Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 16
More Physical Exercise is Required for Overweight or Obese Women with Gestational Diabetes Mellitus to Achieve Good Plasma Glucose Control During Pregnancy: Finding from a Prospective Cohort in Shanghai
Authors Gao X , Zhang X, Kuai L, Yang Q, Li H, Zhang R, Li B, Wang R
Received 7 September 2023
Accepted for publication 29 November 2023
Published 5 December 2023 Volume 2023:16 Pages 3925—3935
DOI https://doi.org/10.2147/DMSO.S439106
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 4
Editor who approved publication: Dr Konstantinos Tziomalos
Xiangjin Gao,1,2,* Xiuqi Zhang,1,* Le Kuai,3,* Qing Yang,4 Huan Li,4 Rui Zhang,1 Bin Li,1 Ruiping Wang1,2
1Clinical Research Center, Shanghai Skin Diseases Hospital, Medical School of Tongji University, Shanghai, People’s Republic of China; 2School of Public Health, Shanghai University of Traditional Chinese Medicine, Shanghai, People’s Republic of China; 3Yueyang Hospital, Shanghai University of Traditional Chinese Medicine, Shanghai, People’s Republic of China; 4Obstetrics and Gynecology Department, Songjiang Maternal and Child Health-Care Hospital, Shanghai, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Ruiping Wang, Clinical Research Center, Shanghai Skin Diseases Hospital, Medical School of Tongji University, 1278 Baode Road, Jing’an District, Shanghai, 200443, People’s Republic of China, Tel +86-189 1879 1651, Fax +86-21-3680 3000, Email [email protected]
Objective: This study was based on a gestational diabetes mellitus (GDM) cohort in Shanghai to examine the association between physical exercise and plasma glucose control among GDM women with and determine what the effects of pre-pregnancy body mass index (BMI).
Methods: In this study, GDM was diagnosed if the plasma glucose values at any of the following time points reached the diagnostic threshold: fasting blood glucose (5.1 mmol/L), 1-hour blood glucose (10.0 mmol/L), and 2-hour blood glucose (8.5 mmol/L) by 75 g oral glucose tolerance test (OGTT). Information on GDM women was extracted from the hospital’s health records and prenatal examination forms and was obtained through face-to-face interviews after delivery. A restricted cubic spline curve with four knots was used to flexibly model the relationship between the duration of moderate-intensity physical exercise and the percentage of abnormal plasma glucose among GDM patients with different BMI values. In this study, a P-value less than 0.05 (two-tailed) was considered as statistical significance.
Results: Among 1139 GDM women with GDM, the median percentage of abnormal plasma glucose (PG) was 40.0% (interquartile range (IQR): 20.0– 66.7%), and the difference between overweight-obese group and underweight-normal group was statistically significant (50.0% vs 40.0%, P < 0.001). In this study, engaging in more physical exercise during pregnancy contributed to a higher prevalence of satisfactory glycemic control, and women with BMI < 25 kg/m2 should engage in no less than 90 minutes of moderate-intensity physical activity per day to achieve satisfactory glycemic control (prevalence of abnormal PG < 35%). However, over 120 minutes of daily moderate-intensity physical activity is required for GDM women with a BMI ≥ 25 kg/m2 to achieve satisfactory glycemic control.
Conclusion: Overweight or obese women with GDM have a higher risk of poor glycemic control and require a longer duration of physical exercise to achieve the same level of blood glucose control.
Keywords: gestational diabetes mellitus, plasma glucose control, physical exercise, overweight and obesity
Introduction
Gestational diabetes mellitus (GDM) is defined as any degree of abnormal plasma glucose tolerance that occurs during pregnancy.1,2 GDM not only leads to common complications such as macrosomia, fetal distress, and fetal malformation but also leads to long-term adverse pregnancy outcomes such as cardiovascular disease, metabolic syndrome and diabetes mellitus type 2.3,4 Therefore, effective management of GDM is urgently needed to avoid severe adverse pregnancy outcomes.5
Diabetes mellitus is a naturally occurring, chronic, low-grade inflammatory disease characterized by the activation of the immune system. Additionally, some scholars propose that obesity itself constitutes a mild systemic inflammatory disease.6 Previous researches have indicated that pregnant women who are overweight or obese have a higher chance of suffering from gestational diabetes mellitus and poor plasma glucose control.7,8 A study indicated that pregnant women with a pre-pregnancy body mass index (BMI) exceeded 25.0 kg/m2 had higher GDM incidence compared to those with pre-pregnancy BMI between 18.0 and 22.9 kg/m2.9 Physical exercise has been proven to be an effective intervention measure in preventing gestational diabetes mellitus, stabilizing gestational blood glucose and reducing adverse pregnancy outcomes.10,11 However, evidence regarding the appropriate levels of physical activity for GDM women across different BMI levels is limited, especially in China. The significance of this study lies in its ability to offer valuable guidance regarding physical exercise in women with GDM at different BMI levels.
We implemented this descriptive study based on a cohort of women with GDM in Shanghai to ascertain the characteristics of GDM patients, examine the relationship between physical exercise and glycemic control, and explore any differences caused by pre-pregnancy BMI on the association between physical exercise time and plasma glucose control. We hypothesized that overweight or obese women have a higher risk of poor plasma glucose control and require longer physical exercise time to achieve the same level of glycemic control as underweight or normal weight GDM women.
Methods
Study Population
During 2019 and 2020, we established a prospective cohort of women with GDM to explore the influence of physical exercise on plasma glucose control during pregnancy and adverse pregnancy outcomes in Songjiang District, Shanghai, China. Detailed information regarding the sample size calculation is available in our previously published work.12 GDM women in this study were recruited from the Songjiang Maternal and Children’s Healthcare Hospital during their prenatal examination. The inclusion criteria were as follows: (1) age 18–45 years; (2) residence in Songjiang District without any migration plan in the next two years; (3) gestation of 24–28 weeks; (4) singleton pregnancy; (5) without preexisting diabetes history; (6) confirmed GDM diagnosis with 75 g oral glucose tolerance test (OGTT); and (7) ability to read and sign the informed consent form.12–14 GDM women taking drugs for carbohydrate metabolism during pregnancy were excluded. A total of 1139 pregnant woman with GDM were enrolled in this study. The Review Board of Songjiang Maternal and Children’s Healthcare Hospital approved this study (IRB#-2019-12-003). Informed consent was signed by each participant before the questionnaire interview. This study was conducted following the Helsinki Declaration and was registered in the Chinese Clinical Trial Registry (ChiCTR2000028832) (Figure 1).
 |
Figure 1 The technical flowchart of this study population. |
Data Collection
The present study used a questionnaire consisting of four distinct sections to gather data from all GDM women, which consisted of four distinct sections. Part A focused on demographic information including age, education level, occupation, residency status, and individual monthly income. Part B included details regarding pregnancy and childbirth history, diabetes history, pre-pregnancy height and weight, and information on routine antenatal checkups. Part C focused on data related to newborn delivery, including gestational age, mode of delivery, and adverse pregnancy outcomes. Part D sought to assess the frequency and duration of moderate-intensity physical exercise among women with GDM between the 27th and 40th week of gestation.12–14 Part D covered 20 types of physical exercise in pregnancy (walking, hand washing clothes, mopping the floor, cycling to work, swimming, climbing stairs, Tai Chi Boxing, Square dancing, soft gymnastics, practicing yoga, aerobic dancing, etc) (Supplementary Table). Data for GDM women in Parts A, B, and C were extracted directly from the health records and antenatal checkup tables of the hospital. Data in Part D were obtained through face-to-face interviews conducted by trained investigators with GDM women after delivery. Records with missing values were appropriately flagged and cross-referenced with original paper records. Each investigator underwent comprehensive and standardized training to ensure the accuracy of the collected data. It is important to note that all information within this cohort was denominated to ensure that it could not be linked to any particular individual.
Definition and Index Calculation
The diagnostic criteria for GDM were based on the International Association of Diabetes and Pregnancy Study Groups (IADPSG) standard. Specific standard are as follows: pregnant women during 24–28 weeks of gestation who have not been diagnosed with diabetes are measured by 75 g oral glucose tolerance test (OGTT), and GDM can be diagnosed when the blood glucose value at any of the following time points reaches the diagnostic threshold: the diagnostic threshold of fasting blood glucose, 1h blood glucose and 2h blood glucose is 5.1 mmol/L, 10.0 mmol/L and 8.5 mmol/L, respectively.15 During each regular antenatal checkup subsequent to the confirmation of GDM, an abnormal level of plasma glucose was identified as having a morning plasma glucose value of ≥5.10 mmol/L after fasting for a minimum of 10 hours, and a value of ≥8.5 mmol/L within 2 hours after consuming a standardized breakfast. The evaluation of glycemic control during pregnancy involved calculation of the percentage of abnormal blood glucose levels, which was determined by dividing the number of abnormal plasma glucose tests by the total number of plasma glucose tests conducted in each GDM woman. To evaluate plasma glucose control in this study, we defined the percentage of abnormal plasma glucose levels < 35% among GDM women as satisfactory glycemic control.
Pre-pregnancy BMI was calculated as weight (kg) divided by 2 times of height (m) and was then categorized as <25 kg/m2 (underweight or normal weight) and ≥25 kg/m2 (overweight or obese). Furthermore, we classified the age of GDM women into 18–25 years, 26–30 years, 31–35 years, 36–45 years. Education was recorded as the number of years of completed schooling and was categorized into 6–9 years (primary/junior high), 10–12 years (senior high), and >12 years (college and above). Individual monthly incomes were divided into three groups (≤5000 RMB, 5001–10,000 RMB, and >10,000 RMB). The amount of moderate-intensity (an intensity that increases breathing rate whilst still being able to hold a conversation) physical activity was evaluated based on reported total daily activity time. GDM women in this cohort were classified according to their total moderate-intensity physical activity time as “<30 min/day”, “30–59 min/day”, “60–89 min/day”, “90–119 min/day”, and “≥120 min/day”.
Statistical Analysis
The current study utilized SAS (version 9.4) and R software (version 4.3.0) for data analysis. The mean and standard deviation (SD) were used for normally distributed quantitative data, and the median and interquartile range (IQR) were employed for skewed quantitative data. Qualitative data are expressed as frequencies and percentages (%). To compare the differences between overweight-obese GDM women and underweight-normal GDM women with varying demographic characteristics, moderate-intensity physical activity, glucose control status, and adverse pregnancy outcomes, Student’s t-test, Mann–Whitney U-test, and Chi-square test were used, as appropriate. With the adjustment of potential confounding factors, Odds ratios (OR) and 95% confidence intervals (CI) were calculated to explore the association between physical exercise duration and satisfactory glycemic control among GDM women with pre-pregnant BMI <25 kg/m2 and ≥25 kg/m2, respectively. The potential confounding factors adjusted were identified by using the single factor logistic regression analysis. Restricted cubic spline curves with four knots were used to flexibly model the dose-response relationship between the duration of physical exercise and the percentage of abnormal plasma glucose among GDM patients with different BMI levels. In this study, a statistically significant P-value was considered as 0.05 (two-tailed) and lower.
Results
Characteristics of GDM Women
The 1139 GDM women included 336 local residents (32.1%) with an average age of 30.5 years (SD:4.3 years). The majority of GDM women had an education of college and above (60.3%), approximately three-quarters of GDM patients earned a monthly income over 5000 RMB, and 40.5% had a balanced diet with doctors’ suggestions. Table 1 indicates that women with a BMI of <25 kg/m2 had a lower proportion of advanced education than those with a BMI ≥ of 25 kg/m2 (P <0.001). As shown in Table 2, the median daily moderate-intensity physical exercise time in GDM patients was 65 minutes (IQR:45–90 min). The percentage of GDM women with daily moderate-intensity physical exercise times of <30, (30–59) min, (60–89) min, (90–119) min, and ≥120 min were 4.8%, 34.5%, 33.2%, 19.7%, and 7.8%, respectively. The difference in moderate-intensity physical exercise duration between GDM women with a BMI <25 kg/m2 and those with a BMI ≥ of 25 kg/m2 was not statistically significant. For types of physical activity during pregnancy, the median value was 3.0 (IQR:2.0–4.0), and the difference between GDM women with BMI <25 kg/m2 and those with BMI ≥25 kg/m2 was also not statistically significant (Table 2).
 |
Table 1 The Demographic Features Among Women with GDM (n = 1139) |
 |
Table 2 Moderate-Intensity Physical Exercise, Glucose Control, and Adverse Pregnancy Outcomes Status Among Women with GDM (n = 1139) |
Plasma Glucose Status and Adverse Pregnancy Outcomes Status Among GDM Women
The median number of antenatal checkup was 6.0 (IQR:5.0–7.0), and the difference between GDM women with BMI <25 kg/m2 and those with BMI ≥25 kg/m2 was not statistically significant. The median percentage of abnormal plasma glucose in 1139 GDM women was 40.0% (IQR:20.0%-66.7%), and the difference between GDM women with BMI <25 kg/m2 and those with BMI ≥25 kg/m2 was statistically significant (40.0% vs 50.0%, P <0.001). 50.6% of GDM women had satisfactory glycemic control during their pregnancy, the difference between GDM women with BMI <25 kg/m2 and those with BMI ≥25 kg/m2 was statistically significant (53.2% vs 42.9%, P =0.003). The median value of weight gain during gestation was 9.5 kg (IQR:7.0–12.3 kg). Table 2 indicates that overweight or obese women with GDM (BMI ≥25 kg/m2) had a higher proportion of adverse pregnancy outcomes than GDM women with underweight or normal weight (BMI <25 kg/m2) (36.2% vs 27.1%, P =0.003) (Table 2).
Association Between Physical Exercise Time and Plasma Glucose Control
GDM women with engaging in more physical exercise per day had a higher proportion of satisfactory glycemic control, and the difference was statistically significant for GDM women with a BMI ≥ of 25 kg/m2 (P =0.029) (Table 3). GDM women with engaging in more physical exercise per day had a lower proportion of adverse pregnancy outcomes, and the difference was statistically significant for GDM women with a BMI < of 25 kg/m2 (P =0.025) (Table 4). Figure 2 indicates that engaging in a longer duration of physical exercise per day during pregnancy contributes to a higher prevalence of satisfactory glycemic control (Figure 2).
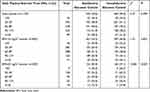 |
Table 3 Moderate-Intensity Physical Exercise Time Among GDM Women with Different Glucose Control Status (n = 1139) |
 |
Table 4 Moderate-Intensity Physical Exercise Time Among GDM Women with Different Pregnancy Outcome Status (n = 1139) |
In this study, the predicted percentage of abnormal plasma glucose increased gradually and was above 35% among GDM women when physical exercise time was <60 min/day, while it continuously decreased once physical exercise time exceeded 60 min/day. The percentage of abnormal plasma glucose was below 35% when physical exercise time was over 100 min/day (Figure 3A). Regarding the inverted U-shaped relationship between moderate-intensity physical exercise time and the predicted percentage of abnormal plasma glucose in GDM women with BMI <25 kg/m2 (Figure 3B), a substantial increase in the abnormal plasma glucose (PG) percentage was associated with more moderate-intensity physical exercise time within 60 min/day, and the percentage of abnormal PG decreased thereafter and reached a satisfactory glycemic control standard (<35%) until the daily physical exercise time was over 90 min. For GDM women with a BMI ≥ of 25 kg/m2, the percentage of abnormal PG decreased substantially with an increase in daily physical exercise time, which was initiated at a percentage of abnormal PG as high as 50%, and then reached a satisfactory glycemic control standard until the daily physical exercise time was over 120 min (Figure 3C). Therefore, overweight or obese women with GDM have a higher risk of poor plasma glucose control and require longer physical exercise to achieve the same level of glycemic control (Figure 3).
Discussion
GDM can have severe consequences if left unmanaged and is characterized by high blood glucose levels during pregnancy. The detrimental effects of GDM extend beyond the mother’s well-being; the developing fetus is also vulnerable to its adverse effects.16,17 In addition, the number of elderly pregnant women has rapidly increased with the implementation of the “3-child” policy, leading to a continuous increase in the prevalence of GDM in China.18,19 Therefore, it is crucial to address and mitigate the potential dangers associated with GDM to ensure the health of both mother and infant in China.20,21 In our previous research based on the GDM cohort, we observed a negative correlation between the duration of physical activity and the percentage of abnormal blood glucose levels in GDM women.12 Furthermore, we found that multiparous women had a lower efficacy in controlling blood glucose levels through physical exercise than primiparous women.13 In this study, is crucial to address and mitigate the potential dangers associated with GDM women with overweight or obesity to ensure the health of both mother and baby in pregnancy.
The present study employed restricted cubic splines to investigate the association between the prevalence of abnormal plasma glucose levels during pregnancy, varying BMI levels, and the duration of moderate-intensity physical activity among GDM patients. By fitting relevant models, regarding the inverted U-shaped relationship between moderate-intensity physical exercise time and the predicted percentage of abnormal plasma glucose in GDM women with underweight or normal weight, they would achieve satisfactory glycemic control if moderate-intensity physical activity exceeded 90 min/day. In addition, satisfactory glycemic control can be attained when daily physical activity is > 120 min among GDM women with overweight or obese. Therefore, overweight or obese women have a higher risk of poor plasma glucose control and require longer physical exercise times to achieve the same level of glycemic control. It is advisable for underweight or normal weight GDM women and overweight or obese GDM women to engage in at least 90 or 120 minutes of daily moderate-intensity physical exercise, respectively. In this study, we noticed that the predicted prevalence of abnormal plasma glucose among underweight or normal weight GDM women increased with more daily moderate-intensity physical activity time within 60 min. This may be attributed to the fact that GDM women with worse glycemic status are more likely to be advised by healthcare professionals to engage in physical activity; however, the amount of physical activity of less than 60 min/day remains insufficient to achieve individual glycemic control, which leads to a positive association between physical exercise time and the percentage of abnormal PG.
We discovered that, compared to women who were underweight or normal weight (46.8%), those who were overweight or obese had a higher incidence of abnormal plasma glucose levels during pregnancy (57.1%). The increased risk of poor glycemic control in overweight or obese women during the late stages of pregnancy may be attributed to the impact of overweight and obesity on the secretion of insulin antagonists, resulting in reduced insulin activity and consequently affecting blood glucose levels during pregnancy.22 Furthermore, GDM women with overweight or obesity have a higher risk of adverse pregnancy outcomes than women with underweight or normal weight in this study, consistent with previous studies from different countries and regions.23–25 In a meta-analysis conducted by Yu et al, it was observed that pregnant women with overweight or obesity prior to conception have a 1.67 times higher risk of delivering macrosomia infants compared to those with a normal pre-pregnancy BMI.26 We observed that engaging in physical exercise during pregnancy can contribute to a reduction in the incidence of abnormal plasma glucose levels during pregnancy among GDM women. Relevant research has shown that engaging in physical exercise during pregnancy can increase glucose transporter 4 levels in muscle cells, enhance insulin sensitivity, improve glucose utilization, and reduce insulin resistance, thereby fundamentally preventing and treating GDM. Through physical exercise, the glucose utilization rate of muscles increases, fat accumulation decreases and muscle mass increases. The increase of muscle mass helps to improve basal metabolic levels, and activating insulin-like enzymes and proteins, improving glucose uptake and utilization.27 Meanwhile, due to the significant association between obesity and GDM, engaging in physical activities can potentially mitigate the risk of abnormal plasma glucose levels by promoting weight loss among GDM women.
Compared to the recommendations of the American College of Obstetricians and Gynecologists (ACOG) and the Royal College of Obstetricians and Gynaecologists (RCOG) for pregnant women to engage in 150 min of moderate-intensity physical activity per week,28,29 the median value of moderate-intensity physical exercise time in this prospective cohort of GDM women was 65 min per day. Although the physical activity time for GDM women in this study exceeded that recommended by the RCOG, the effectiveness of glycemic control was still unsatisfactory. This may be attributed to the fact that GDM patients originally had poor blood glucose control, necessitating more physical activity to achieve the ideal glycemic control levels. Furthermore, this also may be related to the tendency of pregnant women to engage in low-intensity forms of exercise such as walking in China, because pregnancy is considered a special state that necessitates additional rest and nutritional supplementation in traditional Chinese beliefs.12 Additionally, this could also be associated with other factors such as racial differences, dietary structure, and living environment. Available research on the impact of physical exercise of diverse types, durations, and frequencies on the plasma glucose levels of pregnant women with different racial backgrounds, geographical locations, and characteristics is still limited. Further studies are necessary to provide appropriate sports guidance for pregnant women under different circumstances.
The major strength of the present study is that it was a prospective cohort study with a large population size of 1139 GDM women, based on real-world clinical data. Furthermore, this study conducted a quantitative assessment to determine the impact of BMI on the relationship between physical activity duration and glycemic control among GDM women based on this prospective cohort to offer valuable guidance regarding physical exercise for GDM women with different BMI levels. In addition, the potential recall bias and measurement bias in this study was substantially alleviated through direct extraction of information from routine prenatal examination forms and delivery records of GDM women in the hospital.
In this study, there are several limitations that need to be considered. Firstly, the data analyzed in this study were derived from a previously established GDM women cohort, and the sample size was not specifically calculated for the current study. Meanwhile, the sample size of pregnant GDM women with overweight or obese engaging in moderate-intensity physical activity for more than 120 minutes per day was limited in this study, which have potentially impacted the reliability of the research findings to some degree. Secondly, the data on physical exercise time in GDM women were collected through self-reported questionnaires interview, which might have induced reporting bias. Thirdly, this study only recruited GDM women from Shanghai, which may limit the generalizability of the study findings to different populations. Fourthly, not all potential confounding factors were collected, such as daily dietary information and other environmental factors, indicating that this study may not have all potential confounders well controlled. Future research should consider incorporating improvements in order to overcome these limitations.
Conclusion
GDM women who are overweight or obese have a higher risk of poor glycemic control and require a longer duration of physical exercise to achieve the same level of blood glucose control. It is advisable for overweight or obese women with GDM to engage in at least 120 min of daily physical exercise to achieve good glycemic control during pregnancy.
Data Sharing Statement
Raw data supporting the conclusions of this study will be made available upon request from the corresponding author.
Ethics Statement
Studies involving human participants were reviewed and approved by the Review Board of Songjiang Maternal and Children’s Healthcare Hospital (IRB#-2019-12-003). Informed consent was signed by each participant before the questionnaire interview.
Acknowledgments
We thank Michael Engelau from the Centers for Disease Control and Prevention and Los Angeles from the University of Sydney for providing suggestions and comments on this manuscript.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study was supported by grants from Intelligence Funds of Shanghai Skin Disease Hospital (2021KYQD01), Shanghai Talent Development Fund (2021073), Shanghai Shenkang Hospital Development Center Management Research Program (2020SKMR-32), and China Fund for Medical Equipment (IIT2022-01). The funder had no role in the study design, data collection and analysis, manuscript preparation, or publication decision.
Disclosure
The authors report no conflicts of interest in this work.
References
1. American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2013;36(Suppl 1):S67–S74. doi:10.2337/dc13-S067
2. Kim C. Gestational diabetes: risks, management, and treatment options. Int J Womens Health. 2010;2:339–351. doi:10.2147/IJWH.S13333
3. Sklempe Kokic I, Ivanisevic M, Biolo G, Simunic B, Kokic T, Pisot R. Combination of a structured aerobic and resistance exercise improves glycaemic control in pregnant women diagnosed with gestational diabetes mellitus. A randomised controlled trial. Women Birth. 2018;31(4):e232–e238. doi:10.1016/j.wombi.2017.10.004
4. Magon N, Seshiah V. Gestational diabetes mellitus: insulinic management. J Obstet Gynaecol India. 2014;64(2):82–90. doi:10.1007/s13224-014-0525-4
5. American Diabetes Association 14. Management of diabetes in pregnancy: standards of medical care in diabetes-2020. Diabetes Care. 2020;43(Suppl 1):S183–S192. doi:10.2337/dc20-S014
6. Pickup JC. Inflammation and activated innate immunity in the pathogenesis of type 2 diabetes. Diabetes Care. 2004;27(3):813–823. doi:10.2337/diacare.27.3.813
7. Carolan-Olah M, Steele C, Krenzin G. Development and initial testing of a GDM information website for multi-ethnic women with GDM. BMC Pregnancy Childbirth. 2015;15(1):145. doi:10.1186/s12884-015-0578-0
8. Hu G, Liu H, Leng J, et al. Effects of a lifestyle intervention in young women with gdm and subsequent diabetes. Nutrients. 2022;14(24):5232. doi:10.3390/nu14245232
9. Kim C. Gestational diabetes mellitus in Korean women: similarities and differences from other racial/ethnic groups. Diabetes Metab J. 2014;38(1):1–12. doi:10.4093/dmj.2014.38.1.1
10. Mottola MF, Artal R. Role of exercise in reducing gestational diabetes mellitus. Clin Obstet Gynecol. 2016;59(3):620–628. doi:10.1097/GRF.0000000000000211
11. Mottola MF, Davenport MH, Ruchat SM, et al. Canadian guideline for physical activity throughout pregnancy. Br J Sports Med. 2018;52(21):1339–1346. doi:10.1136/bjsports-2018-100056
12. Wang R, Yang Q, Sun T, et al. Physical exercise is associated with glycemic control among women with gestational diabetes mellitus: findings from a prospective cohort in Shanghai, China. Diabetes Metab Syndr Obes. 2021;14:1949–1961. doi:10.2147/DMSO.S308287
13. Wang R, Chen J, Yao F, et al. Number of parous events affects the association between physical exercise and glycemic control among women with gestational diabetes mellitus: a prospective cohort study. J Sport Health Sci. 2022;11(5):586–595. doi:10.1016/j.jshs.2022.03.005
14. Zhang R, Gao X, Sun T, et al. Longer physical exercise duration prevents abnormal fasting plasma glucose occurrences in the third trimester: findings from a cohort of women with gestational diabetes mellitus in Shanghai. Front Endocrinol. 2023;14:1054153. doi:10.3389/fendo.2023.1054153
15. Metzger BE, Gabbe SG, Persson B, et al., International Association of Diabetes and Pregnancy Study Groups Consensus Panel. International association of diabetes and pregnancy study groups recommendations on the diagnosis and classification of hyperglycemia in pregnancy. Diabetes Care. 2010;33(3):676–682. doi:10.2337/dc09-1848
16. Filardi T, Tavaglione F, Di Stasio M, Fazio V, Lenzi A, Morano S. Impact of risk factors for gestational diabetes (GDM) on pregnancy outcomes in women with GDM. J Endocrinol Invest. 2018;41(6):671–676. doi:10.1007/s40618-017-0791-y
17. Gao C, Sun X, Lu L, Liu F, Yuan J. Prevalence of gestational diabetes mellitus in mainland China: a systematic review and meta-analysis. J Diabetes Investig. 2019;10(1):154–162. doi:10.1111/jdi.12854
18. Gu C, Wang X, Zhang Z, et al. Pregnant women’s clinical characteristics, intrapartum interventions, and duration of labour in urban China: a multi-center cross-sectional study [published correction appears in BMC pregnancy childbirth. BMC Pregnancy Childbirth. 2020;20(1):386. doi:10.1186/s12884-020-03072-x
19. Zhang HX, Zhao YY, Wang YQ. Analysis of the characteristics of pregnancy and delivery before and after implementation of the two-child policy. Chin Med J. 2018;131(1):37–42. doi:10.4103/0366-6999.221268
20. González-Plaza E, Bellart J, Martínez-Verdú MÁ, Arranz Á, Luján-Barroso L, Seguranyes G. Pre-pregnancy overweight and obesity prevalence and relation to maternal and perinatal outcomes. Enferm Clin. 2022;32((Suppl 1)):S23–S30. doi:10.1016/j.enfcle.2021.04.006
21. Menting MD, van de Beek C, de Rooij SR, Painter RC, Vrijkotte TGM, Roseboom TJ. The association between pre-pregnancy overweight/obesity and offspring’s behavioral problems and executive functioning. Early Hum Dev. 2018;122:32–41. doi:10.1016/j.earlhumdev.2018.05.009
22. Liu L, Hong Z, Zhang L. Associations of prepregnancy body mass index and gestational weight gain with pregnancy outcomes in nulliparous women delivering single live babies. Sci Rep. 2015;5(1):12863. doi:10.1038/srep12863
23. Song Z, Cheng Y, Li T, Fan Y, Zhang Q, Cheng H. Effects of obesity indices/GDM on the pregnancy outcomes in Chinese women: a retrospective cohort study. Front Endocrinol. 2022;13:1029978. doi:10.3389/fendo.2022.1029978
24. Mistry SK, Das Gupta R, Alam S, Kaur K, Shamim AA, Puthussery S. Gestational diabetes mellitus (GDM) and adverse pregnancy outcome in South Asia: a systematic review. Endocrinol Diabetes Metab. 2021;4(4):e00285. doi:10.1002/edm2.285
25. Yu Z, Han S, Zhu J, Sun X, Ji C, Guo X. Pre-pregnancy body mass index in relation to infant birth weight and offspring overweight/obesity: a systematic review and meta-analysis. PLoS One. 2013;8(4):e61627. doi:10.1371/journal.pone.0061627
26. Wang C, Guelfi KJ, Yang HX. Exercise and its role in gestational diabetes mellitus. Chronic Dis Transl Med. 2016;2(4):208–214. doi:10.1016/j.cdtm.2016.11.006
27. Alwash SM, McIntyre HD, Mamun A. The association of general obesity, central obesity and visceral body fat with the risk of gestational diabetes mellitus: evidence from a systematic review and meta-analysis. Obes Res Clin Pract. 2021;15(5):425–430. doi:10.1016/j.orcp.2021.07.005
28. ACOG Committee Opinion No. 650. Physical activity and exercise during pregnancy and the postpartum period. Obstet Gynecol. 2015;126(6):e135–e142. doi:10.1097/AOG.0000000000001214
29. Royal College of Obstetricians and Gynaecologists. Physical activity and pregnancy [EB/OL]. Available form: https://www.rcog.org.uk/for-the-public/browse-our-patient-information/physical-activity-and-pregnancy/.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


