Back to Journals » Diabetes, Metabolic Syndrome and Obesity » Volume 16
Knowledge, Attitude, and Practice of Insulin Pump Among Non-Endocrinology Nurses in South China
Authors Mo C, Huang X, Lu X, Zhou Y, Su Y, Zhang H
Received 31 March 2023
Accepted for publication 1 August 2023
Published 30 October 2023 Volume 2023:16 Pages 3417—3423
DOI https://doi.org/10.2147/DMSO.S414327
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Konstantinos Tziomalos
Video abstract presented by Cuiying Mo.
Views: 103
Cuiying Mo,1,* Xufen Huang,2,* Xiaohua Lu,3 Yan Zhou,4 Yingyi Su,1 Huanhua Zhang1
1Department of Endocrinology, The First People’s Hospital of Foshan, Foshan, People’s Republic of China; 2Department of Pediatrics, The First Affiliated Hospital of Jinan University, Guangzhou, People’s Republic of China; 3Department of Endocrinology, The First Affiliated Hospital of Jinan University, Guangzhou, People’s Republic of China; 4Department of Interventional Radiology & Vascular Surgery, The First Affiliated Hospital of Jinan University, Guangzhou, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Xiaohua Lu, Department of Endocrinology, The First Affiliated Hospital of Jinan University, No. 613, Huangpu Avenue West, Tianhe District, Guangzhou, 510630, People’s Republic of China, Tel +8618028089803, Email [email protected] Yan Zhou, Department of Interventional Radiology & Vascular Surgery, The First Affiliated Hospital of Jinan University, Guangzhou, 510630, People’s Republic of China, Email [email protected]
Purpose: To investigate the knowledge, attitude, and practice (KAP) on insulin pump among non-endocrinology nurses in Southern China.
Methods: This multicenter cross-sectional study enrolled non-endocrinology nurses in Southern China between November 2020 and December 2020. A structured questionnaire about insulin pumps was designed and used to collect data.
Results: A total of 1118 nurses from 29 hospitals participated in the study. The majority of them were female (98.48%), and 513 worked in the department of internal medicine (45.89%), followed by surgery (235, 21.00%), pediatrics (147, 13.14%), gynecology (127, 11.35%), and oncology (96, 8.71%). None of the nurses answered all questions correctly in the knowledge section. The score of knowledge was 50.12 ± 3.42 (total score range, 0 to 85). The attitude score of nurses in the department of gynecology was 47.76 ± 5.11 (total score range, 10 to 50), followed by nurses in the department of internal medicine (47.43 ± 4.65), pediatrics (46.71 ± 4.96), surgery (46.77 ± 5.78) and oncology (46.25 ± 5.87). The practice score of nurses in the internal medicine department was 79.16 ± 9.03 (total score range, 17 to 85), followed by nurses in the department of gynecology (78.76 ± 10.76), surgery (78.14 ± 10.09), oncology (76.89 ± 12.70) and pediatrics (73.35 ± 19.04).
Conclusion: There was limited knowledge regarding insulin pumps among nurses, although they had a positive attitude and attached importance to the management of insulin pumps. In clinical practice, their implementation of insulin pump management norms was acceptable.
Keywords: nurse, insulin pumps, knowledge, attitude, practice
Introduction
Diabetes mellitus (DM) is a major public health issue, and its prevalence is increasing worldwide.1–3 In China, the estimated prevalence rate of DM has reached 11.6% and might even double in the coming decades due to population growth.4–6 Uncontrolled blood glucose leads to hyperglycemia and is associated with increased morbidity related to longer hospital stays, delayed healing, increased incidence of infections, and macrovascular and microvascular complications, as well as with mortality in non-critical inpatients.1,2,7 Therefore, well-controlled blood glucose is essential. Many patients will gradually fail oral treatments and eventually require insulin.1,2 The use of insulin is unpractical and can lead to poor treatment adherence,8 affecting prognosis. Insulin pump therapy is a form of insulin treatment that maximally mimics the physiological secretion pattern of insulin to achieve better glycemic control, and it does not require repeated injections.9,10
Still, insulin pumps are highly specialized and sophisticated equipment, requiring specific knowledge.9,10 Insulin pump therapy was initially concentrated in hospital endocrinology departments, but many patients with DM can be admitted to other departments for various reasons or procedures, but nurses in those departments might be ill-prepared to deal with insulin pumps. Furthermore, in recent years many tertiary hospitals in China gradually adopted the endocrinology team management model of DM to manage hyperglycemic patients in other departments. The management team of DM includes specialist endocrinologists and nurses who carry out daily visits to those hyperglycemic patients treated with insulin pumps. This management model can increase the rate of glycemic compliance, reduce the average length of stay, and improve patient clinical outcomes.11,12
Nurses are at the front line of health service delivery and play a central role in insulin pump practice.10 A knowledge, attitudes, and practice (KAP) study showed that even in DM liaison nurses, the KAP of insulin pump management could be as low as 18–29%.13 Therefore, using and managing insulin pump therapy in China might be quite challenging, and there might be safety risks associated with insulin pump application. Indeed, poor knowledge among healthcare workers would lead to poor patient health education.14
This cross-sectional study aimed to investigate the KAP regarding insulin pumps among non-endocrinology nurses.
Materials and Methods
Study Design and Participants
This multicenter cross-sectional study enrolled nurses from tertiary hospitals in Southern China between November 2020 and December 2020. The participants were recruited by convenience sampling. The inclusion criteria were 1) Individuals holding a nurse license and 2) With experience with insulin pumps. The exclusion criteria were 1) nurses in the endocrinology department, 2) working in a department where insulin pumps had never been used in clinical practice, or 3) On departmental rotations. The research was carried out in accordance with the Declaration of Helsinki. The study was approved by the ethics committee of The First People’s Hospital of Foshan [# Ren Shenyan (2022) No. 143]. All participants signed the informed consent form prior to the study.
Procedure
A self-administered questionnaire regarding the KAP towards insulin pump was developed using the Delphi method. Based on the social cognitive theory and self-management theory, the first draft of the questionnaire was developed through a literature review and group discussion, with the guidance of the “China Insulin Pump Nursing Management Practice”. The Delphi method was applied to conduct two rounds of expert consultation, and 26 experts were invited to screen and evaluate the indicators of the scale. The effective recall rates for the two rounds of correspondence questionnaires were 96% and 100%, respectively, and the expert opinion rates were 8.5% and 6.3%. The expert authority coefficients for the two rounds were 0.892 and 0.888, respectively, and Kendall’s W for items increased round by round. After two rounds of expert consultation, a structured questionnaire was developed containing 44 items in three sections: knowledge, attitude, and practice (Supplementary Materials). There were 17 items in the knowledge section, 10 in the attitude, and 17 in practice. Each correct answer in the knowledge section was given 1 point, with a total score of 17; incorrect or do not know were given a score of zero. The attitude and practice of nurses were rated on a 5-point Likert scale ranging from 1 (extremely negative) to 5 (highly positive), with a total score range of 10–50 and 17–85, respectively. The reliability and internal consistency of attitudes and practices were determined by the Cronbach’s α coefficient, with ≥ 0.7 being considered to have a high degree of reliability and consistency.
Data Collection
The project leader of each hospital was briefed on the background and objective of the study, and their approval was obtained. The Diabetes Specialist Nursing Group members at the surveyed hospital acted as surveyors or survey contacts for that hospital. The surveyors were responsible for distributing and retrieving questionnaires. The nurses completed questionnaires anonymously within 20 consecutive minutes. After 2 weeks, the surveyors in each hospital were reminded to submit the questionnaire in time and reminded again if not returned. Incomplete questionnaires, or those answered with all the same answers, were considered invalid.
Statistical Analysis
Statistical analyses were performed using SPSS 25.0 (IBM, Armonk, NY, USA). Continuous variables that conformed to the normal distribution were presented as mean ± standard deviation (SD), and that with skewed distribution were presented as median (range). Categorical variables were presented as n (percentage). Descriptive statistics were used to analyze the data.
Results
A total of 1118 questionnaires from 29 hospitals were included in the study; 86% were valid, ie, incomplete questionnaires or those answered with all the same answers. Among these nurses, 17 were male (1.52%), and the others were female (98.48%). There were 513 nurses working in the department of internal medicine (45.8%), followed by surgery (235, 21.00%), pediatrics (147, 13.14%), gynecology (127, 11.35%), and oncology (96, 8.71%) (Table 1).
 |
Table 1 Demographic Characteristics of Nurses |
None of the nurses answered all the questions correctly in the knowledge section, and the correct response rates were below 60% in all departments (26.38% in the department of surgery, 37.35% in internal medicine, 25.00% in oncology, 53.54% in gynecology, and 37.41% in pediatrics). The score of knowledge was 50.12 ± 3.42 (total score range, 0 to 85). The items with the highest incorrect rate among nurses were the type of insulin used in the insulin pump (56.17% in the department of surgery, 36.96% in internal medicine, 54.17% in oncology, 29.13% in gynecology, and 27.89% in pediatrics). In addition, there was also a high incorrect rate of the items regarding “how insulin is administered by the insulin pump” (40.85% in the department of surgery, 29.96% in internal medicine, 54.17% in oncology, 20.47% in gynecology, and 34.01% in pediatrics) (Table 2).
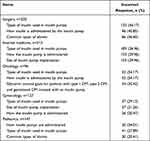 |
Table 2 Knowledge Items with Low Correct Rate in Different Departments |
The Cronbach’s α coefficient of the 10 attitude items was 0.959 (0.968 among nurses in the department of surgery, 0.947 among internal medicine nurses, 0.978 among oncology nurses, 0.968 among gynecology nurses, and 0.949 among pediatrics nurses). The attitude score of nurses in the department of gynecology was 47.76 ± 5.11 (total score range, 10 to 50), followed by nurses in the department of internal medicine (47.43 ± 4.65), pediatrics (46.71 ± 4.96), surgery (46.77 ± 5.78) and oncology (46.25 ± 5.87) (Table 1).
The Cronbach’s α coefficient of the 17 practice items was 0.954 among surgery nurses, 0.938 among internal medicine nurses, 0.960 among oncology nurses, 0.953 among gynecology nurses, and 0.984 among pediatrics nurses, respectively. The practice score of nurses in the internal medicine department was 79.16 ± 9.03 (total score range, 17 to 85), followed by nurses in the department of gynecology (78.76 ± 10.76), surgery (78.14 ± 10.09), oncology (76.89 ± 12.70) and pediatrics (73.35 ± 19.04) (Table 1).
Discussion
This cross-sectional study demonstrated limited knowledge of the application and management of insulin pumps among nurses, although they had a positive attitude and attached importance to the management of insulin pumps. In clinical practice, they could follow the norms of insulin pump management in most cases.
Insulin pump therapy is an insulin treatment method that uses an artificially intelligent controlled insulin input device to achieve better glycemic control by continuous subcutaneous insulin infusion, which maximally mimics the physiological secretion pattern of insulin.9 It is currently the most physiologically appropriate infusion method to control blood glucose to normal, and it is accepted by most patients as it reduces the pain associated with repeated punctures compared to the insulin pen.15 The American College of Endocrinology’s clinical resource, Clinical Practice Guidelines for Hyperglycemia in the Non-Emergency Inpatient Setting,16 suggest basal and prandial insulin injection as a standard treatment, but in those patients who use insulin pump therapy in an outpatient setting, it can be considered to continue using insulin pump in the inpatient setting if the patients have the mental and physical capacity to do so. Some studies showed that insulin pumps were effective in controlling blood glucose levels in patients with DM17–19 and were particularly effective in controlling blood glucose in patients with type I DM.20,21
It has been 20 years since insulin pump therapy was introduced in China at the beginning of the 21st century. Nearly 50,000 people with DM at home are long-term pump users. There are more than 3000 hospitals that conduct and use insulin pump therapy. Approximately more than 500,000 patients receive short-term intensive insulin pump therapy during hospitalization each year.14 However, there are still many problems in clinical application, such as abnormal hyperglycemia and hypoglycemia in patients using insulin pumps, infusion disorders, and skin abnormalities at the infusion site due to its complicated operation and other reasons.22,23 Western studies showed that insulin pump devices are associated with many pump-related adverse events and can lead to life-threatening or unexplained hyperglycemia in patients.24,25 A study by Xu26 and Tao27 also showed that with the widespread use of insulin pumps for hyperglycemic patients throughout the hospital, there were certain common problems in the management of insulin pumps in all departments. Thus, the role and significance of standardized management of patients on insulin and standardized evaluation of insulin pump caregivers during in-hospital use of insulin pump therapy are significant. Nevertheless, non-endocrinology healthcare professionals have limited knowledge of the working principles and operational procedures of insulin pumps and also experience in the management of DM due to the limitations of the specialty.
The knowledge of insulin pumps was low among nurses who participated in this study. Another study of DM liaison nurses in China revealed that even DM liaison nurses had a poor KAP of insulin pumps.13 Therefore, if DM liaison nurses had a low KAP of the insulin pump,13 it could be expected that nurses not directly involved in DM care would have even lower scores, as observed in the present study. According to the KAP theory, spreading knowledge about insulin pumps was an essential measure that would contribute significantly to the correct implementation of insulin pump operation and management since there were several models available.10 Nevertheless, the results indicate that the nurse training is not strong enough. From a clinical point of view, since the knowledge component of nurses in the survey was low, safety issues probably arose during the use of insulin pumps.28 Although such events were not analyzed in the present study, future studies should look at correlations between insulin pump KAP and safety issues.
In terms of attitudes, the oncology nurses had the lowest score. For example, some nurses answered that they never inform the supervising physician and the endocrinology nurse when hyperglycemia (≥ 16.7 mmol/L, a critical bedside value1) occurs. It was probably related to individual nurses’ limited understanding of specialist techniques. Therefore, provided that the number of years of service cannot be changed, the knowledge of clinical nurses in non-DM specialties can be improved by developing effective and targeted training about DM and insulin pumps.
In terms of practice, on the practice scale for insulin pump use, pediatric nurses had the lowest score, which could be related to a limited understanding of specialist techniques. Insulin pumps are increasingly used in many departments in China but not in specific practice and management.29 The results of this study helped express that nurses should standardize the management of insulin pumps, assess current knowledge about insulin pumps as it relates to an individual’s healthcare role, and assist in identifying training programs needed for hospital-wide education programs to ensure the successful implementation of glucose-lowering regimens using insulin pumps. Despite the limited knowledge of insulin pump management compared to clinical best practices, the survey highlighted the most important areas of concern and provided a platform to successfully create targeted training programs before optimizing current glycemic protocols and providing a basis for developing a reasonable and effective insulin pump training program.
To our knowledge, this study investigated KAP towards insulin pumps among non-endocrinology nurses in southern China for the first time. However, this study also had some limitations. Even though the sample size was large, the results apply to a single region in China. In addition, the KAP questionnaire was self-made and probably reflected the local practice, with limited generalizability. Convenience sampling was used, which can result in bias. Safety events were not examined during the study period.
In conclusion, there was limited knowledge regarding insulin pumps among nurses, although they had a positive attitude and attached importance to the management of insulin pumps. Training programs should be implemented to improve the knowledge of non-endocrinology nurses about insulin pump application.
Data Sharing Statement
All data generated or analyzed during this study are included in this published article.
Ethics Approval and Consent to Participate
The research was carried out in accordance with the Declaration of Helsinki. The study was approved by the ethics committee of The First People’s Hospital of Foshan [# Ren Shenyan (2022) No. 143]. All participants signed the informed consent form prior to the study.
Author Contributions
Xiaohua Lu and Yan Zhou are co-corresponding authors. All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all these areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work. It was revised in the manuscript.
Funding
Research Talent Cultivation Fund Project of School of Nursing, Jinan University (JHA20230604).
Disclosure
The authors declare that they have no competing interests.
References
1. American Diabetes Association. Introduction: standards of medical care in diabetes-2022. Diabetes Care. 2022;45(Suppl 1):S1–S2. doi:10.2337/dc22-Sint
2. Chatterjee S, Khunti K, Davies MJ. Type 2 diabetes. Lancet. 2017;389(10085):2239–2251. doi:10.1016/S0140-6736(17)30058-2
3. Zhou B, Lu Y, Hajifathalian K; Collaboration NCDRF. Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet. 2016;387(10027):1513–1530. doi:10.1016/S0140-6736(16)00618-8
4. Yan Y, Wu T, Zhang M, Li C, Liu Q, Li F. Prevalence, awareness and control of type 2 diabetes mellitus and risk factors in Chinese elderly population. BMC Public Health. 2022;22(1):1382. doi:10.1186/s12889-022-13759-9
5. Wang L, Peng W, Zhao Z, et al. Prevalence and treatment of diabetes in China, 2013–2018. JAMA. 2021;326(24):2498–2506. doi:10.1001/jama.2021.22208
6. Yuan H, Li X, Wan G, et al. Type 2 diabetes epidemic in East Asia: a 35-year systematic trend analysis. Oncotarget. 2018;9(6):6718–6727. doi:10.18632/oncotarget.22961
7. McAllister DA, Read SH, Kerssens J, et al. Incidence of hospitalization for heart failure and case-fatality among 3.25 million people with and without diabetes mellitus. Circulation. 2018;138(24):2774–2786. doi:10.1161/CIRCULATIONAHA.118.034986
8. Alshehri KA, Altuwaylie TM, Alqhtani A, Albawab AA, Almalki AH. Type 2 diabetic patients adherence towards their medications. Cureus. 2020;12(2):e6932. doi:10.7759/cureus.6932
9. Nimri R, Nir J, Phillip M. Insulin pump therapy. Am J Ther. 2020;27(1):e30–e41. doi:10.1097/MJT.0000000000001097
10. Berget C, Messer LH, Forlenza GP. A clinical overview of insulin pump therapy for the management of diabetes: past, present, and future of intensive therapy. Diabetes Spectr. 2019;32(3):194–204. doi:10.2337/ds18-0091
11. Dajkovich G, Barkley TW Jr. Understanding insulin pump therapy. J Community Health Nurs. 2015;32(3):131–140. doi:10.1080/07370016.2015.1057064
12. McCrea D. Management of the hospitalized diabetes patient with an insulin pump. Crit Care Nurs Clin North Am. 2013;25(1):111–121. doi:10.1016/j.ccell.2012.11.010
13. Zhou W, Huang J, Yang L, et al. Long-term training in diabetes-related knowledge, attitudes, and self-reported practice among diabetes liaison nurses. J Int Med Res. 2020;48(2):300060519882838. doi:10.1177/0300060519882838
14. Kaisen AR, Parkosewich JA, McAvoy KH, Bak LB, Knobf MT. “Finding the balance”: a qualitative study of the experience of nurses and patients with diabetes on an insulin pump in the hospital. Diabetes Educ. 2020;46(6):587–596. doi:10.1177/0145721720964587
15. Strini V, Schiavolin R, De Barbieri I, Prendin A. The perceptions and experience of the diabetic person with an insulin pump: a review of the literature. Acta Biomed. 2021;92(S2):e2021502. doi:10.23750/abm.v92iS2.11506
16. Umpierrez GE, Hellman R, Korytkowski MT, et al. Management of hyperglycemia in hospitalized patients in non-critical care setting: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2012;97(1):16–38. doi:10.1210/jc.2011-2098
17. Pickup J. Insulin pumps. Int J Clin Pract Suppl. 2011;170:16–19. doi:10.1111/j.1742-1241.2010.02574.x
18. Klonoff DC, Reyes JS. Insulin pump safety meeting: summary report. J Diabetes Sci Technol. 2009;3(2):396–402. doi:10.1177/193229680900300224
19. AbdulAziz YH, Al-Sallami HS, Wiltshire E, et al. Insulin pump initiation and education for children and adolescents - a qualitative study of current practice in New Zealand. J Diabetes Metab Disord. 2019;18(1):59–64. doi:10.1007/s40200-019-00390-6
20. Benkhadra K, Alahdab F, Tamhane SU, McCoy RG, Prokop LJ, Murad MH. Continuous subcutaneous insulin infusion versus multiple daily injections in individuals with type 1 diabetes: a systematic review and meta-analysis. Endocrine. 2017;55(1):77–84. doi:10.1007/s12020-016-1039-x
21. Yeh HC, Brown TT, Maruthur N, et al. Comparative effectiveness and safety of methods of insulin delivery and glucose monitoring for diabetes mellitus: a systematic review and meta-analysis. Ann Intern Med. 2012;157(5):336–347. doi:10.7326/0003-4819-157-5-201209040-00508
22. Pickup JC, Yemane N, Brackenridge A, Pender S. Nonmetabolic complications of continuous subcutaneous insulin infusion: a patient survey. Diabetes Technol Ther. 2014;16(3):145–149. doi:10.1089/dia.2013.0192
23. Sweeney TJ, Kenny DJ, Schubert CC. Inpatient insulin pump therapy: assessing the effectiveness of an educational program. J Nurses Prof Dev. 2013;29(2):84–89. doi:10.1097/NND.0b013e318286c5da
24. Deiss D, Adolfsson P, Alkemade-van Zomeren M, et al. Insulin infusion set use: European perspectives and recommendations. Diabetes Technol Ther. 2016;18(9):517–524. doi:10.1089/dia.2016.07281.sf
25. Heinemann L, Fleming GA, Petrie JR, Holl RW, Bergenstal RM, Peters AL. Insulin pump risks and benefits: a clinical appraisal of pump safety standards, adverse event reporting, and research needs: a joint statement of the European Association for the Study of Diabetes and the American Diabetes Association Diabetes Technology Working Group. Diabetes Care. 2015;38(4):716–722. doi:10.2337/dc15-0168
26. Xu J, Zhu M, Wei HE. Model and effects of interdisciplinary team cooperation in meticulous glycemic management for patients receiving insulin pump therapy in non-endocrine department. Chin Nurs Manag. 2018;18(8):1021–1024.
27. Tao J, Huang G, Gao L. Practice of reducing adverse events of insulin pump in non-endocrinology department. Chin Nurs Manag. 201919:725–729.
28. Thompson B, Leighton M, Korytkowski M, Cook CB. An overview of safety issues on use of insulin pumps and continuous glucose monitoring systems in the hospital. Curr Diab Rep. 2018;18(10):81. doi:10.1007/s11892-018-1056-7
29. Huo L, Deng W, Lan L, et al. Real-world application of insulin pump therapy among patients with type 1 diabetes in China: a Cross-Sectional Study. Front Endocrinol. 2022;13:891718. doi:10.3389/fendo.2022.891718
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
