Back to Journals » Infection and Drug Resistance » Volume 15
Risk Factors for Mortality and Antimicrobial Regimens in Pediatric Intensive Care Unit Patients with Carbapenem-Resistant Enterobacteriaceae Infections: A Six-Year Retrospective Study
Authors Liu P , Mai Y, Yuan W, Xie L, Ma W, Liu J, Xu L, Yang J, Wang P, Wang H
Received 20 October 2022
Accepted for publication 6 December 2022
Published 13 December 2022 Volume 2022:15 Pages 7307—7316
DOI https://doi.org/10.2147/IDR.S394283
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Suresh Antony
Peng Liu,1,* Yumiao Mai,2,* Wenhua Yuan,1 Lei Xie,1 Wei Ma,1 Jian Liu,2 Lu Xu,3 Jing Yang,4 Peile Wang,4 Huaili Wang1
1Department of Pediatric Intensive Care Unit, The First Affiliated Hospital of Zhengzhou University, Zhengzhou, People’s Republic of China; 2Department of Pediatrics, The First Affiliated Hospital of Zhengzhou University, Zhengzhou, People’s Republic of China; 3Department of Clinical Laboratory, Henan Children’s Hospital, Zhengzhou, People’s Republic of China; 4Department of Pharmacy, The First Affiliated Hospital of Zhengzhou University, Zhengzhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Huaili Wang; Peile Wang, Email [email protected]; [email protected]
Purpose: Limited data are available on the characteristics, risk factors, and antimicrobial treatment of critically ill pediatric patients with carbapenem-resistant Enterobacteriaceae (CRE) infections. This study was to identify the risk factors for 30-day mortality in pediatric intensive care unit (PICU) patients with CRE infections and compare the clinical outcomes of different antimicrobial regimens.
Methods: A retrospective, observational cohort study was performed on patients admitted to the PICU with positive CRE cultures between January 2016 and December 2021.
Results: For the 56 patients, the overall 30-day mortality was 50% (n=28). Multivariable logistic regression analysis revealed that pediatric critical illness score (PCIS; HR = 0.879; 95% CI, 0.827– 0.935; P < 0.001) and serum albumin levels (HR = 0.921; 95% CI, 0.860– 0.987; P = 0.019) were independently associated with 30-day mortality. At the same time, there was no significant difference in 30-day mortality (42.9% versus 45.5%, P = 0.854) or clinical efficiency rate (53.4% versus 40.9%, P = 0.374) between with and without polymyxin B therapy.
Conclusion: The study revealed PCIS and serum albumin levels were the independent mortality-related risk factors of CRE infections in critically ill pediatric patients. Treatment with polymyxin B could not reduce 30-day mortality. Future prospective cohort studies are needed to investigate the optimal antimicrobial regimens for CRE infection in PICU patients.
Keywords: carbapenem-resistantEnterobacteriaceae, pediatric intensive care unit patients, mortality, risk factors, antimicrobial regimens
Introduction
With the worldwide prevalence of carbapenem-resistant Enterobacteriaceae (CRE), it has become a significant problem in terms of public health.1,2 Multi-drug resistance profile of CRE leads to considerable mortality. The overall 30-day mortality of CRE infections is approximately 30–50% in adult patients,3–5 and as high as 52% in children.6–8 Several factors such as immunocompromised status, sepsis/septic shock, and neutropenia have been reported to be significant risk factors for 30-day mortality in adult patients with CRE infection.5,9,10 However, limited data are available on the characteristics and risk factors of children with CRE infections, especially critically ill pediatric patients.
In addition, antimicrobial options against CRE infections are limited, and only a few antibiotics are available, including carbapenems, polymyxins, quinolone, aminoglycosides, and tigecycline.11,12 Due to significant adverse effects of some antibiotics, such as musculoskeletal adverse reactions of quinolones and ototoxicity and nephrotoxicity of aminoglycosides.13,14 And serious underlying diseases and complications, the treatment of CRE infections in pediatric intensive care unit (PICU) patients is a real challenge for clinicians.
This study aimed to identify the risk factors for 30-day mortality in PICU patients with CRE infections and to compare the clinical outcomes of different antimicrobial regimens for CRE infections.
Materials and Methods
Study Design and Patient Selection
We conducted a retrospective, observational cohort study of hospitalized patients with positive CRE cultures in PICU between January 2016 and December 2021. Inclusion criteria were (ⅰ) patients with positive cultures of CRE; (ⅱ) > 1 month old and < 18 years old. Exclusion criteria were (ⅰ) age < 1 month old or >18 years old; (ⅱ) polymicrobial infections; (ⅲ) hospital stay after positive culture of CRE < 24 h; (ⅳ) without clinical manifestation of CRE infection, which were determined by 3 experienced clinicians. The study was approved by the ethics review committee of the research project of the First Affiliated Hospital of Zhengzhou University (2022-KY-0168) and waived informed consent given the retrospective nature.
The primary outcome was all-cause mortality on day 30 after the onset of CRE infection. Clinical efficiency of antibiotic therapies was also analyzed.
Microbiology
The Vitek® 2 COMPACT automated system (France Biomerieux) was employed for bacterial identification and drug sensitivity tests. The biological samples included blood, sputum, urine, bronchial‐alveolar lavage fluid, abdominal drainage fluid, cerebrospinal fluid, and skin sanies. Carbapenem-resistant Enterobacteriaceae was defined as Enterobacteriaceae were resistant to ≥ 1 carbapenem antibiotics. Minimum inhibitory concentration (MIC) breakpoint ≥ 4 mg/L for meropenem/imipenem/doripenem or ≥ 2 mg/L for ertapenem was defined as carbapenem resistance.15 Isolated with MIC ≤ 2 mg/L were considered susceptible to polymyxins.16 Meanwhile, in accordance with the US FDA, MIC ≥ 8 mg/L represented bacterial resistance to tigecycline.17
Study Definitions
The severity of infection was assessed by pediatric critical illness score (PCIS) on the day of positive cultures of CRE.18 Pediatric index of mortality (PIM) 3 and pediatric risk of mortality (PRISM) III on the day of admission to PICU were used to predict the risk of mortality from CRE infection. Probability of death was determined by the PIM3 score, which was calculated from this formula (probability of death = exp (PIM3 score)/[1+exp (PIM3 score)]).19 Immunosuppression included immunosuppressive therapy and primary immune deficiency diseases. Multi-site infection was defined as the isolation of pathogens from ≥ 2 sites. Clinical efficiency was defined as clinical or microbiological improvement, including remission or resolution of infection symptoms and clearance of pathogenic microorganisms, which were determined by 3 experienced clinicians.
Data Collection
Data extracted from the electronic medical record, included demographics (age, weight, and gender), PCIS, underlying disease, invasive procedures (central venous catheterization, urinary catheterization, gastric catheterization), clinic features, infection sites and sensitivity of pathogenic bacteria, and blood biochemical indices on the day of positive cultures of CRE. Antimicrobial regimens and clinical efficiency were assessed at the end of CRE treatment. Thirty-day all-cause mortality was recorded from the day of positive cultures of CRE.
Statistical Analysis
Continuous variables were presented as median (interquartile ranges, IQR), and were analyzed by Mann–Whitney U-test. The Categorical variables were presented as numbers (%) and were analyzed by the Chi-square test or Fisher’s exact test. To determine risk factors for mortality, baseline feature between deceased and survived patients at the 30-day point were compared using univariate analysis. Risk factors with P<0.1 were included into a Cox proportional hazards model to establish independent predictors for the 30-day mortality. Statistical analyses were performed with SPSS software (version 26; SPSS Inc., Chicago, IL, USA). All tests were two-tailed, with the significance level set at 0.05.
Results
Patient Overview
During the study period, a total of 116 patients with CRE infection were included. Finally, 60 patients were excluded and 56 patients were enrolled in the analysis (Figure 1). Patient characteristics were shown in Table 1. The median patient age was 10 years (IQR, 2.7–11.7 years) and 39 (69.6%) were male. The highest proportion of pathogen was Klebsiella pneumoniae (n=37, 66.1%), followed by Escherichia coli (n=16, 28.6%), Klebsiella oxytoca (n=1, 1.8%), Citrobacter freundii (n=1, 1.8%), and Raoultella planticola (n=1, 1.8%). Among them, 12 patients (21.4%) had multi-site infections. The sites of CRE infection included bloodstream (n=29, 51.8%), pulmonary (n=27, 48.2%), intraperitoneal infection (n=5, 8.9%), and others (n=7, 12.5%; urinary tract n=2; intracranial n=2; skin n=3). The resistance rate to meropenem was over 90%, while the rest 10% was resistant to imipenem or ertapenem (Table S1). All isolated pathogens were susceptible to polymyxin B and 96.4% of them were susceptible to tigecycline.
 |
Table 1 Patient Characteristics |
 |
Figure 1 Flow chart of included patients with CRE infections. CRE, carbapenem-resistant Enterobacteriaceae; PICU, pediatric intensive care unit. |
Risk Factors for 30-Day Mortality in CRE-Infected Pediatric Patients
The overall 30-day mortality was 50% (n=28, Table 1). Among them, 25 children had infection-related mortality. As to the other 3 children, one died of pneumothorax and 2 died of pulmonary hemorrhage, unexpectedly (Table S2). Risk factors for 30-day mortality associated with CRE infection were investigated by Cox regression analysis. Since the probability of death was calculated by PIM3 score, only the probability of death was included in further analysis. Cox regression results suggested that serum albumin level (hazard ratio [HR] = 0.921; 95% confidence level [CI], 0.860–0.987; P = 0.019) and PCIS (HR = 0.879; 95% CI, 0.827–0.935; P < 0.001) were correlated with 30-day mortality (Figure 2), which was consistent with the result of infection-related mortality analysis (Figure S1).
 |
Figure 2 Cox regression of factors associated with 30-day mortality. HR, hazard ratio; CI, confidence interval; PCIS, pediatric critical illness score; MODS, multiple organ dysfunction syndrome. |
Furthermore, the area under the curve (ROC) of PCIS and serum albumin level for the perspective of 30-day mortality was 0.804 (95% CI, 0.692–0.916; P = 0.001) and 0.754 (95% CI, 0.627–0.881; P = 0.001), respectively (Figure 3). The optimum cut-off value of PCIS was 91, and its sensitivity and specificity were 57.1% and 46.4%, respectively. And the optimum cut-off value of serum albumin level was 28.4 g/L corresponding to 92.9% sensitivity and 46.2% specificity.
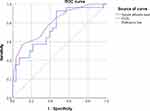 |
Figure 3 The area under the area under the curve of risk factor for the survive of CRE infections. CRE, carbapenem-resistant Enterobacteriaceae; PCIS, pediatric critical illness score. |
The Impacts of Different Antimicrobial Regimens on the 30-Day Mortality
Since 6 children received antibiotics treatment for less than 72 h, a total of 50 patients were included in the subgroup analysis. To investigate the effect of antimicrobial regimens on the 30-day mortality, patients were divided into polymyxin B group (n =28) and without polymyxin B group (n =22, Table 2). The 30-day mortality between patients with and without polymyxin B was no statistically significant difference (42.9% versus 45.5%, P = 0.854). The survival curves of the two treatment groups were shown in Figure 4. At the same time, there was also no statistically significant difference (53.4% versus 40.9%, P = 0.374; Table 3) for clinical efficiency.
 |
Table 2 Comparison of Characteristics and Treatment Between Patient with and without Polymyxin B |
 |
Table 3 The Impacts of Different Therapy on the 30-Day Mortality |
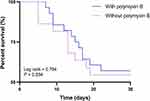 |
Figure 4 Survival rates of patients treated with polymyxin B and without polymyxin B. |
Discussion
We performed an observational cohort study that evaluated risk factors for 30-day mortality of CRE infections in PICU patients over a 6-year study period. The overall 30-day mortality of PICU patients with CRE infections was 50% and the most frequently isolated pathogen was K. pneumoniae (n=37, 66.1%), which was consistent with previous domestic and international epidemiologic data.3–8,20 In this study, hematological system disease, PCIS, serum albumin, platelet count, serum creatinine, and C-reactive protein were associated with mortality (Table 1). While only PCIS and serum albumin levels were the independent mortality-related risk factors in the Cox regression analysis (Figure 2).
For PICU patients, PIM3, PRISM III, and PCIS are commonly used mortality prediction models in pediatric patients.21–23 In this study, PCIS, as a pediatric scoring system based on China’s national conditions, showed a better correlation with 30-day mortality than PIM3 and PRISM III scores (Table 1). This may be because PCIS was assessed on the day of positive cultures of CRE, whereas PIM3 and PRISM III scores were assessed within 1 h and 24 h of PICU admission, respectively. Without dynamically assessing the scores at different time points, PIM3 and PRISM scores could not reflect the variable of diseases, leading to the inability to accurately predict the outcome. Nevertheless, PCIS does not include etiological scores, which may inaccurately predict the severity of the disease.22,23 Since this study only selected PICU patients with CRE infection, which model is more suitable for PICU patients needs to be further studied.
In general, blood biochemical indexes are also important signals reflecting the pathological status of diseases. This study showed that children who deceased were more likely to have lower albumin levels than survivors (28.1 versus 34.3 g/L, P = 0.001; Table 1). Low albumin levels or the more serious condition known as hypoalbuminemia, refers to serum albumin < 30 g/L, is a common clinical complication in critically ill patients.24 It is mainly caused by the following two reasons: a) inadequate intake and/or synthesis, such as liver disease and malnutrition; b) excessive consumption and/or loss, such as long-term fever, burns, nephrotic syndrome, etc. Low albumin levels can not only reflect the ailing physical condition but also affect the pharmacokinetics of drugs with high protein binding rates, thus affecting drug efficacy and clinical outcomes.24
Previous studies have identified several risk factors associated with the mortality of CRE infection, including sepsis/septic shock, immunosuppression or immunocompromised status, mechanical ventilation, and invasive procedures.8–10,25 Nevertheless, in our cohort more children suffered immunosuppression in the deceased group than those in the survived group, but it had no statistically significant difference (P = 0.086; Table 1). Other factors were not predictive of higher mortality.
To date, there are few universal standards of treatment for CRE infection in children.26 Due to limited available CRE-active antibiotics and for safety reasons, carbapenem-containing combination therapy tended to be the mainstay of treatment options.10 In this study, 41 children were treated with carbapenem. With regard to other antibacterial agents, polymyxin B was relaunched in China in 2018 for the treatment of drug-resistant Gram-negative infections. While pediatric data related to polymyxin B are limited.26 A systematic review of studies suggested that the microbiologic cure and survival of colistin were consistent with those reported in neonates and pediatrics in which multidrug-resistant Gram-negative bacteria were treated with other antibiotics,27,28 which was also found in this study (Table 3). However, due to the large time span of this study, new treatments and medications may affect mortality, such as extracorporeal membrane oxygenation and ceftazidime-avibactam.
In recent years, novel β-lactam-β-lactamase inhibitor agents (eg, ceftazidime-avibactam, meropenem-vaborbactam, and imipenem-relebactam) are gradually being used in the treatment of CRE infection in children.26 Among them, only ceftazidime-avibactam was available in China since 2019. In adults, retrospective studies have supported the preferential use of ceftazidime-avibactam over polymyxins for CRE infections.29,30 In our cohort, only three patients used ceftazidime-avibactam, and two showed clinical efficacy and survived (Table 3). However, although ceftazidime-avibactam is effective for most KPC- and OXA-48-producing Enterobacteriaceae, it has a narrow antibacterial spectrum which is not available against metallo-beta-lactamase (MBL)-producing Enterobacteriaceae,31 which is playing an increasingly important role in infections caused by CRE, especially in children.32 These findings in children require confirmation by randomized controlled trials in the future.
This study had several limitations. Firstly, this was a single-center retrospective study with a relatively small sample size. Therefore, the power of the analysis to identify risk factors of mortality and potential treatment regimens was limited. Secondly, the pharmacokinetics of antibiotics and drug-resistance genes in the bacteria isolated were not tested, which also could affect clinical outcomes.
Conclusion
In conclusion, the overall 30-day mortality of PICU patients with CRE infections was considerably high. PCIS and serum albumin levels were the independent mortality-related risk factors of CRE infections. There was no significant difference in the 30-day mortality between the antimicrobial regimens that did or did not contain polymyxin B. Future prospective cohort studies are needed to investigate the optimal antimicrobial therapies for CRE infection in critically ill pediatric patients.
Ethical Statement
This study has been approved by the ethics review committee of the research project of the First Affiliated Hospital of Zhengzhou University (2022-KY-0168) and waived informed consent given the retrospective nature. All samples were collected as part of routine management/surveillance and were anonymized prior to research use.
Acknowledgments
This work was supported by the Henan Province Science and Technology Research Project (grant 212102310442) and the Joint Construction Project of Henan Province Medical Science and Technology Program (grant LHGJ20200340).
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Potter RF, D’Souza AW, Dantas G. The rapid spread of carbapenem-resistant Enterobacteriaceae. Drug Resist Updat. 2016;29:30–46. doi:10.1016/j.drup.2016.09.002
2. Bogan C, Kaye KS, Chopra T, et al. Outcomes of carbapenem-resistant Enterobacteriaceae isolation: matched analysis. Am J Infect Control. 2014;42:612–620. doi:10.1016/j.ajic.2014.02.013
3. Almangour TA, Ghonem L, Aljabri A, et al. Ceftazidime-avibactam versus colistin for the treatment of infections due to carbapenem-resistant Enterobacterales: a multicenter cohort study. Infect Drug Resist. 2022;15:211–221. doi:10.2147/IDR.S349004
4. Zhou R, Fang X, Zhang J, et al. Impact of carbapenem resistance on mortality in patients infected with Enterobacteriaceae: a systematic review and meta-analysis. BMJ Open. 2021;11:e054971. doi:10.1136/bmjopen-2021-054971
5. Chen L, Han X, Li Y, et al. Assessment of mortality-related risk factors and effective antimicrobial regimens for treatment of bloodstream infections caused by carbapenem-resistant enterobacterales. Antimicrob Agents Chemother. 2021;65:e0069821. doi:10.1128/AAC.00698-21
6. Logan LK, Renschler JP, Gandra S, et al. Carbapenem-resistant Enterobacteriaceae in children, United States, 1999–2012. Emerg Infect Dis. 2015;21:2014–2021. doi:10.3201/eid2111.150548
7. Montagnani C, Prato M, Scolfaro C, et al. Carbapenem-resistant Enterobacteriaceae infections in children: an Italian retrospective multicenter study. Pediatr Infect Dis J. 2016;35:862–868. doi:10.1097/INF.0000000000001188
8. Nabarro LEB, Shankar C, Pragasam AK, et al. Clinical and bacterial risk factors for mortality in children with carbapenem-resistant Enterobacteriaceae bloodstream infections in India. Pediatr Infect Dis J. 2017;36:e161–e166. doi:10.1097/INF.0000000000001499
9. Zhou C, Jin L, Wang Q, et al. Bloodstream infections caused by carbapenem-resistant Enterobacterales: risk factors for mortality, antimicrobial therapy and treatment outcomes from a prospective multicenter study. Infect Drug Resist. 2021;14:731–742. doi:10.2147/IDR.S294282
10. Li C, Li Y, Zhao Z, et al. Treatment options and clinical outcomes for carbapenem-resistant Enterobacteriaceae bloodstream infection in a Chinese university hospital. J Infect Public Health. 2019;12(1):26–31. doi:10.1016/j.jiph.2018.08.002
11. David S, Reuter S, Harris SR, et al. Epidemic of carbapenem-resistant Klebsiella pneumoniae in Europe is driven by nosocomial spread. Nat Microbiol. 2019;4:1919–1929. doi:10.1038/s41564-019-0492-8
12. Durante-Mangoni E, Andini R, Zampino R. Management of carbapenem-resistant Enterobacteriaceae infections. Clin Microbiol Infect. 2019;25:943–950. doi:10.1016/j.cmi.2019.04.013
13. Patel K, Goldman JL. Safety concerns surrounding quinolone use in children. J Clin Pharmacol. 2016;56:1060–1075. doi:10.1002/jcph.715
14. Germovsek E, Barker CI, Sharland M. What do I need to know about aminoglycoside antibiotics? Arch Dis Child Educ Pract Ed. 2017;102:89–93. doi:10.1136/archdischild-2015-309069
15. Clinical and Laboratory Standards Institute. Performance Standards for Antimicrobial Susceptibility Testing.
16. European Committee on Antimicrobial Susceptibility Testing. Breakpoint Table for Interpretation of MICs and Zone Diameters, Version 9.0. Edition. European Committee on Antimicrobial Susceptibility Testing; 2019.
17. Wang H, Yu YS, Wang MG, et al. Expert consensus on the operating procedures for tigecycline in vitro susceptibility testing. Chin J Lab Med. 2013;36:584–587.
18. Watson RS, Choong K, Colville G, et al. Life after critical illness in children-toward an understanding of pediatric post-intensive care syndrome. J Pediatrics. 2018;198:16–24. doi:10.1016/j.jpeds.2017.12.084
19. Straney L, Clements A, Parslow RC, et al. Paediatric index of mortality 3: an updated model for predicting mortality in pediatric intensive care. Pediatr Crit Care Med. 2013;14:673–681. doi:10.1097/PCC.0b013e31829760cf
20. Haytoglu Z, Gundeslioglu OO, Yildizdas D, et al. Carbapenem and colistin resistance in children with Enterobacteriaceae infections. Turk J Pediatr. 2020;62:778–786. doi:10.24953/turkjped.2020.05.009
21. Gemke RJ, van Vught J. Scoring systems in pediatric intensive care: PRISM III versus PIM. Intensive Care Med. 2002;28:204–207. doi:10.1007/s00134-001-1185-2
22. Zhang LD, Huang HM, Cheng YC, et al. Predictive value of four pediatric scores of critical illness and mortality on evaluating mortality risk in pediatric critical patients. Chin Crit Care Med. 2018;30:51–56. doi:10.3760/cma.j.issn.2095-4352.2018.01.010
23. Lee OJ, Jung M, Kim M, et al. Validation of the pediatric index of mortality 3 in a single pediatric intensive care unit in Korea. J Korean Med Sci. 2017;32:365–370. doi:10.3346/jkms.2017.32.2.365
24. Vincent JL, Russell JA, Jacob M, et al. Albumin administration in the acutely ill: what is new and where next? Crit Care. 2014;18:231. doi:10.1186/cc13991
25. Bar-Yoseph H, Cohen N, Korytny A, et al. Risk factors for mortality among carbapenem-resistant Enterobacteriaceae carriers with focus on immunosuppression. J Infect. 2019;78:101–105. doi:10.1016/j.jinf.2018.10.003
26. Tamma PD, Gerber JS, Hayes M, et al. Treatment of carbapenem-resistant Enterobacteriaceae infections in children. J Pediat Inf Dis Soc. 2020;9:56–66. doi:10.1093/jpids/piz085
27. Sahbudak Bal Z, Kamit Can F, Yazici P, et al. The evaluation of safety and efficacy of colistin use in pediatric intensive care unit: results from two reference hospitals and review of literature. J Infect Chemother. 2018;24:370–375. doi:10.1016/j.jiac.2017.12.017
28. Nakwan N, Chokephaibulkit K, Imberti R. The use of colistin for the treatment of multidrug-resistant Gram-negative infections in neonates and infants: a review of the literature. Pediatr Infect Dis J. 2019;38:1107–1112. doi:10.1097/INF.0000000000002448
29. van Duin D, Lok JJ, Earley M, et al. Colistin versus ceftazidime-avibactam in the treatment of infections due to carbapenem-resistant Enterobacteriaceae. Clin Infect Dis. 2018;66:163–171. doi:10.1093/cid/cix783
30. Hakeam HA, Alsahli H, Albabtain L, et al. Effectiveness of ceftazidime-avibactam versus colistin in treating carbapenem-resistant Enterobacteriaceae bacteremia. Int J Infect Dis. 2021;109:1–7. doi:10.1016/j.ijid.2021.05.079
31. Castanheira M, Rhomberg PR, Flamm RK, et al. Effect of the beta-lactamase inhibitor vaborbactam combined with meropenem against serine carbapenemase-producing Enterobacteriaceae. Antimicrob Agents Chemother. 2016;60:5454–5458. doi:10.1128/AAC.00711-16
32. Fu B, Yin D, Sun C, et al. Clonal and horizontal transmission of blaNDM among Klebsiella pneumoniae in children’s intensive care units. Microbiol Spectr. 2022;10:e0157421. doi:10.1128/spectrum.01574-21
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
