Back to Journals » Infection and Drug Resistance » Volume 16
Multidrug-Resistant Bacteria on Critically Ill Patients with Sepsis at Hospital Admission: Risk Factors and Effects on Hospital Mortality
Authors Maia MDO, da Silveira CDG, Gomes M, Fernandes SES , Bezerra de Santana R , de Oliveira DQ, Amorim FFP , Neves FDAR , Amorim FF
Received 17 January 2023
Accepted for publication 17 March 2023
Published 23 March 2023 Volume 2023:16 Pages 1693—1704
DOI https://doi.org/10.2147/IDR.S401754
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Prof. Dr. Héctor Mora-Montes
Marcelo de Oliveira Maia,1,2 Carlos Darwin Gomes da Silveira,1,3,4 Maura Gomes,5 Sérgio Eduardo Soares Fernandes,3 Rosália Bezerra de Santana,3 Daniella Queiroz de Oliveira,3 Felipe Ferreira Pontes Amorim,4 Francisco de Assis Rocha Neves,2 Fábio Ferreira Amorim1,2
1Graduation Program in Health Sciences of School Health Sciences, Escola Superior de Ciências da Saúde (ESCS), Brasília, Federal District, Brazil; 2Graduation Program in Health Sciences, University of Brasília (UnB), Brasília, Federal District, Brazil; 3Medical School, Escola Superior de Ciências da Saúde (ESCS), Brasília, Federal District, Brazil; 4Medical School, Centro Universitário do Planalto Central (UNICEPLAC), Brasília, Federal District, Brazil; 5Intensive Care Unit, Hospital Santa Luzia Rede D’Or São Luiz, Brasília, Federal District, Brazil
Correspondence: Fábio Ferreira Amorim, Coordenação de Pesquisa e Comunicação Científica - Escola Superior de Ciências da Saúde, SMHN Quadra 03, conjunto A, Bloco 1 - Edifício FEPECS, Brasília, Federal District, 70701-907, Brazil, Email [email protected] Marcelo de Oliveira Maia, Programa de Pós-Graduação em Ciências da Saúde - Escola Superior de Ciências da Saúde, SMHN Quadra 03, conjunto A, Bloco 1 - Edifício FEPECS, Brasília, Federal District, 70701-907, Brazil, Email [email protected]
Purpose: To evaluate the effect of MDRO infection on hospital mortality and the risk factors among critically ill patients with sepsis at hospital admission.
Patients and Methods: A cross-sectional study was performed between April 2019 and May 2020, followed by a cohort to evaluate hospital mortality that prospectively included all consecutive patients 18 years or older with sepsis admitted within 48 hours of hospital admission to an adult ICU in Brazil. Patients’ characteristics, blood samples within one hour of ICU admission, and microbiological results within 48h of hospital admission were collected. In addition, descriptive statistics, binary logistic regression, and propensity score matching were performed.
Results: At least one MDRO was isolated in 85 patients (9.8%). The extended-spectrum beta-lactamase-producing Enterobacterales are the most frequent organism (56.1%). Hypoxemic acute respiratory failure (OR 1.87, 95% CI 1.02– 3.40, p = 0.04), Glasgow Coma Score below 15 (OR 2.57, 95% CI 1.38– 4.80, p < 0.01), neoplasm (OR 2.66, 95% CI 1.04– 6.82, p = 0.04) and hemoglobin below 10.0 g/dL (OR 1.82, 95% CI 1.05– 3.16, p = 0.03) were associated with increased MDRO. Admission from the Emergency Department (OR 0.25, 95% CI 0.14– 0.43, p < 0.01) was associated with decreased MDRO. In the multivariate analysis, MDRO at hospital admission increased hospital mortality (OR 2.80, 95% CI 1.05– 7.42, p = 0.04). After propensity score-matching adjusted to age, APACHE II, SOFA, and dementia, MDRO at hospital admission was associated with significantly high hospital mortality (OR 2.80, 95% CI 1.05– 7.42, p = 0.04). The E-value of adjusted OR for the effect of MDRO infection on hospital mortality was 3.41, with a 95% CI of 1.31, suggesting that unmeasured confounders were unlikely to explain the entirety of the effect.
Conclusion: MDRO infection increased hospital mortality, and MDRO risk factors should be accessed even in patients admitted to ICU within 48 hours of hospital admission.
Keywords: drug resistance, multiple, bacterial, community-acquired infections, sepsis, risk factors, mortality
Introduction
Sepsis remains a significant cause of death in critically ill patients, with more than a third of septic patients dying during the hospital stay. Furthermore, it accounts for a considerable amount of the intensive care unit (ICU) costs.1–3 In an attempt to reduce mortality and morbidity from sepsis and septic shock, initiatives, such as the Surviving Sepsis Campaign, were established to support the choice of therapies, improving the care of sepsis.4–7
Despite the advances in its knowledge and management, sepsis treatment remains a challenge. Nowadays, antibiotics are still the only effective drugs against sepsis, mainly when used early. Indeed, the outcomes of patients with sepsis, regardless of the resistance condition of the agent causing the infection, improve significantly if timely and appropriate therapy. On the other hand, inappropriate antibiotic therapy is undoubtedly associated with several serious consequences, including increased mortality.7–12 However, the treatment with broad-spectrum antibiotics in patients with a low risk of multidrug-resistant organisms (MDRO) infection may expose patients to the risk of the emergence of drug-resistant pathogens.13–17
In recent decades, a surge of MDRO in community-acquired infections has been identified, such as extended-spectrum beta-lactamase-producing Enterobacteriaceae (ESBL-Enterobacteriaceae) and methicillin-resistant Staphylococcus aureus (MRSA).18–21 Furthermore, MDRO infections are traditionally associated with nosocomial infections, and there is a rising risk of this condition not being suspected or even identified late in community-acquired infections. These aspects may increase the chance of instituting inadequate initial empirical antibiotic therapy and mortality in these infections.21–23
Regarding the increased prevalence of MDRO, the primary purpose of the study was to evaluate the effect of MDRO infection at hospital admission on hospital mortality among critically ill adult patients with sepsis at hospital admission. The secondary purposes were to identify the prevalence of MDRO infection, and factors associated with MDRO infection at hospital admission and hospital mortality.
Materials and Methods
Study Design and Participants
This was a cross-sectional study performed between April 2019 and May 2020, followed by a cohort to evaluate hospital mortality that prospectively included all consecutive patients 18 years or older with sepsis admitted within 48 hours of hospital admission to the Hospital Santa Luzia Rede D’Or São Luis adult ICU. The Hospital Santa Luzia Rede D’Or São Luis adult ICU is a 60-bed mixed medical/surgical adult ICU at a private tertiary hospital in Federal District, Brazil.
The inclusion criteria were patients 18 or older, sepsis as the primary reason for ICU admission, and ICU admission within 48 hours of hospital admission. The exclusion criteria were patients transferred to an ICU of another hospital, incomplete medical records that would hamper the analysis, and absence of culture collected within 48 hours of hospital admission. Eight hundred and seventy-seven adult patients with sepsis were admitted to the ICU within 48 hours of hospital admission. Thirteen patients were excluded due to transfer to an ICU of another hospital (1.48%), and no patient was excluded due to the other exclusion criteria. Thus, 864 patients were included in the study.
Data Collection
Patients’ general characteristics and blood samples within the first hour of ICU admission were collected from the hospital medical records and electronic systems. The variables collected were age, gender, the primary reason for hospital admission, referred unit (Emergency Department (ED), surgery room, ward and nursing home or long-term care facility), site of primary infection, Acute Physiology and Chronic Health Evaluation II (APACHE II) score, Sequential Organ Failure Assessment (SOFA) score, functional independence, comorbidities, vasopressor use on the first hour of ICU admission, axillary temperature, Glasgow Coma Score, the fraction of inspired oxygen (FiO2), and laboratory and microbiological data. Laboratory samples (blood count, serum creatinine, arterial oxygen partial pressure - PaO2, and arterial lactate) were collected within the first hour of ICU admission. Hypoxemic acute respiratory failure was defined as a PaO2/FiO2 ratio below 300. Sepsis was defined according to the Third International Consensus Definitions for Sepsis and Septic Shock.24 Immunosuppression was defined by at least one of the following medical conditions: active hematologic malignancy, transplantation, immunosuppressive therapy, chemotherapy, and radiotherapy within the 30 days before ED admission, chronic systemic steroid therapy, splenectomy, and autoimmune disease.
Microbiological results performed within 48 hours of hospital admission were recorded, including blood, sputum, tracheobronchial aspirate, urine, wound, and mucosal swab cultures. Per routine clinical practice, mucosal swabs were obtained from all patients at ICU admission as a screening for MDRO. However, MDRO detected on ICU admission only by the mucosal swab was treated as colonization and was not considered sepsis causative microbiological.
Species identification and antimicrobial susceptibility testing were performed using an automated system; susceptibility breakpoints were based on the Brazilian version of the European Committee on Antimicrobial Susceptibility Testing (EUCAST/BrCAST version) guideline.25 Pseudomonas spp and Acinetobacter spp resistant to three classes of antibiotics among antipseudomonal penicillins, antipseudomonal cephalosporins, carbapenems, quinolones, and aminoglycosides, ESBL-Enterobacteriaceae, carbapenemase-producing Pseudomonas spp, Acinetobacter spp or Enterobacterales (KPC), vancomycin-resistant Enterococcus spp (VRE), staphylococci resistant to oxacillin, and other pathogens with acquired non-susceptibility to at least one agent in three or more antimicrobials categories were considered as an MDRO.1,26 For ESBL and Carbapenemases producing organisms, phenotypic tests have been performed to define the resistance. ESBL enzyme research was tested through the technique of the E-test, and Carbapenemase (KPC, New Delhi metallo-β -lactamase – NDM, VIMP, and OXA-48) was evaluated using the Blue-Carba test and enzymatic inhibition by phenylburonic acid to inhibit KPC, EDTA to inhibit metallo-β-lactamase, and cloxacillin to inhibit Oxa 48. The predominant Carbapenemases are KPC and NDM. Phenotypic tests for metallo-β-lactamase production in those positive for an enzymatic test by EDTA were taken by genetic method to search for the dominant gene. All were positive for BLANDM, the gene that proves the presence of NDM enzyme production.
The main outcomes evaluated were MDRO infection at hospital admission and hospital mortality. Other outcomes evaluated were ICU length of stay (ICU-LOS), and hospital length of stay (hospital-LOS).
Statistical Analysis
According to their distribution evaluated by the Kolmogorov–Smirnov test with Liliefors correction, quantitative data with normal distribution are expressed as mean ± standard deviation (SD) and quantitative data with non-parametric distribution as median and interquartile range 25–75% (IQR 25–75%). The variables with normal distribution were age and APACHE II. Categorical variables are expressed as numbers and percentages (%).
Patients were grouped according to the independent variable studied, considering the outcome to be analyzed (MDRO infection at hospital admission, ICU-LOS, hospital-LOS, ICU mortality, and hospital mortality). Contingency tables were used for categorical variables, and Pearson’s Chi-square test (χ2) or Fisher’s exact test was used as appropriate. Regarding the hospital mortality, Student’s t-test was used to compare age and APACHE II and Mann–Whitney test to compare SOFA between survivors and non-survivors.
To evaluate independent factors associated with MDRO infection at hospital admission and hospital mortality, an enter method binary logistic regression analysis was performed, including non-collinear variables associated with the outcome with a p-value <0.05 in the univariate analysis and the confounding factors according to previous knowledge with p-value <0.20 in the univariate analysis.27 Non-collinearity was accepted when the tolerance was higher than 0.10 and the variance inflation factor (VIF) was lower than 10.0. The odds ratio (OR) expressed the results with their respective 95% confidence interval (95% CI).
To assess the effect of MDRO infection at hospital admission on hospital mortality, propensity score-matching for MDRO infection at hospital admission applying a logit regression model adjusted to factors independently associated with hospital mortality (age, APACHE II, SOFA, and dementia) and MDRO infection at hospital admission (hypoxemic acute respiratory failure, Glasgow Coma Score below 15, neoplasm, anemia with hemoglobin below 10.0 g/dL, and admission from ED) was performed using the EZR software version 1.54 (Saitama Medical Center, Jichi Medical University, Japan) with a 1:1 pair-matching ratio without replacement on the logit of the propensity score applying a caliper of width equal to 0.2. The OR and 95% CI of the MDRO infection at hospital admission effect on hospital mortality were calculated in the sample after matching and is shown as a forest plot.
For sensitivity analysis, we used the E-value to measure the robustness of the association between MDRO infection at hospital admission and hospital mortality for unmeasured or unadjusted confounding.28 E-values were computed with an online E-value calculator (https://www.evalue-calculator.com/).29
Statistical analyses were performed using IBM Statistical Package for Social Sciences 20.0 for Mac (SPSS 20.0 Mac, SPSS Inc., Chicago, USA), statistical software R version 4.0.5 (R Foundation for Statistical Computing), and EZR software version 1.54 (Saitama Medical Center, Jichi Medical University, Japan). The level of statistical significance was defined as a two-sided p-value ≤0.05.
Ethical Approval and Consent Form
The Institutional Review Board of the Education and Research Foundation of Health Sciences (FEPECS), Brasília, Federal District, Brazil, approved the study under opinion number 3,246,136 with a waiver of informed consent. The study was conducted following the Declaration of Helsinki. Since this study had no specific intervention and only used anonymized medical record data that generated results in an aggregate manner that did not allow participants’ identification, the written consent form was unnecessary.
Results
Among the 864 patients included in the study, the mean age was 62.5 ± 21.3 years, and APACHE II was 15.1 ± 7.3. Median SOFA was 2.0 (IQR 25–75%: 2.0–4.0), 56.1% were female (485/864), and 9.8% had at least one MDRO isolated at the time of ICU admission (85/864). ICU mortality and hospital mortality were 9.8% (85/864) and 11.6% (100/864), respectively (Supplementary Table S1)
The main sites of primary infection were the lung (50/85, 58.8%), urinary tract (16/85, 18.8%), and digestive/abdominal cavity (9/85, 10.6%). The main MDROs were ESBL-Enterobacterales (64/114, 56.1%), oxacillin-resistant coagulase-negative Staphylococcus spp (17/114, 14.9%), methicillin-resistant Staphylococcus aureus (10/114, 8.8%), and carbapenemase-producing Pseudomonas spp, Acinetobacter spp, or Enterobacterales e (7/114, 6.1%). (Supplementary Table S2)
Table 1 shows the univariate analysis of variables associated with MDRO infection at hospital admission. Age above 60 years (75.3% versus 56.9%, p < 0.01), APACHE II above 16 (71.8% versus 42.6%, p < 0.01), two or more system failure on SOFA score (75.3% versus 57.6%, p < 0.01), hypoxemic acute respiratory failure (31.8% versus 16.8%, p < 0.01), Glasgow Coma Score below 15 (60.0% versus 22.5%, p < 0.01), anemia with hemoglobin below 10.0 g/dL (43.5% versus 21.2%, p < 0.01), leukocytosis with more than 11,000 leukocytes/mm3 (44.7% versus 34.0%, p = 0.05) were higher in patients with MDRO infection at hospital admission than in patients without MDRO infection. Among the comorbidities, MDRO infection at hospital admission was increased in oncologic patients (29.4% versus 17.7%, p = 0.01), immunosuppression (32.9% versus 23.1%, p = 0.04), thrombocytopenia with lower than 200,000 platelets/mm3 (41.2% versus 34.0%, p = 0.05), and patients with previous stroke with permanent sequels (11.8% versus 4.9%, p = 0.01). Patients admitted referred from ED (44.7% versus 77.9%, p < 0.01) and functional independence (17.6% versus 40.0%, p < 0.001) were associated with decreased MDRO infection at hospital admission.
Table 2 shows the multivariate analysis of variables associated with MDRO infection at hospital admission. Hypoxemic acute respiratory failure (OR 1.87, 95% CI 1.02–3.40, p = 0.04), Glasgow Coma Score below 15 (OR 2.57, 95% CI 1.38–4.80, p < 0.01) neoplasm (OR 2.66, 95% CI 1.04–6.82, p = 0.04) and anemia with hemoglobin below 10.0 g/dL (OR 1.82, 95% CI 1.05–3.16, p = 0.03) were independently associated with a high rate of MDRO infection at hospital admission, while admission from ED (OR 0.25, 95% CI 0.14–0.43, p < 0.01) was independently associated with a low rate of MDRO infection at hospital admission.
 |
Table 2 Multivariate Analysis of Variables Associated with Multidrug-Resistant Organisms Infection at Hospital Admission |
Patients with MDRO infection at hospital admission had increased ICU-LOS (median 13.0 days, IQR 25–75% 6.5–29.5 days versus 4.0 days, IQR 25–75% 3.0–8.0 days, p < 0.01), hospital-LOS (median 20.0 days, IQR 25–75% 11.0–42.5 days versus 8.0 days, IQR 25–75% 5.0–7.0 days, p < 0.01), ICU mortality (25.0% versus 8.1%, p < 0.01), and hospital mortality (29.4% versus 9.5%, p < 0.01) (Supplementary Table S3).
Table 3 shows the univariate analysis of variables associated with hospital mortality. MDRO infection at hospital admission (25.0% versus 7.9%, p < 0.01), hypoxemic acute respiratory failure (33.0% versus 16.4%, p < 0.01), vasopressor use on the first hour of ICU admission (18.0% versus 3.1%, p < 0.01), and serum creatinine above 1.4 mg/dL (40.4% versus 19.1%, p < 0.01) were increased in non-survivors (25.0% versus 7.9%, p < 0.01). Non-survivors were older (77.6 ± 15.6 years versus 63.6 ± 21.4 years, p < 0.01), and had higher APACHE II (22.8 ± 7.2 years versus 14.1 ± 6.7 years, p < 0.01), and SOFA (median 5.0, IQR 25–75% 3.0–7.0 versus 2.0 days, IQR 25–75% 2.0–3.8, p < 0.01) than survivors. Among the comorbidities, immunossupression (35.0% versus 22.6%, p = 0.01), neoplasm (31.0% versus 17.3%, p = 0.001), and dementia (12.0% versus 3.3%, p < 0.01) were increased in non-survivors. Non-survivors had a decreased functional independence (15.0% versus 41.4%, p < 0.01) than survivors.
 |
Table 3 Univariate Analysis of Variables Associated with Hospital Mortality (n = 864) |
Table 4 shows the multivariate analysis of variables associated with hospital mortality. Age (OR 1.04, 95% CI 1.02–1.07, p < 0.01), APACHE II (OR 1.07, 95% CI 1.01–1.13, p = 0.02), SOFA (OR 1.23, 95% CI 1.09–1.50, p < 0.01), MDRO bacterial infection at hospital admission (OR 2.00, 95% CI 1.06–3.77, p = 0.03) and dementia (OR 2.57, 95% CI 1.10–5.98, p = 0.03) were independently associated with an increased hospital mortality.
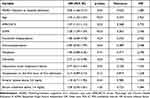 |
Table 4 Multivariate Analysis of Variables Associated with Hospital Mortality |
Figure 1 shows the effect of MDRO infection at hospital admission on hospital mortality after propensity score-matching adjusted to age, APACHE II, SOFA, and dementia. MDRO infection at hospital admission was associated with significantly high hospital mortality (OR 2.80, 95% CI 1.05–7.42, p = 0.04). The E-value of adjusted OR for the association between MDRO infection at hospital admission and hospital mortality in multivariate analysis was 3.41, with a 95% CI of 1.31, suggesting that unmeasured confounders were unlikely to explain the entirety of the effect.
Discussion
In this study, almost one in every ten patients admitted with sepsis had at least one MDRO infection at hospital admission. This condition was independently associated with increased hospital mortality. Besides, ICU-LOS and hospital-LOS were longer in patients admitted with MDRO infection than those without MDRO infection. Hypoxemic acute respiratory failure, alteration in the level of consciousness (GCS < 15), neoplasm and anemia (Hb <10.0 g/dL) were independently associated with a high rate of MDRO infection. On the contrary, admission referred from ED was independently associated with a decreased MDRO infection at hospital admission. These findings reinforce the importance of being aware of the possibility of MDRO infection even in patients with sepsis at hospital admission to guide an appropriate antibiotic therapy with a broad spectrum, especially in patients with risk factors for MDRO infection.7–12,30,31
Previous studies have shown conflicting results regarding MDRO infection and mortality.1,32–34 Either way, there is an agreement that MDRO is a risk factor for inappropriate antibiotic therapy, which is undoubtedly associated with increased mortality.7–12,30,31 Similar to our finding, one study that evaluated patients with sepsis from the community, the MDRO was also associated with increased mortality.1 It might be discussed if other factors that influence the risk for MDRO and mortality might have influenced the high mortality observed among patients with MDRO infections.1,21 However, in our study, the effect of MDRO infection at hospital admission on hospital mortality remained after adjustment for the propensity score matching with an odds ratio of 2.8.
The incidence of MDRO at hospital admission in our study (9.8%) is slightly lower than observed in a United States study (12.0%)34 and an Italian study (17.0%)1 that also included patients with sepsis coming from the community. In a study that evaluated only patients with urinary tract infections presented to an ED, the prevalence of MDRO at hospital admission (6.7%) was lower than observed in our study.35 It should be noted that the primary site of sepsis in our study was the lung (57.5%), representing more than half of the cases, followed by the urinary tract (17.9%), agreeing with previously published studies.1,36,37
As observed in previous studies involving patients with community-acquired infectious and nosocomial infectious1,21,35,38–42 gram-negative bacteria (GNB) were the most prevalent MDRO in our study, and the ESBL-Enterobacterales was the most isolated agent. However, one finding that should be highlighted is that 6.1% of isolated MDRO were carbapenemase-producing GNB, and 82.9% of patients with MDRO infections at hospital admission were not referred from nursing homes or long-term care facilities. This emergence of carbapenemases-producing GNB is worrisome since the carbapenemases give resistance to a broad range of antibiotics, including the carbapenems, the class of antibiotics with a broader spectrum for bacterial infectious treatment. Furthermore, carbapenemases-producing GNB commonly has additional resistance mechanisms against beta-lactamase inhibitors and other antimicrobials, including resistance to aminoglycosides and fluoroquinolones.43 Thus, the presence of a carbapenemase-producing GNB leads to a small range of therapeutic options and greatly increases the risk of inappropriate therapy.43–45 Indeed, there are reports of community infections by ESBL-producing Enterobacterales that have acquired the ability to produce carbapenemases, especially related to the clone Escherichia coli ST131 in India and the United States.45–48 It is also important to note that, although GNB was the most common MDRO in our study, the patterns of the MDRO infections and the resistance highly depend on the studied region. For example, in the United States, one study observed that the most prevalent MDRO was vancomycin-resistant Enterococci, followed by MRSA. At the same time, GNB infections were uncommon, and carbapenemases-producing Enterobacterales was isolated in only one patient.34 In another study that included only patients with pneumonia presenting to the ED, MRSA was the most prevalent MDRO.11
Hypoxemic acute respiratory failure, alteration in consciousness level (GCS < 15), neoplasm and anemia (Hb <10.0 g/dL) were independently associated with MDRO-related sepsis among the MDRO risk factors evaluated in our study. Besides, referred ICU admissions from hospital units other than ED were associated with MDRO infection. Classically, the two risk factors mainly reported for MDRO in patients from the community are prior hospitalization in the past 90 days and nursing home or long-term care facility.21,38,49–51 In this respect, in our study, only 8.0% of patients were referred from nursing homes or long-term care facilities. Besides, the patients referred from ED also had fewer MDRO infections at hospital admission than those from the surgery room and wards. This finding highlights that a patient who passed through another hospital unit from the ED before ICU admission is more prone to have an MDRO infection than an ICU-admitted patient directly from the ED, even if that admission occurred within the first 48 hours of hospitalization. However, it is unclear why our analysis identified patients referred from ED had a reduced risk for MDRO infection. We suspect it may be a surrogate marker for other factors associated with MDRO infection risks, such as recent hospitalization and previous antibiotic use. Besides, even though they were admitted before 48 hours of hospitalization, these patients tend to stay longer in the hospital until the ICU admission than patients admitted directly from the ED, which may have exposed them to contact with MDRO even for a short period. It is essential to note that previous studies that evaluated factors associated with MDRO in patients with community-acquired infections did not assess the hospital unit that referred to the ICU admission or included only patients admitted from the ED.1,21,34,38,41,49–51
Our study has some limitations. First, the study included patients from only one center, which has intrinsic limitations for generalizing the results, primarily because different causative pathogens of sepsis, different rates of antibiotic resistance, and risk factors related to different health-care organizations have been recognized worldwide. Second, the study was performed in a private tertiary hospital, limiting the generalization to other Brazilian health-care services, especially public ones, since there is a well-documented difference in access to technologies between Brazilian public and private health-care services.52 Third, we cannot rule out that the difference in outcomes among the groups may have been affected by factors not evaluated in our study. In an Italian study that assessed a wide range of risk factors for MDRO in a large sample of patients with sepsis from the community, the independent risk factors for MDRO were septic shock and hospitalization in the past 90 days.1 Regarding septic shock, our study did not show an association between vasopressor use and arterial lactate above 2.0 mg/dL during the first hour of ICU admission and sepsis by MDRO infection at hospital admission. Regarding the previous hospitalization, we did not assess this variable, and also the antimicrobial use in the past 90 days that is another classical risk factor for MDRO infection, especially considering that there were 24.1% immunosuppressed patients (32.9% of patients with MDRO) that is a condition associated with therapeutic or prophylactic antimicrobial use. Although the lack of information on these variables may be one of the study limitations, it depends mainly on the patients’ or family members’ retrospection, and it is not always informed accurately during the initial management of a patient with sepsis when the initial antibiotic therapy needs to be chosen quickly. Despite these limitations, the sensitivity analysis using the E-value suggests that unmeasured confounders were unlikely to explain the entirety of the effect observed in our study to the point of modifying the observed results. Finally, we did not evaluate the appropriateness of the initial antibiotic therapy. According to our institutional protocol, adult patients with sepsis or septic shock without known traditional risk factors for MDRO infection use Piperacillin and Tazobactam as an empiric treatment for GNB based on Brazilian local epidemiology. In contrast, patients with a known risk for MDRO infection use carbapenem. It is interesting to note that the hospital mortality in our study (11.6%) was below that observed in previous studies that evaluated patients with sepsis coming from the community, such as an Italian study (25.7%)1 and a United States study (20.2%).34 The factors associated with this finding may be associated with the sepsis protocol of our institution that aims to promote rapid recognition and implement early management for this condition, including the appropriate initial antibiotic therapy, considering that only 58.7% of the patients had appropriate empiric antibiotic therapy according to local guidelines and 66.8% according to antibiotic susceptibility of the isolated pathogen in the Italian study.1 Nevertheless, notwithstanding if the MDRO infection is an independent risk factor for mortality or a risk factor for inappropriate antibiotic therapy,7–12,28,29 our study shows that identifying septic patients with a high risk for MDRO is crucial for appropriate antibiotic therapy and reduces sepsis mortality. Regardless of the limitations, our findings reinforce the importance of being aware of the possibility of MDRO infection, even in patients with sepsis at hospital admission, since it was associated with a high hospital mortality rate.
Conclusion
In our study, almost ten percent of critically ill patients admitted with sepsis at hospital admission had at least one MDRO infection. This condition was independently associated with increased hospital mortality. Due to the increased risk of MDRO infection, treatment with broader antibiotic choices should be considered in patients with sepsis from the community associated with hypoxemic acute respiratory failure, impaired consciousness, neoplasm, and anemia. Besides, patients referred to ICU from the Emergency Department were at lower risk for MDRO infection than patients from nursing homes, long-term care facilities, or wards, even if the ICU admission occurred within 48 hours of hospital admission.
Disclosure
The authors report no conflicts of interest in this work.
References
1. Capsoni N, Bellone P, Aliberti S, et al. Prevalence, risk factors and outcomes of patients coming from the community with sepsis due to multidrug resistant bacteria. Multidiscip Respir Med. 2019;14:23. doi:10.1186/s40248-019-0185-4
2. Fleischmann C, Scherag A, Adhikari NK, et al. Assessment of global incidence and mortality of hospital-treated sepsis. current estimates and limitations. Am J Respir Crit Care Med. 2016;193(3):259–272. doi:10.1164/rccm.201504-0781OC
3. Rhodes A, Evans LE, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock: 2016. Intensive Care Med. 2017;43(3):304–377. doi:10.1007/s00134-017-4683-6
4. Nguyen HB, Rivers EP, Abrahamian FM, et al. Emergency department sepsis education program and strategies to improve survival (ED-SEPSIS) working group. Severe sepsis and septic shock: review of the literature and emergency department management guidelines. Ann Emerg Med. 2006;48(1):28–54. doi:10.1016/j.annemergmed.2006.02.015
5. Dellinger RP, Carlet JM, Masur H, et al. Surviving sepsis campaign management guidelines committee. surviving sepsis campaign guidelines for management of severe sepsis and septic shock. Crit Care Med. 2004;32(3):858–873. doi:10.1097/01.ccm.0000117317.18092.e4
6. Evans L, Rhodes A, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Crit Care Med. 2021;49(11):e1063–e1143. doi:10.1097/CCM.0000000000005337
7. Lisboa T, Nagel F. Infection with multi-resistant agents in the ICU: how to escape? Rev Bras Ter Intensiva. 2011;23(2):120–124. doi:10.1590/S0103-507X2011000200003
8. Ibrahim EH, Sherman G, Ward S, Fraser VJ, Kollef MH. The influence of inadequate antimicrobial treatment of bloodstream infections on patient outcomes in the ICU setting. Chest. 2000;118(1):146–155. doi:10.1378/chest.118.1.146
9. Kumar A, Ellis P, Arabi Y, et al. Initiation of inappropriate antimicrobial therapy results in a fivefold reduction of survival in human septic shock. Chest. 2009;136(5):1237–1248. doi:10.1378/chest.09-0087
10. Chen HC, Lin WL, Lin CC, et al. Outcome of inadequate empirical antibiotic therapy in emergency department patients with community-onset bloodstream infections. J Antimicrob Chemother. 2013;68(4):947–953. doi:10.1093/jac/dks475
11. Shorr AF, Micek ST, Welch EC, Doherty JA, Reichley RM, Kollef MH. Inappropriate antibiotic therapy in Gram-negative sepsis increases hospital length of stay. Crit Care Med. 2011;39(1):46–51. doi:10.1097/CCM.0b013e3181fa41a7
12. Kang CI, Kim SH, Park WB, et al. Bloodstream infections caused by antibiotic-resistant gram-negative bacilli: risk factors for mortality and impact of inappropriate initial antimicrobial therapy on outcome. Antimicrob Agents Chemother. 2005;49(2):760–766. doi:10.1128/AAC.49.2.760-766.2005
13. Tandon P, Delisle A, Topal JE, Garcia-Tsao G. High prevalence of antibiotic-resistant bacterial infections among patients with cirrhosis at a US liver center. Clin Gastroenterol Hepatol. 2012;10(11):1291–1298. doi:10.1016/j.cgh.2012.08.017
14. Klevens RM, Morrison MA, Nadle J, et al. Invasive methicillin-resistant Staphylococcus aureus infections in the United States. JAMA. 2007;298(15):1763–1771. doi:10.1001/jama.298.15.1763
15. Moran GJ, Krishnadasan A, Gorwitz RJ, et al. Methicillin-resistant S. aureus infections among patients in the emergency department. N Engl J Med. 2006;355(7):666–674. doi:10.1056/NEJMoa055356
16. Zilberberg MD, Shorr AF, Micek ST, Vazquez-Guillamet C, Kollef MH. Multi-drug resistance, inappropriate initial antibiotic therapy and mortality in Gram-negative severe sepsis and septic shock: a retrospective cohort study. Crit Care. 2014;18(6):596. doi:10.1186/s13054-014-0596-8
17. Trouillet JL, Chastre J, Vuagnat A, et al. Ventilator-associated pneumonia caused by potentially drug-resistant bacteria. Am J Respir Crit Care Med. 1998;157(2):531–539. PMID: 9476869. doi:10.1164/ajrccm.157.2.9705064
18. Banerjee R, Strahilevitz J, Johnson JR, et al. Predictors and molecular epidemiology of community-onset extended-spectrum β-lactamase-producing Escherichia coli infection in a Midwestern community. Infect Control Hosp Epidemiol. 2013;34(9):947–953. doi:10.1086/671725
19. Pitout JD. Enterobacteriaceae that produce extended-spectrum β-lactamases and AmpC β-lactamases in the community: the tip of the iceberg? Curr Pharm Des. 2013;19(2):257–263. doi:10.2174/1381612811306020257
20. Doi Y, Park YS, Rivera JI, et al. Community-associated extended-spectrum β-lactamase-producing Escherichia coli infection in the United States. Clin Infect Dis. 2013;56(5):641–648. doi:10.1093/cid/cis942
21. van Duin D, Paterson DL. Multidrug-resistant bacteria in the community: trends and lessons learned. Infect Dis Clin North Am. 2016;30(2):377–390. doi:10.1016/j.idc.2016.02.004
22. Vardakas KZ, Rafailidis PI, Konstantelias AA, Falagas ME. Predictors of mortality in patients with infections due to multi-drug resistant Gram negative bacteria: the study, the patient, the bug or the drug? J Infect. 2013;66(5):401–414. doi:10.1016/j.jinf.2012.10.028
23. Bodi M, Ardanuy C, Rello J. Impact of Gram-positive resistance on outcome of nosocomial pneumonia. Crit Care Med. 2001;29(4 Suppl):N82–N86. doi:10.1097/00003246-200104001-00005
24. Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315(8):801–810. doi:10.1001/jama.2016.0287
25. European Committee on Antimicrobial Susceptibility Testing (EUCAST). Breakpoint tables for interpretation of MICs and zone diameters. Version 9.0. Basel: EUCAST; 2003.
26. Magiorakos AP, Srinivasan A, Carey RB, et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: an international expert proposal for interim standard definitions for acquired resistance. Clin Microbiol Infect. 2012;18(3):268–281. doi:10.1111/j.1469-0691.2011.03570.x
27. Heinze G, Wallisch C, Dunkler D. Variable selection - A review and recommendations for the practicing statistician. Biom J. 2018;60(3):431–449. doi:10.1002/bimj.201700067
28. VanderWeele TJ, Ding P. Sensitivity analysis in observational research: introducing the E-value. Ann Intern Med. 2017;167(4):268–274. doi:10.7326/M16-2607
29. Mathur MB, Ding P, Riddell CA, VanderWeele TJ. Web site and R package for computing E-values. Epidemiology. 2018;29(5):e45–e47. doi:10.1097/EDE.0000000000000864
30. Vazquez-Guillamet C, Scolari M, Zilberberg MD, Shorr AF, Micek ST, Kollef M. Using the number needed to treat to assess appropriate antimicrobial therapy as a determinant of outcome in severe sepsis and septic shock. Crit Care Med. 2014;42(11):2342–2349. doi:10.1097/CCM.0000000000000516
31. Trecarichi EM, Cauda R, Tumbarello M. Detecting risk and predicting patient mortality in patients with extended-spectrum β-lactamase-producing Enterobacteriaceae bloodstream infections. Future Microbiol. 2012;7(10):1173–1189. doi:10.2217/fmb.12.100
32. Cosgrove SE. The relationship between antimicrobial resistance and patient outcomes: mortality, length of hospital stay, and health care costs. Clin Infect Dis. 2006;42(Suppl 2):S82–9. doi:10.1086/499406
33. Blot S, Vandewoude K, De Bacquer D, Colardyn F. Nosocomial bacteremia caused by antibiotic-resistant gram-negative bacteria in critically ill patients: clinical outcome and length of hospitalization. Clin Infect Dis. 2002;34(12):1600–1606. doi:10.1086/340616
34. Oxman D, Lohr K, Gupta E, Madara J, Len E, Hseih J. Incidence of multidrug resistant infections in emergency department patients with suspected sepsis. Am J Med Sci. 2020;360(6):650–655. doi:10.1016/j.amjms.2020.07.019
35. Faine BA, Harland KK, Porter B, Liang SY, Mohr N. A clinical decision rule identifies risk factors associated with antimicrobial-resistant urinary pathogens in the emergency department: a retrospective validation study. Ann Pharmacother. 2015;49(6):649–655. doi:10.1177/1060028015578259
36. Angus DC, van der Poll T. Severe sepsis and septic shock. N Engl J Med. 2013;369(9):840–851. doi:10.1056/NEJMra1208623
37. Mayr FB, Yende S, Angus DC. Epidemiology of severe sepsis. Virulence. 2014;5(1):4–11. doi:10.4161/viru.27372
38. Aliberti S, Di Pasquale M, Zanaboni AM, et al. Stratifying risk factors for multidrug-resistant pathogens in hospitalized patients coming from the community with pneumonia. Clin Infect Dis. 2012;54(4):470–478. doi:10.1093/cid/cir840
39. Vincent JL, Rello J, Marshall J, et al. International study of the prevalence and outcomes of infection in intensive care units. JAMA. 2009;302(21):2323–2329. doi:10.1001/jama.2009.1754
40. Luzzaro F, Ortisi G, Larosa M, Drago M, Brigante G, Gesu G. Prevalence and epidemiology of microbial pathogens causing bloodstream infections: results of the OASIS multicenter study. Diagn Microbiol Infect Dis. 2011;69(4):363–369. doi:10.1016/j.diagmicrobio.2010.10.016
41. Rodríguez-Baño J, López-Prieto MD, Portillo MM, et al. Epidemiology and clinical features of community-acquired, healthcare-associated and nosocomial bloodstream infections in tertiary-care and community hospitals. Clin Microbiol Infect. 2010;16(9):1408–1413. doi:10.1111/j.1469-0691.2009.03089.x
42. Kollef MH, Zilberberg MD, Shorr AF, et al. Epidemiology, microbiology and outcomes of healthcare-associated and community-acquired bacteremia: a multicenter cohort study. J Infect. 2011;62(2):130–135. doi:10.1016/j.jinf.2010.12.009
43. Fraimow HS, Tsigrelis C. Antimicrobial resistance in the intensive care unit: mechanisms, epidemiology, and management of specific resistant pathogens. Crit Care Clin. 2011;27(1):163–205. doi:10.1016/j.ccc.2010.11.002
44. Ramphal R, Ambrose PG. Extended-spectrum beta-lactamases and clinical outcomes: current data. Clin Infect Dis. 2006;42(Suppl 4):S164–S172. doi:10.1086/500663
45. Mehrad B, Clark NM, Zhanel GG, Lynch JP. Antimicrobial resistance in hospital-acquired gram-negative bacterial infections. Chest. 2015;147(5):1413–1421. doi:10.1378/chest.14-2171
46. Hussain A, Ranjan A, Nandanwar N, Babbar A, Jadhav S, Ahmed N. Genotypic and phenotypic profiles of Escherichia coli isolates belonging to clinical sequence type 131 (ST131), clinical non-ST131, and fecal non-ST131 lineages from India. Antimicrob Agents Chemother. 2014;58(12):7240–7249. doi:10.1128/AAC.03320-14
47. Pannaraj PS, Bard JD, Cerini C, Weissman SJ. Pediatric carbapenem-resistant enterobacteriaceae in los angeles, California, a high-prevalence region in the United States. Pediatr Infect Dis J. 2015;34(1):11–16. doi:10.1097/INF.0000000000000471
48. Peirano G, Schreckenberger PC, Pitout JD. Characteristics of NDM-1-producing Escherichia coli isolates that belong to the successful and virulent clone ST131. Antimicrob Agents Chemother. 2011;55(6):2986–2988. doi:10.1128/AAC.01763-10
49. Sibila O, Rodrigo-Troyano A, Shindo Y, Aliberti S, Restrepo MI. Multidrug-resistant pathogens in patients with pneumonia coming from the community. Curr Opin Pulm Med. 2016;22(3):219–226. doi:10.1097/MCP.0000000000000263
50. Shindo Y, Ito R, Kobayashi D, et al. Risk factors for drug-resistant pathogens in community-acquired and healthcare-associated pneumonia. Am J Respir Crit Care Med. 2013;188(8):985–995. doi:10.1164/rccm.201301-0079OC
51. Gross AE, Van Schooneveld TC, Olsen KM, et al. Epidemiology and predictors of multidrug-resistant community-acquired and health care-associated pneumonia. Antimicrob Agents Chemother. 2014;58(9):5262–5268. doi:10.1128/AAC.02582-14
52. Quintano Neira RA, Hamacher S, Japiassú AM. Epidemiology of sepsis in Brazil: incidence, lethality, costs, and other indicators for Brazilian unified health system hospitalizations from 2006 to 2015. PLoS One. 2018;13(4):e0195873. doi:10.1371/journal.pone.0195873
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


