Back to Journals » Cancer Management and Research » Volume 14
Real-World Clinical and Patient-Reported Outcomes from the Longitudinal Telotristat Ethyl Treatment Registry of Patients with Neuroendocrine Tumors
Authors Li D , Darden C, Osman N, Sayeed S, Jackson L, Garbinsky D, Chauhan A
Received 16 August 2022
Accepted for publication 7 October 2022
Published 17 October 2022 Volume 2022:14 Pages 3009—3020
DOI https://doi.org/10.2147/CMAR.S386419
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Kattesh Katti
Daneng Li,1 Christina Darden,2 Noran Osman,3 Salma Sayeed,3 Laurin Jackson,2 Diana Garbinsky,2 Aman Chauhan4
1City of Hope Comprehensive Cancer Center and Beckman Research Institute, Duarte, CA, USA; 2RTI Health Solutions, Research Triangle Park, NC, USA; 3TerSera Therapeutics, Deerfield, IL, USA; 4Markey Cancer Center, University of Kentucky, Lexington, KY, USA
Correspondence: Daneng Li, Department of Medical Oncology & Therapeutics Research, City of Hope, 1500 E. Duarte Road, Duarte, CA, 91010, USA, Tel +626-471-9200, Fax +626-301-8233, Email [email protected]
Background: Telotristat ethyl (TE) is an oral tryptophan hydroxylase inhibitor approved for the treatment of carcinoid syndrome diarrhea (CSD) in combination with somatostatin analogs (SSAs).
Methods: This prospective, observational, single-arm study evaluated long-term patient-reported outcomes for adults initiating TE in US clinical practice from 2017 through January 2022. The primary objective was satisfaction with overall CS symptom control 6 months after initiating TE. Secondary objectives evaluated satisfaction with control of CSD, flushing, and CS symptoms, as well as work productivity/activity impairment, SSA use, and weight. All analyses were descriptive in nature.
Results: A total of 223 patients completed the baseline survey; 56% also completed the 6-month follow-up survey. Mean age was 61 years and 61% were women. After 6 months of TE treatment, the majority of patients (76%, n=95/125) reported being satisfied with control of their CS symptoms which was markedly improved from baseline (41%, n=91). Similarly, the majority of patients (78%, n=97/125) were satisfied with control of their CSD after 6 months of TE, markedly improved from baseline (36%).
Conclusion: This longitudinal observational study showed improvements in real-world clinical and humanistic outcomes for patients with CS and at least 6 months of TE treatment.
Keywords: neuroendocrine tumors, gastrointestinal neoplasms, medical management, carcinoid syndrome, telotristat ethyl, work productivity, healthcare resource use
Plain Language Summary
This study evaluated patient-reported outcomes for adults initiating telotristat ethyl (TE) for carcinoid syndrome diarrhea (CSD) not adequately controlled by somatostatin analogs in US clinical practice from 2017 through January 2022. The primary objective was satisfaction with overall CS symptom control 6 months after starting TE. Secondary objectives evaluated satisfaction with control of CSD and flushing, CS symptoms, work productivity and activity impairment, SSA use, and weight. After 6 months of TE treatment, the majority of patients (76%) reported being satisfied with control of their CS symptoms which was markedly improved from baseline (41%). Similarly, the majority of patients (78%) were satisfied with control of their CSD after 6 months of TE, markedly improved from baseline (36%). The majority of patients (73%) reported gaining or maintaining their weight after 6 months of TE treatment. These data provide real-world patient-reported improvement in CS with TE treatment for at least 6 months.
Introduction
Carcinoid syndrome (CS) is caused by the overproduction of several hormones and vasoactive compounds from well-differentiated secretory neuroendocrine tumors (NETs), where serotonin plays a key role, and is associated with flushing, carcinoid syndrome diarrhea (CSD), and wheezing.1–3 Approximately 20% to 35% of patients with NETs have CS,4,5 which has a substantial negative impact on health-related quality of life (HRQoL) and patient-reported reductions in energy (71%), personal finances (59%), and emotional health (58%).6,7
Treatment goals for patients with NETs and CS are to slow tumor growth and address CS symptoms. Somatostatin analogs (SSAs) are first-line standard of care for medical management and have antiproliferative effects.8–10 Approximately 60% of patients receiving SSAs are expected to have a clinical response, though refractory symptoms often occur with a loss of treatment effect over time.11–14 Hepatic arterial embolization and peptide receptor radiotherapy are recommended with radiographic progression, but not for patients with worsening symptoms in the context of otherwise stable disease.15
Telotristat ethyl (TE; Xermelo®; TerSera Therapeutics, Deerfield, IL, USA) is an oral tryptophan hydroxylase inhibitor that was developed to help improve CSD and CS symptoms for patients unresponsive to SSAs alone or whose clinical response to SSAs may wane over time. TE mediates the rate limiting step in serotonin biosynthesis, reducing the production of peripheral serotonin and, in turn, CSD.16–18 TE is approved for the treatment of CSD in combination with SSAs for adults not adequately controlled by SSAs alone.18 The efficacy and safety of TE has been demonstrated in Phase 3 clinical trials16,17 and in the real-world TELEPRO-I and TELEPRO-II studies of patients receiving TE in US clinical practice.19,20 Interim analyses from the ongoing RELAX registry (Real-world Evidence Study Evaluating Patient-Reported Outcomes With XERMELO; NCT03223428) have reported high patient satisfaction with control of CS symptoms and CSD among patients receiving TE in clinical practice.21,22 This paper reports final results from completed follow-up of all patients receiving TE in the RELAX study from 2017 through January 2022.
Materials and Methods
Study Design and Participants
The RELAX study was a prospective, observational, single-arm study of adults (≥ 18 years old) receiving TE in US clinical practice. Participation was offered to patients initiating TE by specialty pharmacy providers or nurse educators during prescription onboarding and follow-up phone calls. Patients who were not able to access the internet, understand and communicate in English, or who had prior exposure to TE were excluded. Patients who agreed to participate were referred to the study team (RTI Health Solutions, Research Triangle Park, NC, USA) for enrollment and completion of the baseline survey and follow-up surveys every 6 months for up to 3 years or study completion. A participant was considered lost to follow-up if the study team was unable to reach the participant after 3 attempts and the participant did not complete the follow-up survey within a prespecified window. When a change in the participant’s status was communicated to the study team (ie, withdrawal of consent or treatment discontinuation), the patient’s unique study link was disabled and no further survey invitations or reminders were sent. Participation in the study was voluntary however a modest monetary reward was granted to participants for their time and effort. Participants received a modest monetary reward after completion of each survey.
This study was conducted in compliance with the principles of the Declaration of Helsinki, and all participants provided informed consent via checkbox prior to initiating the survey. The study protocol, materials, amendments, and annual renewals were approved by the RTI Institutional Review Board (Federal-Wide Assurance #3331; www.rti.org).
Objectives and Outcomes
The primary objective was to estimate the proportion of patients with CS who were satisfied with control of their overall CS symptoms 6 months after initiating TE treatment. Secondary and exploratory objectives evaluated satisfaction with control of CSD and flushing, number of bowel movements, Patient Global Impression of Change (PGIC) related to CS symptoms, and changes in work productivity and activity impairment at 6 months. Patient-reported changes in SSA use and healthcare resource use were evaluated at baseline and all 6-month follow-up timepoints. Patient-reported changes in weight “since starting TE” were evaluated at each 6-month timepoint. The questionnaires used to evaluate patient satisfaction and clinical aspects of their CS-related care were based on those used in exit interviews conducted with a subsample of patients (n=35) in 5 countries who completed the treatment portion of the TELESTAR trial.6 The CS-specific questionnaire items were developed by the study team to address the specific objectives of this study, which were not covered by a pre-existing questionnaire.
At baseline, patients were asked to report their level of satisfaction with control of their CS symptoms (“Currently, how satisfied are you with how your carcinoid syndrome/diarrhea/flushing is controlled?”). Follow-up questions asked patients to indicate their satisfaction with TE control of CS symptoms (“Overall, how satisfied are you with how Xermelo [TE] has controlled your carcinoid syndrome symptoms/diarrhea/flushing?”). Patients reported satisfaction with control of CS symptoms, CSD and flushing on a 5-point Likert scale where 1 indicated “very dissatisfied” and 5 indicated “very satisfied”; a response of 0 for “not applicable” was available those who did not have CSD or flushing. The PGIC recorded patients’ perceptions of changes in their CS symptoms on a 7-point Likert scale from “very much worse” (coded as 1 point) to “very much improved” (coded as 7 points). Patients reported changes in the frequency of bowel movements on a 7-point Likert scale from “a great deal worse” (coded as 1 point) to “a great deal better” (coded as 7 points).
At each 6-month follow-up survey, patients were asked to qualitatively assess their weight change since initiating TE using one of four response options (“I weigh less”, “I weigh about the same”, “I weigh more” and “I don’t know”). Patients indicated short-acting rescue SSA therapy use as “less frequent”, “about the same” or “more frequent” through 36 months. Dosing and frequency of long-acting SSAs among those receiving them were also captured as “less frequent”, “stayed the same” or “increased.”
Work productivity and activity impairment was evaluated using the Work Productivity and Activity Impairment–Specific Health Problem (WPAI-SHP) questionnaire (Reilly Associates; www.reillyassociates.net). The WPAI-SHP is a self-administered questionnaire comprising six questions measuring the effect of specific health problems on individuals’ ability to work and participate in regular activities based on their experiences in the previous 7 days. Work-related impairments were only assessed among employed participants: absenteeism (proportion of work time missed in the previous 7 days due to CS), presenteeism (impaired productivity while at work due to CS), and overall work productivity loss due to CS (expressed as a percentage). Presenteeism was captured on a 0–10-point scale where 0 indicated “CS had no effect on my work” and 10 indicated “CS completely prevented me from working”. Activity impairment was assessed for all participants as the percentage of impairment in daily activities due to CS according to a 0–10-point scale where 0 indicated “CS had no effect on my daily activities” and 10 indicated “CS completely prevented me from doing my daily activities”. For all WPAI-SHP items, higher mean scores indicate a greater level of impairment.
Healthcare resource use was evaluated at baseline and each 6-month follow-up timepoint, where patients were asked about Emergency Department (ED) visits and hospitalizations during the previous 6 months. Patients were asked about the number of CS-related ED visits and hospitalizations, the number of nights per CS-related hospital stay, and the specific reason for their CS-related ED visit or hospital stay (such as the symptom[s] that lead to visiting the ED or hospital).
Statistical Analysis
All analyses were descriptive in nature and included measures of central tendency, frequencies, and proportions. Missing values and “prefer not to answer” responses were not included in the denominator when computing proportions. Exploratory analyses were conducted among patients with both baseline and follow-up responses for the primary and secondary objectives related to changes in CS symptoms. All analyses were conducted in SAS version 9.4 (SAS Institute, Cary, NC, USA).
Results
Patients
A total of 349 patients initiating TE were invited to participate in the RELAX study, of whom 223 (64%) were enrolled and completed the baseline survey (Figure 1). Approximately half of those completing a baseline survey also completed the 6-month follow-up survey (n=125/223; 56%). Completion rates from one follow-up visit to the next were generally >60%. At baseline, the mean age was 61 years (median, 61 years; range, 19–87), and 38% of patients were aged 65 years or older (n=84/222). More than half of patients were women (61%), and the mean weight was 80.9 kg (178.4 lb.; Table 1). The majority of patients had completed high school or equivalent (26%) or a higher level of education (73%) and self-identified as White (85%). Most patients had their primary NET of the small intestine (64%), and the mean time from CS diagnosis to baseline (initiation of TE) was 5.6 years (Table 1). Nearly all patients were receiving monthly SSA therapy (96%), and most (73%) had not received additional treatments for their CS in the previous 6 months (not counting short-acting SSAs).
 |
Table 1 Baseline Demographic and Clinical Characteristics (n = 223) |
 |
Figure 1 Patient attrition and survey completion. Discontinued patients were not invited to complete the survey. Abbreviation: TE, telotristat ethyl. |
Satisfaction and Changes Related to Control of CS Symptoms
At baseline, before initiating TE, 41% of patients (n=91/223) reported satisfaction with control of their CS symptoms. Among patients who completed the 6-month follow-up survey, 76% (n=95/125; 95% CI: 68.5%, 83.5%) were satisfied with TE control of their CS symptoms (Figure 2). However, since all patients completing the baseline survey did not also complete a 6-month follow-up survey, an exploratory analysis was conducted among 125 patients who completed both baseline and Month 6 responses. This analysis showed similar findings as the primary analysis, where 46% (n=58/125) and 76% (n=95/125) reported satisfaction with control of their overall CS symptoms before and after initiating TE, respectively.
 |
Figure 2 Patient satisfaction with control of CS symptoms. |
Based on responses to the PGIC, most patients (78%, n=97/125) reported improvement in CS symptoms after 6 months of TE treatment. Only 8 patients (6%) reported worsened CS symptoms, and 20 patients (16%) reported no change (Supplementary Figure S1).
Satisfaction and Changes Related to Control of CSD and Flushing
Approximately one-third of patients reported satisfaction with control of their CSD at baseline (36%; n=80/221), and 78% (n=97/125) reported satisfaction with control of CSD after 6 months of TE (Figure 3A). An exploratory analysis was conducted among patients who provided both baseline and Month 6 responses, where 46% (n=57/125) and 78% (n=97/125) reported satisfaction with control of their CSD before and after initiating TE, respectively. The majority of patients reported improvement in the number of bowel movements (fewer) after 6 months of TE (82%; n=103/125) (Figure 3B).
Approximately half of the patients who reported experiencing flushing were satisfied with control of their flushing symptoms at baseline (49%; n=94/193). After 6 months, 58% (n=63/108) reported satisfaction with TE control of their flushing (Figure 3C). Among those with flushing and both baseline and Month 6 responses, 53% (n=56/105) and 58% (n=63/108) reported satisfaction with control of their flushing before and after initiating TE, respectively.
Patient-Reported Weight Change or Maintenance
After 6 months of TE treatment, 24 of the 125 patients (19%) responding to the 6-month follow-up survey reported weighing more since initiating TE, and half (54%, n=67) reported weighing about the same. Taken together, weight gain or maintenance was reported by 73% (n=91) of patients after 6 months of TE, which remained generally consistent through 30 months of follow-up (Figure 4). Among the 17 patients with 36-month responses, a slightly lower proportion reported weighing the same or more (59%, n=10) compared with earlier timepoints.
 |
Figure 4 Patient-reported weight gain/maintenance or loss. Note: Two patients reported “I do not know” regarding weight change at Month 12. |
Patient-Reported Use of SSAs and Other Treatments
The proportion of patients receiving long-acting SSAs remained generally stable from baseline (96%) through 6 months (94%) and 36 months (100%), consistent with the approved use of TE in addition to an SSA (Supplementary Figure S2A). Similarly, nearly all patients reported consistent dosing and frequency of long-acting SSAs over time (Supplementary Figure S3).
Some patients reported using less short-acting rescue SSA therapy after initiating TE through 24 months (Supplementary Figure S2B). Among those who reported receiving short-acting rescue SSA treatment, the majority reported the same or less frequent use at 6 months (94%) which remained consistent over time (Figure 5). Few patients reported receiving additional treatments for CS during the study period; 11–14% received chemotherapy, 0–14% received radionuclide therapy, and 0–12% received radiation.
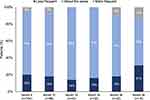 |
Figure 5 Patient-reported change in short-acting rescue SSA medication use. Abbreviation: SSA, somatostatin analog. |
Work Productivity and Activity Impairment
Consistent with the age distribution of the study population (38% were ≥65 years at baseline), most patients were not employed (66% at baseline, 72% at Month 6). The 75 patients who were employed at baseline reported missing an average of 3.8 hours (SD, 6.98) of work over the previous 7 days due to problems associated with their CS, which decreased to 2.4 hours (4.71) among the 35 patients who reported employment at Month 6. Absenteeism was essentially unchanged from baseline to Month 6, from an average of 10.3% (17.82) to 10.4% (24.48) time missed from work due to CS over the previous 7 days. Employed patients reported a decreased impact of CS on their productivity while working, from an average of 4.2/10 (2.48) at baseline (n=70) to 3.0/10 (2.32) at Month 6 (n=32). The proportion of work time impaired by CS (presenteeism) decreased from 42.1% (24.78) at baseline to 29.7% (23.21) at Month 6. Overall, employed patients reported a mean of 45.3% (27.03) overall work productivity loss at baseline and 31.6% (24.21) at Month 6.
Regardless of employment, when asked to indicate the degree to which CS affected their ability to perform regular activities, patients reported a mean of 5.6/10 (2.61) at baseline and 4.5/10 (2.73) at Month 6. Employed patients reported an overall mean of 56% (26.07) activity impairment at baseline, and 45% (27.27) at Month 6.
Healthcare Resource Use
At baseline, 16% (n=36/223) of patients reported ≥1 CS-related ED visit in the previous 6 months, most often for abdominal pain (65%), dehydration (56%), exhaustion (47%), diarrhea (39%) and/or vomiting (35%). After 6 months of TE, 12% of patients (n=15/124) reported a CS-related ED visit in the previous 6 months (mean [SD], 0.3 [0.88]), most often for abdominal pain (63%) and/or dehydration (41%). Most patients receiving TE had not reported a CS-related ED visit at Month 6 (88%) or by Month 36 (66%).
Before initiating TE, 24% of patients (n=53/222) reported ≥1 CS-related hospitalization in the previous 6 months for a mean (SD) of 7.4 (8.71) nights, most often for abdominal pain (51%), dehydration (49%), diarrhea (43%), vomiting (36%), another unspecified CS-related reason (34%), and/or flushing (32%). After 6 months of TE, 12% (n=15/124) reported ≥1 CS-related hospitalization in the previous 6 months for a mean of 5.9 (6.78) nights, most often for abdominal pain (35%), diarrhea (20%) and/or flushing (5%). As with ED visits, most patients receiving TE had not reported a CS-related hospitalization at Month 6 (88%) or by Month 36 (69%). Similarly, most patients had not reported either a CS-related ED visit or a CS-related hospitalization by Month 6 (82%) or by Month 36 (60%). The proportions of patients reporting ≥1 ED visit and/or ≥1 hospitalization during the study period are presented in Supplementary Figure S4.
Discussion
This real-world study provided longitudinal patient-reported outcomes related to changes in CS symptoms, SSA use, and work productivity/activity impairment for patients with CS initiating TE in US clinical practice. Patients reported greater satisfaction with control of their CS symptoms after 6 months of TE treatment as compared to baseline symptoms following long-acting SSA treatment only. The majority of patients reported improvement in the number of bowel movements, which was consistent with findings from patient interviews following the TELESTAR clinical trial.6 Most patients also reported maintaining or gaining weight (73%), an important surrogate marker for overall health in patients with CS and CSD. While use of long-acting SSAs remained generally stable for nearly all patients over the 3-year study period, the frequency of short-acting rescue SSA therapy use decreased substantially during the first 12 to 24 months of TE treatment, from 21% to 17% and 8%, respectively.
These findings further support prior reports of improved control of CS symptoms and CSD with TE treatment. The real-world TELEPRO (2019) and TELEPRO-II (2021) studies reported a high baseline burden of CSD and CS symptoms for patients receiving SSAs only, and substantial improvements in patient-reported experience and outcomes after 3 months of TE in US clinical practice.19,20 TELEPRO-II showed significant improvements in overall CS symptoms, daily bowel movement frequency, stool consistency, nausea, abdominal pain, urgency, and flushing as early as 1 month through 3 months of TE treatment.20 After 3 months of TE, approximately half (52%) of patients in the TELEPRO study reported a reduction of ≥2 bowel movements per day.19 The majority of patients in the RELAX study reported less frequent bowel movements (82%) after 6 months of TE, underscoring the importance of continued follow-up and treatment adherence.
This study should be interpreted in the context of certain strengths and limitations. The observational nature of this patient registry provided external validity for extrapolation of findings to patients with NETs and CS receiving TE in US clinical practice. The specialty pharmacy providers managing enrollment were the sole distributers of TE on study initiation. Since patients were offered to participate as they were initiating treatment, the study population is likely to be largely representative of patients receiving TE in practice. Although a physician-confirmed diagnosis of CS was not directly recorded, study participants had to have a new, valid TE prescription filled by the specialty pharmacy. In this way, a CS diagnosis was indirectly confirmed since TE was only approved for the treatment of patients with CSD. As with all voluntary survey studies, there was potential for responder bias. All findings were self-reported by patients without confirmation against medical records or insurance claims, which may have introduced a reporting bias. The attrition rate was 36% from the time patients expressed interest/verbal agreement to participate and completion of the baseline survey, where unobserved differences may have been present between those who did and did not complete the baseline survey. All study materials were internet-based; although internet-based surveys are a universally accepted method of participation, some patients may have been unable to participate due to a lack or unwilling use of internet access. Finally, decreasing sample sizes of patients responding to the surveys presented challenges to interpretation of findings after approximately 24–30 months, and the small sample size and patient-reported nature of healthcare resource use suggests that these findings should be interpreted with caution.
Conclusions
This longitudinal observational study showed improvements in real-world clinical and humanistic outcomes for patients with CS and at least 6 months of TE treatment. Patients reported improved experience of overall CS symptom control and reduced bowel movements in particular, and reduced impact of CS on their weight, need for rescue SSA therapy, and work productivity and activity impairment. These real-world outcomes are consistent with findings from clinical trials and shorter observational studies, providing evidence of real-world patient-reported improvements in CSD and CS symptoms with TE treatment for at least 6 months, while improving measures of health and wellness for patients with CS and inadequate responsiveness to SSA monotherapy.
Data Sharing Statement
The data presented in this study may be available on request from the corresponding author. The data are not publicly available.
Institutional Review Board Statement
This study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the RTI Institutional Review Board (Federal-Wide Assurance #3331; www.rti.org).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Acknowledgments
This study was sponsored by TerSera Therapeutics. The authors received medical writing/editorial support from Jeff Frimpter, MPH, funded by TerSera Therapeutics.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research was funded by TerSera Therapeutics.
Disclosure
D.L. reports research funding to his institution from AstraZeneca and Brooklyn ImmunoTherapeutics. He serves as a consultant and has received honoraria from Adagene, Advanced Accelerator Applications, Coherus BioSciences, Eisai, Exelixis, Genentech, Ipsen Biopharmaceuticals, Lexicon Pharmaceuticals, Merck, MiNA Therapeutics, QED Therapeutics, Servier, Sun Pharma, TerSera Therapeutics, and Delcath. A.C. reports research support from Bristol Myers Squibb, Clovis, Nanotherapeutics, TerSera Therapeutics, Lexicon Pharmaceuticals, and ECS Progastrin. He has served as an advisor to TerSera Therapeutics, Lexicon Pharmaceuticals, Novartis, Ipsen, and Crinetics. C.D., L.J. and D.G. are employees of RTI Health Solutions which received research funding for this study from TerSera Therapeutics. S.S., J.C., and N.O. are employees and shareholders of TerSera Therapeutics. The authors report no other conflicts of interest in this work.
References
1. Gustafsson BI, Hauso O, Drozdov I, Kidd M, Modlin M. Carcinoid heart disease. Int J Cardiol. 2008;129(3):318–324. doi:10.1016/j.ijcard.2008.02.019
2. Zuetenhorst JM, Bonfrer JMGM, Korse CM, Bakker R, van Tinteren Taal BG. Carcinoid heart disease: the role of urinary 5-hydroxyindoleacetic acid excretion and plasma levels of atrial natriuretic peptide, transforming growth factor-Beta and fibroblast growth factor. Cancer. 2003;97(7):1609–1615. doi:10.1002/cncr.11226
3. Pandit S, Bhusal K. Carcinoid Syndrome. Treasure Island, FL: StatPearls Publishing; 2017. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448096/.
4. Dasari A, Shen C, Halperin D, et al. Trends in the incidence, prevalence, and survival outcome in patients with neuroendocrine tumors in the United States. JAMA Oncol. 2017;3(10):1335–1342. doi:10.1001/jamaoncol.2017.0589
5. Halperin DM, Shen C, Dasari A, et al. Frequency of carcinoid syndrome at neuroendocrine tumour diagnosis: a population-based study. Lancet Oncol. 2017;18(4):525–534. doi:10.1016/S1470-2045(17)30110-9
6. Anthony L, Ervin C, Lapuerta P, et al. Understanding the patient experience with carcinoid syndrome: exit interviews from a randomized, placebo-controlled study of telotristat ethyl. Clin Ther. 2017;39(11):2158–2168. doi:10.1016/j.clinthera.2017.09.013
7. Wolin EM. The expanding role of somatostatin analogs in the management of neuroendocrine tumors. Gastrointest Cancer Res. 2012;5(5):161–168.
8. Rinke A, Müller HH, Schade-Brittinger C, et al. Placebo-controlled, double-blind, prospective, randomized study on the effect of octreotide LAR in the control of tumor growth in patients with metastatic neuroendocrine midgut tumors: a report from the PROMID Study Group. J Clin Oncol. 2009;27:4656–4663. doi:10.1200/JCO.2009.22.8510
9. Caplin ME, Pavel M, Ruszniewski P. Lanreotide in metastatic enteropancreatic neuroendocrine tumors. N Engl J Med. 2014;371:1556–1557. doi:10.1056/NEJMoa1316158
10. Barrows SM, Cai B, Copley-Merriman C, et al. Systematic literature review of the antitumor effect of octreotide in neuroendocrine tumors. World J Meta Anal. 2018;6(2):9–20. doi:10.13105/wjma.v6.i2.9
11. Toumpanakis C, Garland J, Marelli L, et al. Long-term results of patients with malignant carcinoid syndrome receiving octreotide LAR. Aliment Pharmacol Ther. 2009;30:733–740. doi:10.1111/j.1365-2036.2009.04083.x
12. Ferrari ACR, Glasberg J, Riechelmann RP. Carcinoid syndrome: update on the pathophysiology and treatment. Clinics. 2018;73(suppl 1):e490s. doi:10.6061/clinics/2018/e490s
13. Riechelmann RP, Pereira AA, Rego JFM, Costa FP. Refractory carcinoid syndrome: a review of treatment options. Ther Adv Med Oncol. 2017;9(2):127–137. doi:10.1177/1758834016675803
14. Burton T, Lapuerta P. Economic analysis of inadequate symptom control in carcinoid syndrome in the United States. Future Oncol. 2018;14(23):2361–2370. doi:10.2217/fon-2018-0129
15. Kunz PL, Reidy-Lagunes D, Anthony LB, et al. Consensus guidelines for the management and treatment of neuroendocrine tumors. Pancreas. 2013;42(4):557–577. doi:10.1097/MPA.0b013e31828e34a4
16. Pavel M, Gross DJ, Benavent M, et al. Telotristat ethyl in carcinoid syndrome: safety and efficacy in the TELECAST phase 3 trial. Endocr Rel Cancer. 2018;25:309–322. doi:10.1530/ERC-17-0455
17. Kulke MH, Hörsch D, Caplin ME, et al. Telotristat ethyl, a tryptophan hydroxylase inhibitor for the treatment of carcinoid syndrome. J Clin Oncol. 2017;35:14–23. doi:10.1200/JCO.2016.69.2780
18. XERMELO® (telotristat ethyl) [prescribing information]. Deerfield, IL: TerSera Therapeutics; 2020.
19. Strosberg J, Joish VN, Giacalone S, et al. TELEPRO: patient-reported carcinoid syndrome symptom improvement following initiation of telotristat ethyl in the real world. Oncologist. 2019;24:1–7. doi:10.1634/theoncologist.2018-0921
20. Kulke MH, Kennecke HF, Murali K, Joish VN. Changes in carcinoid syndrome symptoms among patients receiving telotristat ethyl in US clinical practice: findings from the TELEPRO-II real-world study. Cancer Manag Res. 2021;13:7439–7446. doi:10.2147/CMAR.S330429
21. Li D, Darden C, Sayeed S, et al. Patient-reported clinical and productivity outcomes from the longitudinal telotristat ethyl treatment registry (98).
22. Darden C, Joish VN, Price MA, et al. Patient-reported activity impairment, work productivity loss, and carcinoid syndrome outcomes: interim analyses of the RELAX patient registry (113).
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

