Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 17
Stability of Blood Eosinophils in COPD with Multiple Acute Exacerbations Within 1 Year and Its Relationship with Prognosis
Received 8 October 2022
Accepted for publication 16 December 2022
Published 22 December 2022 Volume 2022:17 Pages 3123—3128
DOI https://doi.org/10.2147/COPD.S392660
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Richard Russell
Yaya Gong, Hongyan Sun
Department of Respiratory Medicine, Anhui No.2 Provincial People’s Hospital, Hefei, People’s Republic of China
Correspondence: Hongyan Sun, Department of Respiratory Medicine, Anhui No.2 Provincial People’s Hospital, Hefei, Anhui, 230001, People’s Republic of China, Tel +86 13856934496, Email [email protected]
Background: The relationship between increased blood eosinophils (EOS) and the prognosis of patients with chronic obstructive pulmonary disease (COPD) remains controversial. We aimed to explore the stability of blood eosinophils in patients with multiple hospitalizations for acute exacerbations of chronic obstructive pulmonary disease (AECOPD) over a 1-year period and its relationship with readmission rates and mortality.
Methods: Prospectively include patients with at least 2 hospitalizations for AECOPD in 1 year between June 2019 and December 2021. Using 150 cells/ul as the cut-off value, the study population was divided into EOS, non-EOS, and fluctuating groups based on the longitudinal stability of blood EOS. The relationship between blood EOS and readmission rate and mortality was analyzed according to the 6-month follow-up after hospital discharge.
Results: A total of 202 patients were included. 48, 108, and 46 patients were in the EOS, non-EOS, and fluctuating groups, respectively. The stability of blood EOS at 1 year was 77.2%. The risk of death was lower in the EOS group compared to the non-EOS group (HR=0.323, 95% CI 0.113– 0.930, P =0.036). The risk of readmission was lower in both the EOS group (HR=0.486, 95% CI 0.256– 0.923, P =0.027) and the non-EOS group (HR=0.575, 95% CI 0.347– 0.954, P = 0.032) than in the fluctuating group.
Conclusion: The blood EOS of COPD patients is relatively stable over 1 year. Patients with consistently high blood EOS had a lower risk of all-cause mortality after discharge; patients with fluctuating blood EOS had a higher risk of readmission.
Keywords: chronic obstructive pulmonary disease, acute exacerbation, blood eosinophils
Introduction
Chronic obstructive pulmonary disease (COPD) is a highly heterogeneous disease, and COPD patients with different phenotypes differ in terms of response to treatment and prognosis. Therefore, it is important to use biomarkers to identify specific phenotypes of COPD for personalized management and thus improve patient prognosis.1
Some patients with COPD have asthma-like features, such as significant bronchodilator reversibility, blood eosinophilia, and/or atopy. Suzuki et al showed that the presence of asthma-like features was associated with better clinical course in COPD patients under appropriate treatment.2 Among these, blood eosinophils (EOS) is used as a biomarker to assess the responsiveness of COPD patients to corticosteroids. Moreover, blood EOS seems to correlate with the prognosis of COPD.3–5 However, the stability of blood EOS is controversial due to its vulnerability to many factors.6,7 In addition, the results of studies related to the relationship between the stability of blood EOS and the prognosis of COPD patients are divergent due to the different threshold values used in different domestic and international studies and the different types of patients included (eg, stable and acute exacerbation). The results of a study showed that in patients with stable COPD, a sustained blood EOS of ≥300 cells/ul was not a risk factor for COPD progression. Also, patients with sustained blood EOS ≥300 cells/ul had low mortality.8 The results of another study showed a high risk of readmission in patients with acute exacerbation COPD with a sustained blood EOS of ≥300 cells/ul.9
Therefore, we evaluated the stability of blood EOS in patients hospitalized for acute exacerbations of COPD at least 2 times within 1 year and analyzed the relationship between blood EOS and all-cause mortality and readmission rates within 6 months of patient discharge.
Method
Patients
Inpatients who were admitted to the Department of Respiratory and Critical Care Medicine of the Second People’s Hospital of Anhui Province due to acute exacerbation of COPD at least 2 times within 1 year from June 2019 to December 2021 were included as study subjects. This study is prospective and conforms to the Declaration of Helsinki guidelines. The Ethics Committee of the Anhui No.2 Provincial People’s Hospital approved the experimental protocols. All participants provided informed consent.
Inclusion and Exclusion Criteria
Inclusion criteria (1) age ≥ 40 years; (2) meeting the diagnostic criteria for acute exacerbation of chronic obstructive pulmonary disease (2019 GOLD guidelines).10
Exclusion criteria: (1) combination of bronchial asthma, increased EOS, allergic diseases, parasitic infections, and other diseases that can cause increased EOS; (2) combination of severe cardiac, hepatic, and renal diseases; (3) maintained by OCS for a long time or had used oral or intravenous corticosteroids 48 hours before admission.
Data Collection
- General information and laboratory data: Medical history information provided at the admission of the study subjects was collected, including gender, age, comorbidities, mMRC classification, duration of disease, history of hospital admission in the previous year, and history of inhaled drugs. Peripheral blood EOS counts within 24 hours of admission were collected from the study subjects.
- Grouping: All study subjects underwent measurements of blood EOS counts at least 2 times within 1 year of the measurement interval. According to the blood EOS count, 150 cells/ul was used as the cut-off value, and the study subjects were divided into the EOS group (≥150 cells/ul), non-EOS group (<150 cells/ul), and fluctuating group (fluctuating between ≥150 cells/ul and <150 cells/ul).
- Follow-up: Patients or patients’ families were followed up by telephone to obtain information on whether patients were readmitted, time of readmission, and time of death within 6 months of discharge.
Statistical Analysis
IBM SPSS 24.0 was used for data analysis. Count data were expressed as frequencies and percentages (n, %), and rates were compared using the χ²-test. Measures that did not conform to normal distribution were expressed as median and interquartile spacing. Means of two groups of indicators with uneven variance and non-normal distribution were compared by Mann Whitney U nonparametric test. Kaplan Meier survival curves were used to analyze the correlation of different subgroups with all-cause mortality and readmission within 6 months after discharge. The association between blood EOS and the risk of death and readmission within 6 months after discharge was assessed using COX regression model analysis. In the COX regression model, adjustments were made for potential confounders, such as age and history of acute exacerbation in the previous year. P < 0.05 was considered a statistically significant difference.
Results
A total of 208 patients were enrolled, and 6 patients were excluded due to loss of follow-up. 202 patients were finally included in the study, 48, 108, and 46 in the EOS, non-EOS, and fluctuating groups, respectively. The stability of blood EOS over 1 year in patients with AECOPD was 77.2%. There were no statistically significant differences between the groups in terms of gender, age, comorbidities, mMRC classification, disease duration, history of hospital admission in the previous year, history of inhaled drugs, and acute comorbidities of congestive heart failure, cardiovascular disease, and cerebrovascular (P > 0.05). There were more cases of the EOS combination with type 2 diabetes compared with the non-EOS group, and the difference was statistically significant (P = 0.04), as shown in Table 1.
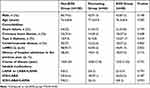 |
Table 1 Characteristics of Patients |
During the follow-up time within six months of discharge, there were 34 deaths (16.8%) and 97 readmissions (48.0%) within 6 months of discharge. The number of deaths in the EOS, non-EOS, and fluctuating groups were 4, 25, and 5, respectively. Among them, there were fewer post-discharge deaths in the EOS group compared with the non-EOS group (P = 0.028), and the difference was statistically significant. Multiple-adjusted COX regression analysis showed that the EOS group was associated with a lower risk of mortality (HR=0.323, 95% CI 0.113–0.930, P =0.036). 15, 38, and 26 readmissions were recorded in the EOS, non-EOS, and fluctuating groups, respectively, with the fluctuating group having the highest number of readmissions. There were more readmissions after discharge in the fluctuating group compared with the non-EOS group (P = 0.032). Multiple-adjusted COX regression analysis showed that the fluctuating group was associated with higher risk readmission rates (HR = 0.575, 95% CI 0.347–0.954, P = 0.032). There were more readmissions after discharge in the fluctuating group compared with the EOS group (P = 0.021), and multiple-adjusted COX regression analysis showed that the fluctuating group also showed an association with high-risk wind readmission rates (HR = 0.486, 95% CI 0.256–0.923, P = 0.027). As shown in Table 2.
 |
Table 2 Mortality and Readmission Rates in Each Group |
Discussion
Unlike some previous studies on patients with stable COPD, our study was conducted on patients hospitalized repeatedly for AECOPD for 1 year. Moreover, we not only performed a prognostic analysis of the EOS and non-EOS groups but also included the fluctuating group in our discussion. We had two main findings when using a blood EOS count of 150 cells/ul as the cut-off value. First, among patients hospitalized with AECOPD, the stability of blood EOS at 1 year was 77.2%, which was moderately stable. Secondly, the risk of death was lower in the EOS group and the risk of readmission was higher in the fluctuating group.
Prediction of COPD prognosis by a single blood EOS count seems to be less reliable due to the vulnerability of blood ESO to multiple factors. Therefore, further studies on the stability of blood EOS over time are needed. Oshagbemi et al followed up stable COPD patients for 1 year with a cut-off value of 340 cells/ul and showed an EOS stability of 75%.11 Citgez et al analyzed the EOS of patients hospitalized for AECOPD on two occasions before and after, based on cut-off values of 200/ul, 300/ul, 2%, and 3%, respectively, and showed overall stability of EOS of 70–85%.12 We chose a cut-off value of 150 cells/ul because studies have shown that this value is more useful for assessing the stability of blood EOS and also for differentiating patients prone to deterioration.13,14 Our results showed that the stability of blood EOS was 77.2%, suggesting that the stability of blood EOS in patients hospitalized with AECOPD was relatively stable over 1 year.
Regardless of the longitudinal level of eosinophils, there were no significant differences in patients’ mMRC classification, history of acute exacerbations in the previous year, duration of disease, or history of inhaled drugs. In terms of comorbidities, the proportion of patients with combined cardiovascular and cerebrovascular disease and congestive heart failure was similar in all groups. However, the number of patients with comorbid type 2 diabetes mellitus was significantly higher in the EOS group compared to the non-EOS group. This result is similar to a study from 2017, which found that the EOS group had more patients with comorbid diabetes than the non-EOS group, using a cut-off value of 150 cells/ul, through a retrospective collection of clinical data from 7245 patients with AECOPD.15 However, we are unable to explain this phenomenon for the time being.
During the 6-month follow-up period after discharge, 34 patients died. In the Cox regression model, the risk of death was significantly lower in the EOS group than in the non-EOS group, and the association analysis remained significant even after adjusting for age, a factor that may affect mortality outcome. This result is consistent with the findings of several studies using patients with stable COPD.8,16 Our findings for patients with AECOPD are more favorable for practical clinical use than studies from stable patients. This is because blood EOS data from patients hospitalized with AECOPD are more accessible and do not require patients to specifically visit the clinic in the stable phase to complete an EOS examination. Previous studies have also been conducted with patients hospitalized with AECOPD. Zhang et al selected patients hospitalized with AECOPD at least three times in five years for their study.17 Although the time span over which they obtained blood EOS was different from ours, it was also concluded that patients with elevated EOS had a low risk of all-cause mortality. When assessing the relationship between EOS and readmission risk, the results showed no significant difference in readmission risk between the EOS and non-EOS groups. In previous studies, some studies showed no significant difference in the risk of reoccurrence of acute exacerbation between the EOS and non-EOS groups,17–19 and some studies showed a high risk of reoccurrence of acute exacerbation in patients with high EOS.15,20,21 However, when we included the fluctuating group for analysis, we found that the risk of readmission was significantly higher in the fluctuating group than in the EOS and non-EOS groups. Also, the association analysis remained significant after adjusting for age, and history of acute exacerbation in the previous year in the Cox regression model. As our study was a single-center study, it is expected that this result will be validated in further multicenter studies.
Our study also has some limitations. Firstly, our study is observational, and some confounding factors such as pulmonary function examinations were not analyzed (some patients were unable to complete the examinations during the study period due to medical and other reasons, resulting in incomplete data), which may affect the study results to some extent. Secondly, this is a single-center study and some results may need to be further confirmed in a multicenter study.
The relatively stable blood EOS in patients with AECOPD and its correlation with prognosis may provide direction for individualized management of patients.
Summary
Blood EOS appears to correlate with COPD prognosis. However, the stability of blood EOS is controversial due to its vulnerability to many factors. In addition, the results of studies related to the relationship between the stability of blood EOS and the prognosis of COPD patients are divergent due to the different threshold values used in different domestic and international studies and the different types of patients included and further studies are needed.
The blood EOS of AECOPD patients is relatively stable over 1 year. Patients with consistently high blood EOS had a lower risk of all-cause mortality after discharge; patients with fluctuating blood EOS had a higher risk of readmission.
Author Contributions
Yaya Gong: (I) conception and design; (II) collection and assembly of data; (III) data analysis and interpretation; (IV) manuscript writing; (V) final approval of the manuscript. Hongyan Sun: (I) conception and design; (II) data analysis and interpretation; (III) manuscript writing; (IV) final approval of the manuscript. All authors contributed to data analysis, drafting or revising the article, have agreed on the journal to which the article will be submitted, gave final approval of the version to be published, and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Barnes PJ. Inflammatory endotypes in COPD. Allergy. 2019;74(7):1249–1256. doi:10.1111/all.13760
2. Suzuki M, Makita H, Konno S, et al. Asthma-like features and clinical course of chronic obstructive pulmonary disease. An analysis from the Hokkaido COPD cohort study. Am J Respir Crit Care Med. 2016;194(11):1358–1365. doi:10.1164/rccm.201602-0353OC
3. Barnes NC, Sharma R, Lettis S, Calverley PM. Blood eosinophils as a marker of response to inhaled corticosteroids in COPD. Eur Respir J. 2016;47(5):1374–1382. doi:10.1183/13993003.01370-2015
4. Oh YM, Lee KS, Hong Y, et al. Blood eosinophil count as a prognostic biomarker in COPD. Int J Chron Obstruct Pulmon Dis. 2018;13:3589–3596. doi:10.2147/COPD.S179734
5. Turato G, Semenzato U, Bazzan E, et al. Blood eosinophilia neither reflects tissue eosinophils nor worsens clinical outcomes in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2018;197(9):1216–1219. doi:10.1164/rccm.201708-1684LE
6. Kim VL, Coombs NA, Staples KJ, et al. Impact and associations of eosinophilic inflammation in COPD: analysis of the AERIS cohort. Eur Respir J. 2017;50(4):1700853. doi:10.1183/13993003.00853-2017
7. Schumann DM, Tamm M, Kostikas K, Stolz D. Stability of the blood eosinophilic phenotype in stable and exacerbated COPD. Chest. 2019;156(3):456–465. doi:10.1016/j.chest.2019.04.012
8. Casanova C, Celli BR, de-Torres JP, et al. Prevalence of persistent blood eosinophilia: relation to outcomes in patients with COPD. Eur Respir J. 2017;50(5):1701162. doi:10.1183/13993003.01162-2017
9. Cui Y, Zhang W, Ma Y, Zhan Z, Chen Y. Stability of blood eosinophils in acute exacerbation of chronic obstructive pulmonary disease and its relationship to clinical outcomes: a prospective cohort study. Respir Res. 2021;22(1):301. doi:10.1186/s12931-021-01888-5
10. Global initiative for chronic obstructive lung disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease (2020 REPORT)[EB/OL]; 2019. Available from: https://goldcopd.org/goldreports/.
11. Oshagbemi OA, Burden AM, Braeken DCW, et al. Stability of blood eosinophils in patients with chronic obstructive pulmonary disease and in control subjects, and the impact of sex, age, smoking, and baseline counts. Am J Respir Crit Care Med. 2017;195(10):1402–1404. doi:10.1164/rccm.201701-0009LE
12. Citgez E, van der Palen J, van der Valk P, Kerstjens HAM, Brusse-Keizer M. Stability in eosinophil categorisation during subsequent severe exacerbations of COPD. BMJ Open Respir Res. 2021;8(1):e000960. doi:10.1136/bmjresp-2021-000960
13. Pascoe S, Locantore N, Dransfield MT, Barnes NC, Pavord ID. Blood eosinophil counts, exacerbations, and response to the addition of inhaled fluticasone furoate to vilanterol in patients with chronic obstructive pulmonary disease: a secondary analysis of data from two parallel randomised controlled trials. Lancet Respir Med. 2015;3(6):435–442. doi:10.1016/S2213-2600(15)00106-X
14. Southworth T, Beech G, Foden P, Kolsum U, Singh D. The reproducibility of COPD blood eosinophil counts. Eur Respir J. 2018;52(1):1800427. doi:10.1183/13993003.00427-2018
15. Zeiger RS, Tran TN, Butler RK, et al. Relationship of blood eosinophil count to exacerbations in chronic obstructive pulmonary disease. J Allergy Clin Immunol Pract. 2018;6(3):944–954 e945. doi:10.1016/j.jaip.2017.10.004
16. Shin SH, Park HY, Kang D, et al. Serial blood eosinophils and clinical outcome in patients with chronic obstructive pulmonary disease. Respir Res. 2018;19(1):134. doi:10.1186/s12931-018-0840-x
17. Zhang Y, Liang LR, Zhang S, et al. Blood eosinophilia and its stability in hospitalized COPD exacerbations are associated with lower risk of all-cause mortality. Int J Chron Obstruct Pulmon Dis. 2020;15:1123–1134. doi:10.2147/COPD.S245056
18. Adir Y, Hakrush O, Shteinberg M, Schneer S, Agusti A. Circulating eosinophil levels do not predict severe exacerbations in COPD: a retrospective study. ERJ Open Res. 2018;4(3):00022–2018. doi:10.1183/23120541.00022-2018
19. Zysman M, Deslee G, Caillaud D, et al. Relationship between blood eosinophils, clinical characteristics, and mortality in patients with COPD. Int J Chron Obstruct Pulmon Dis. 2017;12:1819–1824. doi:10.2147/COPD.S129787
20. Yun JH, Lamb A, Chase R, et al. Blood eosinophil count thresholds and exacerbations in patients with chronic obstructive pulmonary disease. J Allergy Clin Immunol. 2018;141(6):2037–2047 e2010. doi:10.1016/j.jaci.2018.04.010
21. Vedel-Krogh S, Nielsen SF, Lange P, Vestbo J, Nordestgaard BG. Blood eosinophils and exacerbations in chronic obstructive pulmonary disease. The Copenhagen general population study. Am J Respir Crit Care Med. 2016;193(9):965–974. doi:10.1164/rccm.201509-1869OC
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
