September 2015 and August 2021. Among them, 3681 hospitalized patients were conducted with blood culture. Finally, 683 true strains in 646 inpatients were analyzed (Figure 1).
 |
Figure 1 Flow chart of bloodstream infections screening. |
Basic characteristics in 646 patients with positive blood culture are shown in Table 1. The median age was 38 years in these patients, 86.84% of whom was male. Ninety-five percent of patients had CD4 counts less than 200 cells/µL and 65.33% of them had a load of HIVRNA >1×105IU/mL (Table 1).
 |
Table 1 Baseline Characteristics in HIV Hospitalized Patients with Bloodstream Infection (N = 646) |
Six hundred and forty-six (17.55%) HIV hospitalized patients were found with positive blood culture. Thirty-four (0.92%) patients were polymicrobial. The overall contamination rate was 1.71% (Table 2). The total isolated rate of microorganisms in blood culture was 18.55%, in which the lowest rate was 12.01% in 2018 and the highest rate was 22.36% in 2016 (Table 3). The incidence of TM BSI ranged from 8.3% to 15.00% in this period (Table 3). The most prevalent strain was TM which was responsible for 66.91% of the pathogens (Table 4).
 |
Table 2 Characteristics of Bloodstream Infection Among Inpatients with HIV |
 |
Table 3 The Isolation Rate of Microorganisms in Bloodstream Infection Patients |
 |
Table 4 The Composition of Microorganisms Isolated from Blood Culture (N = 683) |
Patients with TM BSI had lower HB level, WBC counts and CRP level than those with other pathogens BSI (P < 0.001, P = 0.004, P = 0.012, respectively). The proportion of patients with age <50 years was also lower in TM group (P < 0.001). The proportion of individuals with CD4<200cells/µL or HIVRNA >1× 104IU/mL was higher in TM group (both P < 0.001) (Table 5).
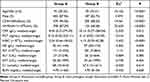 |
Table 5 Comparison Between Patients with TM BSI and Other Pathogens BSI |
Discussion
We performed a 6-year retrospective study (2015–2021) to investigate the prevalence and etiology of BSI in patients with HIV in Mengchao Hepatobiliary Hospital of Fujian Medical University. To our best knowledge, this was the largest sample size of study on BSI over a long period of time among HIV patients in Fujian, China.
There are several important findings in this study. Firstly, the results showed that the incidence of BSI in HIV patients still remains high in the post ART era in Fujian, China. Secondly, the study demonstrated that TM accounts for the vast majority isolates of BSI in HIV patients in Fujian. Finally, the results revealed that patients with TM BSI are more likely to have lower CD4 level, WBC counts and HB level, but higher HIVRNA loads than those with other pathogens BSI.
The BSI rate in our study was similar to the results showed by Artico et al, which was 13.5%.14 However, our result was higher than the findings reported in Shanghai, Italy and Portugal, which were 9.38%, 5.8% and 6.8%, respectively.6,13,15 On the contrary, the positive rate in blood culture in our study was much lower than the results demonstrated in Africa, which were 28% and 34.5%, respectively.16,17 Obviously, there is a significant variation in BSI rate among different countries and even among different regions within the same country. It is primarily attributed to differences in the geographical distribution of pathogens, ART accessibility and economic development.
We found that fungemia was the overwhelming BSI and TM continued to be the dominant isolated pathogen among HIV-infected patients in Fujian in recent years. Similarly, a study reported that Cryptococcus neoformans was the most common stain followed by TM.6 TM has been increasing concurrently with HIV prevalence in Thailand and Vietnam.5 In Spain, Common causative fungi were Candida and Cryptococcus neoformans in HIV patients.12,18 In contrast, Staphylococci spp., Streptococcus pneumoniae and Enterobacterium were found to be the leading organisms in Taiwan, Belgium, Italy and Portugal.7,9,11,13 However, studies showed a higher rate of Salmonella, Mycobacteria, and Cryptococci species conducted in the developing settings, particularly in Africa and Southeast Asia.3–5
Our results can be explained as follows: on one hand, Fujian located in Southeast China, is the TM endemic region.19,20 The burden of TM infection in South China is heavy.21 On the other hand, HIV was diagnosed at a late stage in most of these patients, who had low CD4 counts and were easy to suffer TM. Compared to patients with other pathogens, those with TM BSI had lower WBC counts, HB level and CD4 counts, but higher HIV RNA loads. Thus, it still needs to further conduct HIV counseling and testing services to promote individuals with HIV to test and treat early.
Mycobacteria BSI may have been underestimated due to various results: insufficient blood samples, contaminated specimens, culture skills of being further improved and patients might have been treated with fluoroquinolone antibiotics in other medical institutions before sampling. So, the positive rate of Mycobacteria was very low in this study. It increased slightly in recent years due to the improvement of culture technique. Yet, we still regard these organisms as an important public health problem in Fujian, China. Efforts are needed to enhance our awareness and culture technique.
With the economic development and the improvement of people’s life, safe food and water have been well supplied in China in past decades. This contributes to the low rate of BSI due to Enterobacterium such as E. coli and Salmonella spp. in this study.
Some reports demonstrated that Staphylococcus spp. were the common organisms due to high proportion of drug users or nosocomial in origin.10,22 While the drug users were very few and patients with contaminated Cons were excluded in our study. Therefore, the Staphylococcus spp. BSI was less common in this study. As to Candida, we also found that candidemia was rare. It could be attributed to the fact that patients acquired BSI almost from community in this study. While Candida infection usually occurs in hospitals, and especially in intensive care units.10,12,13
Streptococcus spp. is found to be one of the most prevalent causes of BSI worldwide.23 Nevertheless, Streptococcus spp. only accounted for 0.11% in our study. It is consistent with the result reported in Shanghai, China, which showed 2.2%.6 One possible explanation is that HIV is diagnosed at a late stage in large proportion of HIV patients in China and the patients therefore have low CD4 counts and late-stage AIDS.24,25 Opportunistic pathogens were the overwhelming etiology among HIV patients in China.
This study has some limitations: firstly, it is a retrospective study; thus, potential confounders cannot be ruled out. In addition, it is a single center study and the results are more appropriate to guide local physicians.
Conclusion
BSI remains a major concern in the post ART era in these patients. Fungus, especially TM is the predominant pathogen in Fujian, China. It seems to be related to a poor viro-immunological status in these patients. This emphasizes the importance of an early HIV diagnosis and early onset ART. Physicians should improve the awareness of opportunistic pathogens to avoid BSI in these patients.
Funding
This study was funded by grants from Natural Science Foundation of Fujian Province (grant no. 2020J011165 and 2021J011295).
Disclosure
Dr Jinglan Lai, Mr Yuming Liu, Professor Hanhui Ye and Mrs Yahong Chen report grants from Natural Science Foundation of Fujian Province, during the conduct of the study. The authors declare that they have no other competing interests.
References
1. Taramasso L, Tatarelli P, Di Biagio A. Bloodstream infections in HIV-infected patients. Virulence. 2016;7(3):320–328. doi:10.1080/21505594.2016.1158359
2. Jemal M, Deress T, Belachew T, Adem Y. Antimicrobial resistance patterns of bacterial isolates from blood culture among HIV/AIDS patients at Felege Hiwot Referral Hospital, Northwest Ethiopia. Int J Microbiol. 2020;2020:8893266. doi:10.1155/2020/8893266
3. Crump JA, Ramadhani HO, Morrissey AB, et al. Invasive bacterial and fungal infections among hospitalized HIV-infected and HIV-uninfected adults and adolescents in northern Tanzania. Clin Infect Dis. 2011;52(3):341–348. doi:10.1093/cid/ciq103
4. Kiertiburanakul S, Watcharatipagorn S, Chongtrakool P, Santanirand P. Epidemiology of bloodstream infections and predictive factors of mortality among HIV-infected adult patients in Thailand in the era of highly active antiretroviral therapy. Jpn J Infect Dis. 2012;65(1):28–32. doi:10.7883/yoken.65.28
5. Nga TV, Parry CM, Le T, et al. The decline of typhoid and the rise of non-typhoid salmonellae and fungal infections in a changing HIV landscape: bloodstream infection trends over 15 years in southern Vietnam. Trans R Soc Trop Med Hyg. 2012;106(1):26–34. doi:10.1016/j.trstmh.2011.10.004
6. Qi T, Zhang R, Shen Y, et al. Etiology and clinical features of 229 cases of bloodstream infection among Chinese HIV/AIDS patients: a retrospective cross-sectional study. Eur j Clin Microbiol Infect Dis. 2016;35(11):1767–1770. doi:10.1007/s10096-016-2724-7
7. Lee CC, Chou YJ, Lin JN, et al. Clinical predictors of the leading pathogens in human immunodeficiency virus-infected adults with community-onset bacteremia in the emergency department: the importance of transmission routes. J Microbiol Immunol Infect. 2018;51(3):392–400. doi:10.1016/j.jmii.2016.08.001
8. Yehia BR, Fleishman JA, Wilson L, Hicks PL, Gborkorquellie TT, Gebo KA. Incidence of and risk factors for bacteraemia in HIV-infected adults in the era of highly active antiretroviral therapy. HIV Med. 2011;12(9):535–543. doi:10.1111/j.1468-1293.2011.00919.x
9. Declercq S, De Munter P, Derdelinckx I, et al. Characteristics, causes, and outcome of 54 episodes of bloodstream infections in a cohort of HIV patients. Infect Dis. 2015;47(9):611–617. doi:10.3109/23744235.2015.1033002
10. Taramasso L, Liggieri F, Cenderello G, et al. Bloodstream infections in patients living with HIV in the modern cART era. Sci Rep. 2019;9(1):5418. doi:10.1038/s41598-019-41829-3
11. Franceschini E, Santoro A, Menozzi M, et al. Epidemiology and outcomes of bloodstream infections in HIV-patients during a 13-year period. Microorganisms. 2020;8(8):1210. doi:10.3390/microorganisms8081210
12. Ortega M, Almela M, Soriano A, et al. Bloodstream infections among human immunodeficiency virus-infected adult patients: epidemiology and risk factors for mortality. Eur j Clin Microbiol Infect Dis. 2008;27(10):969–976. doi:10.1007/s10096-008-0531-5
13. De Matos A, Lopes SB, Serra JE, Ferreira E, da Cunha JS. Mortality predictive factors of people living with human immunodeficiency virus and bloodstream infection. Int J Infect Dis. 2021;110:195–203. doi:10.1016/j.ijid.2021.06.032
14. Artico MJ, Rocchi M, Gasparotto A, et al. Community-acquired bacteremia in adult patients attending the emergency service of a teaching hospital. Rev Argent Microbiol. 2012;44(1):10–15. doi:10.1590/S0325-75412012000100003
15. Bonadio M, Gigli C, Maccanti O, Longo B, Smorfa A. Bloodstream infections in HIV-positive patients: a review of sixty-eight episodes. J Chemother. 1998;10(3):243–247. doi:10.1179/joc.1998.10.3.243
16. Bell M, Archibald LK, Nwanyanwu O, et al. Seasonal variation in the etiology of bloodstream infections in a febrile inpatient population in a developing country. Int J Infect Dis. 2001;5(2):63–69. doi:10.1016/S1201-9712(01)90027-X
17. Reddy EA, Shaw AV, Crump JA. Community-acquired bloodstream infections in Africa: a systematic review and meta-analysis. Lancet Infect Dis. 2010;10(6):417–432. doi:10.1016/S1473-3099(10)70072-4
18. López Moral L, Tiraboschi IN, Schijman M, Bianchi M, Guelfand L, Cataldi S. Fungemia in hospitals of the city of Buenos Aires, Argentina. Rev Iberoam Micol. 2012;29(3):144–149. doi:10.1016/j.riam.2011.11.001
19. Lai JL, Chen YH, Liu YM, et al. Prevalence and risk factors of anaemia in hospitalized HIV-infected patients in southeast China: a retrospective study. Epidemiol Infect. 2019;147:e81. doi:10.1017/S0950268818003618
20. Cao C, Xi L, Chaturvedi V. Talaromycosis (penicilliosis) due to talaromyces (penicillium) marneffei: insights into the clinical trends of a major fungal disease 60 years after the discovery of the pathogen. Mycopathologia. 2019;184(6):709–720. doi:10.1007/s11046-019-00410-2
21. Qin Y, Huang X, Chen H, et al. Burden of Talaromyces marneffei infection in people living with HIV/AIDS in Asia during ART era: a systematic review and meta-analysis. BMC Infect Dis. 2020;20(1):551. doi:10.1186/s12879-020-05260-8
22. Wang JT, Sheng WH, Chen MY, et al. Nosocomial bloodstream infection in human immunodeficiency virus-infected patients in Taiwan: descriptive epidemiology and risk factors for mortality. J Formosan Med Assoc. 2004;103(10):743–748.
23. Calik Basaran N, Ascioglu S. Epidemiology and management of healthcare-associated bloodstream infections in non-neutropenic immunosuppressed patients: a review of the literature. Therap Adv Infect Dis. 2017;4(6):171–191. doi:10.1177/2049936117733394
24. Jin X, Xiong R, Wang LY, Mao YR. Analysis on the ‘late diagnosis’ (LD) phenomena among newly identified HIV/AIDS cases in China, 2010–2014. Zhonghua Liu Xing Bing Xue Za Zhi. 2016;37(2):218–221. doi:10.3760/cma.j.issn.0254-6450.2016.02.014
25. Yue Q, Liu YF, Li J, Zang CP. Analysis on late HIV diagnosis among newly reported human immunodeficiency virus/acquired immunodeficiency syndrome cases between 2009 and 2017 in medical institutions. Zhonghua Yu Fang Yi Xue Za Zhi. 2018;52(12):1248–1253. doi:10.3760/cma.j.issn.0253-9624.2018.12.011
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
