Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 17
Impact of Spirometrically Confirmed Chronic Obstructive Pulmonary Disease on Arterial Stiffness and Surfactant Protein D After Percutaneous Coronary Intervention. The CATEPOC Study
Authors Malik K, Diaz-Coto S, de la Asunción Villaverde M, Martinez-Camblor P, Navarro-Rolon A, Pujalte F, De la Sierra A, Almagro P
Received 8 May 2022
Accepted for publication 9 September 2022
Published 14 October 2022 Volume 2022:17 Pages 2577—2587
DOI https://doi.org/10.2147/COPD.S373853
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Russell
Komal Malik,1 Susana Diaz-Coto,2 Maria de la Asunción Villaverde,1 Pablo Martinez-Camblor,3,4 Annie Navarro-Rolon,5,6 Francisco Pujalte,6 Alejandro De la Sierra,1 Pere Almagro1
1Internal Medicine Service, University Hospital Mútua de Terrassa, University of Barcelona, Barcelona, Spain; 2Epidemiology Department, Geisel School of Medicine at Dartmouth, Hanover, NH, USA; 3Department of Anesthesiology, Dartmouth-Hitchcock Medical Center, Lebanon, NH, USA; 4Faculty of Health Sciences, Universidad Autonoma de Chile, Providencia, 7500912, Chile; 5Pneumology Service, University Hospital Mútua de Terrassa, University of Barcelona, Barcelona, Spain; 6Immunology Department, Catlab Laboratory, Barcelona, Spain
Correspondence: Pere Almagro, Email [email protected]
Background: Several mechanisms have been proposed to explain why chronic obstructive pulmonary disease (COPD) impairs the prognosis of coronary events. We aimed to explore COPD variables related to a worse prognosis in patients undergoing percutaneous coronary intervention (PCI).
Methods: Patients with an acute coronary event treated by PCI were prospectively included. One month after discharge, clinical characteristics, comorbidities measured with the Charlson index, and prognostic coronary scales (logistic EuroSCORE; GRACE 2.0) were collected. Post-bronchodilator spirometry, arterial stiffness, and serum inflammatory and myocardial biomarkers were measured. Lung plasmatic biomarkers (Surfactant protein D, desmosine, and Clara cell secretory protein-16) were determined with ELISA. COPD was defined by the fixed ratio (FEV1/FVC < 70%). Spirometric values were also analyzed as continuous variables using adjusted and non-adjusted ANCOVA analysis. Finally, we evaluated the presence of a respiratory pattern defined by non-stratified spirometric values and pulmonary biomarkers.
Results: A total of 164 patients with a mean age of 65 (± 10) years (79% males) were included. COPD was diagnosed in 56 (34%) patients (68% previously undiagnosed). COPD patients had a longer smoking history, higher scores on the EuroSCORE (p < 0.0001) and GRACE 2.0 (p < 0.001) scales, and more comorbidities (p = 0.006). Arterial stiffness determined by pulse wave velocity was increased in COPD patients (7.35 m/s vs 6.60 m/s; p = 0.006). Serum values of high sensitive T troponin (p = 0.007) and surfactant protein D (p = 0.003) were also higher in COPD patients. FEV1% remained significantly associated with arterial stiffness and surfactant protein D in the adjusted ANCOVA analysis. In the cluster exploration, 53% of the patients had a respiratory pattern.
Conclusion: COPD affects one-third of patients with an acute coronary event and frequently remains undiagnosed. Several mechanisms, including arterial stiffness and SPD, were increased in COPD patients. Their relationship with the prognosis should be confirmed with longitudinal follow-up of the cohort.
Keywords: acute coronary event, chronic obstructive pulmonary disease, ischaemic heart disease, percutaneous coronary intervention, arterial stiffness, surfactant protein D
Introduction
According to the Global Burden of Disease Study data, ischaemic heart disease (IHD) and chronic obstructive pulmonary disease (COPD) are the first and third causes of global mortality for chronic diseases.1 Their joint prevalence exceeds that expected for their shared risk factors and impairs the prognosis of subjects affected by the two pathologies.2 In COPD patients, the prevalence of IHD is two-fold higher than that observed in the general population, while a third of patients with IHD have COPD.3–6 Several previous studies have shown that IHD accounts for a third of COPD deaths and suggest that COPD increases coronary events and cardiovascular mortality risk.7–10
An essential component of COPD is the presence of airway obstruction defined by a spirometric fixed ratio FEV1/FVC lower than 0.7. Without spirometric data, COPD underdiagnosis reaches figures of 70% in both general populations and IHD patients.2,3,11 Hence, the relevance of COPD in studies performed on IHD patients without spirometric tests is challenging to assess. Although some studies suggest that COPD worsens the prognosis after an acute coronary event, nearly all of them had a retrospective design, and the diagnosis of COPD was based only on clinical criteria without any pulmonary function data.12 Previous studies of IHD patients have shown that this approach has a very low sensitivity (23%).13 Moreover, the reported COPD prevalence in these studies is around 10% compared to the 30% observed in IHD patients with spirometric evaluation.14–16 Therefore, it seems likely that in studies without pulmonary function data, two-thirds of COPD patients were undiagnosed and hence analyzed as non-COPD.
In a recent meta-analysis performed to evaluate the prognostic relevance of COPD after a percutaneous coronary intervention (PCI), only one of the ten studies included had a prospective design with spirometric confirmation of COPD.12 The follow-up of this cohort showed an increased risk of new coronary events and cardiovascular mortality in COPD patients, independent of IHD treatment.15,17
Furthermore, the relationship between pulmonary function and cardiovascular risk is non-dichotomic. FEV1/FVC is a continuous variable that usually descends progressively during the evolution of the disease. Some patients may have significant radiologic lung pathology and symptoms before reaching the accepted threshold of airway obstruction, and the incidence of cardiovascular events increases progressively with pulmonary function impairment.18–21 More recent studies have shown that even in the absence of rapid pulmonary function loss (the primary mechanism traditionally related to COPD development), some subjects with incomplete lung development in early adulthood present an earlier incidence of COPD and cardiovascular comorbidities.22,23
Multiple variables have been proposed to explain the increased risk of cardiovascular events in COPD patients, including arterial stiffness and inflammatory, cardiac, and respiratory biomarkers.24–34 However, their association in patients with a coronary event and concomitant COPD remains unclear.35,36
Our main objective was to explore the differences between patients with and without COPD in several variables previously considered relevant to explain the risk of new coronary events in those with IHD treated by PCI. Differences in lung function data were analyzed as continuous variables and dichotomized according to the fixed ratio (FEV1/FVC <0.7). Finally, we aimed to investigate the existence of respiratory clusters based on the combination of non-dichotomized lung function parameters and serum pulmonary biomarkers.
Methods
We prospectively studied patients admitted due to an acute coronary event diagnosed and treated by PCI at the University Hospital Mutua de Terrassa. Our study accomplishes the criteria of the Declaration of Helsinki. The ethical and clinical trial committee of the Mutua de Terrassa University Hospital approved the study, and all patients signed the informed consent form. Only patients with a significant coronary obstruction (>50%) in the main coronary arteries and attending the follow-up visit were included. The reason for performing PCI, the number of arteries stenosed and treated, and the left ventricular ejection fraction were recorded. Logistic EuroSCORE and Global Registry of Acute Coronary Events (GRACE 2.0) risk scores were calculated after PCI, while the complexity of coronary artery disease was evaluated using the SYNTAX 1.0 score.37–39
A month after discharge, all patients completed a standardized questionnaire including cardiovascular and respiratory variables. A complete physical examination was performed. The Charlson index was used to measure comorbidities.40 Scores on the Charlson index represent clinical history previous to the coronary event and spirometry.
Evaluation of Arterial Stiffness
Arterial stiffness was determined in the follow-up visit through two different methods. First, carotid-femoral pulse wave velocity (cfPWV) was measured by applanation tonometry using a Sphygmocor Xcel device (AtCor Medical Pty Ltd). Augmentation index (AIx), central systolic pressure, and central pulse pressure were also calculated with the Sphigmocor device. Aix measures the supplementary increase in blood pressure during systole due to the reflection of the forward-travelling pressure waves from the peripheral circulation.41 Secondly, the cardio-ankle vascular index (CAVI) was obtained using a VaSera 1500 (Fukuda Denshi, Tokyo) device. CAVI measures arterial stiffness using extrapolated brachial-ankle pulse and ankle/brachial index (ABI) values.42
Evaluation of Pulmonary Function
Postbronchodilator spirometry was performed according to international guidelines after evaluation of arterial stiffness.43 Airway obstruction was diagnosed using the fixed ratio (FEV1/FVC <0.7), while obstruction severity was stratified according to FEV1% predicted values from the Global Obstructive Lung Disease (GOLD) thresholds.44 COPD diagnosis was confirmed by airway obstruction and compatible clinical criteria. A separate analysis was made using continuous values of lung function (FEV1, FVC, and FEV1/FVC).
Evaluation of Blood and Urine Biomarkers
A fasting blood sample was obtained in the follow-up visit. Red and white blood cell count, renal and hepatic function, inflammatory serum parameters [high sensitivity C reactive protein (Hs-CRP) and fibrinogen], cardiac biomarkers [brain natriuretic peptides (NT-proBNP), high sensitivity troponin (Hs-TNT)], and urine albumin-creatinine ratio in urine sample were measured with standard routine methods. In a subgroup of patients, surfactant protein D (SPD), desmosine, and Clara cell secretory protein-16 (CC-16) were analyzed with ELISA immunoassay (DYNEX technologies).
Statistical Analysis
Data are presented as means ± standard deviation (S.D.) for symmetric continuous variables or as medians and interquartile ranges for non-symmetric continuous variables. Because of its strongly asymmetric distribution, the albumin-creatinine ratio was log-transformed and expressed as the geometrical mean. Differences were compared with robust Welch’s t-test or non-parametric Wilcoxon test. Frequency distribution (number and percentages) was provided for qualitative variables. The Chi-2 test or the Fisher exact test was used to compare proportions.
We performed an ANCOVA analysis to study the association between unstratified lung function and the rest of the variables. In this analysis, FEV1% and FEV1/FVC analyzed as continuous variables were the dependent factors, while the rest of the measures–adjusted for age and gender–were the independent variables. Coefficients and 95% confidence intervals were reported.
Finally, to explore the latent groups of patients based on their respiratory profile, including non-stratified lung function values and biomarkers of pulmonary damage, we used hierarchical unsupervised learning algorithms based on the combination of FEV1%, FVC%, FEV1/FVC, CC-16, SPD, and package-years. In this analysis, the chained equation for multivariate imputation was used to replace missing values (R package mice used with this goal). A case-complete approach is provided as supplementary material. The numbers of groups were determined after a visual inspection of the resulting dendrogram. A forest plot describing the mean and 95% confidence intervals of the standardized measures represents the differences among the resulting groups. R (www.r-project.org) was used for statistical analysis. Two-sided p-values are provided, and those below 0.05 were considered significant.
Results
A total of 170 patients were evaluated during the follow-up visit. Of these, six were excluded (4 for non-valid spirometry and 2 with coronary obstruction below 50%). The mean age of patients included was 65 ±10 years, and 79% were males. The main reasons for performing PCI were myocardial infarction without ST-elevation (NSTEMI) in 70 (42.7%), myocardial infarction with ST-elevation (STEMI) in 67 (40.9%), and unstable angina in 27 (16.5%). Respiratory biomarkers (CC-16, Desmosine and SPD) were obtained in 101 (61.6%) patients. No differences were observed between patients with and those without respiratory biomarker determination regarding age, FEV1%, FEV1/FVC, cfPWV, CAVI, Charlson index, Hs-TNT, NT-proBNP, or Hs-CRP.
Prevalence and Previous Underdiagnosis of COPD
A total of 56 (34.1%) patients met the spirometric criteria for COPD, according to the fixed ratio (FEV1/FVC <0.7). Thirty-eight (67.9%) had not been previously diagnosed. All of them presented clinical criteria compatible with COPD. Eight patients classified with COPD were never smokers; none of them had asthma or bronchiectasis as the predominant disease. Four had a previous diagnosis of COPD. In the rest, the symptoms, radiological findings, and subsequent spirometries were compatible with the diagnosis.
According to the GOLD spirometric criteria, nineteen (33.9%) had mild COPD, twenty-five (44.6%) had moderate COPD, and twelve (21.5%) had severe or very severe airway obstruction. Two patients with severe COPD had not been previously diagnosed, while a lack of a previous diagnosis accounted for 76% and 89% of those with moderate or mild COPD (Figure 1). Respiratory biomarkers were available for 35 (62.5%) COPD patients and 66 (61.1%) (p = 0.862) non-COPD patients.
 |
Figure 1 Flowchart of participants, COPD prevalence, and underdiagnosis levels according to the fixed ratio (FEV1/FVC <0.7). |
Differences Between COPD and Non-COPD Patients According to the Fixed Ratio
Compared to non-COPD patients, those with COPD diagnosed by fixed ratio were older, with greater tobacco history, and higher logistic EuroSCORE and GRACE 2.0 score (Table 1). COPD patients had more comorbidities measured by adjusted and non-adjusted Charlson indexes and presented peripheral arterial disease (p = 0.035) and arrhythmias (p = 0.012) more frequently (Table S1; Supplementary Material). According to the fixed ratio, no other demographic or clinical characteristics differed significantly between patients with and those without COPD.
 |
Table 1 Differences in Demographic and Clinical Characteristics of Patients with and without COPD |
Measures of Arterial Stiffness
As shown in Table 2, cfPWV was significantly higher in COPD compared to non-COPD patients: 7.35 m/s (IQR: 6.40–8.70) vs 6.60 m/s (IQR: 5.73–7.88) (p = 0.006). Likewise, CAVI was also higher in COPD patients: 9.70 (IQR: 8.63–10.80) vs 9.01 (IQR: 8.40–9.99) (p = 0.023). Other values of central hemodynamics, such as central systolic, pulse pressure, and AIx, did not differ between patients with and those without COPD. cfPWV and CAVI measures were moderately correlated [rho = 0.18; p = 0.043 (95% CI: 0.005–0.038)], and both were related with FEV1% and FEV1/FVC values. Figure S1 (Supplementary material). Since carotid-femoral wave velocity is correlated with age and blood pressure values, we performed a logistic regression analysis adjusted for age and central blood pressure. In this analysis pulse wave velocity and age remained statistically significant [PWV (p = 0.022); age (p = 0.001), central blood pressure (p = 0.058)]. Given that the CAVI index is independent of blood pressure, we did not perform additional adjustment analysis.
 |
Table 2 Descriptive Statistics for Arterial Stiffness, Analytic Parameters, and Serum Biomarkers for the Total Cohort Stratified by COPD Diagnosis |
Biomarkers
In the analysis of serum biomarkers, COPD patients had higher serum values of Hs-TNT: 14.19 (IQR: 10.28–24.26) ng/mL vs 10.97 (IQR: 7.42–18.06) ng/mL (p = 0.007) and SPD: 19.64 (IQR: 15.01–26.01) ng/mL vs 14.71 (IQR: 11.67–18.39) ng/mL (p = 0.003) (Table 2).
ANCOVA Analysis
ANCOVA analysis was used to explore the association between FEV1/FVC ratio and FEV1% values expressed as continuous values in relation to the rest of the variables. In this analysis, FEV1% was significantly associated with cfPWV, Hs-TNT, Hs-CRP, SPD, GRACE, and the non-adjusted Charlson index. FEV1/FVC ratio was associated with cfPWV, Hs-TNT, EuroSCORE, GRACE, and non-adjusted Charlson index.
After adjusting for age and gender, FEV1% remained significantly associated with cfPWV, Hs-CRP, SPD, and Charlson index, while FEV1/FVC was associated with cfPWV, SYNTAX, and Charlson index (Table 3).
 |
Table 3 Standardized Beta Coefficient for the Unadjusted and Adjusted (Age and Gender) Models. ANCOVA Analysis |
Cluster Analysis
Finally, we performed a cluster analysis to explore the existence of different subgroups among the patients according to pulmonary variables, including respiratory function continuous values (FEV1%, FVC%, and FEV1/FVC ratio) and serum biomarkers of lung damage (SPD and CC-16). This analysis did not include desmosine due to the lack of significance in the previous explorations. Three clusters of patients were identified after an exploratory visualization of the dendrogram, although one had a small number of patients (5). (Figure 2) The other two clusters included 82 and 77 patients. The first of these was characterized by a respiratory pattern with decreased pulmonary function values, higher accumulated smoking history, increased inflammatory serum parameters (Hs-CRP and fibrinogen), and SPD in blood serum, and augmented values of arterial stiffness measured with cfPWV (Figure 3; Tables 4 and Table S2 Supplementary Material). The case-complete analysis is shown in the supplementary material (Table S3; Figure S3 Supplementary Material).
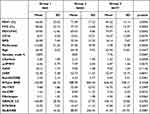 |
Table 4 Differences in Relevant Variables According to Cluster Group |
 |
Figure 2 Dendrogram according to pulmonary related measures (FEV1%, FEV1/FVC, SPD and CC-16). |
 |
Figure 3 Forest plot with mean and 95% confidence interval comparison between selected variables stratified by clusters. |
Discussion
Our results demonstrate that after an acute coronary event treated by PCI, arterial stiffness, Hs-TNT, and SPD are increased in COPD patients, even those without a previous COPD diagnosis. SPD and cfPWV remain significantly related to unstratified postbronchodilator FEV1% after adjustment for age and gender. Moreover, in the cluster analysis, nearly half of the patients present a respiratory pattern defined by lower lung function parameters and higher serum biomarkers of pulmonary damage (SPD and CC-16).
The COPD prevalence observed in our cohort (34%) is similar to that reported in prospective studies performed on IHD patients after spirometric evaluation, both in stable conditions and after PCI.14–17,45 This prevalence drops to around 10% in retrospective cohorts without lung function data, suggesting that in these studies, two-thirds of COPD patients were non-diagnosed and consequently analyzed as non-COPD.12,13 To our knowledge, only one prospective study performed on patients treated by PCI and with spirometric evaluation has demonstrated that COPD patients—with or without a previously known diagnosis—have a higher number of new coronary events and increased mortality after median follow-up of 3 and 6 years.15,17
Given the lack of previous prospective studies with confirmed COPD in this population, the reasons for this adverse prognosis remain unclear.2 Our study is an attempt to explore possible mechanisms to explain the worse evolution after a PCI procedure in COPD patients. IHD and COPD share an increased prevalence of classic cardiovascular risk factors, including arterial hypertension, diabetes mellitus, dyslipidemia, smoking, and low-grade systemic inflammation.3,6,46 More recently, other variables, such as arterial stiffness and myocardial or pulmonary serum biomarkers, have been related to a worse prognosis in patients with IHD or COPD.
Arterial stiffness is a significant predictor of cardiovascular events in the general population and in patients with established IHD.26 The most widely validated method for evaluating arterial stiffness is pulse wave velocity, measured between the carotid and femoral arteries.26,28,41 Greater values for cfPWV reflect impairment of aortic distensibility, which is associated with arterial ageing and atherosclerosis.41,47,48 An alternative way to calculate arterial stiffness is the cardio-ankle vascular index, which uses extrapolated values from the ascending aorta to the ankle arteries.29,42 Previous studies have shown that arterial stiffness is inversely related to lung function parameters and is a predictor of 3-year mortality in COPD patients.27,28,48
Similarly, in several prospective cohorts, arterial stiffness measured with cfPWV or CAVI was an independent predictor of major cardiovascular events in IHD patients treated by PCI.29,33,49–51 Arterial stiffness measured by other methods such as magnetic resonance or arteriography was also related to new coronary events, stent occlusion, and decreased survival after an acute coronary event.52–54 Regrettably, in none of these studies was pulmonary function explored. In our cohort, cfPWV and CAVI were increased in patients with IHD and COPD, offering a possible explanation for the increased risk of cardiovascular events in COPD patients.
Hs-TNT and SPD were also increased in our study in COPD patients. Hs-TNT measures cardiomyocyte damage and is related to the risk of cardiovascular death both in patients with a coronary event and in the general population.55,56 Higher values of Hs-TNT have also been related to COPD patients’ prognosis in the stable phase and after an acute exacerbation.30,56 In a cohort study performed on patients with severe exacerbations of COPD and elevated levels of troponins at admission, coronary angiography showed significant coronary stenosis in 67% of patients, suggesting an imbalance between coronary flow and oxygen demand.57
SPD is a highly lung-specific glycoprotein secreted by type-2 pneumocytes, and it is also expressed in the endothelium of the cardiovascular system. Serum levels of SPD are increased in COPD patients, and these high levels have been associated in longitudinal studies with increased cardiovascular mortality.25,58 Circulating SPD levels are also a strong independent predictor of 10-year cardiovascular mortality in patients referred for selective coronary angiography, although, again, lung function was not assessed in this cohort.32
Beyond lung function, arterial stiffness, troponins, and SPD are correlated.33,59 A longitudinal study performed on COPD patients has shown that arterial stiffness and troponins increase simultaneously during acute exacerbations of COPD compared with their values in the stable phase.34 Similarly, SPD values are also increased during COPD exacerbations and are related to arterial stiffness.58,59
Inflammatory biomarkers (Hs-CRP and fibrinogen) are associated with the risk of cardiovascular events in the general population, and they predict mortality in patients with IHD or COPD.24,25,60,61 In our study, no differences in inflammatory biomarkers were found between COPD and non-COPD patients defined according to the fixed ratio. However, Hs-CRP was related significantly to airway obstruction measured by post-bronchodilator FEV1% values after adjusting for age and gender.
Finally, in the cluster analysis, a 53% of included patients had a respiratory pattern characterized by a combination of non-dichotomized lung function values and serum pulmonary biomarkers, suggesting that pulmonary damage may be more frequent than previously reported in this population.
Our study has several limitations. First, it was performed in a single centre, and in predominantly male patients. This low percentage of women in IHD patients treated by PCI is similar to that reported in similar cohorts with spirometric confirmation.14,16 It may be partially explained by the underuse of PCI in women with an acute coronary event.62,63 Finally, our study assessed variables previously recognized as being related to IHD patients’ prognosis, but the follow-up was insufficient to confirm their relationship with new coronary events and mortality.
In conclusion, our results confirm the high prevalence of COPD in patients treated by PCI and the increased values of arterial stiffness and serum biomarkers in COPD patients. Their relationship with the occurrence of new coronary events and mortality should be confirmed with longitudinal follow-up of the cohort.
Acknowledgments
The authors thank Tom Yohannan for medical editing services.
Funding
This study was supported by a grant from the Fundacion Mutua de Terrassa (FMTBE0128) and SEPAR (SEPAR 506-2018).
Disclosure
The authors declare that they have no conflict of interest in this article.
References
1. Wang H, Naghavi M, Allen C, et al. Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980–2015: a systematic analysis for the Global Burden of Disease Study 2015. Lancet. 2016;388(10053):1459–1544.
2. Almagro P, Boixeda R, Diez-Manglano J, Gómez-Antúnez M, López-García F, Recio J. Insights into chronic obstructive pulmonary disease as critical risk factor for cardiovascular disease. Int J Chron Obstruct Pulmon Dis. 2020;15:755–764. doi:10.2147/COPD.S238214
3. Chen W, Thomas J, Sadatsafavi M, FitzGerald JM. Risk of cardiovascular comorbidity in patients with chronic obstructive pulmonary disease: a systematic review and meta-analysis. Lancet Respir Med. 2015;3(8):631–639.
4. Putcha N, Drummond MB, Wise RA, Hansel NN. Comorbidities and chronic obstructive pulmonary disease: prevalence, influence on outcomes, and management. Semin Respir Crit Care Med. 2015;36(4):575–591.
5. Müllerova H, Agusti A, Erqou S, Mapel DW. Cardiovascular comorbidity in COPD: systematic literature review. Chest. 2013;144(4):1163–1178.
6. Mapel DW, Dedrick D, Davis K. Trends and cardiovascular comorbidities of COPD patients in the veterans administration medical system, 1991–1999. COPD. 2005;2:35–41.
7. Anthonisen NR, Connett JE, Enright PL, Manfreda J. Hospitalizations and mortality in the Lung Health Study. Am J Respir Crit Care Med. 2002;166:333–339.
8. Anthonisen NR, Skeans M, Wise R, Manfreda J, Kanner RE, Connett JE. The effects of a smoking cessation intervention on 14.5-year mortality. Ann Intern Med. 2005;142(4):233–239.
9. McGarvey LP, John M, Anderson JA, Zvarich M, Wise RA. Ascertainment of cause-specific mortality in COPD: operations of the TORCH Clinical Endpoint Committee. Thorax. 2007;62(5):411–415.
10. Donaldson G, Hubbard R, Wedzicha JA. Increased risk of myocardial infarction and stroke following exacerbation of COPD. Chest. 2010;137(5):1091–1097. doi:10.1378/chest.09-2029
11. Almagro P, Soriano JB. Underdiagnosis in COPD: a battle worth fighting. Lancet Respir Med. 2017;5(5):5. doi:10.1016/S2213-2600(17)30133-9
12. Bundhun PK, Gupta C, Xu GM. Major adverse cardiac events and mortality in chronic obstructive pulmonary disease following percutaneous coronary intervention: a systematic review and meta-analysis. BMC Cardiovasc Disord. 2017;17(1):1–13. doi:10.1186/s12872-017-0622-2
13. Mooe T, Stenfors N. The prevalence of COPD in individuals with acute coronary syndrome: a spirometry-based screening study. COPD. 2014;2555:1–9.
14. Franssen FME, Soriano JB, Roche N, et al. Lung function abnormalities in smokers with ischemic heart disease. Am J Respir Crit Care Med. 2016;194(5):568–576. doi:10.1164/rccm.201512-2480OC
15. Almagro P, Lapuente A, Pareja J, et al. Underdiagnosis and prognosis of chronic obstructive pulmonary disease after percutaneous coronary intervention: a prospective study. Int J Chron Obstruct Pulmon Dis. 2015;10:43.
16. Soriano JB, Rigo F, Guerrero D, et al. High prevalence of undiagnosed airflow limitation in patients with cardiovascular disease. Chest. 2010;137(2):333–340. doi:10.1378/chest.09-1264
17. Almagro P, De la Sierra A, Acosta E, et al. Spirometrically confirmed chronic obstructive pulmonary disease worsens long-term prognosis after percutaneous coronary intervention. Am J Respir Crit Care Med. 2018;197(6):824. doi:10.1164/rccm.201707-1389LE
18. Regan EA, Lynch DA, Curran-Everett D, et al. Clinical and radiologic disease in smokers with normal spirometry. JAMA Intern Med. 2015;175(9):1539–1549. doi:10.1001/jamainternmed.2015.2735
19. Woodruff PG, Barr RG, Bleecker E, et al. Clinical significance of symptoms in smokers with preserved pulmonary function. N Engl J Med. 2016;374(19):1811–1821. doi:10.1056/NEJMoa1505971
20. Ramalho SHR, Shah AM. Lung function and cardiovascular disease: a link. Trends Cardiovasc Med. 2021;31(2):93–98. doi:10.1016/j.tcm.2019.12.009
21. Cheng Y-J, Chen Z-G, Li Z-Y, Mei W-Y, Bi W-T, Luo D-L. Longitudinal change in lung function and subsequent risks of cardiovascular events: evidence from four prospective cohort studies. BMC Med. 2021;19(1):1. doi:10.1186/s12916-021-02023-3
22. Agustí A, Noell GM, Brugada J, et al. Lung function in early adulthood and health in later life: a transgenerational cohort analysis. Lancet Respir Med. 2017;5(12):935–945. doi:10.1016/S2213-2600(17)30434-4
23. Celli BR, Wedzicha JA. Update on clinical aspects of chronic obstructive pulmonary disease. N Engl J Med. 2019;381(13):1257–1266.
24. Emerging risk factors collaboration. C-reactive protein, fibrinogen, and cardiovascular disease prediction. N Engl J Med. 2012;367(14):1310–1320.
25. Celli BR, Locantore N, Yates J, et al. Inflammatory biomarkers improve clinical prediction of mortality in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2012;185(10):1065–1072.
26. Ben-Shlomo Y, Spears M, Boustred C, et al. Aortic pulse wave velocity improves cardiovascular event prediction: an individual participant meta-analysis of prospective observational data from 17,635 subjects. J Am Coll Cardiol. 2014;63(7):636–646.
27. Fisk M, McEniery CM, Gale N, et al. Surrogate markers of cardiovascular risk and chronic obstructive pulmonary disease. Hypertension. 2018;71(3):499–506.
28. Crim C, Anderson JA, Calverley PMA, et al. Pulse wave velocity in chronic obstructive pulmonary disease and the impact of inhaled therapy (SUMMIT): a randomized double-blind clinical trial. Am J Respir Crit Care Med. 2020;201(10):1307–1310.
29. Kirigaya J, Iwahashi N, Takahashi H, et al. Impact of cardio-ankle vascular index on long-term outcome in patients with acute coronary syndrome. J Atheroscler Thromb. 2020;27(7):657–668.
30. Pavasini R, D’Ascenzo F, Campo G, et al. Cardiac troponin elevation predicts all-cause mortality in patients with acute exacerbation of chronic obstructive pulmonary disease: systematic review and meta-analysis. Int J Cardiol. 2015;191:187–193.
31. Pavasini R, Tavazzi G, Biscaglia S, et al. Amino terminal pro brain natriuretic peptide predicts all-cause mortality in patients with chronic obstructive pulmonary disease: systematic review and meta-analysis. Chron Respir Dis. 2017;14(2):117–126.
32. Hill J, Heslop C, Man SFP, et al. Circulating surfactant protein-D and the risk of cardiovascular morbidity and mortality. Eur Heart J. 2011;32(15):1918–1925.
33. Siasos G, Oikonomou E, Maniatis K, et al. Prognostic significance of arterial stiffness and osteoprotegerin in patients with stable coronary artery disease. Eur J Clin Invest. 2018;48(3):e12890.
34. Patel AR, Kowlessar BS, Donaldson GC, et al. Cardiovascular risk, myocardial injury, and exacerbations of chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2013;188(9):1091–1099.
35. Zemans RL, Jacobson S, Keene J, et al. Multiple biomarkers predict disease severity, progression and mortality in COPD. Respir Res. 2017;18(1):117.
36. Serban KA, Pratte KA, Bowler RP. Protein biomarkers for COPD outcomes. Chest. 2021;159(6):2244–2253.
37. Coluccia V, Burzotta F, Romagnoli E, et al. EuroSCORE predicts long-term mortality of unselected patients undergoing percutaneous coronary interventions. Int J Cardiol. 2013;167(4):1232–1236.
38. Fox KA, FitzGerald G, Puymirat E, et al. Should patients with acute coronary disease be stratified for management according to their risk? Derivation, external validation and outcomes using the updated GRACE risk score. BMJ Open. 2014;4(2):e004425.
39. Sianos G, Morel MA, Kappetein AP, et al. The SYNTAX Score: an angiographic tool grading the complexity of coronary artery disease. EuroIntervention. 2005;1(2):219–227.
40. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383.
41. Butlin M, Qasem A. Large artery stiffness assessment using SphygmoCor technology. Pulse. 2016;4(4):180–192.
42. Matsushita K, Ding N, ED Kim, et al. Cardio-ankle vascular index and cardiovascular disease: systematic review and meta-analysis of prospective and cross-sectional studies. J Clin Hypertens. 2019;21(1):16–24.
43. Miller MR, Hankinson J, Brusasco V, et al. Standardization of spirometry. Eur Respir J. 2005;26(2):319–338.
44. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary diseases (2022 report). Global initiative for chronic obstructive Pulmonary Disease (GOLD). Available from: https://goldcopd.org/2022-gold-reports-2/.
45. Khassawneh BY, Samrah SM, Jarrah MI, et al. Prevalence of undiagnosed COPD in male patients with coronary artery disease: a cross-sectional study in Jordan. Int J Chron Obstruct Pulmon Dis. 2018;13:2759–2766.
46. Finkelstein J, Cha E, Scharf SM. Chronic obstructive pulmonary disease as an independent risk factor for cardiovascular morbidity. Int J Chron Obstruct Pulmon Dis. 2009;4:337–349.
47. Vivodtzev I, Tamisier R, Baguet JP, Borel JC, Levy P, Pépin JL. Arterial stiffness in COPD. Chest. 2014;145(4):861–875. doi:10.1378/chest.13-1809
48. Zaigham S, Östgren CJ, Persson M, et al. The association between carotid-femoral pulse-wave velocity and lung function in the Swedish CArdioPulmonary bioImage study (SCAPIS) cohort. Respir Med. 2021;185:106504.
49. Fang Y, Zhong Q. Investigation of the value of carotid-femoral pulse wave velocity and coronary artery lesions in prognosis of percutaneous coronary intervention patients. Am J Transl Res. 2021;13(6):6646.
50. Chen BW, Wang ZG, Liu Q, Wang X, Dang A. Combination of pulse wave velocity with clinical factors as a promising tool to predict major adverse cardiac events after percutaneous coronary intervention. J Cardiol. 2015;65(4):318–323.
51. Park HW, Kang MG, Kim K, et al. Prognostic value of brachial-ankle pulse wave velocity in patients with non-ST-elevation myocardial infarction. Coron Artery Dis. 2017;28(8):642–648.
52. Lechner I, Reindl M, Tiller C, et al. Determinants and prognostic relevance of aortic stiffness in patients with recent ST-elevation myocardial infarction. Int J Cardiovasc Imaging. 2022;38(1):237–247.
53. Feistritzer HJ, Klug G, Reinstadler SJ, et al. Prognostic value of aortic stiffness in patients after ST-elevation myocardial infarction. J Am Heart Assoc. 2017;6:9.
54. Prskalo Z, Brizić I, Markota D, et al. Arterial stiffness in patients with coronary artery disease: relation with in-stent restenosis following percutaneous coronary intervention. BMC Cardiovasc Disord. 2016;16:1. doi:10.1186/S12872-016-0305-4
55. Aimo A, Georgiopoulos G, Panichella G, et al. High-sensitivity troponins for outcome prediction in the general population: a systematic review and meta-analysis. Eur J Intern Med. 2022;98:61–68.
56. Adamson PD, Anderson JA, Brook RD, et al. Cardiac troponin I and cardiovascular risk in patients with chronic obstructive pulmonary disease. J Am Coll Cardiol. 2018;72(10):1126–1137.
57. Pizarro C, Herweg-Steffens N, Buchenroth M, et al. Invasive coronary angiography in patients with acute exacerbated COPD and elevated plasma troponin. Int J Chron Obstruct Pulmon Dis. 2016;11:2081–2089.
58. Nandy D, Sharma N, Senapati S. Systematic review and meta-analysis confirms significant contribution of surfactant protein D in chronic obstructive pulmonary disease. Front Genet. 2019;10:339.
59. Labonté LE, Bourbeau J, Daskalopoulou SS, et al. Club Cell-16 and RelB as novel determinants of arterial stiffness in exacerbating COPD patients. PLoS One. 2016;11(2):e0149974.
60. Carrero JJ, Andersson Franko M, Obergfell A, Gabrielsen A, Jernberg T. hsCRP level and the risk of death or recurrent cardiovascular events in patients with myocardial infarction: a healthcare-based study. J Am Heart Assoc. 2019;8(11):e012638.
61. Ernst E, Resch KL. Fibrinogen as a cardiovascular risk factor: a meta-analysis and review of the literature. Ann Intern Med. 1993;118:956–963.
62. Jackson J, Alkhalil M, Ratcovich H, Wilkinson C, Mehran R, Kunadian V. Evidence base for the management of women with non-ST elevation acute coronary syndrome. Heart. 2022:3:34.
63. Khan E, Brieger D, Amerena J, et al. Differences in management and outcomes for men and women with ST-elevation myocardial infarction. Med J Aust. 2018;209(3):118–123.
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
