Back to Journals » International Journal of General Medicine » Volume 16
Viral and Atypical Pathogen’s Epidemiology of a Large Cohort of Patients with Acute Respiratory Tract Infections in Shaanxi Province, Northwest China
Authors Liu X, Li M, Yang T , He R , Guo X, Chen M
Received 3 December 2022
Accepted for publication 7 April 2023
Published 5 May 2023 Volume 2023:16 Pages 1671—1679
DOI https://doi.org/10.2147/IJGM.S400118
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Xinyu Liu,1,* Meng Li,1,* Tian Yang,1 Ruiqing He,1 Xuan Guo,2 Mingwei Chen1
1The Department of Respiratory and Critical Care Medicine of the First Affiliated Hospital of Xi’an Jiaotong University, Xi’an, Shaanxi, People’s Republic of China; 2Laboratory Department of the First Affiliated Hospital of Xi’an Jiaotong University, Xi’an, Shaanxi, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Mingwei Chen, The Department of Respiratory and Critical Care Medicine of the First Affiliated Hospital of Xi’an Jiaotong University, 277 West Yanta Road, Xi’an, Shaanxi, People’s Republic of China, Email [email protected]
Purpose: To analyze and summarize the etiological and epidemiological characteristics of acute respiratory tract infections (ARIs) in northwest China to improve the clinical management and prevention of local ARIs.
Methods: Patients with ARIs in Shaanxi Province, from January 2014 to December 2018, were retrospectively analyzed. Indirect immunofluorescence assay (IFA) was used to detect the IgM antibody of eight respiratory pathogens.
Results: A total of 15,543 eligible patients were included in this study. Overall, 36.01% of the patients (5597/15543) were positive for at least one of eight pathogens, among which single and mixed infections accounted for 74.65% (4178/5597) and 25.35% (1419/5597), respectively. Mycoplasma (MP) showed the highest detection rate (18.12%), followed by influenza virus B (Flu B, 11.65%), chlamydia (CP, 7.00%), respiratory syncytial virus (RSV, 4.18%), parainfluenza virus (PIV, 2.83%), influenza virus A (Flu A, 1.69%), legionella (LP, 1.00%) and adenovirus (ADV, 0.70%). Flu B (17.54%, 759/4327) was the most prevalent virus in patients aged less than 18 years. In addition, common respiratory infections with higher detection rates were found in autumn (39.65%), followed by winter (37.37%), summer (36.21%) and spring (30.91%). There were significant differences in the detection rates of pathogens in different seasons (P < 0.001).
Conclusion: These findings serve as a reference for local health authorities to develop further plans for the prevention and control of ARIs.
Keywords: acute respiratory tract infections, respiratory viruses, atypical pathogens, epidemiology, etiology
Introduction
Acute respiratory tract infections (ARIs) are a global public health issue due to their high morbidity and mortality, especially in infants and children.1–4 Pathogens affect the upper and lower respiratory tracts, leading to diseases such as pharyngitis, laryngitis, bronchitis, and pneumonia.2 Respiratory syncytial virus (RSV), influenza virus A (Flu A), influenza virus B (Flu B), parainfluenza virus (PIV) and adenovirus (ADV) are considered to be the common pathogens of most ARIs.5 RSV is the leading cause of severe lower respiratory tract infections (LRTIs) in infants and young children,6,7 while influenza viruses (IFVs) are the main pathogens causing LRTIs in hospitalized adults.8 In addition, with the increase of antibiotic resistance rate and the development of pathogen detection technology, the research on mycoplasma (MP), chlamydia (CP), legionella (LP) and other atypical pathogens is gradually deepening, and their role in respiratory tract infections has aroused people’s attention.9–11
Respiratory viruses and atypical pathogens have differences in spatial, temporal and population distribution. Although several epidemiological studies on ARIs have been reported in other parts of China and other countries, the epidemiological characteristics of common pathogens of ARIs are different due to factors such as inclusion criteria, climate, environmental pollution and population.12–18 Moreover, most of these studies only conducted epidemiological analysis on children or single pathogens, and did not include atypical pathogens and northwest China, the target of this study.
As a core city in northwest China, the spread and prevalence of respiratory diseases are more likely to occur in Xi’an due to its rapid industrial development, large floating population, serious environmental pollution, etc. Thus, the epidemiology of viral and atypical pathogen's etiologies associated with ARIs in Xi’an, Shaanxi Province, were investigated in this study in order to provide basic data on etiologies of ARIs for disease prevention, control, clinical diagnosis and treatment.
Methods
Subjects and Data Collection
A total of 15,543 patients with ARIs admitted to the department of respiratory medicine and pediatrics of the First Affiliated Hospital of Xi‘an Jiaotong University, Shaanxi, China, from January 2014 to December 2018, were enrolled in the study, including upper and lower respiratory tract infections, such as sinusitis, tonsillitis, acute bronchitis, pneumonia, bronchiectasis with infection, acute exacerbation of chronic obstructive pulmonary disease, acute attack of bronchial asthma, lung cancer with infection, and pneumoconiosis with infection, etc.
The diagnosis for each enrolled patient was made by physicians and based on standard clinical criteria. All patients enrolled in this study must meet the following characteristics: (1) at least one of the following conditions: fever (≥37.5 °C), chills, leukocytosis (white blood cell count >10×109/L) or leukopenia (white blood cell count <4×109/L); (2) must have at least one of the following signs/symptoms: rhinorrhea, nasal congestion, throat pain, cough, the presence of sputum, shortness of breath, dyspnea, lung auscultation abnormality (rale or wheeze) and chest pain. Baseline, examination data and relevant information were extracted from the Electronic Medical Records. This study was approved by the Ethics Review Committee of the First Affiliated Hospital of Xi‘an Jiaotong University, and informed consent was waived because it was a non-traumatic and non-interventional retrospective study that only collected patients’ basic clinical information and examination data. We are in strict compliance with the Helsinki Declaration and all patient data will be kept strictly confidential.
Detection of Respiratory Pathogens
PNEUMOSLIDE IgM kit (VIRCELL PNEUMOSLIDE; Vircell, Granada, Spain) was used to detect IgM antibodies from the clinical samples. The detected respiratory viruses included Flu A, Flu B, ADV, PIV (serum types 1, 2 and 3), RSV, MP, CP and LP.
Statistical Analysis
SPSS 18.0 statistical software (SPSS Inc, Chicago, IL) and Microsoft Excel (Microsoft Corp., Redmond, WA) were used for data analysis, Mann–Whitney U-test or t-test were used to compare the measurement data of the two groups and comparison of measurement data in more than two groups used Kruskal–Wallis H-test or ANOVA test. The chi-square tests were used to compare the positive detection rate of various pathogens in the respiratory tract in different groups. P < 0.05 was considered to be statistically significant.
Results
Baseline Characteristics
A total of 15,543 patients with ARIs were collected in this study, including 9725 males (62.57% of total) and 5818 females (37.43% of total), with an average age 49.33 ± 19.31 years, the ages of the eligible patients were from 21 days to 87 years old. The subjects included 5701 (36.68%) upper respiratory infection (URTIs) and 9842 (63.32%) LRTIs, the baseline characteristics are shown in Table 1.
 |
Table 1 Demographic and Clinical Characteristics of Enrolled Patients with ARIs |
Overall Detection Rate of Eight Common Pathogens
As shown in Table 2, among the 15,543 samples, 5597 specimens carried at least one virus or atypical pathogen, with a positive detection rate of 36.01%, of which 4178 (74.65%) were single infection and 1419 (25.35%) were mixed infections. The most predominant pathogen was MP, with a detection rate of 18.12% (2816/15543), followed by Flu B (11.65%, 1811/15543), CP (7.00%, 1088/15543), RSV (4.18%, 649/15543), PIV (2.83%, 440/15543), Flu A (1.69%, 26/15543), LP (1.00%, 156/15543) and ADV (0.70%, 109/15543).
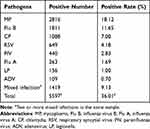 |
Table 2 Detection Rate of Eight Common Pathogens of ARIs |
Detection Rate of Virus and Atypical Pathogen from Different Gender Groups
As shown in Table 3, there was no significant difference in total positive detection rate between different genders (χ2 = 1.15, P = 0.284). However, the detection rate of Flu A, MP and ADV was significantly higher in males (Flu A: χ2= 6.90, P = 0.009; MP: χ2= 15.70, P < 0.001; ADV: χ2= 7.51, P = 0.006), the positive detection rate of PIV and mixed infection was higher in females (PIV: χ2= 22.34, P < 0.001; Mixed infection: χ2= 26.73, P < 0.001).
 |
Table 3 Detection Rate of Individual Pathogens in Different Gender Groups of ARIs |
Detection Rate of Viral and Atypical Pathogen from Different Age Groups
All of the ARIs patients are divided into four age groups, ages of <18, 18–45, 46–69 and >69, representing children and adolescents, young adults, middle-aged person and elderly adults. As shown in Table 4, the predominant pathogen among different age groups varied. In ages <18 years, Flu B (17.54%, 759/4327) was the most prevalent virus, followed by MP (10.98%, 475/4327) and RSV (8.20%, 355/4327). In ages 18–45, MP (33.76%, 1018/3014) had the highest incidence, followed by CP (7.53%, 227/3014) and Flu B (4.28%, 129/3014). In the groups of 46–69 years and >69 years, MP (middle-aged: 19.27%, 726/3767; elderly: 13.46%, 597/4435) was the most predominant pathogen. The positive detection rates of Flu A, Flu B, PIV, RSV and MP were significantly different in different age groups (Flu A: χ2=9.07, P =0.028, Flu B: χ2=9.72, P =0.021, PIV: χ2=22.83, P <0.001, RSV: χ2=86.8, P <0.001, MP: χ2=134.45, P <0.001), and all of them, except MP, were infected frequently in patients under 18 years old, and MP was most common in patients aged 18–45 years. In addition, the mixed infection rate (11.05%) of <18 years was significantly higher than that of other age groups.
 |
Table 4 Detection Rate of Individual Pathogens in Different Age Groups of ARIs |
Detection Rate of Virus and Atypical Pathogen from Different Season Groups
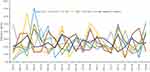
According to the meteorological division method, all the patients were divided into four groups: spring (March, April and May), summer (June, July and August), autumn (September, October and November) and winter (January, February and December). The results showed that the most common respiratory infection in northwest China was seasonal, with higher detection rates in autumn (39.65%, 1287/3246) followed by winter (37.37%, 1727/4622), summer (36.21%, 1439/3974) and spring (30.91%, 1144/3701), with significant differences in pathogen detection rates in different seasons (χ2= 64.17, P <0.001). Flu A, Flu B, ADV and MP were mainly detected in winter, PIV mostly occurred in spring, CP, LP and RSV were more infectious in autumn, mixed infections were more common in autumn and spring (Table 5, Figure 1). The detection rate of all pathogens in different seasons was statistically significant (P < 0.001).
 |
Table 5 Detection Rate of Individual Pathogens in Different Season Groups of ARIs |
Discussion
ARIs are the third leading cause of death in the world, causing a major medical care and economic burden.6 LRTIs are a significant source of morbidity and mortality, especially in children under 5 years old.19 Although viral infection is the dominant cause of ARIs, the proportion of infections with atypical pathogens is increasing due to the abuse of antibiotics and the development of detection technology.9–11 At present, several studies on the epidemiology and etiology of respiratory pathogens of children in different areas have been reported,7,16,20–23 however, the epidemiological and etiological data of ARIs in different regions and hospitals have not been systematically summarized. In addition, studies on ARIs both in hospitalized children and adults in northwest China are limited, This report analyzes the epidemiological characteristics of eight common pathogens in the northwest China, providing references for local disease prevention and clinical diagnosis and treatment.
The results of this study show that the top three most prevalent pathogens were MP (18.12%, 2816/5597), Flu B (11.65%, 1811/5597) and CP (7.00%, 1088/5597). The total positive detection rate is 36.01% (5597/15443) in Xi’an, which is similar with the previous study in Turkey (33.4%) and Shandong province in China (35.75%),12,18 and significantly higher than that reported in Beijing (5.64%), Shenzhen (14.55%), Suzhou (13.6%) and Gansu province in China (29.2%),13–16 but lower than that reported in north China (39.3%).17 The finding also illustrates that the mixed infections rate is 9.13% (1419/15543) in northwest China, which is significantly lower than that in Shandong province (15.67%),18 but higher than that in Beijing (2.13%), Gansu province (4.70%) and north China (7.6%).13,14,17
Similar to the studies in Turkey and other areas in China including Suzhou, Shandong and Gansu province,12,14,15,18 Flu B is the most common respiratory virus in Xi’an, Shaanxi, in which children are mainly infected. However, RSV, ADV and PIV are common in Shenzhen,16 RSV and rhinovirus infection are the main pathogens in north China.17 The dynamic changes in influenza viruses can explain this result. pdm01 of H1N1 influenza virus occupied a dominant position in 2010 due to the low antibody level and high susceptibility to infectious disease in the population.24 Influenza surveillance data also confirmed that influenza A H1N1 was the main strain in Shaanxi Province in 2012.25 After 2011, due to the limited immune cross-responsiveness between influenza subtypes, Flu B became the dominant strain in the infected population after 2012.24,25
By analyzing the detection of pathogens in different genders, we found that the positive rate in males (36.33%) was slightly higher than that in females (35.48%), but there was no significant difference between them, which was similar to the results of Shandong province,18 however, compared with males, women were more likely to have mixed infections, which may be attributable to pregnancy-related or hormone-related immune-suppression. Immune responses can be suppressed during the menstrual cycle and pregnancy.26,27
The analysis of pathogens detected in different age groups showed that the positive rate of the minor population was significantly higher than that of the middle aged and elderly, especially virally (Flu A, flu B, PIV, RSV) and with mixed infections. The infection rate of Flu B was the highest, followed by MP and RSV in minors (<18 years), which was similar to the previous research results in Turkey, eastern China and north China.12,14,18 It may be associated with immature immune systems in children and adolescents. What’s more, malnutrition, exposure to crowded conditions, indoor air pollution, lack of breastfeeding and low birth weight can increase the risk of ARIs in children.28 Our findings confirm that IFVs and RSV are an important health threat for minors in Xi’an, which highlights the need to develop effective vaccines and new methods of treatment to improve the treatment of virus infections in Xi’an.29
The difference of seasonal pathogens in ARIs may be related to a region’s climate and demographic factors. Our study finds that eight respiratory tract pathogens can be detected throughout the year, most of which have significantly higher circulation in autumn and winter. The detection rate is lowest in the spring and highest in the autumn in Xi’an, Shaanxi, China. Flu A, Flu B, RSV, ADV, MP and mixed infections are more common in autumn, LP infections are mainly in summer and autumn, this is different from previous studies in Shandong province and south China, which showed that the highest detection rates were in the spring or winter.18,30
Compared with previous studies, this study has the following advantages. First, a larger sample size is included in our study (15,543 samples). Second, epidemiological analysis of eight respiratory pathogens (Flu A, Flu B, PIV, RSV, ADV, MP, CP, LP) was conducted in Xi’an for the first time. Third, the etiology and epidemiology of ARIs in hospitalized children and adults were simultaneously analyzed. Four, the epidemiological characteristics of eight common respiratory pathogens in different genders, ages, seasons and infection sites are systematically analyzed, and the characteristics of pathogens under different classification conditions are summarized in detail. At the same time, this research also has certain limitations. First, sample selection is limited to the First Affiliated Hospital of Xi’an Jiaotong University, more samples from other hospitals in Xi’an were not included systematically and comprehensively, which may result in some bias. Second, epidemiological characteristics of other pathogens such as bacteria and fungi were not analyzed. Third, the detection technology adopts the traditional IFA method instead of multiple real-time fluorescence quantitative PCR.
Conclusion
The respiratory infections reveal significant regional and seasonal differences. Flu B and MP are the most common pathogens in ARIs in Xi’an. People younger than 18 years old are more likely to be infected with the virus, and MP infection is common in adults. Juveniles are the key protected objects due to high infection rates. In summary, the results of the current study provide important information for the etiology of ARIs in Shaanxi province, China, which may contribute to a reference for the health department to formulate further prevention and control plans of respiratory infections, and provide guidance for further research.
Abbreviations
ADV, adenovirus; ARIs, acute respiratory infection; CAP, community acquired pneumonia; CP, chlamydia pneumoniae; Flu A, influenza virus A; Flu B, influenza virus B; IFA, immunofluorescence assay; LP, legionella pneumophila; LRTIs, lower respiratory tract infection; MCT-PCR, multiple real-time fluorescence quantitative; MP, mycoplasma pneumoniae; PIV, parainfluenza virus; RSV, respiratory syncytial virus; URTIs, upper respiratory tract infection.
Data Sharing Statement
The datasets generated and/or analyzed during the current study are not publicly available due to other related research which is ongoing, but are available from the author on reasonable request.
Ethics Approval and Consent to Participate
This study was approved by the Ethics Review Committee of the First Affiliated Hospital of Xi‘an Jiaotong University, informed consent was waived for this non-traumatic retrospective study.
Acknowledgments
A preprint has previously been published.
Thanks to Dr. Jingming Yuan, Dr. Anqi Li and Dr. Jiejun Zhou from the Department of Respiratory and Critical Care Medicine of the First Affiliated Hospital of Xi’an Jiaotong University for their help in data sorting and data analysis; Thanks to Dr. Jing Wang from the Department of Pulmonary and Critical Care Medicine, Shaanxi Provincial Second People’s Hospital for her advice and help in the clinical research and design. Thanks to Professor Jun Lu from the School of Science, and School of Public Health and Interdisciplinary Studies, Faculty of Health & Environmental Sciences, Auckland University of Technology for his great support and guidance in the design guidance and translation of the paper.
Funding
Financial support was provided by National Science and Technology Major Project (2017ZX10103004), and the key research and Development Plan of Shaanxi Province (2020KW-044).
Disclosure
The authors declared no conflicts of interest in this work.
References
1. Roberts NL, Mountjoy-Venning WC, Anjomshoa M, Banoub JA, Yasin YJ. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the global burden of disease study 2017. Lancet. 2018;392:1789–1858. doi:10.1016/S0140-6736(18)32279-7
2. Troeger C, Forouzanfar M, Rao PC, et al. Estimates of the global, regional, and national morbidity, mortality, and aetiologies of lower respiratory infections in 195 countries, 1990–2016: a systematic analysis for the global burden of disease study 2016. Lancet Infect Dis. 2018;18:1191–1210. doi:10.1016/S1473-3099(18)30310-4
3. Bicer S, Giray T, Col D, et al. Virological and clinical characterizations of respiratory infections in hospitalized children. Ital J Pediatr. 2013;39(1):22. doi:10.1186/1824-7288-39-22
4. Williams BG, Gouws E, Boschi-Pinto C, et al. Estimates of world-wide distribution of child deaths from acute respiratory infections. Lancet Infect Dis. 2002;2:25–32. doi:10.1016/S1473-3099(01)00170-0
5. Pavia AT. Viral infections of the lower respiratory tract: old viruses, new viruses, and the role of diagnosis. Clin Infect Dis. 2011;52(Suppl 4):S284–289. doi:10.1093/cid/cir043
6. Shi T, McAllister DA, O’Brien KL, et al. Global, regional, and national disease burden estimates of acute lower respiratory infections due to respiratory syncytial virus in young children in 2015: a systematic review and modelling study. Lancet. 2017;390:946–958. doi:10.1016/S0140-6736(17)30938-8
7. Kini S, Kalal BS, Chandy S, et al. Prevalence of respiratory syncytial virus infection among children hospitalized with acute lower respiratory tract infections in Southern India. World J Clin Pediatr. 2019;8:33–42. doi:10.5409/wjcp.v8.i2.33
8. Troeger CE, Blacker BF, Khalil IA. Mortality, morbidity, and hospitalisations due to influenza lower respiratory tract infections, 2017: an analysis for the Global burden of disease study 2017. Lancet Respir Med. 2019;7:69–89. doi:10.1016/S2213-2600(18)30496-X
9. Guo DX, Hu WJ, Wei R, et al. Epidemiology and mechanism of drug resistance of Mycoplasma pneumoniae in Beijing, China: a multi-center study. Bosn J Basic Med Sci. 2019. doi:10.17305/bjbms.2019.4053
10. Cui J, Yan W, Xie H, et al. A retrospective seroepidemiologic survey of Chlamydia pneumoniae infection in patients in Beijing between 2008 and 2017. PLoS One. 2018;13:e0206995. doi:10.1371/journal.pone.0206995
11. Qin T, Zhou H, Ren H, et al. Combined use of real-time PCR and nested sequence-based typing in survey of human Legionella infection. Epidemiol Infect. 2016;144:2006–2010. doi:10.1017/S0950268815003301
12. Cicek C, Arslan A, Karakus HS, et al. Akut Solunum Yolu Enfeksiyonu Olan Hastalarda Solunum Viruslarının Prevalansı ve Mevsimsel Dağılımı, 2002-2014 [Prevalence and seasonal distribution of respiratory viruses in patients with acute respiratory tract infections, 2002–2014]. Mikrobiyol Bul. 2015;49:188–200. Turkish. doi:10.5578/mb.9024
13. Yao LH, Wang C, Wei TL, et al. Human adenovirus among hospitalized children with respiratory tract infections in Beijing, China, 2017–2018. Virol J. 2019;16:78. doi:10.1186/s12985-019-1185-x
14. Li X, Li J, Meng L, et al. Viral etiologies and epidemiology of patients with acute respiratory infections based on sentinel hospitals in Gansu Province, Northwest China, 2011–2015. J Med Virol. 2018;90:828–835. doi:10.1002/jmv.25040
15. Zhang WQ, Yu J, Chen LL, et al. 2016—2018 年苏州5岁以下儿童流感相关的严重急性呼吸道感染住院情况研究 [Hospitalization rates for influenza-associated severe acute respiratory illness in children younger than five years old in Suzhou of China, 2016–2018]. Zhonghua Yu Fang Yi Xue Za Zhi. 2019;53:1056–1059. Chinese. doi:10.3760/cma.j.issn.0253-9624.2019.10.019
16. Wang H, Zheng Y, Deng J, et al. Prevalence of respiratory viruses among children hospitalized from respiratory infections in Shenzhen, China. Virol J. 2016;13:39. doi:10.1186/s12985-016-0493-7
17. Yu J, Xie Z, Zhang T, et al. Comparison of the prevalence of respiratory viruses in patients with acute respiratory infections at different hospital settings in North China, 2012–2015. BMC Infect Dis. 2018;18:72. doi:10.1186/s12879-018-2982-3
18. Liu T, Li Z, Zhang S, et al. Viral Etiology of acute respiratory tract infections in hospitalized children and adults in Shandong Province, China. Virol J. 2015;12:168. doi:10.1186/s12985-015-0388-z
19. Rudan I, Chan KY, Zhang JS, et al. Causes of deaths in children younger than 5 years in China in 2008. Lancet. 2010;375:1083–1089. doi:10.1016/S0140-6736(10)60060-8
20. Yu J, Zhang X, Shan W, et al. Influenza-associated hospitalization in children younger than 5 Years of Age in Suzhou, China, 2011–2016. Pediatr Infect Dis J. 2019;38:445–452. doi:10.1097/INF.0000000000002178
21. Khuri-Bulos N, Lawrence L, Piya B, et al. Severe outcomes associated with respiratory viruses in newborns and infants: a prospective viral surveillance study in Jordan. BMJ Open. 2018;8:e021898. doi:10.1136/bmjopen-2018-021898
22. Ng KF, Tan KK, Sam ZH, et al. Epidemiology, clinical characteristics, laboratory findings and severity of respiratory syncytial virus acute lower respiratory infection in Malaysian children, 2008–2013. J Paediatr Child Health. 2017;53:399–407. doi:10.1111/jpc.13375
23. Kumar P, Medigeshi GR, Mishra VS, et al. Etiology of acute respiratory infections in infants: a prospective birth cohort study. Pediatr Infect Dis J. 2017;36:25–30. doi:10.1097/INF.0000000000001359
24. Wabwire-Mangen F, Mimbe DE, Erima B, et al. Epidemiology and surveillance of influenza viruses in Uganda between 2008 and 2014. PLoS One. 2016;11:e0164861. doi:10.1371/journal.pone.0164861
25. Ping M, Wang JJ, Zhang Y, et al. Eepidemiological characteristics and influence factors of influenza outbreak in Shaanxi province, 2006–2013. Chin J Public Health. 2015;31:17–21.
26. Giefing-Kröll C, Berger P, Lepperdinger G, et al. How sex and age affect immune responses, susceptibility to infections, and response to vaccination. Aging Cell. 2015;14:309–321. doi:10.1111/acel.12326
27. Klein SL, Hodgson A, Robinson DP. Mechanisms of sex disparities in influenza pathogenesis. J Leukoc Biol. 2012;92:67–73. doi:10.1189/jlb.0811427
28. Walker CLF, Rudan I, Liu L, et al. Global burden of childhood pneumonia and diarrhoea. Lancet. 2013;381:1405–1416. doi:10.1016/S0140-6736(13)60222-6
29. Mazur NI, Martinon-Torres F, Baraldi E, et al. Lower respiratory tract infection caused by respiratory syncytial virus: current management and new therapeutics. Lancet Respir Med. 2015;3:888–900. doi:10.1016/S2213-2600(15)00255-6
30. GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the global burden of disease study 2016. Lancet. 2017;390:1151–1210. doi:10.1016/S0140-6736(17)32152-9
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.