Back to Journals » Advances in Medical Education and Practice » Volume 14
Skill Retention of Light-Curing Technique Using Only Verbal Instructions versus Using an Instructional Video: A 2-Year Follow-Up Study of Dental Students
Authors Al-Zain AO , Alsolami AH, Jamalellail HM, Price RB
Received 8 December 2022
Accepted for publication 5 April 2023
Published 21 April 2023 Volume 2023:14 Pages 391—405
DOI https://doi.org/10.2147/AMEP.S400823
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Balakrishnan Nair
Afnan O Al-Zain,1 Abdulmajeed H Alsolami,2 Hattan MH Jamalellail,3 Richard B Price4
1Restorative Dentistry Department, Faculty of Dentistry, King Abdulaziz University, Jeddah, Saudi Arabia; 2Faculty of Dentistry, King Abdulaziz University, Jeddah, Saudi Arabia; 3General Dentistry, Primary Health Care-Jizan Department, Ministry of the National Guard-Health Affairs, Jeddah, Saudi Arabia; 4Department of Dental Clinical Sciences, Faculty of Dentistry, Dalhousie University, Halifax, Nova Scotia, Canada
Correspondence: Afnan O Al-Zain, Restorative Dentistry Department, King Abdulaziz University Faculty of Dentistry, P.O. Box 80209, Jeddah, 21589, Saudi Arabia, Tel +966539116467, Fax +9666403316, Email [email protected]
Purpose: To evaluate the retention of light-curing skills among dental students after two years of clinical experience and determine if there are any differences in the skills retention between students who received verbal instructions or those who had received an instructional video. The students’ satisfaction with past learning, self-confidence, and general knowledge about light-curing were also evaluated.
Methods: This study is a 2-year evaluation of previous work. Students had previously been divided into two groups: those who received only verbal instructions, and those who received only an instructional video about the correct light curing technique to use clinically. Each student had light-cured simulated restorations (anterior and posterior) for 10 sec using the Managing Accurate Resin Curing-Patient Simulator (MARC-PS) (BlueLight Analytics, Halifax, Nova Scotia, Canada) and a multiple-emission peak light-emitting-diode (Bluephase N, Ivoclar Vivadent, Schaan, Liechtenstein) curing light. Students then received instructions according to their assigned group and light-cured the simulated cavities again. Two years later, students from both groups light-cured the same simulated cavities. Then, they completed a modified version of the National League of Nursing (NLN) satisfaction and self-confidence questionnaire and answered light-curing knowledge questions. Statistical analysis: The mean radiant exposure values delivered before receiving specific instructions on light curing, immediately after, and two years after instruction for both teaching methods (Friedman test followed by Wilcoxon signed-rank post hoc test), and the difference between both teaching methods was assessed (two-sample Wilcoxon rank-sum test). The satisfaction and self-confidence scores were compared between teaching method groups (Wilcoxon rank-sum test) (p< 0.05).
Results: The mean and median irradiance values ranged between 194-1777 and 1223– 1302 mW/cm2 before instructions, 320-1689 and 1254– 1394 mW/cm2 immediately after instructions, and 95-1945 and 1260– 1331 mW/cm2 two years later regardless of the simulated restoration or the teaching method. The mean and median radiant exposure values ranged between 2-23 and 12.5– 13.6.4 J/cm2 before instructions, 3-28 and 12.8– 14.3 mW/cm2 immediately after instructions, and 0.7-20 and 12.8– 13.6 mW/cm2 two years later regardless of the simulated tooth being light cured and the teaching method. Students retained their light-curing skills after two years of clinical experience, with no significant differences between both groups. The instructional video group delivered significantly higher radiant exposure values (p=0.021) when light-curing the anterior tooth than the posterior. Students were satisfied with their past learning and confident in their light-curing skills (p=0.020). There were statistical differences in how well the two groups remembered what they had been taught about light-curing. Only 5.7% of students answered all knowledge questions correctly.
Conclusion: Students retained their light-curing skills after two years of clinical experience, with no significant difference between verbal instructions or instructional video teaching methods. However, their knowledge about light curing remained very poor. Nevertheless, the students were satisfied with how they had been taught and had confidence in both teaching methods.
Keywords: dental education, light curing, dental students, satisfaction, self-confidence, teaching method
Introduction
Most dental resins and bonding agents are delivered as unfinished products that must be adequately light-cured by the dentist in the tooth. Without adequate light-curing, the products that the dentist purchases will not meet the manufacturer’s intended properties. Consequently, light-curing has become an essential step in everyday dentistry.1 However, most dental students overlook the importance of light curing due to the lack of emphasis in most restorative dentistry courses.2 The inability to master the skill of proper light-curing technique affects the quality of dental treatment delivered by dental students and negatively affects the properties and longevity of the final restoration.1–3
With today’s technology, there are new ways for students to interact with the faculty and enhance their learning experience. Information about the curing light and how to use it could be taught using instructional videos that show the procedure from a broader perspective.4 Several studies have already explored the effectiveness of verbal or video instruction methods.4,5 Live demonstrations and video-recorded teaching methods were equally successful in teaching how to apply fissure sealants. They can be used as an alternative to each other, or they can be combined when teaching medical students clinical knowledge and skills.6,7 It was shown that students who watched live demonstrations that were video recorded developed a similar level of understanding of the principles behind the exercise when teaching removable partial denture techniques. However, live demonstrations were still preferred by students.8,9 Furthermore, a live demonstration can help students improve their communication skills and develop confidence.10
New skills can be taught using simulators. Light-curing skills can be improved using the Managing Accurate Resin Curing-Patient Simulator (MARC-PS) system (BlueLight Analytics, Halifax, Nova Scotia, Canada) because it provides an objective instant digital and visual feedback.3,4,11 One study has shown that active learning and displaying learning objectives for the given training or simulation is helpful to the learner.12 Greater self-confidence and satisfaction occur when active learning is delivered in an environment where the students can actively interact with one another and their instructors. In this simulation, the student develops mechanical, cognitive psychological, and social skills to achieve a better learning outcome.12
Skill retention after knowledge acquisition has been a concern when learning any practical skill. For example, there is a noticeable decline in the retention of cardiopulmonary resuscitation skills one month after training.13,14 Since dental students acquire many practical skills in different subjects throughout dental school, it is not surprising for students to experience some loss of skill retention during their dental training, especially if the procedure is not practiced often or if the relevance of the skill to successful dentistry is unclear. This is supported by the Skill Retention Theory, where after the first stage of learning, skill retention and knowledge may degrade due to a lack of use.15 This means that specific steps of a procedure may not be retained if it was not practiced and reinforced. There are several methods to assess skill retention of cognitive skills, one of which is achieving a minimum passing score to demonstrate competency.13,14,16 One study showed that after receiving simulation-based training how to insert a central venous catheter, this skill was retained after one year; however, the performance of individuals cannot be predicted, and periodic refresher training and testing are recommended to maintain competence.16 Another method reported to assess skill retention is an adaptive virtual reality training system. One study investigated the acquisition and retention of medical skills, and found that using the adaptive virtual reality training system was beneficial.15 Light-curing skill retention can be simulated using the MARC-PS, which provides an objective method of measuring the ability of the student to deliver light to a simulated restoration.17 One study that evaluated dental students’ light-curing skills immediately after training and then evaluated the skill retention one and two years after training using the MARC-PS before starting patient care showed some loss in the skill taught as the time after training increased.17
A previous study by the authors published in 2021 showed no significant differences between teaching light-curing techniques among dental students using an instructional video versus using verbal instructions.4 In this study, the MARC-PS was used to deliver immediate individual feedback to the student and objectively compare how much irradiance and radiant exposure (RE) were received by simulated cavities in a dental mannequin head.4 Now, after two years of clinical experience, the authors reassessed and evaluated the retention of the information to determine if there was any improvement in the light-curing technique using the MARC-PS system compared to the results from the original baseline results. The light-curing performance was evaluated using the same MARC-PS and the performance was scored using a rubric. In addition, the students were asked how satisfied they were with how the skill had been taught. In addition, the student’s holistic light-curing performance and learning experience were examined.
The study aims were: 1) to assess how well the students had retained their light-curing skills after 2 years of clinical experience. 2) to evaluate if there were differences in the skill retention after 2 years of using curing lights depending on if they had been taught using verbal instructions versus an instructional video. 3) to evaluate student satisfaction with how they had been taught previously and their self-confidence in learning the light-curing skill, and 4) to determine if there were any differences in the student’s didactic knowledge when they had received light-curing instructions via verbal instructions compared to when they had been taught using an instructional video.
The null hypotheses were:
Materials and Methods
Ethical approval for this study was obtained from the Ethical Research Committee at King Abdulaziz University Faculty of Dentistry (proposal no. 258-08-21). The study complies with the Declaration of Helsinki and is a continuation of a previously published study.4 A signed consent form was obtained from the participants. Two years ago, when students were in their third year of the dental program, two light-curing teaching methods were assessed during their first exposure to a light-curing procedure in the Preclinical Operative and Esthetic Dentistry course. After attending the didactic lecture, 120 students were randomly divided into two groups (n= 60/teaching method); each student light-cured the two simulated cavities (anterior and posterior) on a MARC-PS before receiving any further instructions. Then, depending on the group they were allocated to, each student either just watched a light-curing technique instructional video or they received some verbal instructions and then light-cured the simulated cavities again using a multiple-emission peak light-emitting-diode (LED) (Bluephase N, Ivoclar Vivadent, Schaan, Lichtenstein) light-curing unit (LCU) for 10 seconds. The irradiance and the amount of RE the two groups of students delivered to the simulated cavities were compared. At the beginning of the study, the first author light-cured the anterior and posterior simulated teeth for a 10-second exposure time using the same LCU to record the maximum irradiance and radiant exposure that could be delivered to the simulated teeth (n=3) from the curing light used in this study.
When students were in their fifth year of the dental program, they received one light-curing lecture at the end of the first semester. The learning outcomes from the lecture were to explain the factors affecting light-curing, the LCU types, the advantages and disadvantages of each type, the parameters to consider when selecting the LCU, to review their light-curing technique, and how to maintain LCUs. All the students had received similar hours of training in the preclinical laboratory and in their fourth and fifth academic years of clinical training in the dental program.
After two years of clinical experience and when the students were in their sixth year of the dental program, how well the students had retained their light-curing skills was reassessed in the first two weeks of the academic year, and any changes in their light-curing technique were determined. Each student’s light-curing performance was determined using the MARC-PS, and the light-curing steps they used were scored using a rubric. In addition, the student satisfaction with how they had been taught and their self-confidence in how they learned about light-curing were evaluated. The MARC-PS was mounted on the dental chair to simulate a typical clinical scenario and the experiment took place at the beginning of the students’ clinical sessions.
A total of 105 students were included in the study: 53 students were taught using the instructional video and 52 were taught using the verbal instructions teaching method. However, 15 students were not retested (11 males and four females) either because they had transferred to different schools, or they had fallen behind in their courses and were no longer in the same class as their peers. Thus, they were excluded because they did not have the same light-curing experience on patients.
Two calibrated evaluators tested the students. First, they assessed the student’s light-curing performance using the same rubric used in the previous study5 in terms of: 1) did they check if the light guide on the LCU was damaged, 2) did the operator wear eye protection, 3) did they place eye protection on the MARC-PS mannequin head, 4) was the light guide tip was placed perpendicularly on the simulated tooth, 5) if the distance between the guide tip and the simulated tooth was as close as possible, 6) did they use a finger to support the light guide, 7) did the participant maintain eye contact with the specified tooth throughout the light-curing cycles, 8) did they activate LCU for 10 seconds.
Each student performed one light-curing cycle on the anterior and the posterior simulated teeth individually on the MARC-PS using the same LCU used in the first study. Other students were not allowed to watch their peers during the experiment. In addition, students were not allowed to ask questions when they were evaluated.
After finishing the light-curing exercise, each student completed a questionnaire to determine their satisfaction with how they had been taught and their self-confidence in their light curing skills. Their knowledge about light curing was assessed using three knowledge questions, and what other sources they had used to obtain additional knowledge about light-curing in the past two years. The student satisfaction with learning and self-confidence questionnaire was assessed using a modified National League of Nursing (NLN) questionnaire that determines the students’ satisfaction with learning and their self-confidence in how they obtained the skills they learned.10 The questionnaire was composed of five sections; Section 1: demographic information, including the gender, pre-assigned serial number, and the original group the students were in (instructional video or verbal instructions); Section 2: satisfaction and self-confidence section targeting the light-curing technique learning skill; Section 3: three knowledge questions about light curing; Section 4: didactic questions that ask the students if they obtained additional information about light-curing other than from the lectures received in the dental curriculum, and the type of media they have received the additional information from during their 2 years of clinical experience; Section 5: an open-ended question about their experiences. The modified NLN survey and other parts of the questionnaire were validated and piloted before starting the study (Supplementary Material 1). The students included in the pilot study were not from the 105 students included in the study. In addition, the evaluators were asked to complete a digital feedback survey with open and closed-ended questions about their observations of the student’s performance and their opinions about both teaching methods (Supplementary Material 2). The study design is presented in Figure 1.
 |
Figure 1 Study design. |
Statistical Analysis
A descriptive comparison of the examiners’ observations of the student’s light-curing technique based on the rubric after two years of clinical experience as they light-cured the anterior and posterior simulated restorations was calculated, and the aggregate percentage score of higher than 70% represented competency in the light-curing procedure. The percentage score of light-curing performance according to the rubric was calculated by adding the scores of all rubric items and dividing this score by the rubric maximum (11 points) and multiplying the product by 100. In addition, the examiners’ feedback on the students’ performance was collected. Visual comparisons of the graphs of the irradiance delivered when light-curing the anterior teeth were performed at each of the three-time points evaluated (before instruction, immediately after instruction, and two years later). Normality was confirmed using the Shapiro–Wilk W-test. Medians and interquartile ranges (IRQ) were calculated, and Friedman test was used to assess the distributions of mean irradiance and RE values measured for anterior tooth and posterior tooth before instructions, immediately after instruction, and two years after the instruction for both teaching methods (verbal instructions or just the instructional video). Post-hoc analyses using Wilcoxon signed-rank tests were used for pairwise comparisons, and significance values were adjusted using the Bonferroni correction for multiple tests. The significance level was set at 0.05.
Two-sample Wilcoxon rank-sum (Mann–Whitney) test was used to assess if there were any differences between the students who received verbal instructions and those who received just the instructional video in each of the measurements. The aggregate scores for the satisfaction and self-confidence scales were calculated. For the satisfaction section of the scale, questions 1–5 aggregated scores range from 5 to 25. For the self-confidence section of the scale, questions 6–13 aggregated scores range from 5 to 40. The Shapiro–Wilk test was used to check that the data was normally distributed among the groups. The scores of items and the aggregate scores for both scales were compared between the two groups of light-curing instructions (verbal instructions versus instructional video) using the Wilcoxon rank-sum test.
The aggregate score for students’ general knowledge about light-curing was calculated by adding the scores of the three knowledge questions. The percentage of Knowledge score was calculated by adding the scores of all three questions, dividing this score by the didactic maximum (3 points) and multiplying the product by 100. Since the assumption of normality for each of the variables does not hold for this data, the Spearman correlation coefficient and its p values were estimated to assess the correlation between the student’s general knowledge about light-curing and their performance after 2 years of clinical experience.
The effect of obtaining additional information about light-curing during the past 2 years on each student’s performance immediately after instructions and after 2 years of clinical experience was explored to assess the statistical difference between the participants who obtained additional information about light-curing and who did not, regardless of the instructional group. The statistical comparisons were carried out using related-samples Friedman’s analysis of variance by ranks. The effect of obtaining additional information about light-curing during their 2 years of clinical experience was tested using a two-sample Wilcoxon rank-sum (Mann–Whitney) test for each instructional group. Both IBM Statistical Package for Social Sciences Statistics version 28 (SPSS Inc, Armonk, NY, USA), and Stata software, version 16 (StataCorp, College Station, TX, USA) were used for the statistical analyses.
Results
The mean irradiance (standard diviation) and RE (standard diviation) values obtained by the expert were 1559 (75.0) mW/cm2 and 16.0 (0.79) J/cm2, the range was between 1463-1671 mW/cm2 and 15-17.2 J/cm2 at the anterior tooth, and a mean of 1537 (46.2) mW/cm2 and 15.7 (0.50) J/cm2, the range was between 1501-1615 mW/cm2 and 15.3-16.6 J/cm2 at the posterior tooth. The difference in the irradiance and the RE percentage between the expert and the values delivered by the students were 22–35% before students received any instructions on light curing, 14–21% immediately after receiving the instructions, and 16–22% after they had been treating patients for 2 years. These differences were similar between the two instructional methods and were unaffected by the tooth position.
Table 1 reports the examiner’s observations of the student’s light-curing technique based on the rubric after two years of clinical experience when light-curing the anterior and posterior simulated teeth. Examiners observed that 80% (84) of the students did not check that the light-guide tip was clean and not broken before using it. The examiners observed that 1% (one student) did not maintain contact at all with the tooth when light-curing. In addition, 1% (one student) did not place the light-guide tip as close as possible to the tooth, and 1% (one student) did not place the light-guide tip perpendicular to the posterior tooth. Interestingly, only 4.8% (five students) correctly performed all the light-curing technique steps in the rubric. The examiners reported that approximately 80% of the students did not practice proper ergonomics while light-curing the simulated cavities. Nevertheless, all students were considered competent when performing the light-curing, where only 3.5% (4 students) scored a 72.7%, and the remaining students scored above 80%.
 |
Table 1 Examiner’s Observation of the Students’ Light-Curing Technique After Two Years of Clinical Experience When Light-Curing the Anterior and Posterior Simulated Teeth |
Figures 2 and 3 shows that before receiving their light-curing instructions two years before the evaluation, students delivered a variable amount of irradiance to the simulated cavities in the anterior and posterior teeth. Immediately after receiving either video or verbal instructions, the students delivered a more stable irradiance. Two years later, most students showed some retention of the light-curing skill, and they delivered a stable irradiance, while some still delivered an unstable irradiance. Of note, Figures 2 and 3 also shows no obvious improvement between immediately after the students received instructions, and some two years later.
Figure 4 shows box plots of the median, minimum and maximum RE values that the students delivered to the anterior and posterior simulated teeth before receiving instructions, immediately after instructions, and after two years of clinical experience after receiving only verbal instructions and the group that received the instructional video. The irradiance and RE values delivered to the anterior and posterior simulated teeth ranged between 194-1777 mW/cm2 and 2-23 J/cm2 before receiving instructions, ranged between 320-1689 mW/cm2 and 3-28 J/cm2 immediately after instructions, and ranged between 95-1945 mW/cm2 and 0.7-20 J/cm2 after two years of clinical experience for both teaching methods used. Table 2 reported the median, the interquartile range (IQR), and p-values of the mean irradiance and RE values that the students delivered to the anterior and posterior simulated teeth before receiving instructions, immediately after receiving instructions, and after two years of clinical experience for the group that received only verbal instructions and the group that received the instructional video. Significant differences were observed in the mean irradiance (p=0.018), and RE (p=0.021) values delivered by the instructional video group when light-curing the anterior tooth.
 |
Table 2 Medians and Interquartile Ranges for the Irradiance (mW/cm2) Radiant Exposure (J/cm2) Values and Friedman Test p-values |
Table 3 shows the pairwise comparisons for the RE distributions for students that received the instructional video. Higher significant differences in the RE values delivered to the anterior tooth were observed before receiving any instructions compared to immediately after instructions (p=0.016). In addition, significant differences were found in the results measured before the students received any detailed instructions on light curing, compared to their results 2 years later (p<0.001).
Table 4 shows that there were no significant differences in the RE values delivered to both simulated teeth between the groups that received verbal instructions and the group that received the instructional video after two years of clinical experience (two-sample Wilcoxon rank-sum Mann–Whitney tests).
Table 5 shows that the students were generally satisfied with their learning experiences, and they were confident in their ability to use the LCU. The sections on the self-satisfaction of the students past learning about light-curing showed that the individual score median was 5, and the total aggregate score median was 25 for both teaching method groups. The differences between both groups were not significant. The sections about the self-confidence of both groups in their light-curing technique showed that the individual score median was 5, and the total aggregate score median was 38 for both groups. There were significant differences in the last (13th) item regarding how well the two groups remembered what they had been taught about light-curing two years ago and how to use the light-curing skills they learned two years ago.
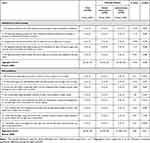 |
Table 5 Statistical Comparisons for the Student Satisfaction in Past Learning and Self-Confidence in Learning Scale and Its Items Between Verbal Instructions and Instructional Video Teaching Methods |
Table 6 reports the responses to the questions about light-curing. For example, 27.6% (29 students) correctly answered the first question regarding the wavelength range that most curing lights deliver (400 to 500 nm), while 45.7% (48 students) thought the answer was 400 to 500 mW/cm2. For the second question, 23.8% (25 students) solved the irradiance equation correctly (2000 mW/cm2), while 29.5% (31 students) answered 1000 mW/cm2. For the last question, 70.5% (74 students) answered it correctly, that the retina was the most adversely affected by the light from the LCU, while 17.1% (18 students) thought that the oral mucosa was the most affected organ. Of concern is that only 5.7% (six students) answered all three knowledge questions correctly.
 |
Table 6 Student’s Light-Curing Knowledge After Two Years of Clinical Experience |
The results for the Spearman correlation coefficients results showed no correlation between the student’s general knowledge about light-curing and their performance after 2 years of clinical experience regardless of the tooth cured when light-curing the anterior and posterior teeth in terms of irradiance (r=0.036, and r=0.042, respectively), and radiant exposure (r=0.019, and r=0.006, respectively) when students received the two different methods of light-curing instruction (p>0.05).
Considering obtaining additional information regarding LCUs during the past two years, 19–33% of the students had obtained additional information from sources, other than from the lectures given in the third and fifth years. This additional information was mainly from books, scientific articles, and social media. However, the results showed that obtaining additional information from sources other than from their lectures did not significantly change the students’ performance after 2 years of clinical experience when light-curing the simulated teeth, regardless of the teaching method used (p>0.05).
Discussion
When observing the students at the two-year follow-up, the examiners noticed that 80% of the students did not check the light guide tip before using it. This could affect the light output of the LCU and results in possible failure of routine restorative treatment. In addition, 1–8.6% of the students missed other parts of the rubric. This can indicate that students did not understand the relevance of delivering an adequate amount of light to their resins. Consequently, each step of the students’ light-curing technique should be reemphasized, monitored and periodically re-evaluated during clinical sessions to ensure that each step of the light-curing technique is performed, and that it is performed correctly. The fact that only 5 students (4.8%) performed all steps correctly in the rubric is a concern, especially because the self-confidence data revealed that students felt confident with their light-curing technique. In reality, 95.2% of students did not perform all steps correctly, and this was supported by the observations of the observers. Although some steps were missed, most of the students thought that they were competent performing the procedure.
Based on Figures 2 and 3, in the anterior teeth simulation, after immediately receiving both verbal and video instructions, the students of both groups managed to deliver a stable amount of light compared to the follow-up measurements. However, there were some slight fluctuations in the irradiance delivered. This might indicate a lack of clinical experience in treating anterior teeth during the student’s two years of clinical experience compared to treating and light-curing posterior teeth. Regarding the posterior teeth visual comparisons, the amount of light delivered by the students was stable and efficient both after receiving both types of instructions and at the two-year follow-up, with no noticeable differences between the verbal and video instruction groups.
The RE is the amount of energy received by the restoration over time (RE = irradiance x time).18,19 The same exposure time was used and statistical comparisons for the RE values were reported in the figures and tables. The results of this were similar to a previous study where the light output was delivered to the MARC-PS simulator by pre-clinical students and dental interns.20 In this study, the amount of light delivered to the sensor in the anterior tooth was higher in both groups compared to the sensor in the posterior tooth. This was attributed to differences in the access to the anterior and posterior teeth.20 Another study measured the light output delivered to the MARC-PS in the upper left posterior maxillary area by first-year dental students.3 This study reported that students who received individualized instructions and instant feedback retained their light-curing skill for at least five months and delivered a higher RE compared to the students who did not receive instructions and feedback.3
Based on the two-year follow-up measurements, the first hypothesis is partially rejected. The significant difference in the instructional video group in terms of irradiance and RE values when light-curing the anterior tooth could be explained by the fact that in the preliminary study, some of the students reported difficulty in achieving proper light cure guide-tip support on the anterior tooth because they had to retract the upper lip of the mannequin head and support the LCU guide-tip at the same time. However, in the two-year follow-up, the students could easily light cure the anterior tooth. These results suggest that the students retained light-curing skills and they had learned how to retract the lip after two years of clinical experience treating patients.
Since there was no significant difference between verbal instruction and instructional video groups, the second hypothesis was accepted. This indicates that the teaching method did not significantly affect how the students retained the light curing skills they learned in their pre-clinical courses. The results support the absence of significant differences in the initial study.4 In another study that evaluated long-term skill retention of students who underwent hands-on light-curing training and were measured using the MARC-PS simulator as well, the results show that after hands-on training and two years of clinical experience, there was a marked improvement in the RE measurements when curing the anterior and posterior teeth.17 Comparing the results with the obtained data in our study, there was a slight decrease in the RE related to the quantitative readings of the posterior tooth in both groups. This reduction was similar in both studies, and there was evidence of some skill retention and a slight improvement. This was most noticeable in the readings from the anterior tooth sensor.
The third hypothesis was partially rejected because there was no significant difference in the satisfaction of verbal and instructional video groups of students but there was a statistical significance in the last (13th) item of the self-confidence scale for both verbal and instructional video groups. This indicated that students were satisfied with their past learning experiences and felt confident when light-curing restorations regardless of the teaching method used. This was also evident in the students’ responses in the open-ended section where they expressed that the simulation experience was helpful and beneficial. The significant difference observed in the last (13th) item of the self-confidence scale indicated that not all students could remember the details taught in the lectures, but they could perform the procedure confidently. The lack of self-confidence was demonstrated in the knowledge section of the survey, where most of the students did not retain the didactic knowledge regarding light-curing asked in the study, and some students reported in the open-ended question that they could not remember the didactic details. This could be explained by the fact that students are only exposed to the didactic information about light-curing in the lectures and this information was not emphasized in the clinic when treating patients.
Not remembering the didactic information was evident in the students’ responses in the open-ended section, where some students expressed that they could not remember some of the didactic information, calculations, and units taught in the lectures. For example, hen answering the question about the wavelength range that most curing lights deliver, 29 students (27.6%) gave the correct range, but could not remember the correct unit. Also, 45.7% of students selected the answer using the unit of irradiance, and one student (1%) selected the option with the meter unit. Similarly, when asked to calculate the irradiance value, the curing light must deliver 2000 mW/cm2 over 10 seconds to achieve the desired 20 J/cm2, 21% of the students provided the correct value, but did not remember the correct units. Regarding the last knowledge question asking which part of the body was most affected by the blue light, 70.5% selected the retina as the correct answer. This was not surprising because this information was emphasized in their lectures on light-curing. Also, it is well documented in the other literature that the retina is the most affected part of the body by blue light LEDs, tablets, computers and from the LCU.21,22 The fact that only 5.7% of participants answered all three knowledge questions correctly is a concern. This may be because students were not exposed to the didactic information frequently (twice in this case, once in the third year and another in the fifth year), unlike the light curing technique that is constantly being practiced by the students in the clinics.
Obtaining additional information regarding light-curing during the past 2 years or even the information they already learned did not significantly affect the students’ performance and there was no correlation between the information they had learned from other sources and their performance. This may indicate that students learn for the test and do not retain much information after the test is over. Nevertheless, they did remember the practical part. Therefore, the didactic aspect of this topic should be discussed or evaluated during clinical sessions as it is part of the procedure that students are performing.
There were certain limitations of the present study. We were unable to standardize the knowledge retention of the students as it is challenging to control if any of the students have been exposed to additional knowledge during the past two years of clinical experience. However, their knowledge skills were very poor. In addition, students were aware that they were participating in a study, so they might have focused on their light-curing technique to obtain a good evaluation. Also, the study was conducted during students’ clinical sessions. Therefore, the students might have been in a hurry to perform the measurement to go back and continue the treatment of their patients during the session, but then this reflects the clinical reality in a busy dental office.
It is recommended that the light-curing technique be reinforced and tested throughout the dental curriculum to reinforce the didactic knowledge and each step of the light-curing technique so students would not miss steps during the light-curing procedure. This would likely improve their knowledge retention so that they could provide optimum patient care. With the development of simulation technology, using devices such as the MARC-PS that allow interaction and the students can receive instant feedback, the students can develop and improve their skills before treating patients. The MARC-PS can be used throughout the dental curriculum to ensure that the students continue to practice good light-curing technique. Outside the rubric, the examiners also noticed that many students had a very poor ergonomic posture when using the LCU, and some students had their backs excessively bent forward as they attempted to deliver light to the posterior tooth on the occlusal surface of tooth No. 27. Further studies should be conducted and relate the ergonomics and student posture when light-curing to the irradiance and RE readings using the MARC-PS simulator. It would be useful to conduct an ophthalmic examination upon entry and exit of dental school to determine if any changes had occurred. Using a virtual reality simulation in the teaching process and comparing the quantitative readings to instructional video and verbal instructions method might also be beneficial. In addition, conducting the study in multiple dental institutions would be valuable. Also, the light-curing performance of the students should be routinely tested using the patient simulator. Finally, since much of modern dentistry epends on photo-cured resins, it is recommended that the important aspects of the light-curing skill and knowledge about light-curing be reemphasized throughout the dental curriculum.
Conclusion
After two years of clinical experience treating patients, the students had retained the light-curing skills they had learned pre-clinically. Generally, there were no significant differences in the skill retention of dental students when they received teaching from an instructional video or by a verbal instruction teaching method, except when light-curing the anterior tooth for the instructional video group. In addition, generally, there were no significant differences in satisfaction with past learning, self-confidence in learning the light-curing skill, and general knowledge about light-curing among the students between both teaching methods. The students did not retain the basic science knowledge they had been taught pre-clinically about light-curing. Obtaining additional information during the past two years about light-curing from resources other the lectures in the dental curriculum did not significantly improve students’ performance.
Acknowledgments
The authors would like to thank Dr. Ameerah Mansour for her assistance in the statistical analysis.
Disclosure
All authors report no conflicts of interest in this work.
References
1. Rueggeberg FA, Giannini M, Arrais CAG, et al. Light curing in dentistry and clinical implications: a literature review. Braz Oral Res. 2017;31:e61. doi:10.1590/1807-3107bor-2017.vol31.0061
2. Price RB, Ferracane JL, Shortall AC. Light-curing units: a review of what we need to know. J Dent Res. 2015;94:1179–1186. doi:10.1177/0022034515594786
3. Price RB, Strassler HE, Price HL, et al. The effectiveness of using a patient simulator to teach light-curing skills. J Am Dent Assoc. 2014;145:32–43. doi:10.14219/jada.2013.17
4. Al-Zain AO, Al-Osaimi TM. Effectiveness of using an instructional video in teaching light-curing technique. Adv Med Educ Pract. 2021;12:289–302. doi:10.2147/AMEP.S298556
5. Alqahtani ND, Al-Jewair T, Al-Moammar K, et al. Live demonstration versus procedural video: a comparison of two methods for teaching an orthodontic laboratory procedure. BMC Med Educ. 2015;15:199. doi:10.1186/s12909-015-0479-y
6. Mirkarimi M, Kalati F, Moghadam AA. A comparison between video tape and live demonstration methods for teaching of fissure sealant placement procedures for dental students of Zahedan University of Medical Sciences in 2010–2011. J Dent Med. 2012;25:252–257.
7. Mir MA, Marshall RJ, Evans RW, et al. Comparison between videotape and personal teaching as methods of communicating clinical skills to medical students. Br Med J. 1984;289:31–34. doi:10.1136/bmj.289.6436.31
8. Packer ME, Scott BJ, Davis DM. An assessment of the influence of clinical demonstrations on the confidence of undergraduate dental students, when treating patients requiring removable partial dentures. Eur J Dent Educ. 1999;3:133–139. doi:10.1111/j.1600-0579.1999.tb00079.x
9. Packer ME, Rogers JO, Coward TJ, et al. A comparison between videotaped and live demonstrations, for the teaching of removable partial denture procedures. Eur J Dent Educ. 2001;5:17–22. doi:10.1034/j.1600-0579.2001.005001017.x
10. Zapko KA, Ferranto MLG, Blasiman R, et al. Evaluating best educational practices, student satisfaction, and self-confidence in simulation: a descriptive study. Nurse Educ Today. 2018;60:28–34. doi:10.1016/j.nedt.2017.09.006
11. Tauböck TT, Par M, Attin T, et al. Effectiveness of using a patient simulator with real-time feedback to improve light-curing skills of dental students. Appl Sci. 2020;10:156.
12. Olaussen C, Heggdal K, Tvedt CR. Elements in scenario-based simulation associated with nursing students’ self-confidence and satisfaction: a cross-sectional study. Nurs Open. 2020;7:170–179. doi:10.1002/nop2.375
13. Madden C. Undergraduate nursing students’ acquisition and retention of CPR knowledge and skills. Nurse Educ Today. 2006;26:218–227. doi:10.1016/j.nedt.2005.10.003
14. Wilson E, Brooks B, Tweed WA. CPR skills retention of lay basic rescuers. Ann Emerg Med. 1983;12:482–484. doi:10.1016/S0196-0644(83)80643-X
15. Siu KC, Best BJ, Kim JW, et al. Adaptive virtual reality training to optimize military medical skills acquisition and retention. Mil Med. 2016;181:214–220. doi:10.7205/MILMED-D-15-00164
16. Barsuk JH, Cohen ER, McGaghie WC, et al. Long-term retention of central venous catheter insertion skills after simulation-based mastery learning. Acad Med. 2010;85:S9–12. doi:10.1097/ACM.0b013e3181ed436c
17. Balhaddad AA, Marghalani AA, Raderman MA, et al. Hands-on training based on quantifying radiant exposure improves how dental students cure composites: skill retention at 2-year follow-up. Eur J Dent Educ. 2020;25:582–591. doi:10.1111/eje.12635
18. Leprince JG, Palin WM, Hadis MA, et al. Progress in dimethacrylate-based dental composite technology and curing efficiency. Dent Mater. 2013;29:139–156. doi:10.1016/j.dental.2012.11.005
19. Price RBT. Light curing in dentistry. Dent Clin North Am. 2017;61:751–778. doi:10.1016/j.cden.2017.06.008
20. Suliman AA, Abdo AA, Elmasmari HA. Training and experience effect on light-curing efficiency by dental practitioners. J Dent Educ. 2020;84:652–659. doi:10.1002/jdd.12113
21. Alasiri RA, Algarni HA, Alasiri RA. Ocular hazards of curing light units used in dental practice - a systematic review. Saudi Dent J. 2019;31:173–180. doi:10.1016/j.sdentj.2019.02.031
22. Fluent MT, Ferracane JL, Mace JG, et al. Shedding light on a potential hazard: dental light-curing units. J Am Dent Assoc. 2019;150:1051–1058. doi:10.1016/j.adaj.2019.08.012
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.





