Back to Journals » Clinical Interventions in Aging » Volume 18
Construction and Validation of a Nomogram for Predicting Acute Kidney Injury After Hip Fracture Surgery
Authors Pan L, Liu Z, Wu H , Wang H, Wang H, Ning T, Liang G, Cao Y
Received 29 November 2022
Accepted for publication 8 February 2023
Published 12 February 2023 Volume 2023:18 Pages 181—191
DOI https://doi.org/10.2147/CIA.S399314
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Zhi-Ying Wu
Liping Pan,* Zhenning Liu,* Hao Wu, Hao Wang, Hongbin Wang, Taiguo Ning, Guanghua Liang, Yongping Cao
Department of Orthopedics, Peking University First Hospital, Beijing, 100034, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Yongping Cao, Department of Orthopedics, Peking University First Hospital, No. 8 Xishiku Street, XiCheng District, Beijing, 100034, People’s Republic of China, Email [email protected]
Background: Acute kidney injury (AKI), characterized by sudden impairment of kidney function, is an uncommon complication following hip fracture surgery that is associated with increased morbidity and mortality. We constructed a nomogram to stratify patients according to risk of AKI after hip fracture surgery to guide clinicians in the implementation of timely interventions.
Methods: Patients who received hip fracture surgery from January 2015 to December 2021 were retrospectively identified and divided into a training set (n=448, surgery from January 2015 to December 2019) and a validation set (n=200, surgery from January 2020 to December 2021). Univariate and multivariate logistic regression were used to identify risk factors for AKI after surgery in the training set. A nomogram was constructed based the risk factors for AKI, and was evaluated by receiver operating characteristic (ROC) analysis, calibration curves, and decision curve analysis (DCA).
Results: The mean age was 82.0± 6.22 years-old and the prevalence of post-surgical AKI was 13.3%. Age, American Society of Anesthesiologists (ASA) score, the preexistence of chronic kidney disease (CKD), cemented surgery and the decrease of hemoglobin on the first day after surgery were identified as independent risk factors of AKI after hip fracture surgery, and a predictive nomogram was established based on the multivariable model. The predictive nomogram had good discrimination ability (training set: AUC: 0.784, 95% CI: 0.720– 0.848; validation set: AUC: 0.804, 95% CI: 0.704– 0.903), and showed good validation ability and clinical usefulness based on a calibration plot and decision curve analysis.
Conclusion: A nomogram that incorporated five risk factors including age, ASA score, preexisting CKD, cemented surgery and the decrease of hemoglobin on the first day after surgery had good predictive performance and discrimination. Use of our results for early stratification and intervention has the potential to improve the outcomes of patients receiving hip fracture surgery. Future large, multicenter cohorts are needed to verify the model’s performance.
Keywords: hip fracture, geriatrics, acute kidney injury, nomogram
Introduction
Hip fracture in elderly patients is a major public health challenge that has devastating consequences throughout the world because of the large financial burden and because patients have increased morbidity and mortality.1–4 An epidemiology study estimated that hip fractures affect about 18% of women and 6% of men worldwide.3 To improve the survival time, quality of life, and life expectancy of these patients, surgical intervention is the most appropriate option when there are no contraindications for surgery. However, many patients have a high risk of complications during the perioperative period, and these complications can have severe consequences.5
Acute kidney injury (AKI) is a potentially serious complication characterized by the sudden impairment of kidney function, and it can occur following admission to a hospital or intensive care unit. AKI is significantly associated with increased morbidity and mortality, longer hospital stays, and high healthcare costs.6 The clinical practice guidelines for AKI proposed by Kidney Disease Improving Global Outcomes (KDIGO) provides a definition, and describes the major risk factors and optimal treatments.6 The KDIGO guidelines define AKI as an increase of the serum creatinine (SCr) level by 26.5 μmol/L or more within 48 h, an increase of the SCr level to 1.5-fold or more above the baseline level within 1 week, or a urine volume less than 0.5 mL/kg/h for 6 h.
Previous studies have examined the onset, risk factors and outcomes of AKI after hip fracture surgery.7,8 A study in South Korea reported the prevalence of AKI after this surgery ranged from 8% to 24%.9 Another study confirmed that the onset of AKI after surgery for hip fracture or other reasons was an independent contributor to postoperative morbidity and mortality.10 Many risk factors of AKI after hip fracture surgery had been identified in literature.7–9,11 There have also been efforts to develop interventions for the prevention and treatment of AKI after hip fracture surgery based on these reported risk factors. However, rare predictive model for AKI after hip fracture surgery is currently available.
Thus, this study aimed to construct a nomogram for predicting AKI in elderly patients after hip fracture surgery. The results may have significant value for surgeons by helping them to stratify patients according to risk of AKI so that appropriate measures for prevention and treatment can be implemented.
Methods and Patients
Patients and Study Design
This study was approved by the Institutional Ethics Committee of Peking University First Hospital (No. 2021-432), and complied with the Declaration of Helsinki. The informed consent was waived because it was a retrospective study. All the data collected was confidential. The records of patients who underwent hip fracture surgery at Peking University First Hospital (Beijing, China) from January 2015 to December 2021 were retrospectively examined. The inclusion criteria were: (i) diagnosis of hip fracture, namely intertrochanteric fracture or femoral neck fracture; (ii) age of at least 70 years-old; and (iii) receipt of surgery consisting of a plate/screw fixation, a hemiarthroplasty, or a total hip arthroplasty, instead of conservative treatment. The exclusion criteria were: (i) age less than 70 years-old; (ii) receipt of conservative treatment; (iii) end-stage kidney disease with dialysis before surgery for these patients could not be defined as AKI or not according to KDIGO criteria.
Data were extracted from the electronic medical record system. An initial search for the main diagnosis of femoral neck fracture or intertrochanteric fracture yielded 881 patients during the study period. After removing 212 patients who were younger than 70 years-old, 13 patients who received conservative therapy, and 8 patients who received renal dialysis for end-stage chronic kidney disease (CKD), 648 patients were included in the final analysis (Figure 1). Based on the date of surgery, these patients were divided into a training set (n = 448, surgery from January 2015 to December 2019) and a validation set (n = 200, surgery from January 2020 to December 2021).
Data Collection
The basic demographic characteristics (gender, age, and body mass index [BMI]) and clinical characteristics (Charlson Comorbidities Index [CCI], American Society of Anesthesiologists [ASA] score, preexisting comorbidities, fracture type, anesthesia type, intraoperative hypotension, cemented or cementless surgery, duration of surgery, length of hospital stay, complications, transfusion, and laboratory test results) were collected. Intraoperative hypotension was defined as mean arterial pressure of 65 mmHg or less for 10 min or more.12 The hip fracture surgery was classified as cemented surgery (including cemented hip hemiarthroplasty for femoral neck fracture) or cementless surgery (including cementless hip hemiarthroplasty, screw fixation for femoral neck fracture, and plating fixation and intermedullary fixation for intertrochanteric fracture). Laboratory test results included preoperative and postoperative hemoglobin, serum albumin, and sodium. The decrease of hemoglobin during the first day after surgery was calculated as the hemoglobin level before surgery minus the hemoglobin level on one day after surgery.
Definition of AKI
AKI after hip fracture surgery was defined by a change of postoperative SCr. According to the guidelines of the Kidney Disease Improving Global Outcomes (KDIGO) criteria, patients were diagnosed with AKI if any one of the following conditions were present: an increase in the SCr level of 0.3 mg/dL (26.5 µmol/L) or more within 48 h, or an increase in the SCr level of 1.5-times or more within 7 days, or a urine volume less than 0.5 mL/kg/h for 6 h.6
Statistical Analysis
Categorical variables were presented as numbers and percentages, and compared using Pearson’s chi-squared test. Continuous variables were presented as means ± standard deviations (SDs) or medians with 95% confidential intervals (CIs), and analyzed by a one way analysis of variance (ANOVA) or the Kruskal–Wallis test, as appropriate. Baseline characteristics and perioperative data were compared for the training set and the validation set.
The training set was used for construction of a nomogram. Univariate binary logistic regression was conducted to identify potential risk factors for AKI following hip fracture surgery, based on a threshold p value below 0.1. Multivariate binary logistic regression was conducted to identify independent risk factors for AKI, based on a threshold p value below 0.05 to construct a new model. The multivariable logistic regression model was transformed into a nomogram using the significant predictive factors.
The performance of the nomogram was internally evaluated using the training set and externally evaluated using the validation set. The discrimination of the nomogram was evaluated by the area under the receiver operating characteristic (AUC) curve. The calibration was assessed by the Hosmer-Lemeshow goodness of fit test and a calibration plot. Decision curve analysis was used to assess the net benefit of the nomogram and its clinical usefulness.
All statistical analyses were performed using SPSS version 25 and R software version 4.1.2 with the rms, rmda, pROC, PredictABEL, and ResourceSelection packages. A two-sided p value less than 0.05 was considered significant.
Results
Characteristics of the Training Set and Validation Set
We examined the records of 648 patients who had hip fracture surgery (Table 1). Overall, the mean age was 82.0 (±6.22) years-old, 379 patients (58.5%) had femoral neck fractures and 269 (41.5%) had intertrochanteric fractures, and 86 patients (13.3%) had AKI following hip fracture surgery. We divided these 648 patients into a training set and a validation set according to the date of surgery. The validation set was older, had a higher incidence of diabetes mellitus (DM), had lower levels of hemoglobin and albumin at admission, had a higher ASA score, had a higher CCI score, had a longer duration of surgery, was less likely to receive cemented surgery, was more less to receive combined spinal epidural anesthesia, had a longer operation duration, and had a greater decrease of hemoglobin on the first day after surgery (all P < 0.05).
 |
Table 1 Baseline and Perioperative Characteristics of Patients Who Received Hip Fracture Surgery in the Training Set and Validation Set |
Characteristics of AKI and Non-AKI Patients in the Training Set
Analysis of the training set indicated that 60 patients (13.4%) had AKI following hip fracture surgery (Table 2). The AKI group was older, had a higher incidence of pre-existing CKD, had a higher sodium level, had a higher ASA score, was more likely to receive cemented surgery, and had greater decreases of hemoglobin and albumin on the first day after surgery (all P < 0.05).
 |
Table 2 Baseline and Perioperative Characteristics of Patients with or Without AKI Who Received Hip Fracture Surgery in the Training Set |
Multivariate Analysis of Risk Factors for AKI in the Training Set and Establishment of a Nomogram
Multivariate analysis of the training set indicated that advanced age, a higher ASA score, pre-existing CKD, receipt of cemented surgery, and a greater decrease of hemoglobin in the one day after surgery were independent and significant predictors of AKI (Table 3). We then used these five predictors to develop a nomogram for prediction of AKI (Figure 2). The nomogram shows a horizontal scale for each of these five predictors. To determine the risk for AKI, an upward vertical line is first drawn from each scale to the Points scale on the top to determine the number of points for each predictor. Then, the total of all five predictors is determined. Finally, a downward vertical line is drawn from the Total Points scale to the AKI scale on the bottom to determine the risk of AKI.
 |
Table 3 Multivariate Logistic Regression Analysis of Risk Factors for AKI in the Training Set |
 |
Figure 2 Nomogram for the risk of AKI after Hip fracture surgery based on logistic regression analysis. |
ROC Analysis and Verification by a Calibration Plot and Decision Curve Analysis
ROC analysis of the training set indicated the AUC was 0.784 (95% CI: 0.720–0.848; Figure 3A). A calibration plot and Hosmer-Lemeshow goodness of fit test for the training set showed good calibration (p > 0.05; Figure 4A). Decision curve analysis showed that the nomogram had good clinical value (Figure 5).
 |
Figure 3 Receiver operating characteristic analysis of the training set (A) and validation set (B). |
 |
Figure 4 Calibration plot of the training set (A) and validation set (B). |
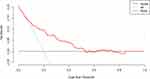 |
Figure 5 Decision curve analysis of the nomogram model. |
We also analyzed the validation set as an external evaluation of the accuracy of nomogram. ROC analysis of the validation set indicated the AUC was 0.804 (95% CI: 0.704-0.903; Figure 3B). As with the training set, the calibration plot and Hosmer-Lemeshow goodness of fit test for the validation set showed good calibration and good clinical value (p > 0.05; Figure 4B).
Discussion
AKI is an uncommon but potentially serious complication in elderly patients who receive surgery for hip fracture, and these patients have increased risk for multiple adverse outcomes, including longer hospital stay, increased mortality, and greater medical costs. Stratification of patients according to the risk of AKI and implementing early interventions following hip fracture surgery could help to preserve kidney function and improve patient outcome. We developed a nomogram to predict the risk of AKI following hip fracture surgery. Based on multivariable analysis, this nomogram had five predictors: age, ASA score, preexisting CKD, cemented surgery, and decrease of hemoglobin on the first day after surgery. The nomogram had good discriminability, with an AUC of 0.784 (95% CI: 0.720–0.848) in the training cohort and 0.804 (95% CI: 0.704–0.903) in the validation cohort. In addition, the corresponding calibration plot showed the nomogram was well-calibrated in the training and validation cohorts and decision curve analysis confirmed that the nomogram had good clinical usefulness.
Our screening for risk factors associated with AKI in patients following hip fracture considered many factors that are known to be associated with morbidity and mortality. Previous studies proposed that risk factors such as age, gender, BMI, preexisting CKD, pre- and postoperative hypoalbuminemia, comorbidities, hemoglobin changes, blood loss, and other factors were independent risk factors for AKI,9,13–16 although some other studies identified different risk factors.11,12 Chen et al studied patients following orthopedic surgery and proposed that age, hypertension, DM, hypoproteinemia, receipt of transfusion, and duration of low mean arterial pressure were independent risk factors for AKI.17 We analyzed the and many other factors, and our multivariate logistic regression results indicated that advanced age, high ASA score, preexisting CKD, receipt of cemented surgery, and large decrease of hemoglobin on the first day after surgery were significant and independent risk factors for AKI.
The ASA score is a useful general evaluation of the health status of a patient before surgery because it indicates the risk of the onset of perioperative complications. Several studies have demonstrated a relationship between high ASA score and AKI after surgery.17–19 Bell et al19 and Chen et al17 reported the ASA score was an independent risk factor for AKI in patients undergoing orthopedic surgery, and they established prediction models. Our results are consistent with the results of these previous studies, in that a higher ASA score indicated a higher risk of AKI after surgery.
Several other studies reported that preexisting CKD was a risk factor for AKI after surgery.20–22 Fontecha-Barriuso et al23 reviewed the relationship of pre-existing CKD with post-surgical AKI and found that these patients had increased risk of AKI. CKD is characterized by progressive and irreversible loss of kidney function. Nephrotoxicity, a cytokine storm, and ischemia-reperfusion injury are more likely to induce the onset of AKI in patients who have impaired kidney function. Because patients with hip fracture and CKD have an increased risk for mortality, we suggest that more attention should be given to these patients.
We found that receipt of cemented surgery for hip fracture was a significant and independent risk factor for AKI. Cemented surgery refers to the use of surgical cement for hip semi-arthroplasty in patients with displaced femoral neck fracture and severe osteoporosis, because the bones of these patients have increased porosity. Vancomycin or other antibiotics are routinely added to the cement. This procedure could increase the risk of AKI because of nephrotoxic effects induced by the cement or the antibiotic. A previous study examined the relationship of using vancomycin with bone cement on AKI after receipt of total knee replacement and found that vancomycin-loaded cement increased the risk of AKI.24
AKI is often associated with hypoperfusion, consistent with our finding that a decreased level of hemoglobin on the first day after surgery was an independent risk factor for AKI. Surgery can lead hypovolemia, and anesthetics can cause vasodilation and hypotension.10 Increased blood loss and a lower blood volume can lead to hypoperfusion of the kidneys and impaired kidney function.14 A decrease of the hemoglobin on the first day after surgery can be caused by obvious hemorrhage during surgery (which can be observed and measured), hidden blood loss (which cannot be observed after incision closure), and inadequate transfusion. The decline in hemoglobin therefore better reflects the change in blood volume and hypoperfusion than the volume of intraoperative blood loss. However, previous studies examined the effect of intraoperative hypotension on the risk of AKI and the results were discordant.12,25–27 We found that patients with intraoperative hypotension did not have a higher risk of AKI, which is consistent with some previous studies.12,27 Although intraoperative hypotension can theoretically cause hypoperfusion of the kidneys, anesthesiologists can successfully reduce the duration and severity of intraoperative hypotension unless there are severe intraoperative complications, such as shock or cardiac arrest. This is likely the reason why intraoperative hypotension was unrelated to the onset of AKI in our patients.
The nomogram proposed in our study, which incorporated age, ASA score, preexisting CKD, receipt of cemented surgery, and decrease of hemoglobin on the first day after surgery, had good performance based on internal and external validation. Some previous studies also proposed models for stratifying the risk of AKI after hip fracture surgery in geriatric patients, and examined the effects of many different risk factors. For example, Porter et al13 proposed a model that incorporated age, CKD, comorbidities, and sex to predict the risk of AKI after surgery for hip fracture. However, these researchers did not provide visual representation of the model, the discriminability of the model was not very good (AUC < 0.7), and they did not perform external validation. Bell et al19 proposed a prediction model for AKI in patients undergoing orthopedic surgery using data from three medical centers. However, they only examined preoperative parameters, and their omission of intraoperative and postoperative factors could adversely affect model performance because events during surgery can influence kidney function. Other studies used nomogram models to assess the risk of AKI after surgery, and these models had good performance, but they did not focus on patients receiving hip fracture surgery.20,21 In particular, Yu et al examined patients undergoing liver resection20 and Wang et al examined patients undergoing pericardiectomy.21 Our nomogram model incorporated preoperative and perioperative factors in patients undergoing hip fracture surgery and showed good performance in the internal and external validation. The nomogram is convenient and easy to use in clinical practice for its clear diagram and algorithm. It is very important for surgeons to identifying the onset of AKI as soon as possible after surgery because early interventions could effectively improve the prognosis.6,10 The five factors incorporated in the nomogram could be easily gained in the first day after surgery. And the high accuracy was validated by the training set and validation set. Thus, the nomogram could help surgeons stratifying the risk of AKI and taking immediate action in early phrase.
Our study had several limitations. First, this was a single center study. Studies of cohorts from other medical centers could help to more precisely identify risk factors and reduce selection bias. Second, although we validated the nomogram using a separate cohort from a different time period, all patients in the training and validation cohorts were from the same institution. Future studies should use cohorts from other centers for external validation.
Conclusion
We identified five risk factors that were significantly and independently associated with AKI following surgery for hip fracture: advanced age, high ASA score, preexisting CKD, receipt of cemented surgery, and a large decrease of hemoglobin on the first day after surgery. A nomogram that incorporated these five factors had good predictive value and was validated using an external cohort, although other large, multicenter cohorts are needed to confirm its clinical usefulness. Early stratification and implementation of appropriate interventions for patients with an increased risk for AKI has the potential to improve patient outcomes. The convenient and low-cost tool described here could be used to facilitate these interventions.
Abbreviations
AKI, Acute kidney injury; ROC, receiver operating characteristic; DCA, decision curve analysis; ASA, American Society of Anesthesiologists; CKD, chronic kidney disease; KDIGO, Kidney Disease Improving Global Outcomes; SCr, serum creatinine; BMI, body mass index; CCI, Charlson Comorbidities Index; AUC, receiver operating characteristic.
Data Sharing Statement
Data available on request from the authors.
Ethics Approval and Consent to Participate
This study was approved by the Institutional Ethics Committee of Peking University First Hospital (No. 2021-432), and complied with the Declaration of Helsinki. The informed consent was waived because it was a retrospective study. All the data collected was confidential.
Acknowledgments
The authors thank the doctors in the Department of Orthopedics, Peking University First Hospital for their help and advices in the process of data collection. Liping Pan and Zhenning Liu are co-first authors for this study.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
There is no funding to report.
Disclosure
The authors declare that they have no competing interests for this work.
References
1. Meagher E, Varghese S, Harty JA, O’Loughlin PF. The decline of hip fracture incidence rates over a 10-year period: a single centre experience. Injury. 2021;52(7):1807–1812. doi:10.1016/j.injury.2021.04.051
2. Trevisan C, Gallinari G, Carbone A, Klumpp R. Fifteen years change in acute management of hip fracture patients: 1-year mortality calls for improvements. Injury. 2021;52(8):2367–2372. doi:10.1016/j.injury.2021.01.025
3. Veronese N, Maggi S. Epidemiology and social costs of hip fracture. Injury. 2018;49(8):1458–1460. doi:10.1016/j.injury.2018.04.015
4. Pan L, Ning T, Wu H, et al. Prognostic nomogram for risk of mortality after hip fracture surgery in geriatrics. Injury. 2022;53(4):1484–1489. doi:10.1016/j.injury.2022.01.029
5. Goh EL, Lerner RG, Achten J, Parsons N, Griffin XL, Costa PML. Complications following hip fracture: results from the world hip trauma evaluation cohort study. Injury. 2020;51(6):1331–1336. doi:10.1016/j.injury.2020.03.031
6. Khwaja A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract. 2012;120(4):c179–c184. doi:10.1159/000339789
7. Zhou X, Zhang Y, Teng Y, et al. Predictors of postoperative acute kidney injury in patients undergoing hip fracture surgery: a systematic review and meta-analysis. Injury. 2021;52(3):330–338. doi:10.1016/j.injury.2020.09.060
8. Kang JS, Moon KH, Youn YH, Park JS, Ko SH, Jeon YS. Factors associated with postoperative acute kidney injury after hip fractures in elderly patients. J Orthop Surg. 2020;28(1):2309499019896237. doi:10.1177/2309499019896237
9. Shin KH, Han SB. Early postoperative hypoalbuminemia is a risk factor for postoperative acute kidney injury following hip fracture surgery. Injury. 2018;49(8):1572–1576. doi:10.1016/j.injury.2018.05.001
10. Zarbock A, Koyner JL, Hoste EAJ, Kellum JA. Update on perioperative acute kidney injury. Anesth Analg. 2018;127(5):1236–1245. doi:10.1213/ane.0000000000003741
11. Li ZC, Pu YC, Wang J, Wang HL, Zhang YL. The prevalence and risk factors of acute kidney injury in patients undergoing hip fracture surgery: a meta-analysis. Bioengineered. 2021;12(1):1976–1985. doi:10.1080/21655979.2021.1926200
12. Kluger MT, Collier JMK, Borotkanics R, van Schalkwyk JM, Rice DA. The effect of intra-operative hypotension on acute kidney injury, postoperative mortality and length of stay following emergency hip fracture surgery. Anaesthesia. 2022;77(2):164–174. doi:10.1111/anae.15555
13. Porter CJ, Moppett IK, Juurlink I, Nightingale J, Moran CG, Devonald MA. Acute and chronic kidney disease in elderly patients with hip fracture: prevalence, risk factors and outcome with development and validation of a risk prediction model for acute kidney injury. BMC Nephrol. 2017;18(1):20. doi:10.1186/s12882-017-0437-5
14. Zhan S, Xie W, Yang M, Zhang D, Jiang B. Incidence and risk factors of acute kidney injury after femoral neck fracture in elderly patients: a retrospective case-control study. BMC Musculoskelet Disord. 2022;23(1):7. doi:10.1186/s12891-021-04966-3
15. Agar A, Gulabi D, Sahin A, et al. Acute kidney injury after hip fracture surgery in patients over 80 years of age. Arch Orthop Trauma Surg. 2021. doi:10.1007/s00402-021-03969-y
16. Pedersen AB, Gammelager H, Kahlert J, Sørensen HT, Christiansen CF. Impact of body mass index on risk of acute kidney injury and mortality in elderly patients undergoing hip fracture surgery. Osteoporos Int. 2017;28(3):1087–1097. doi:10.1007/s00198-016-3836-8
17. Chen Q, Zhang Y, Zhang M, Li Z, Liu J. Application of machine learning algorithms to predict acute kidney injury in elderly orthopedic postoperative patients. Clin Interv Aging. 2022;17:317–330. doi:10.2147/cia.S349978
18. Ko S, Jo C, Chang CB, et al. A web-based machine-learning algorithm predicting postoperative acute kidney injury after total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc. 2022;30(2):545–554. doi:10.1007/s00167-020-06258-0
19. Bell S, Dekker FW, Vadiveloo T, et al. Risk of postoperative acute kidney injury in patients undergoing orthopaedic surgery--development and validation of a risk score and effect of acute kidney injury on survival: observational cohort study. BMJ. 2015;351(nov11 19):h5639. doi:10.1136/bmj.h5639
20. Yu Y, Zhang C, Zhang F, et al. Development and validation of a risk nomogram for postoperative acute kidney injury in older patients undergoing liver resection: a pilot study. BMC Anesthesiol. 2022;22(1):22. doi:10.1186/s12871-022-01566-z
21. Wang J, Yu C, Zhang Y, Huang Y, Prediction A. Model for acute kidney injury after pericardiectomy: an observational study. Front Cardiovasc Med. 2022;9:790044. doi:10.3389/fcvm.2022.790044
22. Ruiz-Ortega M, Rayego-Mateos S, Lamas S, Ortiz A, Rodrigues-Diez RR. Targeting the progression of chronic kidney disease. Nat Rev Nephrol. 2020;16(5):269–288. doi:10.1038/s41581-019-0248-y
23. Fontecha-Barriuso M, Lopez-Diaz AM, Guerrero-Mauvecin J, et al. Tubular mitochondrial dysfunction, oxidative stress, and progression of chronic kidney disease. Antioxidants. 2022;11:7. doi:10.3390/antiox11071356
24. Chan JJ, Robinson J, Poeran J, Huang HH, Moucha CS, Chen DD. Antibiotic-loaded bone cement in primary total knee arthroplasty: utilization patterns and impact on complications using a national database. J Arthroplasty. 2019;34(7s):S188–S94.e1. doi:10.1016/j.arth.2019.03.006
25. Salmasi V, Maheshwari K, Yang D, et al. Relationship between intraoperative hypotension, defined by either reduction from baseline or absolute thresholds, and acute kidney and myocardial injury after noncardiac surgery: a retrospective cohort analysis. Anesthesiology. 2017;126(1):47–65. doi:10.1097/aln.0000000000001432
26. Jang WY, Jung JK, Lee DK, Han SB. Intraoperative hypotension is a risk factor for postoperative acute kidney injury after femoral neck fracture surgery: a retrospective study. BMC Musculoskelet Disord. 2019;20(1):131. doi:10.1186/s12891-019-2496-1
27. Braüner Christensen J, Aasbrenn M, Sandoval Castillo L, et al. Predictors of acute kidney injury after hip fracture in older adults. Geriatr Orthop Surg Rehabil. 2020;11:2151459320920088. doi:10.1177/2151459320920088
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

