Back to Journals » Clinical Interventions in Aging » Volume 17
Preoperative Risk Factor Analysis and Dynamic Online Nomogram Development for Early Infections Following Primary Hip Arthroplasty in Geriatric Patients with Hip Fracture
Authors Cheng X, Liu Y, Wang W, Yan J, Lei X, Wu H, Zhang Y, Zhu Y
Received 5 October 2022
Accepted for publication 13 December 2022
Published 21 December 2022 Volume 2022:17 Pages 1873—1883
DOI https://doi.org/10.2147/CIA.S392393
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Maddalena Illario
Xinqun Cheng,1,2,* Yan Liu,3,* Weitong Wang,4 Jincheng Yan,1 Xiang Lei,1 Haifeng Wu,1 Yingze Zhang,1,2 Yanbin Zhu1,2
1Department of Orthopedic Surgery, the 3rd Hospital of Hebei Medical University, Shijiazhuang, Hebei, 050051, People’s Republic of China; 2Hebei Orthopedic Research Institute, Key Laboratory of Biomechanics of Hebei Province, Shijiazhuang, Hebei, 050051, People’s Republic of China; 3Cheeloo College of Medicine, Qilu Hospital of Shandong University, Jinan, Shandong, 250012, People’s Republic of China; 4Department of Marketing and International Business, Lingnan University, Hong Kong, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yingze Zhang; Yanbin Zhu, Hebei Bone Research Institute, Key Laboratory of Biomechanics of Hebei Province, Shijiazhuang, Hebei, 050051, People’s Republic of China, Email [email protected]; [email protected]
Background: Hip arthroplasty is in increasing demand with the aging of the world population, and early infections, such as pneumonia, surgical site infection (SSI), and urinary tract infection (UTI), are uncommon but fatal complications following hip arthroplasty. This study aimed to identify preoperative risk factors independently associated with early infections following primary arthroplasty in geriatric hip fracture patients, and to develop a prediction nomogram.
Methods: Univariate and multivariate logistical analyses were performed to identify the independent risk factors for early infections, which were combined and transformed into a nomogram model. The prediction model was evaluated by using the area under the receiver operating characteristic curve (AUC), Hosmer–Lemeshow test, concordance index (C-index), 1000 bootstrap replications, decision curve analysis (DCA), and calibration curve.
Results: One thousand eighty-four eligible patients got included and 7 preoperative variables were identified to be independently associated with early infections, including heart disease (odds ratio (OR): 2.17; P: 0.026), cerebrovascular disease (OR: 2.25; P: 0.019), liver disease (OR: 8.99; P: < 0.001), time to surgery (OR: 1.10; P: 0.012), hematocrit (
Conclusion: Heart disease, cerebrovascular disease, liver disease, time to surgery, hematocrit, PMR, and HCRP were significant preoperative predictors for early infections following primary arthroplasty in elderly hip fracture patients, and the converted nomogram model had strong discriminatory ability and translatability to clinical application.
Keywords: early infections, arthroplasty, hip fracture, geriatric, nomogram
Hip arthroplasty is the most common and successful intervention in geriatric patients with cervical hip fractures, but patient outcomes may be compromised by early infections, eg, pneumonia, surgical site infection (SSI), and urinary tract infection (UTI), which are uncommon but may be of clinical importance. It was shown that pneumonia, UTI, and early deep SSI exhibited a 10.7-fold, 1.6-fold, and 2.4-fold increase in 90-day mortality following primary hip arthroplasties, respectively.1,2 In addition, early infections can be important triggers of several severe complications, including deep sepsis, acute heart failure, and disability in activities of daily living.3–5 Given the population aging trend, prevalence of osteoporosis, and the predicted increasing utilization rate of hip arthroplasty worldwide (ie, 184/100,000 population in 2015 and expected to exceed 275/100,000 population in 2050),6 it is of prime importance to find appropriate ways to effectively prevent early infections after hip arthroplasty.
Optimizing surgical plan and perioperative management based on preoperative infection risk scores is a promising strategy to address this issue. Previous studies had confirmed that modifiable surgery-related factors and postoperative management were significantly associated with the development of SSI, such as longer surgical duration, regional anesthesia, and absence of antibiotic stewardship interventions.7–9 To date, multiple studies have been devoted to developing risk prediction models related to infectious complications following hip arthroplasty for any reason (eg, fracture, osteoarthritis, or osteonecrosis), but controversy still surrounded their validity and reliability.10–12 For example, according to the clinical data of 3776 patients with primary total hip or knee arthroplasties, Sweerts et al10 established a scoring system for predicting risk of postoperative complications, including SSI, delirium, nerve damage, and so on. However, the tool was not specifically tailored to infections and would underestimate the risk of SSI when with a predicted probability >0.10. Recently, Bülow et al11 developed and validated a risk prediction model for periprosthetic joint infection (PJI) within 90 days following total hip arthroplasty (THA), and confirmed its superior discriminatory ability compared to traditional models. Nevertheless, the inflammatory biomarkers with high predictive value for infections were not incorporated and the area under the curve (AUC) <0.7 suggested relatively inadequate accuracy of the model in their study. Moreover, isolated investigation may lead to a diminished or neglected predictive value of certain potential risk factors when considering the inherent correlation between infectious complications.13
Therefore, we attempted to investigate the composite complications consisting of pneumonia, SSI, and UTI, aiming to identify independent preoperative risk factors associated with early infections after primary arthroplasty in geriatric patients with hip fracture, based on which, to develop a risk prediction model.
Materials and Methods
General Information
This study retrospectively collected clinical data of acute hip fracture patients over 65 years old undergoing primary total hip arthroplasty or hemiarthroplasty at the 3rd Hospital of Hebei Medical University from January 2016 to January 2021, which were available from the Surgical Site Infection in Orthopaedic Surgery (SSIOS) database. The SSIOS database has been used in many previous studies,14–16 which is a single-center, annually updated, and prospectively manually maintained database of all the data on more than 70,000 inpatients experiencing orthopedic surgeries in the 3rd Hospital of Hebei Medical University. The exclusion criteria: (a) old fracture (time to surgery ≥21 days), (b) pathologic fracture, (c) death for any cause within one month after surgery, (d) multiple fractures or polytrauma, (e) incomplete or missing data, (f) lost to follow-up. According to a staging system, we defined early infection as occurring up to one month after hip arthroplasty. For discharged patients, the follow-up data were obtained through telephone calls and/or outpatient review one month following surgery. The current research complied with the Helsinki Declaration consensus, following the guideline of Strengthening the Reporting of Cohort Studies in Surgery (STROCSS), and approved by the ethics committee of the 3rd Hospital of Hebei Medical University. All patients and/or their families were informed that their clinical data may be collected for medical research and had written their informed consent during hospitalization.
Data Collection
The retrospectively collected clinical data comprised demographics, injury-concerned data, chronic comorbidities, and laboratory biomarkers. The demographics involved age, gender, calculated body mass index (BMI), and living place. The injury-concerned data included fracture type, time to surgery, and the American Society of Anesthesiologists (ASA) index. Time to surgery was calculated by adding the time to admission to the time from admission to surgery, which were obtained from medical records. Based on medical records, the time to admission was obtained from chief complaint (eg, “one day of pain in the left hip caused by a fall”) and the time from admission to surgery was calculated according to the date and time of hospitalization and operation. Time to surgery was in days, and we recorded it as 0 days when it was less than 1 day. The chronic comorbidities comprised hypertension, tumors, diabetes mellitus, heart disease, liver disease, renal disease, cerebrovascular disease, chronic respiratory disease, alcohol consumption, currently smoking, history of allergy, and previous surgeries. The laboratory biomarkers involved the count of neutrophil, platelet, lymphocyte, red blood cell (RBC), and white blood cell (WBC); the levels of high-sensitivity C-reactive protein (HCRP), albumin, total protein (TP), hemoglobin, fasting blood glucose (FBG), hematocrit, mean platelet volume (MPV), the platelet-to-mean platelet volume ratio (PMR), and the neutrophil-to-lymphocyte ratio (NLR). The laboratory biomarkers were collected from routine blood and biochemical examinations before surgery, whichever comes earliest.
Diagnosis of Early Infection
The occurrence of early infections, as a composite adverse outcome, was defined as the onset of any of the following conditions within one month after surgery: SSI, UTI, and pneumonia. Superficial SSI was diagnosed as an infection involving only the skin and/or subcutaneous tissue, combined with one or more of the following presentations: purulent discharge; wound signs (swelling, pain, redness, or heat); spontaneous incision dehiscence and positive culture results of bacterial. Deep SSI was diagnosed when infections involved fascia, muscle, or deep tissues, and accompanied by the abovementioned symptoms.17 Pneumonia was diagnosed as the presence of new pulmonary infiltrations and at least one of the following clinical evidences: (1) presence of new or persistent and progressive respiratory symptoms, involving purulent discharge and cough; (2) hypothermia (body temperature <36.0°C) or fever (body temperature >38.0°C); (3) lung consolidation or moist rale observed during physical examinations; (4) positive culture results of sputum or blood; (5) leukocytosis (>10×109/L) and/or leukopenia (<4×109/L) shown in hematologic examinations.18 The new pulmonary infiltrations were detected by computed tomography (CT) scan or X-rays of the chest. UTI was diagnosed when patients were found to have positive urine bacterial culture results with at least one of the following symptoms: urinary frequency, urgency, hematuria, urinary retention, dysuria, suprapubic pain, or febrile reactions.19
Statistical Analysis
SPSS software 26.0 (IBM Corporation, Armonk, NY, USA) was used for the univariate and multivariate analyses of potential risk factors. According to the normality, continuous variables were evaluated by performing the Student’s t-test or Mann–Whitney test. The categorical variables were assessed by using the Chi-square test or Fisher’s exact test, where the optimal cutoff value of HCRP, NLR, and PMR was calculated based on the maximum Youden index. Then, the variables with P-value <0.1 were taken into multivariate logistic regression analysis, and the backward stepwise regression method was applied to identify the independent risk factors and the optimal predictors combination, which was assessed by the area under the receiver operating characteristic (ROC) curve and Hosmer–Lemeshow goodness-of-fit test. The screened covariates and outcome variable were entered in the R software 3.6.5 (R Foundation for Statistical Computing, Vienna, Austria) to develop a nomogram model by using “rms” and “DynNom” packages. The conformance index (C-index) was used to assess its discriminatory performance, ranging from 0.5 (no discrimination) to 1 (complete discrimination). Calibration curves and decision curve analysis (DCA) were applied to visually evaluate the calibration and clinical net benefit of the risk prediction model. The bootstrap method set to 1000 replications was employed for internal verification. P < 0.05 was considered statistically significant for all analyses.
Results
Clinical Characteristics
A total of 1383 patients were initially enrolled, and 299 were ruled out according to exclusion criteria (Figure 1). If a patient suffered from 2 or more different infections during the observation period, this was counted as only once for the outcome event. Finally, 1084 patients eligible were analyzed in the present study, and 42 (3.9%) cases were diagnosed as early infections after primary hip arthroplasty, among which 9 developed superficial SSI, 1 developed deep SSI, 8 developed UTI and 32 developed pneumonia. Compared to the control group, patients in the infection group were older (years, 80.0 vs 77.0), more male (50.0% vs 30.1%), and had more chronic comorbidities, such as heart disease, cerebrovascular disease, and liver disease (all P < 0.05).
 |
Figure 1 Flowchart of patient eligibility screening. |
Univariate and Multivariate Analysis
In univariable analysis, there were statistically significant differences between early infections and 10 covariates, involving gender (male), heart disease, cerebrovascular disease, liver disease, time to surgery, RBC (<lower limit), hematocrit (<lower limit), MPV (<7.4fL), PMR (>44.52), and HCRP (>78.64mg/L) (Table 1). Eleven factors with P value <0.1 were included in multivariate analysis, and heart disease, cerebrovascular disease, liver disease, time to surgery, hematocrit, PMR, and HCRP were ultimately identified as independent risk factors for early infections (Table 2). The AUC for the combination of the above predictors was 0.807 (95% confidence interval (CI): 0.742–0.873), with the specificity of 0.743 (95% CI: 0.716–0.769) and sensitivity of 0.738 (95% CI: 0.605–0.871) (Figure 2). And the Hosmer-Lemeshow test demonstrated no overfitting (P = 0.522).
 |
Table 1 Univariate Analysis of Variables with Interest Between Infectious and Non-Infectious Groups |
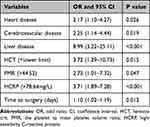 |
Table 2 Multivariate Analyses of the Independent Risk Factors Associated with Early Infections |
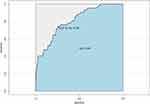 |
Figure 2 Receiver operating characteristic curve (ROC) of the predictors combination for early infections after hip arthroplasty. |
Development and Validation of a Dynamic Nomogram
These seven predictors were substituted into R software and converted into a simple nomogram and a dynamic nomogram (Figure 3). The simple nomogram is suitable for remote areas, and clinicians can eventually obtain the predicted probability of early infections by drawing vertical lines on different fraction axes and adding up the scores of each covariate. By using the web-based dynamic nomogram, clinicians can get the predicted risk and 95% CI of early infections by inputting the results of each covariate. The C-index for the prediction model was 0.807 (95% CI: 0.742–0.872) and was corrected to 0.784 after 1000 bootstrapping validations, which suggested a good discriminatory ability. The calibration curve exhibited good consistency between the actual and predicted probability, and the DCA showed that the nomogram can bring net positive benefit when the threshold probability ranged from 0.01 to 0.78 (Figure 4).
 |
Figure 3 Development of a simple nomogram (A) and a dynamic online nomogram (B, https://nomogramssi.shinyapps.io/Dyn-omogram/) to predict the risk of early infections following Hip arthroplasty in geriatric patients with Hip fracture. Abbreviations: HCT, hematocrit; PMR, the platelet to mean platelet volume ratio; HCRP, high-sensitivity C-reactive protein. |
 |
Figure 4 Calibration curve (A) and decision curve analysis (DCA, B) of the nomogram for predicting the risk of early infections. |
Discussion
In this study, heart disease, cerebrovascular disease, liver disease, time to surgery, hematocrit, PMR, and HCRP were identified as independent risk factors for the occurrence of early infections following primary arthroplasty in geriatric hip fracture patients, based on which, a predictive nomogram was established and showed strong translatability to clinical application.
Early operation within 24–48 hours after admission has been well established to decrease the incidence of postoperative complications (eg, pneumonia, SSI, and even death) in elderly hip fracture patients.20 In this study, we found that delayed admission is a main cause for long interval from injury to operation. In fact, the effect of delayed admission on surgical delay is nonnegligible, especially in tertiary referral trauma centers, because a large number of patients are transferred from relatively remote hospitals, which has been confirmed by Marley et al.21 In addition, we observed a 10% increased risk of early infections for each day of surgical delay, which could be explained by the consumption and imbalance of complement cascade components, and the systemic inflammatory response syndrome (SIRS) secondary to acute trauma.22,23 However, the arbitrary decision on interventions applied to decrease preoperative stay does not necessarily translate into better therapeutic effect, as for geriatric trauma patients, delayed surgery is largely due to the requirement of more time to optimize the poor medical conditions or unstable hemodynamic conditions before surgery, eg, frailty, undesirable soft-tissue conditions, and insulin-dependent. In this case, a co-management model involving geriatricians and orthopedic surgeons may be a feasible and effective approach,24,25 and the clinician should balance the risks and benefits, especially for those of advanced age and poor general conditions, before a decision is made.
Anemia is common in the elderly population, as a significant influential risk factor for poor postoperative outcomes following hip fracture. In a study of 34,805 geriatric patients presenting with unilateral hip fracture, preoperative anemia was independently associated with higher rates of 30-day mortality (5.0% vs 2.5%) and all-cause readmission (9.6% vs 6.7%), compared to non-anemic group.26 As an indicator of anemia, hematocrit (< lower limit) was confirmed to be independently related to a 3.72-fold risk of early infections following hip arthroplasty in this study. The potential mechanism could derive from anemia itself and/or chronic sequelae of anemia.26 However, it should be recognized that adverse reactions of allogeneic blood transfusions, including circulatory overload, potential infections, and allergic transfusion reactions, may put patients at higher risk of infections after arthroplasty.27 Recently, a systematic blood management protocol was reported to be effective in improving 90-day postoperative outcomes and should be considered in clinical application for newly admitted elderly hip fracture patients with anemia.28
CRP is an acute phase protein, with levels increasing with the progression of inflammation, and shows significant predictive role for early infections after arthroplasty in this study. Similar to our findings, Pfitzner et al29 observed significantly elevated concentrations of preoperative CRP in the infection group (1.3 ± 2.5 vs 0.4 ± 0.7 mg/dl) among patients undergoing primary arthroplasty. In addition to bacterial infection, advanced age and bouts of inflammation including burns, cancer, and tissue trauma can trigger subsequent CRP elevation,30 making CRP less specific in diagnosing infections. Therefore, researchers have tried to combine CRP with other biomarkers and compensated this deficiency,31,32 as also employed in our study. Elevated PMR reflects the activity of systemic inflammatory response in the body, and the PMR level above 44.52 was found independently associated with a 2.73-fold increased risk of early infections following hip arthroplasty in this study. This can be interpreted as the fact that circulating platelets can directly facilitate leukocyte response to infection.33 Similarly, Tirumala et al34 found that the combination of PMR and biomarkers in serum and synovial fluid achieved near-perfect diagnostic utility (sensitivity 98.54%, specificity 97.89%) in PJI after TKA. The above findings suggested that combining CRP or PMR with multiple biomarkers would significantly improve the diagnostic accuracy of infectious complications, which deserves consideration for clinical application.
In this study, we observed that cerebrovascular disease is independently associated with a 2.25-fold increased risk of early infections, which could be explained by either the extended immobility duration for functional recovery or potential motor and sensory deficits.35,36 Numerous studies have confirmed that heart disease predisposed trauma patients to infection, and attributed this to the following possible mechanisms. On one hand, blood circulation disorders caused by chronic heart disease can lead to edema at the surgical site and interfere with wound healing.37 On the other hand, in addition to promoting the development of pulmonary congestion, acute heart failure would cause hypoperfusion and poor nutrient supply of organs and peripheral tissue.38 The correlation between liver disease and postoperative infectious complications has been extensively discussed and validated. Notably, Bedair et al39 studied 105 chronic hepatitis C patients with primary THA and found that those on anti-hepatitis C virus (HCV) therapy exhibit significantly lower risk of developing PJI (0.0% vs 14.3%), which suggested that aggressive treatment of liver disease is a promising cost-effective strategy for early prevention of infections after hip arthroplasty.
The major merits of this study are the large sample size, and the development of a nomogram model to allow direct visualization of multivariate analysis results to facilitate risk assessment by clinicians for elderly hip fracture patients scheduled for hip arthroplasty. All seven predictors are rapidly available from routine laboratory tests and the report of patient and/or their families within hours of admission, based on which, the predicted probability can be conveniently obtained by inputting the results on a webpage or drawing vertical lines on corresponding axes. However, some limitations should be pointed out. Firstly, all data were retrospectively collected and some information was reported by the patients as well as their families, thus inherent selection bias and recall bias were inevitable. Secondly, the nomogram model was based on single-center data and lacked external validation, which requires multicenter data to further validate its accuracy and clinical applicability. Thirdly, surgery performed delayed day 5–6 post trauma might influence all data mostly inflammatory parameters. Fourthly, considering the competitive risk of death and inability to determine the infection diagnosis, this study excluded the patients died within 30 days postoperatively (2.8%), which may lead to potential bias and reduced infections. Therefore, for patients died within 30 days postoperatively, the accuracy and reliability of this infection prediction model need to be further verified and optimized in future studies.
Conclusion
On the whole, we identified heart disease, cerebrovascular disease, liver disease, time to surgery, hematocrit, PMR, and HCRP as independent risk factors for the development of early infections following primary arthroplasty in elderly hip fracture patients, and converted the combination of the above predictors into a practical nomogram model, which had strong translatability and discriminatory ability. Clinicians can employ the nomogram to rapidly identify the geriatric trauma patients at high risk for infectious complications after hip arthroplasty, and intervene early to prevent the development of potentially catastrophic consequences.
Abbreviations
SSI, surgical site infection; UTI, urinary tract infection; DCA, decision curve analysis; C-index, concordance index; OR, odds ratio; PJI, periprosthetic joint infection; THA, total hip arthroplasty; ROC, receiver operating characteristic; AUC, the area under the curve; SSIOS, Surgical Site Infection in Orthopaedic Surgery; STROCSS, Strengthening the Reporting of Cohort Studies in Surgery; BMI: Body mass index; ASA, American Society of Anesthesiologists; RBC, red blood cell, reference range: Female, 3.5–5.0×1012/L; males, 4.0–5.5×1012/L; HCT, hematocrit, reference range: Females, 35–45%; males, 40–50%; HGB, hemoglobin, reference range: Females, 110–150g/L; males, 120–160g/L; PLT, platelet; MPV, mean platelet volume; PMR, the platelet to mean platelet volume ratio; WBC, white blood cell; NEU, neutrophil; LYM, lymphocyte; NLR, the neutrophil-to-lymphocyte ratio; TP, total protein; ALB, albumin; FBG, fasting blood glucose; HCRP, high-sensitivity C-reactive protein; CT, computed tomography; SIRS, systemic inflammatory response syndrome; HCV, hepatitis C virus.
Data Sharing Statement
All the data used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Consent to Participate
This study was approved by the ethics committee of the 3rd Hospital of Hebei Medical University and the informed consent was waived for its retrospective nature. All the data were analyzed anonymously to safeguard patient privacy.
Consent for Publication
We have obtained the consent for publication from all participants.
Acknowledgments
The Key Laboratory of Biomechanics of Hebei Province provided the site for querying data.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
The authors have received no external funding in order to support this project.
Disclosure
The authors declare no conflicts of interest in this work.
References
1. Pollmann CT, Dahl FA, Røtterud JHM, Gjertsen J-E, Årøen A. Surgical site infection after Hip fracture – mortality and risk factors: an observational cohort study of 1709 patients. Acta Orthopaedica. 2020;91(3):347–352. doi:10.1080/17453674.2020.1717841
2. Glassou EN, Hansen TB, Pedersen AB. Risk of pneumonia and urinary tract infection within the first week after total Hip arthroplasty and the impact on survival. Clin Epidemiol. 2017;9:31–39. doi:10.2147/CLEP.S122829
3. Schmalzried TP, Amstutz HC, Au MK, Dorey FJ. Etiology of deep sepsis in total Hip arthroplasty. The significance of hematogenous and recurrent infections. Clin Orthop Relat Res. 1992;280:200–207.
4. Rudiger A, Streit M, Businger F, Schmid ER, Follath F, Maggiorini M. The impact of infections on critically ill acute heart failure patients: an observational study. Swiss Med Wkly. 2010;140:w13125. doi:10.4414/smw.2010.13125
5. Caljouw MA, Kruijdenberg SJ, de Craen AJ, Cools HJ, den Elzen WP, Gussekloo J. Clinically diagnosed infections predict disability in activities of daily living among the oldest-old in the general population: the Leiden 85-plus Study. Age Ageing. 2013;42(4):482–488. doi:10.1093/ageing/aft033
6. Pabinger C, Lothaller H, Portner N, Geissler A. Projections of Hip arthroplasty in OECD countries up to 2050. Hip Int. 2018;28(5):498–506. doi:10.1177/1120700018757940
7. Liu X, Dong Z, Li J, et al. Factors affecting the incidence of surgical site infection after geriatric Hip fracture surgery: a retrospective multicenter study. J Orthop Surg Res. 2019;14(1):382. doi:10.1186/s13018-019-1449-6
8. Matharu GS, Garriga C, Rangan A, Judge A. Does regional anesthesia reduce complications following total hip and knee replacement compared with general anesthesia? An Analysis From the National Joint Registry for England, Wales, Northern Ireland and the Isle of Man. J Arthroplasty. 2020;35(6):1521–1528.e5. doi:10.1016/j.arth.2020.02.003
9. Fésüs A, Benkő R, Matuz M, et al. The effect of pharmacist-led intervention on Surgical Antibacterial Prophylaxis (SAP) at an orthopedic unit. Antibiotics. 2021;10(12):1509. doi:10.3390/antibiotics10121509
10. Sweerts L, Hoogeboom TJ, van Wessel T, van der Wees PJ, van de Groes SAW. Development of prediction models for complications after primary total Hip and knee arthroplasty: a single-centre retrospective cohort study in the Netherlands. BMJ Open. 2022;12(8):e062065. doi:10.1136/bmjopen-2022-062065
11. Bülow E, Hahn U, Andersen IT, Rolfson O, Pedersen AB, Hailer NP. Prediction of early periprosthetic joint infection after total hip arthroplasty. Clin Epidemiol. 2022;14:239–253. doi:10.2147/CLEP.S347968
12. Kunutsor SK, Whitehouse MR, Blom AW, Beswick AD. Systematic review of risk prediction scores for surgical site infection or periprosthetic joint infection following joint arthroplasty. Epidemiol Infect. 2017;145(9):1738–1749. doi:10.1017/S0950268817000486
13. Schmitt DR, Schneider AM, Brown NM. Impact of perioperative urinary tract infection on surgical site infection in patients undergoing primary hip and knee arthroplasty. J Arthroplasty. 2020;35(10):2977–2982. doi:10.1016/j.arth.2020.05.025
14. Cheng X, Fan L, Hao J, He H, Yan J, Zhu Y. Red cell distribution width-to-high-density lipoprotein cholesterol Ratio (RHR): a promising novel predictor for preoperative deep vein thrombosis in geriatric patients with hip fracture. Clin Interv Aging. 2022;17:1319–1329. doi:10.2147/CIA.S375762
15. Cheng X, Lei X, Wu H, et al. Development and validation of a predictive nomogram for preoperative deep vein thrombosis (DVT) in isolated calcaneal fracture. Sci Rep. 2022;12(1):5923. doi:10.1038/s41598-022-10002-8
16. Zhu Y, Chen W, Qin S, Zhang Q, Zhang Y. Surgeon volume and risk of deep surgical site infection following open reduction and internal fixation of closed ankle fracture [published online ahead of print, 2022 May 31]. Int Wound J. 2022. doi:10.1111/iwj.13819
17. Horan TC, Gaynes RP, Martone WJ, Jarvis WR, Emori TG. CDC definitions of nosocomial surgical site infections, 1992: a modification of CDC definitions of surgical wound infections. Infect Control Hosp Epidemiol. 1992;13(10):606–608.
18. Kalil AC, Metersky ML, Klompas M, et al. Management of adults with hospital-acquired and ventilator-associated pneumonia: 2016 clinical practice guidelines by the Infectious Diseases Society of America and the American Thoracic Society. Clin Infect Dis. 2016;63(5):e61–e111. doi:10.1093/cid/ciw353
19. Gupta K, Grigoryan L, Trautner B. Urinary Tract Infection. Ann Intern Med. 2017;167(7):ITC49–ITC64. doi:10.7326/AITC201710030
20. Glassou EN, Kjørholt KK, Hansen TB, Pedersen AB. Delay in surgery, risk of hospital-treated infections and the prognostic impact of comorbidity in Hip fracture patients. A Danish nationwide cohort study, 2005–2016. Clin Epidemiol. 2019;11:383–395. doi:10.2147/CLEP.S200454
21. Marley MA, Lambers A, Marley I, Welthy L, Seymour H. The tyranny of distance: how hospital transfer affects time to surgery for hip fracture patients. Cureus. 2022;14(2):e22662. doi:10.7759/cureus.22662
22. Burk AM, Martin M, Flierl MA, et al. Early complementopathy after multiple injuries in humans. Shock. 2012;37(4):348–354. doi:10.1097/SHK.0b013e3182471795
23. Lord JM, Midwinter MJ, Chen YF, et al. The systemic immune response to trauma: an overview of pathophysiology and treatment. Lancet. 2014;384(9952):1455–1465. doi:10.1016/S0140-6736(14)60687-5
24. Basu N, Natour M, Mounasamy V, Kates SL. Geriatric Hip fracture management: keys to providing a successful program. Eur J Trauma Emerg Surg. 2016;42(5):565–569. doi:10.1007/s00068-016-0685-2
25. Baroni M, Serra R, Boccardi V, et al. The orthogeriatric comanagement improves clinical outcomes of Hip fracture in older adults. Osteoporos Int. 2019;30(4):907–916. doi:10.1007/s00198-019-04858-2
26. Ryan G, Nowak L, Melo L, et al. Anemia at presentation predicts acute mortality and need for readmission following geriatric hip fracture. JB JS Open Access. 2020;5(3):
27. Newman ET, Watters TS, Lewis JS, et al. Impact of perioperative allogeneic and autologous blood transfusion on acute wound infection following total knee and total Hip arthroplasty. J Bone Joint Surg Am. 2014;96(4):279–284. doi:10.2106/JBJS.L.01041
28. Partridge J, Harari D, Gossage J, Dhesi J. Anaemia in the older surgical patient: a review of prevalence, causes, implications and management. J R Soc Med. 2013;106(7):269–277. doi:10.1177/0141076813479580
29. Pfitzner T, Krocker D, Perka C, Matziolis G. Das C-reaktive Protein. Ein unabhängiger Risikofaktor für die Entwicklung eines Infekts nach Primärendoprothetik [C-reactive protein. An independent risk factor for the development of infection after primary arthroplasty]. Orthopade. 2008;37(11):1116–1120. German. doi:10.1007/s00132-008-1342-1
30. Bertsch T, Triebel J, Bollheimer C, et al. C-reactive protein and the acute phase reaction in geriatric patients. Z Gerontol Geriatr. 2015;48(7):595–600. doi:10.1007/s00391-015-0938-4
31. Xu H, Xie JW, Liu L, Wang D, Huang ZY, Zhou ZK. Combination of CRP with NLR is a sensitive tool for screening fixation-related infection in patients undergoing conversion total Hip arthroplasty after failed internal fixation for femoral neck fracture. Bone Joint J. 2021;103-B(9):1534–1540. doi:10.1302/0301-620X.103B.BJJ-2021-0105.R1
32. Fury MS, Klemt C, Barghi A, Tirumala V, van den Kieboom J, Kwon YM. Preoperative serum C-reactive protein/albumin ratio is a predictor of complications after single-stage revision for the treatment of periprosthetic joint infection. J Am Acad Orthop Surg. 2021;29(20):e1013–e1024. doi:10.5435/JAAOS-D-20-00613
33. Gaertner F, Ahmad Z, Rosenberger G, et al. Migrating platelets are mechano-scavengers that collect and bundle bacteria. Cell. 2017;171(6):1368–1382.e23. doi:10.1016/j.cell.2017.11.001
34. Tirumala V, Klemt C, Xiong L, Chen W, van den Kieboom J, Kwon YM. Diagnostic utility of platelet count/lymphocyte count ratio and platelet count/mean platelet volume ratio in periprosthetic joint infection following total knee arthroplasty. J Arthroplasty. 2021;36(1):291–297. doi:10.1016/j.arth.2020.07.038
35. Cichos KH, Lehtonen EJ, McGwin G, Ponce BA, Ghanem ES. Inhospital complications of patients with neuromuscular disorders undergoing total joint arthroplasty. J Am Acad Orthop Surg. 2019;27(11):e535–e543. doi:10.5435/JAAOS-D-18-00312
36. Du P, Zhu Y, Guo J, et al. Incidence and risk factors associated with surgical site infection after surgically treated Hip fractures in older adults: a retrospective cohort study. Aging Clin Exp Res. 2022;34(5):1139–1148. doi:10.1007/s40520-021-02027-2
37. Guo S, Dipietro LA. Factors affecting wound healing. J Dent Res. 2010;89(3):219–229. doi:10.1177/0022034509359125
38. Arrigo M, Jessup M, Mullens W, et al. Acute heart failure. Nat Rev Dis Primers. 2020;6(1):16. doi:10.1038/s41572-020-0151-7
39. Bedair HS, Schurko BM, Dwyer MK, Novikov D, Anoushiravani AA, Schwarzkopf R. Treatment for chronic hepatitis C prior to total hip arthroplasty significantly reduces periprosthetic joint infection. J Arthroplasty. 2019;34(1):132–135. doi:10.1016/j.arth.2018.09.036
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
