Back to Journals » Journal of Pain Research » Volume 17
Knowledge Mapping Analysis of Research on Pregnancy-Related Pelvic Girdle Pain (PPGP) from 2002 to 2022 Using Bibliometrics
Authors Xu L, Li Y, He Y, Chen M, Zhang Y, Liu C, Zhang L
Received 6 September 2023
Accepted for publication 30 January 2024
Published 13 February 2024 Volume 2024:17 Pages 643—666
DOI https://doi.org/10.2147/JPR.S431438
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Alaa Abd-Elsayed
Linli Xu,1,* Yuanchao Li,2,* Yanan He,2,* Mengtong Chen,2 Yuting Zhang,2 Chunlong Liu,2 Li Zhang1
1Department of Obstetrics, Guangdong Women and Children Hospital, Guangzhou, Guangdong Province, People’s Republic of China; 2Clinical College of Acupuncture, Moxibustion, and Rehabilitation, Guangzhou University of Chinese Medicine, Guangzhou, Guangdong Province, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Li Zhang, Department of Obstetrics, Guangdong Provincial Maternal and Child Health Care Hospital, Guangzhou, Guangdong Province, People’s Republic of China, Tel +8613432213940, Email [email protected]
Background: Pregnancy-related Pelvic Girdle Pain (PPGP) is a prevalent condition characterized by various physiological and pathological processes in the female body. The objective of this study is to offer a comprehensive understanding of the current research landscape, key areas of interest, and potential future directions in the field of PPGP.
Methods: Using Web of Science, we explored PPGP literature from 2002 to 2022. VOSviewer and CiteSpace facilitated a quantitative analysis, revealing co-authorship patterns, co-occurring themes, citations, and co-citations.
Results: We identified, peaking at 99 publications in 2021. The United States led with 138 publications and the highest citation count (3160). The Karolinska Institute boasted the highest tally of publications (n = 21). Regarding the volume of publications, the esteemed journal of BMC Pregnancy and Childbirth attained the foremost position. Notably, Gutke, Annelie emerged as the most prolific and highly cited author. The analysis of keyword co-occurrence and co-citation clustering unveiled an intricate tapestry of PPGP studies, spanning various domains including risk factors, mechanistic intricacies, diagnostic benchmark, treatment modalities, and far-reaching ramifications on one’s quality of life.
Conclusion: Research endeavors exploring PPGP have unveiled an enduring trajectory of growth in contemporary times. The existing body of research primarily focuses on delving into the intricate interplay of epidemiological factors and the profound implications of interventions encompassing physical therapy, exercise protocols, and diverse modes of pain management within the domain of PPGP. Multidisciplinary integration encapsulates a prevailing trajectory of progress within this domain, while the focal point of future inquiries into PPGP may revolve around subjects pertaining to standardized outcome reporting.
Keywords: pregnancy-related pelvic girdle pain, bibliometric analysis, CiteSpace, VOSviewer, therapeutic
Corrigendum for this paper has been published.
Introduction
One of the prevailing musculoskeletal afflictions encountered during the gestational and postnatal periods is the insidious onset of pelvic girdle pain (PGP), alternatively known as pregnancy-related pelvic girdle pain (PPGP). This condition exerts its grip on a appreciable cohort of women, casting profound and enduring ramifications on their quality of life.1,2 In recent times, there has been an increase in research pertaining to PPGP, reflecting a recognition of the need to better understand the risk factors,3 predictors,4 and effective treatments5 for this condition. A body of research refers to PPGP, which signifies pain or discomfort experienced within the pelvic region during both pregnancy and the postpartum period. The pain is usually felt between the gluteal sulcus and the posterior iliac spine, particularly near the sacroiliac joint (SIJ).2 Occasionally, the pain may radiate to the back of the thigh, either on its own or in combination with the joint.1,2 It can also affect the pubic symphysis, or the hip joint.1,3,6 PPGP can be experienced as a dull ache, sharp pain, or grinding sensation, and it can range from mild to severe and decreased tolerance for prolonged standing, sitting, or walking.2,7 Studies have shown that Women afflicted with pregnancy-related pelvic girdle pain are predisposed to encountering states of despondency, apprehension, and perturbations in their sleep patterns,8 and are also at higher risk of having a caesarean delivery.6 This has led to an increased focus on preventing and alleviating pelvic discomfort during pregnancy.
There is a growing recognition of the crucial role that physiotherapy plays in managing pregnancy-related pelvic discomfort.3 Various healthcare professionals, including physiotherapists, chiropractors, occupational therapists (OTs), medical doctors (MDs), and nurses/NPs, play a crucial role in managing pregnancy-related pelvic discomfort. Physical therapy interventions, such as pelvic floor muscle training and manual therapy, have shown efficacy in mitigating pain and improving functionality among expectant mothers.9 Additionally, a growing body of evidence highlights the impact of lifestyle factors, such as obesity and sedentary behavior, on the development of pregnancy-related pelvic pain. This has prompted an increased emphasis on promoting healthy lifestyle habits, including exercise, among pregnant women to prevent and manage pelvic pain.5 Despite these advancements, little attention has been given to exploring hot spots and trends in PPGP. Bibliometric analysis is a method used to quantitatively and qualitatively assess scholarly literature.10 It involves statistical analysis to extract measurable data from published research studies, providing insights into how knowledge is disseminated and used within publications. This approach helps objectively measure the impact of scholarly work, assessing factors like citations, collaborative efforts among authors, institutions, and countries, as well as the contributions of journals and authors within a specific field.11 In this study, a bibliometric analysis of PPGP publications from 2002 to 2022 is presented. The aim of the current study is to examine prevalent subject trends and focal points within the literature on pregnancy-related pelvic girdle pain (PPGP). Specifically, we explore the quantity of publications, countries, institutions, authors, journals, and keywords associated with PPGP. The ultimate objective of the analysis is to provide guidance for future research endeavors.
Materials and Methods
Data Acquisition and Retrieval Strategy
The search for publications related to pregnancy-related pelvic girdle pain (PPGP) was conducted using the Web of Science (WoS) repository. On January 18, 2023, the search strategy was executed by LLX and YCL. WoS, a widely recognized repository, was chosen for its comprehensive coverage of scholarly literature.
The specified search terms included variations of “pelvic girdle pain”, “PGP”, “symphysis pubis dysfunction”, “SPD”, “pelvic Instability”, “pelvic Joint Instability”, “pregnancy-related pelvic pain”, “sacroiliac joint dysfunction”, “pregnancy pelvic pain”, “low back pain” along with relevant terms like “postpartum period”, “after delivery”, “after childbirth”, “pregnancy”, “gestation”, “maternity”. The search encompassed the extensive WoS Core Collection, including SCI-EXPANDED, with no language restrictions applied. Within the WoS Core Collection, we specifically included SCI-EXPANDED, which stands for Science Citation Index Expanded. SCI-EXPANDED is a citation index within the Web of Science that covers a wide range of scientific disciplines, including life sciences, physical sciences, health sciences, and more. It includes a vast collection of high-impact journals and provides valuable citation information for the articles indexed. Importantly, there were no language limitations imposed during the search, ensuring inclusivity of relevant literature regardless of the language of publication. Articles were identified from January 1, 2002, to December 31, 2022, based on the relevance of titles and abstracts to the study’s focus on PPGP.
Inclusion criteria comprised articles addressing pregnancy-related pelvic girdle pain (PPGP), available in the English language, and conducted between January 1, 2002, and December 31, 2022. Exclusion criteria included articles unrelated to PPGP, publications in languages other than English, and studies conducted outside the specified time frame. Subsequently, full-text screening was conducted to assess eligibility according to the established criteria. In cases of duplicate identification, only the most relevant and complete version of the publication was retained to eliminate redundant data.
Any discrepancies or uncertainties were resolved through team discussion. Ultimately, articles, including prospective studies and reviews, were retrieved and subjected to analysis. For the detailed search strategy, please refer to Appendix A. The seach process is shown in Figure 1.
 |
Figure 1 The flow chart of the screening process. |
Bibliometric Analysis and Visualization
This study aims to investigate national and institutional participation, annual production, publication numbers, journals, and research fields. The analysis will be conducted using the “Analyze Results” function within the Web of Science (WoS) database. In the process of classifying publications, each article within the dataset underwent a comprehensive assessment. This involved a meticulous review of titles and abstracts by the investigators to determine their appropriate classification. The assignment of “article” or “review” was based on a thorough examination of the content and scope of each publication, ensuring accurate categorization, then identified and verified in CiteSpace. Specifically, we will examine the extent of involvement at the national and institutional levels, assess annual research output, quantify the number of publications, identify relevant journals, and categorize the research fields. The “Analyze Results” function in the WoS database will serve as a tool for extracting and processing this information.
In addition, this study examines publication trends over time. Analyses performed using the curve fitting function in IBM SPSS Statistics 22.0 software indicated statistical significance with a two-tailed p-value < 0.05. Journal impact factors and category quartiles were extracted from the 2021 Journal Citation Report. The bibliometrics package in R 4.1.2 was used to analyze the publications from a bibliometric point of view, examining their distribution by country, annual production and citations.
Microsoft Excel 2016 served as the medium for data management. In this scholarly investigation, we conducted meticulous bibliometric and visualization analyses employing two eminent software tools - VOSviewer and CiteSpace. The data obtained from the Web of Science (WoS) was transformed into a txt format to facilitate advanced analysis.
Leveraging tools such as VOSviewer and CiteSpace, we employ visual representations for the analysis of Citation Patterns and Network Relationships, Thematic Analysis, Keyword Co-occurrence, and Identification of Citation Bursts and Trends. VOSviewer was instrumental in scrutinizing the citation patterns of publications, the co-citation relationships among countries, institutions, and authors, as well as the co-citation of authors, journals, and references. The construction of a biplot overlay of journals using CiteSpace allowed for an in-depth examination of the co-occurrence of keywords. Moreover, the identification of references and keywords displaying notable citation bursts was performed by using CiteSpace to efficiently perform cluster analyses of co-cited references and keywords.11
In the visual representations of VOSviewer, an assortment of nodes represents countries, institutions, journals, authors, references, and keywords.10 The size of each node signifies the occurrence of publications, citations, or frequency. The connecting lines, varying in thickness, depict the strength of these collaborations. Distinct hues are employed to indicate clustering or the average year of occurrence, while the thickness of the connecting lines reflects the strength of the links between the nodes. The settings for CiteSpace are configured as follows: time periods (2002–2022), one year allotted for each period, inclusion of all available sources, examination of one node type at a time, establishment of links based on the cosine strength within their respective time periods, selection criteria based on the g index with a value of k=5, pruning executed using pathfinder algorithms, and presentation facilitated through a static clustering view that showcases merged networks. The link retention factor was set to 3, the look back period was established as 5 years, the value of “e” for top N was designated as 1, and the minimum duration for keywords was set at 2, while the minimum duration for references was established at 5.
Results
Global Publication Trend
This study identified 719 publications related to PPGP. Of the 719 publications, 609 were classified as “articles”, and the remaining 110 were categorized as “reviews”. During the period spanning from 2002 to 2022, the magnitude of publications exhibits minimal annual fluctuations, albeit reflecting an overarching pattern of gradual expansion (see Figure 2). The yearly progress pattern corresponded harmoniously with the curve-fitting equation of y = 8.7219e°.1034x (R2 = 0.8573) (Figure 2), indicating a gradual increase in the attention paid to PPGP by scholars and suggesting that it may become a long-term research focus.
Distribution of Countries and Institutions
The United States had the highest output, publishing 138 papers, equivalent to 19.19% followed by Sweden, China, Australia, and England followed with 76, 59, 48, and 46 publications, respectively Table 1 (Part A).
 |
Table 1 The Top 10 Nations and Academic Organizations with the Highest Number of Publications in the Domain of PPGP |
As illustrated in Figure 3A, PPGP research has been distributed in 73 countries globally. The distribution of citations ranged from 329 to 3160 cumulative citations, with the United States, Sweden, and the Netherlands obtaining the highest citations (Figure 3B), each securing commendable standings with citation numbers of 1899, 1666, 1629, and 1615, as demonstrated in Figure 3B. Figure 4A illustrates collaborations among nations, each represented by nodes with sizes corresponding to the number of publications exceeding 15. The connecting lines, varying in thickness, depict the strength of these collaborations. In terms of comprehensive link strength, the United States demonstrates its preeminence by achieving an exceptional total of 59 instances, thereby capturing the attention of observers. Likewise, England attains the second position, showcasing a noteworthy total of 48 link strengths. Subsequently, Australia, Canada, and Sweden occupy the third to fifth positions, showcasing respective link strengths of 44, 42, and 35. This substantiates their scholarly influence.
 |
Figure 3 Countries involved in PPGP: (A) A cartographic representation of global country distribution within this domain (B) The top ten countries with the highest aggregate citation count. |
A total of 1224 academic institutions participated in this field of study. The top ten institutions are detailed in Table 1 (Part B). The Karolinska Institute in Sweden led with 21 publications (2.92% of total). Following were the University of Oslo, Oslo University Hospital, University of Gothenburg, and Sahlgrens University Hospital with 19, 15, 15, and 14 publications. Figure 4B illustrates collaborations among 80 institutions with over 3 publications. After excluding 21 unrelated entries, a co-authorship network among 50 institutions emerged. The Oslo University Hospital stood out with a total link strength of 33 instances. The University of Oslo followed with 30 instances, the Akershus University Hospital with 27, the Karolinska Institute with 24, and the Queens University with 23. We identified the 28 institutions with the most published papers and analysed their average year of publication. Figure 4C illustrates that the majority of these institutions published papers prior to 2019, as indicated by the purple or blue bars. The Vrije University Amsterdam had the earliest average year of publication at 2011.67. In contrast, the Medical University of Warsaw demonstrated temporal currency, boasting the most recent average year of publication at 2021.00.
Analysis of Journals and Research Areas
Since 2002, scholarly discourse has witnessed the emergence of a notable compilation comprising 719 articles dispersed across 340 journals. Table 2 enshrines the top 10 journals distinguished by the highest volume of published articles. BMC Pregnancy and Childbirth claimed the foremost position with 24 publications (3.34% of total articles), followed by Acta obstetrics et gynecologica Scandinavica (19 publications, 2.64%), European Spine Journal (16, 2.23%), Spine (15, 2.09%), and PLoS One (12, 1.67%). Our comprehensive analysis encompassed 20 erudite journals, each accruing no fewer than 150 co-citations, as visually depicted in Figure 5A. Table 2 unfolds an exquisite tableau of scholarly brilliance, revealing the top 10 co-cited journals that have contributed significantly to the scholarly The discerned publications were categorized into 55 distinct research domains. As delineated in Table 3, Obstetrics Gynecology emerges as the predominant domain, encompassing 196 esteemed records, accounting for 27.18% of all articles. General Internal Medicine follows closely with 93 significant contributions (12.89%), while Rehabilitation showcases 84 esteemed works (11.65%). Employing a dual-map system, we analyzed the interplay between subject categories in citing and cited journals. A spline wave elegantly traverses the display, depicting citation pathways, illuminating the intricate connections that bind diverse research areas and showcasing intellectual interconnectedness vividly. Two pivotal citation pathways stand out prominently in verdant green and delicate pink hues. The verdant green pathway signifies the tendency of papers in Health/Nursing/Medicine to frequently cite works from Neurology/Sports/Ophthalmology domains. Conversely, the delicate pink pathway illustrates the inclination of papers from Health/Nursing/Medicine journals to predominantly reference works in Medicine/Medical/Clinical spheres (Figure 5B).
 |
Figure 5 Analysis of journals (A) Articles published in various scholarly journals on PPGPs (B) Network visualization of journals that have been co-cited in more than 150 publications. |
 |
Table 2 The Top 10 Highly Influential Journals and Co-Cited Journals |
 |
Table 3 The Top 10 Prominent Research Domains |
Analysis of Authors
Table 4 presents a cohort of twelve authors known for their extensive publications and citations. Annelie Gutke, affiliated with the University of Gothenburg, emerges as the most productive scholar within this group, contributing 16 articles. Following closely are Britt Stuge from Oslo University Hospital with 15 articles and Per Kristiansson from the Center for Postgraduate Medical Education in Warsaw, Poland, with 10 articles. In terms of citations, Annelie Gutke also claims the top position with 472, followed by Kari Bo from the University of Torino with 391 and Britt Stuge from Oslo University Hospital with 372. The substantial number of publications and citations for Gutke underscores her prominence as the most active scholar in the field, making significant contributions to the academic discourse.
 |
Table 4 The Top 12 Prolific Authors with the Highest Number of Publications and Citations in PGPP Research |
We have systematically identified a group of 85 authors who have collaboratively contributed to a substantial number of publications. In pursuit of scholarly precision, we excluded 41 diverse contributions, focusing exclusively on the synergistic collaborations within a selected cohort of 44 authors (Figure 6A). Annelie Gutke (27 instances), Britt Stuge (27 instances), Per Kristiansson (24 instances), Francesca Wuytack (20 instances), and Birgitta Oberg (20 instances) exhibit the highest total link strength among the authors. Figure 6B illustrates the interconnected co-citation relationships within a distinct group of 21 authors, each having received no fewer than 50 citations. Hans-Christian Ostgaard leads with 340 citations, followed by Annelie Gutke (258), IM Mogren (195), Andry PPGP can be experienced in various ways, including pain between the posterior iliac crest and the gluteal fold, particularly in the vicinity of the sacroiliac joint (SIJ). This pain may also radiate to the posterior thigh and may occur in conjunction with or separately in the symphysis (176), Britt Stuge (165), and Helen Elden (130).
Citation and Co-Citation Analyses
In this research domain, we identified 82 articles garnering over 50 citations. After excluding 43 unrelated items, Figure 7A illustrates the collaborations among 39 articles. The pinnacle of scholarly impact is revealed by the enumeration of the ten most cited documents, as presented in Table 5. “Physical Activity and Exercise During Pregnancy and the Postpartum Period” leads with 508 citations, followed by “Pregnancy-related pelvic girdle pain (PPP), I: Terminology, clinical presentation, and prevalence” with 302 citations, and “The Efficacy of a Treatment Program Focusing on Specific Stabilizing Exercises for Pelvic Girdle Pain After Pregnancy: A Randomized Controlled Trial” with 201 citations. To delve deeper into the complexities of co-citation interconnections, we conducted a detailed examination of a subset of 30 reference, distinguished by being co-cited in no fewer than 30 citations. This analysis was executed using VOSviewer, as illustrated in Figure 7B. Spotlighting scholarly prominence, Table 6 reveals the platform occupied by eleven prominent references, led by the top five authors: Vleeming A (2008, 117 citations), W H Wu (2004, 107 citations), H Albert (2001, 85 citations), Lotta Norén (2002, 75 citations), and H C Ostgaard (2002, 75 citations). The co-cited references were intricately clustered based on indexing terms, resulting in a constellation of nine clusters (Figure 7C): predictors, postpartum period, low back pain, diastasis, prognostic factors, pain management, pelvic floor disorders, effectiveness, and sacroiliac joint.
 |
Table 5 The Top 10 Scholarly Articles with the Highest Number of Citations in the Domain of PGPP |
 |
Table 6 The Co-Citation Analysis of the Top Ten Cited References Within the Field of PGPP |
Ultimately, the top 25 references, characterized by notable citation bursts, are elegantly depicted in Figure 7D. The article “Pregnancy-related pelvic girdle pain (PPP), I: Terminology, clinical presentation, and prevalence”, published in 2004, secured the first position with a strength of 10.68. Furthermore, sustained citation cascades originating from the scholarly contributions of Sperstad JB and Virgara R have enriched the academic landscape, spanning the years from 2020 to 2022.
Co-Occurrence Analysis of Keywords
The VOSviewer was employed for a meticulous examination of keywords prevalent in scientific publications, surpassing a frequency threshold of fifteen occurrences. A total of 54 keywords were identified, with the top five, ranked by frequency, being pregnancy (363), low back pain (208), pelvic girdle pain (193), postpartum (181), and prevalence (154), as illustrated in Figure 8A. Figure 8B graphically represents the average year of publication for these keywords in a chronological progression from dark blue to light yellow. Notably, terms such as distance, ending, postpartum women, and lumbopelvic pain are recent, predominantly appearing in publications from 2019 onwards, while the majority were published before 2018. The temporal progression of keyword clusters is visually portrayed in the esteemed Figure 8C. In total, 11 clusters were identified, including quality of life, lactation, axial spondyloarthritis, low back pain, back pain, pelvic girdle pain, pelvic pain, electromyography, distance, and first-time mother.
CiteSpace was used for the detection of keyword bursts and the minimum duration of a burst was 2 years. The fragmented azure lines symbolize the chronology, wherein every diminutive cobalt rectangle signifies a span of 1 year, while the crimson section of the chronology betokens the duration of the keyword’s burst. Figure 9 showcases the top 15 keywords, distinguished by their utmost burst strength, with the most intense keyword being therapy (strength = 4.68), followed by population (4.48) and complication (4). The keyword “cesarean section” exhibited the lengthiest period of burst activity, spanning a five-year duration from 2012 to 2017. Importantly, the keyword “outcome” and “questionnaire” had a recent surge in citations, suggesting that questionnaire and outcomes might be a research hotspot in the future.
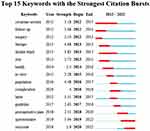 |
Figure 9 The top 15 keywords exhibiting the most pronounced citation bursts as determined by CiteSpace. |
Discussion
In this scholarly endeavor, we embarked upon an all-encompassing bibliometric analysis of the corpus pertaining to PPGP published within the temporal confines spanning from 2002 to 2022. To unravel the intricate tapestry of information, We utilized advanced visual management tools, including VOSviewer and CiteSpace, to gain comprehensive insights into the evolutionary trajectory of the field. This involved a meticulous examination of the temporal and spatial distribution of scholarly endeavors, discerning contributions from nations, institutions, journals, authors, keywords, and research areas. Our analysis aimed to uncover potential future research hotspots, shedding light on shifts in research focus and providing guidance for future research efforts within the domain of PPGP.
Overview of the Development of PPGP in the Past 20 Years
We focused on the literature related to PPGP that was published as early as 2002 in this study, which marks the beginning of our time slice.17,27,28 Since 2018, the tally of annual scholarly publications within the domain of PPGP has experienced a precipitous surge, surmounting the threshold of 100 in the year 2021. In fact, the publications from the past three years make up 76.11% of all the articles identified in this study. This indicates that research in the field of PPGP is rapidly growing as an emerging area. Moreover, a predominant portion of the top 10 exceedingly active and extensively referenced journals within this sphere boasts impact factors surpassing the threshold of 5. This highlights the high academic value of the research being conducted in this field, as well as its wide recognition and impact.
In our analysis of publications in the field of PPGP, we found that BMC Pregnancy and Childbirth was the journal with the most published articles, while SPINE was the journal with the highest number of citations. This demonstrates the strong impact of SPINE in the categories of Medicine, Orthopedics, and Sports Medicine, as it ranked in the top quarter (Q1).
The United States took the lead in terms of national contributions to PPGP research with an unprecedented abundance of scholarly publications and citations worldwide. This highlights the significance of the US in the development and advancement of PPGP research.
We performed a thorough analysis of the mean citation count for countries exhibiting no fewer than 10 academic publications. The foremost three nations were the United States, Sweden, and the United Kingdom, receiving 3160, 1899, and 1666 citations, correspondingly. It’s worth mentioning that the Netherlands has the highest average cited volume at 50.90, indicating that the quality of PPGP-related research in the Netherlands is exceptional and has a lasting impact. Britain and Norway follow closely as the second and third highest average cited countries. The concentration of high-quality and influential research in Europe and the United States, as evidenced by these top cited countries, highlights the significance of PPGP research in these regions. However, the United States dominated this field, with a centrality score of 0.52 and a strength of collaboration of 59, outpacing all other countries. These findings indicate that a substantial quantity of publications does not necessarily correspond to scholarly impact and therefore, nations ought to strive towards fostering innovative and pioneering discoveries, rather than simply emulating prior breakthroughs.
When ranking research institutions according to academic achievements, eight out of the top 10 institutions (with ≥10 publications) are situated in Sweden and Norway. The Sahlgrenska University Hospital in Sweden takes the top spot with the most citations (804) and an early publication year.17
Influential Authors and Studies in the PPGP Research
Among authors contributing to the discourse on PPGP and PLBP, Annelie Gutke emerges prominently with a remarkable volume of publications (16) and citations (472). His highlights their significant contributions to the field. On the other hand, Britt Stuge has played a key role in promoting collaboration and cooperation in this field, leading to more in-depth and relevant research. Both authors have imparted exceptional contributions to the realm of PPGP. The authors Annelie Gutke and Britt Stuge have been actively producing research in the field of PPGP and PLBP from 2004 to 2021. Annelie Gutke, in particular, stands out with the publication of five relevant studies in 2021 and a total of 16 papers with 472 citations, elevating her to the pinnacle of productivity and garnering significant recognition in the field, she stands as the most prolific and extensively cited scholar. Britt Stuge, on the other hand, by fostering collaborative research endeavors and engendering a profound comprehension of the subject matter, substantial contributions have been engendered in the field. It is worth pointing out that before 2004, the classification of PPP (PGP in 2022) and pregnancy-related lower back pain (LBP) as lumbago and abdominal pain, was challenged by Wu WH, who argued that LBP and PPP were two distinct clinical entities.1 Nevertheless, Annelie Gutke and Britt Stuge have been dedicated to PGP research since an earlier stage compared to other researchers in the field.18,29 Their research focused primarily on the epidemiological characteristics of PPGP and identifying risk predictors of PPGP.29 And their research also delved into the long-term prediction of PPGP and the development and validation of preventive and management strategies based on risk factors.13,18 Britt Stuge conducted cohort studies that explored the characteristics of the PGP population and was the first to carry out clinical research on sports therapy, focusing on the development of treatment methods.30
In 2002, it was proposed that muscle dysfunction in the lower back and pelvic area may be the root cause of persistent postpartum back pain and pelvic pain (PPGP). The muscles responsible for maintaining stability in the pelvis, when not functioning properly, may lead to PPGP. This type of pelvic pain differs from other pelvic pains.17
In 2004, Wu and others standardized the term PGP and recognized it as a distinct clinical entity from lower back pain (LBP). This recognition led to increased recognition of the research value of PGP and the formation of a dedicated research field.1 It’s worth mentioning that the prevalence rate of Pregnancy-related pelvic girdle pain (PPGP) can vary significantly, with some studies suggesting that a proportion ranging from 15% to 50% of expectant mothers may encounter various manifestations of pelvic discomfort during the course of their pregnancy. In the postpartum population, the prevalence rate has been estimated to be 35.9%. Several risk factors have been identified that increase PGP prevalence. These include a previous history of low back pain, back or pelvic trauma, and high stress levels.31 However, a small portion of the PPGP population continues to experience chronic pelvic pain, which is associated with factors such as age, muscle function, and level of disability.32
Furthermore, Bo, Kristiansson, Eberhard-gran, Malin, and Wuytack, Francesca et al among others, have laid a robust groundwork for the nascent domain of PPGP.33–36 In 2007, a team from the University of Oslo Norwegian School of Sport Sciences Department of Obstetrics and Gynecology, led by Bo and Kari, showed that their 12-week group training program was effective in preventing or treating lumbago and abdominal pain during pregnancy. This definition of lumbago and abdominal pain includes PPGP.37 It is worth mentioning that Britt Stuge also reported on the epidemiology of PPGP in elite athletes, signaling the beginning of the subgrouping of PPGP epidemiological studies into specialized populations.38 The Sundsvall Hospital research team, led by Kristiansson Per, shifted their focus to studying the impact of long-lasting sacral lower back (Contains the area defined by PPGP latest) pain that starts during pregnancy in 2007.39 And suggested that increased oxygen uptake during pregnancy can have a mitigating effect on back pain intensity.34 And They forged an alliance with Eberhard-Gran Malin, united in their pursuit of studying PPGP, in the year 2017, concerned that progestogenic contraceptives may have potential effects on persistent pelvic girdle pain.40 Eberhard-Gran, Malin, in collaboration with Britt Stuge, conducted an international study in Nepal to investigate the epidemiology of PPGP. The results showed that the incidence and severity of PPGP were high among the population in Nepal.35 Professor Francesca Wuytack from the National University of Ireland Galway analyzed the healthcare seeking behavior of women with pelvic girdle pain. The findings underscored the significance of imparting appropriate knowledge and offering meticulous post-care to these women by practitioners in Maternity and Child Health. Furthermore, they accentuated the hurdles encountered by these women when seeking medical aid.41
In essence, the preliminary endeavors of these teams have established a firm groundwork for comprehending the epidemiological aspect of the PGP populace, identifying risk factors for severe and persistent symptoms, and informing the development of effective diagnostic and management strategies. Significantly, a close-knit collaboration exists among the authors in this field. Out of the 85 authors who have contributed with more than three publications, approximately half, that is 44 authors, have been able to establish interconnected collaborative networks. Nevertheless, within the nearly linear collaboration graph, the vast majority of scholars hail from Norway, and the cooperative efforts are primarily contained within the confines of the research team. Scholars hailing from diverse nations ought to enhance their collaboration, engage in the exchange of knowledge on advantageous platforms, share the advancements in their research endeavors, and foster synergistic advantages. These concerted efforts will pave the way for achieving technological innovation and significant breakthroughs in the clinical translation of PPGP. Notably, according to available studies, the epidemiology of PGP in Europe, America and Oceania has been well studied and PPGP affects 23–36% of women during pregnancy,41 10–30% after delivery, and up to 10 years after delivery.42
However, in the Asia-African-Latin American regions, due to differences in economy and medical level, the epidemiological survey of PPGP is not yet comprehensive and the incidence rate is low, with very few cross-national and regional cooperative studies. Countries in East Asia have conducted ongoing clinical investigations of the PGP population since 2012, which may be due to the 2012 PGP consensus that led to a surge in research worldwide. However, studies in Central Asia, South Asia, and Africa are very scarce, and investigations of PGP are rare or even absent, which is highly detrimental to the study of the epidemiology of PGP worldwide. However, obstetrics and gynecology workers in these regions have recently noticed this and have conducted a small amount of research in recent years,43 which is surprising.
The current emphasis on the therapeutic benefits of exercise and activity in reducing subjective pain and promoting functional remodeling was evident from citation analysis of publications and co-citation analysis of references. The study with the most citations, published by the American College of Obstetricians and Gynecologists in 2015 in the journal Obstetrics and Gynecology, recommended encouraging physical activity for women with uncomplicated pregnancy before, during, and after pregnancy.12 The publication authored by Wu et al, as the second most extensively cited reference, divulged the noteworthy finding that the discriminative potential of PPGP and PLBP is remarkably effective, and PPGP accounts for half of all pregnancy-related low back and leg pain.1 Meanwhile, 25% of pregnant women and 5% of postpartum women have PPGP symptoms that are so severe that they require medical assistance, emphasizing that PGP is an independent clinical entity that deserves to be taken seriously. It is recommended to use multivariate analysis to determine risk factors, laying the foundation and providing a rigorous methodology for future research on the prevalence, risk factors, and management measures of PPGP. Although there is limited evidence, postpartum exercise has a positive impact on preventing excessive weight gain and obesity, as well as improving symptoms and emotional states related to PPGP.44
Amidst the references bearing significant co-citations, greater emphasis was placed upon the examination of the frequency and determinants of PPGP, alongside the therapeutic capacity of exercise in mitigating PPGP. Hanne A proposes subgroups within pelvic girdle pain during pregnancy: sacroiliac joint separation, unilateral sacroiliac syndrome, and bilateral sacroiliac syndrome have good postpartum outcomes, while pelvic girdle syndrome has a poorer prognosis compared to the first three. In 2002, the association between the highest relative risk of chronic pain was linked to a high number of positive tests and a low activity index.21,45 In 2022, The Academy of Pelvic Health Physical Therapy (APHPT) has determined that the following factors may be linked to the development of PP-PGP: pain in the posterior pelvic area, discomfort while lying down and bearing weight, multiple pregnancies, cesarean delivery, symptoms of depression, elevated pre-pregnancy body mass index (BMI), work-related factors, and position during breastfeeding. It is important to carefully consider patient information regarding PPGP, as the underlying cause and progression of the condition are still not fully understood.46
It is noteworthy that the guidelines and statements issued by the Academy of Pelvic Health Physical Therapy (APHPT) under the purview of the American Physical Therapy Association (APTA) is widely acknowledged as the epitome of excellence in guiding clinical practice pertaining to the administration of PPGP. Moreover, an ascendant curiosity has been engendered in the realm of investigations concerning the enduring nature and far-reaching ramifications of pregnancy-related pelvic girdle pain (PPGP), as evidenced by high co-citation of references and strong citation bursts in recent years.42 Most of the long-term PPGP can apparently be early identified and predicted by a history of low back pain and positive pain provocation tests. Early recognition and personalized treatment intervention are emphasized as crucial for preventing long-term pain. A study by Virgara R highlights the importance of considering both the physical and mental health of women during the third trimester of pregnancy. The findings suggest that women with higher symptoms of depression and anxiety may experience a greater degree of functional disability related to their LBPP, highlighting the need for increased attention to both the physical symptoms of PGP and the psychological well-being of pregnant women.47
Research Hotspots and Future Trends
As exemplified in Table 5, PPGP encompasses a diverse array of research domains, converging to form a rich biopsychosocial medical paradigm predominantly centered around the field of epidemiology. The prevalence of Pregnancy-related Pelvic Girdle Pain (PPGP) varies greatly, ranging from 4% to 84%, due to the differences in definitions, diagnostic methods, and research designs.34 The main cause of this large variation is the lack of a standardized PPGP classification index and differing measurement methods, with some studies relying solely on self-reported measures and others incorporating clinical evaluations such as physical exams and imaging tests.48 After reviewing the literature, Vleeming et al found that the prevalence of PPGP during pregnancy was close to 20%,28 which provides strong evidence. However, there are notable geographical differences in the incidence and severity of PPGP, with most studies being conducted in Europe (Figure 3). It is important for all regions of the world to pay attention to PPGP research and establish standardized guidelines to reach a consensus on its prevalence.
Numerous factors have been discerned to bear an intimate association with PPGP, encompassing laborious occupational tasks (characterized by repeated torso torsions and flexions within each passing hour), a prior medical history of low back pain, pelvic belt discomfort, previous pelvic injury, and psychological anguish. Other factors, such as smoking during pregnancy, early menarche, body mass index, birth order, age, exercise level, work experience, job satisfaction, education level, and separation of the rectus abdominis, have shown conflicting results in the literature.3,6,31,49 Family history of PPGP has also been found to increase the risk,50 with women with a mother or sister who experienced lumbar and pelvic pain during pregnancy being at an increased risk. More recent studies have suggested that nausea and vomiting during pregnancy, sitting breastfeeding posture, and cesarean delivery may also increase the risk of postpartum PGP,14,51–53 but further research is needed. It is important to also consider the impact of maternal functional activities when studying the risk factors of PPGP.
Notably, the advent of sports biomechanics, orthopedics, and imaging has extended the boundaries of PPGP research, kindling heightened interdisciplinary collaborations.54–56 Within the realm of PPGP research, the exploration of therapeutic interventions in the form of exercise and physiotherapy has been fortified. In contrast to the prevalent occurrence of low back pain among the broader populace, PPGP demonstrates an amplified intensity of agony and harbors intricate mechanisms that lack explicit etiological and muscular pathological substantiation.57 Hence, the identification of PPGP from the LBP population and the study of this separate clinical entity is of great importance. The study of the clinical characteristics of the PGP population has also been an ongoing research hotspot in various countries and regions, with recent studies focusing on more detailed aspects of the PGP population, such as balance control, correlation with other systemic complications, as opposed to the previous focus on prevalence and pain-related indicators.58–60 In addition to physical therapy and exercise, other treatments that may be helpful for PGP include the use of supportive devices such as pelvic belts or crutches, hot or cold therapy, and transcutaneous electrical nerve stimulation (TENS).12,61 In some cases, a combination of treatments may be required to effectively manage PGP symptoms.
From the co-occurrence of keywords, it becomes apparent that the exploration into the etiology of PPGP necessitates perpetuation, while the identification of risk factors for PPGP should be predicated upon meticulous epidemiological insights pertaining to the PPGP population and the pathological attributes of the ailment. Per the extant body of research, a historical record of low back pain emerges as a noteworthy harbinger for PPGP, substantiated by a substantial corpus of evidence.62,63 Pelvic low back pain during pregnancy is a significant risk factor for postpartum pelvic low back pain,64,65 and depression during pregnancy is a risk and aggravating factor for PPGP.47 In addition pre-pregnancy BMI >25 is also a risk factor and deserves further investigation, following a comprehensive multivariate analysis, Stomp et al crafted two holistic prognostic models: one delineating the ramifications specific to pregnancy, and the other encompassing both the gestational and postpartum periods.64 Notably, the inclusion or exclusion of low back pain (LBP) encompassed disparate findings across various studies,1,47,52 there is no consensus in defining outcome measures for PPGP. However, these clear risk factors associated with PPGP are only at the stage of questionnaire and subsequent multivariate analysis, where the validation of models and studies of etiological pathological explanations of mechanisms remain unreported, although several studies have attempted explanations but lack a validation link. And there is some evidence to suggest that PGP may be associated with an increased risk of assisted vaginal delivery or caesarean section, although more research is needed to fully understand this relationship. Henceforth, additional investigations are merited to elucidate the distinct repercussions of diverse risk factors pertaining to PPGP upon manifold physiological mechanisms and their magnitude. Such elucidation shall serve to impart guidance for the application thereof in the realm of disease therapeutics.
Moreover, due regard should be accorded to the safety aspects inherent in the implementation of all-encompassing therapeutic regimens. Improvement in patient pain and life status as well as treatment approach is a key factor affecting patient outcomes. Treatment options for PPGP include structured physical therapy, acupuncture, and exercise, all of which have a small body of evidence to support their efficacy, while acupuncture and exercise stabilization are effective complements to standard treatment for women with PPGP.66 As Ergonomics and Rehabilitation Medicine evolve, many new techniques are being developed, including the use of supportive devices, such as pelvic support belts, to relieve stress on the lower back, hips, and pelvis.67 The use of manual therapy techniques, such as manual pelvic mobilization and chiropractic care, to improve the function of the pelvic girdle and reduce pain and discomfort. The salience of exercise and physical therapy in the governance of PPGP lies in their instrumental function, replete with an unwavering focus on enhancing fortitude, equilibrium, and malleability within the confines of the pelvic girdle and lumbar realm. The use of pain management techniques, such as medication, acupuncture, and massage, to help alleviate symptoms of PPGP. One of the principal perils associated with movement therapeutics resides in the potential for modifications in intensity and exercise physiology to detrimentally exacerbate or instigate injury to the delicate pelvic floor muscles subsequent to childbirth.68,69 In turn, inherent damage of pelvic floor structure can be incorporated into factors limiting exercise,70 introducing a potential risk to the exercise therapy of PPGP.38,71 In contrast to exercise and standardized physiotherapy, acupuncture exhibits a diminished degree of risk72 and may be comparatively more secure. Nevertheless, our comprehension remains incomplete, necessitating further investigations to juxtapose the safety of individual PPGP physiotherapeutic interventions and their potential risk factors. A burgeoning acknowledgment of the significance surrounding the resolution of physical, psychological, and social determinants that may engender PPGP symptoms, and the development of multidisciplinary care models that bring together healthcare professionals from different specialties to provide comprehensive and integrated care. There is limited research available on the effectiveness of different treatments for PPGP, and further research is needed to better understand this condition and develop more effective treatment options.
The detection of keyword bursts reveals that the utilization of questionnaires and the examination of outcomes has experienced an explosive surge in citations since 2019 and 2020, thus indicating its potential as a burgeoning research focal point. Primarily, he configuration and formation of questionnaires (commonly denoted as scales) bear the potential to influence the epidemiological attributes, risk factors and diagnostic standards applicable to the PPGP population.73 The identification and management of PGP present a formidable task, as discerning between PGP and other ailment manifestations that engender analogous symptoms1 often poses a considerable challenge. Rational and scientific design of questionnaires/scales seems to reduce the differences in prevalence and symptomatology removing unnecessary statistical bias, thus improving the credibility of epidemiological reports of PPGP may improve its quality and academic impact.74 The employment of the Oswestry Disability Index of Pain Intensity (ODI) and the Numeric Rating Scale (NRS) emerged as the prevailing practice in the initial evaluation of PPGP functionality. However, both questionnaires were originally developed for patients with low back pain (LBP),17 and the LBP outcome measures are not necessarily appropriate for PGP.75 Britt Stuge and his team from Oslo University Hospital developed the Pelvic Girdle Questionnaire (PGQ), a reliable, valid and sensitive outcome measure of patient change using a specific methodology that provides a patient-specific, simple and valid assessment tool for the PGP field and continues to be accepted and used worldwide.73,74,76–79
In addition to the need to standardize the scales, the overall PGP outcome indicators are a more important element to standardize and study.80 Although previous studies have applied enough methods to intervene in PGP. As previously mentioned, common treatments for PGP include physical therapy, exercise, pain management techniques, and the use of supportive devices such as pelvic support belts, but the wide variety of outcomes reported in studies and the high heterogeneity among studies make it difficult to combine and interpret the resulting evidence.81 The discrepancy may arise from the use of various measurement tools in different studies to obtain identical results. These limitations hinder the application of the findings. The heterogeneity of the outcome measures reported restricts both direct comparisons and pooling of experimental data, making it tough, and at times impossible to translate the data into clinical practice.82
Thus, the in-depth development of the Core Outcome Set (COS) may represent a canonical part of the PPGP scientific research reports. For another, the updating and expansion of the Core Outcome Set (COS) can also play a role in guiding clinical practice following the evaluation and comparison of clinical outcome indicators before we can provide evidence for a particular treatment.83 The Core Set outcomes is designed to allow the aggregation of clinical findings for the same type of treatment to form a stronger body of evidence, and the efficacy of a single treatment requires additional studies and their aggregation to account for it. In addition to the physical therapy approaches mentioned above, psychological interventions further manifested their therapeutic efficacy across a spectrum of PPGP cases, including reduced pain levels,84 improved activities of daily living (ADL),6 improved motor performance,73 reduced number of positive pain provocation tests,48 and preventing long-term PPGP,85 and only after this can recommendations for combination therapies be made, and this COS update is actually providing the normative means to recommend more reliable combination management strategies, as seen in the co-citation clustering analysis. The prevalence of PPGP has witnessed a substantial surge, thereby exerting detrimental ramifications on both the individuals’ quality of life and imposing a considerable strain on the healthcare infrastructure.86 To address this quandary, a profound exploration into the role and mechanism of comprehensive management strategies in PPGP necessitates immediate attention. Consequently, subjects pertaining to integrated management strategies are poised to become a prominent focal point for future research endeavors in the domain of PPGP.
Strengths and Limitations
We undertook an exhaustive bibliometric analysis of the research on PPGP spanning the period from 2012 to 2022, aiming to present the current state of research, scrutinize its focal points, and forecast future research trends, marking the inaugural endeavor of its kind. Moreover, an array of instruments, such as VOSviewer and CiteSpace, were employed to uphold the credibility and impartiality of the findings. Nevertheless, the current study encompasses a number of limitations that warrant recognition. Although our bibliometric analysis offers invaluable insights into PPGP research, it is imperative to duly acknowledge and rectify its constraints. One limitation is the use of the Web of Science (WoS) database as the primary source for our analysis. While WoS is a comprehensive database, other platforms may offer additional relevant publications that were not captured in our study. Secondly, the selected number of articles, although representative, may not encompass the entire breadth of PPGP research output. Consequently, interpretations should account for this limitation. More studies will be needed to confirm our present findings. Another notable limitation in our study is the potential language bias resulting from our focus on English language publications. In all, we suggest that there is still room for improvement in the field.
Conclusion
By employing CiteSpace and VOSviewer, we curated and scrutinized the worldwide research landscape, evolutionary patterns, focal points, and cutting-edge themes pertaining to PPGPs. In recent times, the realm of PPGPs has garnered significant attention and experienced exponential growth. The analysis of keyword and co-citation clusters revealed that current investigations primarily center around the curative or supportive therapeutic effectiveness of a holistic and cohesive methodology in addressing PPGP. Furthermore, the demographic peculiarities of the PPGP populace in Asia, South America, and Africa continue to hold relevance for scholarly inquiry, which institutions that already have more established experience and databases can also strengthen their collaboration with these regions, and a global PPGP epidemiological study would be of great Clinical value and research appeal.
In addition, epidemiological investigations should be timed to the deficits of PPGP patients under the new crown pandemic, and the loss of access to exercise interventions or lifestyle interventions are also current hot topics. The correlation between the changes brought about by PPGP to patients whether physical, psychological, lifestyle and PPGP may be discussed and become a hot topic in many cases where the disease is explored, such as the COVID pandemic. The consideration that reduced active activity in PPGP may diminish the benefits of physical activity on PPGP has also received a small amount of attention in this aspect of PGP and going forward deserves to be discussed and addressed in more depth. Moreover, PPGP is a common and often debilitating condition that affects many women during pregnancy. While there is still much to be learned about this condition, there are approaches that have shown promise in alleviating symptoms and improving quality of life for women who are affected by PPGP.
Still there are many viable single strategies that are not supported by sufficient evidence, such as physiotherapy, exercise, pain management techniques, and the use of supportive equipment. And the underlying mechanisms involved, including changes in biomechanics, improvements in the anatomy of the local injury, and so on. Alternatively, low-energy shock waves and low-frequency pulsed ultrasound may be promising treatments that have been proven effective in men with pelvic pain syndromes. Synergistic interdisciplinary cooperation stands as an evolving inclination within this domain, poised to substantively augment the clinical implementation of PPGPs. These burgeoning tendencies and prominent subjects underscore the significance of adopting an encompassing and harmonious methodology towards the therapy and governance of PPGP, while accentuating the prospective advantages of amalgamating manifold interventions to attain the utmost favorable outcome for women grappling with this ailment.
Acknowledgments
We thank all the authors of the original studies included in this analysis.
Disclosure
The authors declare that they have no conflicts of interest in this work.
References
1. Wu WH, Meijer OG, Uegaki K, et al. Pregnancy-related pelvic girdle pain (PPP), I: terminology, clinical presentation, and prevalence. Eur Spine J. 2004;13:575–589. doi:10.1007/s00586-003-0615-y
2. Vleeming A, Albert HB, Östgaard HC, Sturesson B, Stuge SB. European guidelines for the diagnosis and treatment of pelvic girdle pain. Eur Spine J. 2008;17(6):794–819. doi:10.1007/s00586-008-0602-4
3. Albert HB, Godskesen M, Korsholm L, Westergaard JG. Risk factors in developing pregnancy-related pelvic girdle pain. Acta Obstet Gyn Scan. 2006;85(5):539–544. doi:10.1080/00016340600578415
4. Caputo EL, Ferreira PH, Ferreira ML, et al. Physical activity before or during pregnancy and low back pain: data from the 2015 pelotas (Brazil) Birth Cohort Study. J Phys Act Health. 2019;16(10):886–893. doi:10.1123/jpah.2018-0624
5. Aldabe D, Lawrenson P, Sullivan J, et al. Management of women with pregnancy-related pelvic girdle pain: an international Delphi study. Physiotherapy. 2022;115:66–84. doi:10.1016/j.physio.2021.09.002
6. Diez‐Buil H, Hernandez‐Lucas P, Leirós‐Rodríguez R, et al. Effects of the combination of exercise and education in the treatment of low back and/or pelvic pain in pregnant women: systematic review and meta‐analysis. Int J Gynecol Obstet. 2023. doi:10.1002/ijgo.15000
7. Ostgaard HC, Zetherstrom G, Roos-Hansson E. Prevalence of pelvic pain in pregnancy. Spine. 1991;16(10):1081–1085. doi:10.1097/00007632-199105000-00011
8. Vleeming A, Albert HB, Ostgaard HC, Sturesson B, Stuge B, Volkers AC. The sacroiliac joint in pregnancy-related pelvic pain: a review. Eur Spine J. 2008;17(6):781–788.
9. Andersen LK, Backhausen M, Hegaard HK, Juhl M. Physical exercise and pelvic girdle pain in pregnancy: a nested case-control study within the Danish National Birth Cohort. Sex Reprod Health. 2015;6:198–203. doi:10.1016/j.srhc.2015.04.004
10. Agarwal A, Durairajanayagam D, Tatagari S, et al. Bibliometrics: tracking research impact by selecting the appropriate metrics. Asian J Androl. 2016;18(2):296–309. doi:10.4103/1008-682X.171582
11. Ma C, Su H, Li H. Global research trends on prostate diseases and erectile dysfunction: a bibliometric and visualized study. Front Oncol. 2020;10:627891. doi:10.3389/fonc.2020.627891
12. Birsner ML, Gyamfi-Bannerman C. Physical activity and exercise during pregnancy and the postpartum period: ACOG committee opinion, number 804. Obstet Gynecol. 2020;135(4):e178–e188. doi:10.1097/AOG.0000000000003772
13. Stuge SB, Veierod MB, Laerum E, Vollestad N. The efficacy of a treatment program focusing on specific stabilizing exercises for pelvic girdle pain after pregnancy - a two-year follow-up of a randomized clinical trial. Spine. 2004;29(10):E197–E203. doi:10.1097/00007632-200405150-00021
14. Pivarnik JM, Chambliss HO, Clapp JF, et al. Impact of physical activity during pregnancy and postpartum on chronic disease risk. Med Sci Sport Exer. 2006;38(5):989–1006. doi:10.1249/01.mss.0000218147.51025.8a
15. Vermani E, Mittal R, Weeks A. Pelvic girdle pain and low back pain in pregnancy: a review. Pain Pract. 2010;10(1):60–71. doi:10.1111/j.1533-2500.2009.00327.x
16. Nascimento SL, Surita FG, Cecatti JG. Physical exercise during pregnancy: a systematic review. Curr Opin Obstet Gynl. 2012;24(6):387–394. doi:10.1097/GCO.0b013e328359f131
17. Noren L, Ostgaard S, Johansson G, Ostgaard HC. Lumbar back and posterior pelvic pain during pregnancy: a 3-year follow-up. Eur Spine J. 2002;11(3):267–271. doi:10.1007/s00586-001-0357-7
18. Stuge SB, Laerum E, Kirkesola G, Vollestad N. The efficacy of a treatment program focusing on specific stabilizing exercises for pelvic girdle pain after pregnancy - A randomized controlled trial. Spine. 2004;29(4):351–359. doi:10.1097/01.BRS.0000090827.16926.1D
19. de Winter J, de Hooge M, van de Sande M, et al. Magnetic resonance imaging of the sacroiliac joints indicating sacroiliitis according to the assessment of SpondyloArthritis international society definition in healthy individuals, runners, and women with postpartum back pain. Arthritis Rheumatol. 2018;70(7):1042–1048. doi:10.1002/art.40475
20. Franke H, Franke JD, Fryer G. Osteopathic manipulative treatment for nonspecific low back pain: a systematic review and meta-analysis. BMC Musculoskelet Dis. 2014;15:286. doi:10.1186/1471-2474-15-286
21. Albert H, Godskesen M, Westergaard J. Prognosis in four syndromes of pregnancy-related pelvic pain. Acta Obstet Gynecol Scand. 2001;80(6):505–510.
22. Ostgaard HC, Andersson GB, Karlsson K. Prevalence of back pain in pregnancy. Spine. 1991;16(5):549–552. doi:10.1097/00007632-199105000-00011
23. Kristiansson P, Svärdsudd K, von Schoultz B. Back pain during pregnancy: a prospective study. Spine. 1996;21(6):702–708. doi:10.1097/00007632-199603150-00008
24. Stgaard HC, Roos-Hansson E, Zetherström G. Regression of back and posterior pelvic pain after pregnancy. Spine. 1996;21(23):2777–2780. doi:10.1097/00007632-199612010-00013
25. Mens JM, Vleeming A, Snijders CJ, Ronchetti I, Stam HJ. Reliability and validity of hip adduction strength to measure disease severity in posterior pelvic pain since pregnancy. Spine. 2002;27(15):1674–1679. doi:10.1097/00007632-200208010-00017
26. Mogren IM, Pohjanen AI. Low back pain and pelvic pain during pregnancy: prevalence and risk factors. Spine. 2005;30(8):983–991. doi:10.1097/01.brs.0000158957.42198.8e
27. Damen L, Buyruk HM, Guler-Uysal F, Lotgering FK, Snijders CJ, Stam HJ. The prognostic value of asymmetric laxity of the sacroiliac joints in pregnancy-related pelvic pain. Spine. 2002;27(24):2820–2824. doi:10.1097/00007632-200212150-00018
28. Mens JM, Vleeming A, Snijders CJ, Koes BW, Stam HJ. Validity of the active straight leg raise test for measuring disease severity in patients with posterior pelvic pain after pregnancy. Spine. 2002;27(2):196–200. doi:10.1097/00007632-200201150-00015
29. Gutke A, Gutke A, Josefsson A, Oberg B. Pelvic girdle pain and lumbar pain in relation to postpartum depressive symptoms. Spine. 2007;32:1430–1436. doi:10.1097/BRS.0b013e318060a673
30. Stuge SB, Holm I, Vollestad N. To treat or not to treat postpartum pelvic girdle pain with stabilizing exercises? Manual Ther. 2006;11(4):337–343. doi:10.1016/j.math.2005.07.004
31. Gutke A, Gutke A, Lundberg M, Ostgaard HC, Oberg B. Impact of postpartum lumbopelvic pain on disability, pain intensity, health-related quality of life, activity level, kinesiophobia, and depressive symptoms. Eur Spine J. 2011;20:440–448. doi:10.1007/s00586-010-1487-6
32. Sjodahl J, Gutke A, Gutke A, Oberg B. Predictors for long-term disability in women with persistent postpartum pelvic girdle pain. Eur Spine J. 2013;22:1665–1673. doi:10.1007/s00586-013-2716-6
33. Bo K, Artal R, Barakat R, et al. Exercise and pregnancy in recreational and elite athletes: 2016/17 evidence summary from the IOC expert group meeting, Lausanne. Part 3-exercise in the postpartum period. BrJ Sport Med. 2017;51:1516–1525. doi:10.1136/bjsports-2017-097964
34. Thorell E, Kristiansson P. Pregnancy related back pain, is it related to aerobic fitness? A longitudinal cohort study. BMC Pregnancy Childb. 2012;12:1–8.
35. Acharya RS, Tveter AT, Grotle M, Eberhard-Gran M, Stuge SB. Prevalence and severity of low back- and pelvic girdle pain in pregnant Nepalese women. BMC Pregnancy Childb. 2019;19:1.
36. Moran PS, Wuytack F, Turner M, et al. Economic burden of maternal morbidity - a systematic review of cost-of-illness studies. PLoS One. 2020;15:1.
37. Morkved S, Salvesen KA, Schei B, Lydersen S, Bo K. Does group training during pregnancy prevent lumbopelvic pain? A randomized clinical trial. Acta Obstet Gyn Scan. 2007;86:276–282. doi:10.1080/00016340601089651
38. Bo K, Backe-Hansen KL. Do elite athletes experience low back, pelvic girdle and pelvic floor complaints during and after pregnancy? Scand J Med Sci Spor. 2007;17:480–487. doi:10.1111/j.1600-0838.2006.00599.x
39. Torstensson T, Lindgren A, Kristiansson P. Corticosteroid injection treatment to the ischiadic spine reduced pain in women with long-lasting sacral low back pain with onset during pregnancy a randomized, double blind, controlled trial. Spine. 2009;34:2254–2258. doi:10.1097/BRS.0b013e3181b07eac
40. Bjelland EK, Owe KM, Nordeng HME, et al. Does progestin-only contraceptive use after pregnancy affect recovery from pelvic girdle pain? A prospective population study. PLoS One. 2017;12:1.
41. Wuytack F, Curtis E, Begley C. The health-seeking behaviours of first-time mothers with persistent pelvic girdle pain after childbirth in Ireland: a descriptive qualitative study. Midwifery. 2015;31(11):1104–1109. doi:10.1016/j.midw.2015.07.009
42. Elden H, Gutke A, Gutke A, Kjellby-Wendt G, Fagevik-Olsen M, Ostgaard H-C. Predictors and consequences of long-term pregnancy-related pelvic girdle pain: a longitudinal follow-up study. BMC Musculoskel Dis. 2016;17:1.
43. Ambule K, Mahakarkar M. Protocol on the effects of postnatal exercises on musculoskeletal pain among postpartum women. J Pharm Res Int. 2021;33:12–16. doi:10.9734/jpri/2021/v33i47A32985
44. Kihlstrand M, Stenman B, Nilsson S, Axelsson O. Water-gymnastics reduced the intensity of back/low back pain in pregnant women. Acta Obstet Gynecol Scand. 1999;78(3):180–185.
45. Wuytack F, Daly D, Curtis E, Begley C. Prognostic factors for pregnancy-related pelvic girdle pain, a systematic review. Midwifery. 2018;66:70–78. doi:10.1016/j.midw.2018.07.012
46. Simonds AH, Abraham K, Spitznagle T. Clinical practice guidelines for pelvic girdle pain in the postpartum population. J Womens Health Phys Ther. 2022;46(1):E1–E38. doi:10.1097/JWH.0000000000000236
47. Virgara R, Maher C, van Kessel G. The comorbidity of low back pelvic pain and risk of depression and anxiety in pregnancy in primiparous women. Bmc Pregnancy Childb. 2018;18:1.
48. Anakaris NK, Roberts CS, Giannoudis PV. Pregnancy-related pelvic girdle pain: an update. BMC Med. 2011;9:15. doi:10.1186/1741-7015-9-15
49. Ceprnja D, Chipchase L, Gupta A. Prevalence of pregnancy-related pelvic girdle pain and associated factors in Australia: a cross-sectional study protocol. BMJ Open. 2017;7(11):e018334. doi:10.1136/bmjopen-2017-018334
50. Ceprnja D, Chipchase L, Fahey P, Liamputtong P, Gupta A. Prevalence and factors associated with pelvic girdle pain during pregnancy in Australian women: a Cross-Sectional Study. Spine. 2021;46(14):944–949. doi:10.1097/BRS.0000000000003954
51. Van De Pol G, Van Brummen HJ, Bruinse HW, et al. Pregnancy-related pelvic girdle pain in the Netherlands. Acta Obstet Gynecol Scand. 2007;86(4):416–422. doi:10.1080/00016340601151683
52. Chortatos A, Iversen PO, Haugen M, et al. Nausea and vomiting in pregnancy - association with pelvic girdle pain during pregnancy and 4–6 months post-partum. Bmc Pregnancy Childb. 2018;18(1):137. doi:10.1186/s12884-018-1764-7
53. Mukkannavar P, Desai BR, Mohanty U, Kulkarni S, Parvatikar V, Daiwajna S. Pelvic girdle pain in Indian postpartum women: a cross-sectional study. Physiother Theor Pr. 2014;30(2):123–130. doi:10.3109/09593985.2013.816399
54. Catena RD, Campbell N, C WC, et al. Anthropometry, standing posture, and body center of mass changes up to 28 weeks postpartum in caucasians in the United States. Gait Posture. 2019;70:196–202. doi:10.1016/j.gaitpost.2019.03.009
55. J HB, Chatfield S, Cameron L, et al. Protocol: evaluating the Management of chronic Pelvic girdle Pain following pregnancy (EMaPP): study protocol for a randomised controlled feasibility trial to compare a customised pelvic orthosis with standard care[J]. BMJ Open. 2022;12(8):1.
56. Vardar Z, S CS, Goldstein AJ, et al. Pelvic ultrasonography of the postpartum uterus in patients presenting to the emergency room with vaginal bleeding and pelvic pain. Ultrasonography. 2022;41(4):782. doi:10.14366/usg.22004
57. Wiezer M, Hage-Fransen MAH, Otto A, et al. Risk factors for pelvic girdle pain postpartum and pregnancy related low back pain postpartum; a systematic review and meta -analysis. Musculoskelet Sci Pract. 2020;48:1.
58. van Benten E, Coppieters MW, Pool JJM, Pool-Goudzwaard AL. Differences in balance control despite self-reported resolution of pregnancy-related pelvic girdle pain. A cross-sectional study. Musculoskelet Sci Pract. 2022;62:1.
59. Yuan S, Wang H, Zhou J. Prevalence and risk factors of low back and pelvic pain in women with rectus abdominis diastasis: a multicenter retrospective cohort study. Korean J Pain. 2022;35:86–96. doi:10.3344/kjp.2022.35.1.86
60. Mutaguchi M, Murayama R, Takeishi Y, et al. Relationship between low back pain and stress urinary incontinence at 3 months postpartum. Drug Discov Ther. 2022;16(1):23–29. doi:10.5582/ddt.2022.01015
61. Quittan M, Bily W, Crevenna R, et al. Transcutaneous Electrical Nerve Stimulation (TENS) in patients with pregnancy-induced low back pain and/or pelvic girdle pain. Phys Med Rehab Kuror. 2016;26:91–95. doi:10.1055/s-0035-1565058
62. Gausel AM, Dalen I, Kjaermann I, et al. Adding chiropractic treatment to individual rehabilitation for persistent pelvic girdle pain 3 to 6 months after delivery: a pilot randomized trial. J Manip Physiol Ther. 2019;42(8):601–607. doi:10.1016/j.jmpt.2018.12.006
63. Robinson HS, Mengshoel AM, Veierod MB, Vollestad N. Pelvic girdle pain: potential risk factors in pregnancy in relation to disability and pain intensity three months postpartum. Manual Ther. 2010;15(6):522–528. doi:10.1016/j.math.2010.05.007
64. Stomp-van den Berg SGM, Hendriksen IJM, Bruinvels DJ, Twisk JWR, van Mechelen W, van Poppel MNM. Predictors for postpartum pelvic girdle pain in working women: the Mom@Work cohort study. Pain. 2012;153(12):2370–2379. doi:10.1016/j.pain.2012.08.003
65. Gausel AM, Kjrmann I, Malmqvist S, Dalen I, Larsen JP, Okland I. Pelvic girdle pain 3–6 months after delivery in an unselected cohort of Norwegian women. Eur Spine J. 2016;25:1953–1959. doi:10.1007/s00586-015-3959-1
66. Elden H, Ladfors L, Olsen OM, et al. Effects of acupuncture and stabilising exercises as adjunct to standard treatment in pregnant women with pelvic girdle pain: randomised single blind controlled trial. BMJ. 2005;330(7494):761. doi:10.1136/bmj.38397.507014.E0
67. Morino S, Ishihara M, Umezaki F, et al. The effects of pelvic belt use on pelvic alignment during and after pregnancy: a prospective longitudinal cohort study. Bmc Pregnancy Childb. 2019;19:1.
68. Stær-Jensen J, Siafarikas F, Hilde G, et al. Postpartum recovery of levator hiatus and bladder neck mobility in relation to pregnancy. Obstet Gynecol. 2015;125(3):531–539. doi:10.1097/AOG.0000000000000645
69. Van Delft KWM, Thakar R, Sultan AH, et al. The natural history of levator avulsion one year following childbirth: a prospective study. BJOG. 2015;122(9):1266–1273. doi:10.1111/1471-0528.13223
70. Shek KL, Dietz HP. Intrapartum risk factors for levator trauma. BJOG. 2010;117(12):1485–1492. doi:10.1111/j.1471-0528.2010.02704.x
71. C SSC, Cheung RYK, Yiu KW, et al. Effect of levator ani muscle injury on primiparous women during the first year after childbirth. Int Urogynecol J. 2014;25(10):1381–1388. doi:10.1007/s00192-014-2340-y
72. Moll R, Derry S, Moore RA, McQuay HJ. Single dose oral mefenamic acid for acute postoperative pain in adults. Cochrane Db Syst Rev. 2011;2011:1.
73. Stuge B, Garratt A, Krogstad Jenssen H, Grotle M. The pelvic girdle questionnaire: a condition-specific instrument for assessing activity limitations and symptoms in people with pelvic girdle pain. Phys Ther. 2011;91(7):1096–1108. doi:10.2522/ptj.20100357
74. Rejano-Campo M, Ferrer-Pena R, Alicia Urraca-Gesto M, et al. Transcultural adaptation and psychometric validation of a Spanish-language version of the ”Pelvic Girdle Questionnaire”. Health Qual Life Out. 2017;15:1.
75. van de Pol G, Leeuw JRJ, van Brummen HJ, Bruinse HW, Heintz APM, van der Vaart CH. The pregnancy mobility index: a mobility scale during and after pregnancy. Acta Obstet Gyn Scan. 2006;85(7):786–791. doi:10.1080/00016340500456373
76. Cong H, Liu H, Sun Y, et al. Cross-cultural adaptation, reliability, and validity of a Chinese version of the pelvic girdle questionnaire. BMC Pregnancy Childb. 2021;21:1.
77. Girard M-P, Marchand -A-A, Stuge SB, Ruchat S-M, Descarreaux M. Cross-cultural adaptation of the pelvic girdle questionnaire for the French-Canadian population. J Manip Physiol Ther. 2016;39(7):494–499. doi:10.1016/j.jmpt.2016.06.002
78. R FF, Kariman N, Ozgoli G, et al. Iranian version of pelvic girdle questionnaire: psychometric properties and cultural adaptation. J Res Med Sci. 2019;2019:1.
79. Gutke A, Gutke A, Stuge SB, et al. The Swedish version of the pelvic girdle questionnaire, cross-cultural adaptation and validation. Disabil Rehabil. 2020;42:1013–1020. doi:10.1080/09638288.2018.1515991
80. Grotle M, Garratt AM, Jenssen HK, Stuge B. Reliability and construct validity of self-report questionnaires for patients with pelvic girdle pain. Phys Ther. 2012;92(1):111–123. doi:10.2522/ptj.20110076
81. Gutke A, Gutke A, Betten C, Degerskar K, Pousette S, Olsen MF. Treatments for pregnancy-related lumbopelvic pain: a systematic review of physiotherapy modalities. Acta Obstet Gyn Scan. 2015;94:1156–1167. doi:10.1111/aogs.12681
82. Wuytack F, Annelie Gutke GA, Stuge SB, et al. Protocol for the development of a core outcome set for pelvic girdle pain, including methods for measuring the outcomes: the PGP-COS study. BMC Med Res Methodol. 2018;18:158. doi:10.1186/s12874-018-0624-5
83. Remus A, Smith V, Annelie Gutke GA, et al. A core outcome set for research and clinical practice in women with pelvic girdle pain: PGP-COS. PLoS One. 2021;16(2):e0247466. doi:10.1371/journal.pone.0247466
84. Kirkham JJ, Davis K, Altman DG, et al. Core outcome set-STAndards for development: the COS-STAD recommendations. PLOS Med. 2017;14(11):e1002447. doi:10.1371/journal.pmed.1002447
85. Desseauve D, Proust S, Carlier-Guerin C, Rutten C, Pierre F, Fritel X. Evaluation of long-term pelvic floor symptoms after an obstetric anal sphincter injury (OASI) at least one year after delivery: a retrospective cohort study of 159 cases. Gynecol Obstet Fertil. 2016;44(7–8):385–390. doi:10.1016/j.gyobfe.2016.05.007
86. Waggoner J, Carline JD, Durning SJ. Is there a consensus on consensus methodology? Descriptions and recommendations for future consensus research. Acad Med. 2016;91(5):663–668. doi:10.1097/ACM.0000000000001092
 © 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2024 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.