Back to Journals » International Journal of Chronic Obstructive Pulmonary Disease » Volume 17
Disability Retirement After First Admission with Acute Exacerbation of Chronic Obstructive Pulmonary Disease: A Danish Nationwide Registry Cohort Study Using a Retrospective Follow-Up Design
Authors Jacobsen PA , Kragholm K , Torp-Pedersen C , Møller Weinreich U
Received 9 June 2022
Accepted for publication 12 September 2022
Published 11 October 2022 Volume 2022:17 Pages 2541—2551
DOI https://doi.org/10.2147/COPD.S377311
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Dr Richard Russell
Peter Ascanius Jacobsen,1,2 Kristian Kragholm,2,3 Christian Torp-Pedersen,4 Ulla Møller Weinreich1,2
1Department of Respiratory Diseases, Aalborg University Hospital, Aalborg, Denmark; 2The Clinical Institute, Aalborg University, Aalborg, Denmark; 3Department of Cardiology, Aalborg University Hospital, Aalborg, Denmark; 4Department of Clinical Research, Hillerød Hospital, Hillerød, Denmark
Correspondence: Peter Ascanius Jacobsen, Department of Respiratory Diseases, Aalborg University Hospital, Mølleparkvej 4, Aalborg, DK-9100, Denmark, Tel +4597664800, Email Mail:[email protected]
Introduction: Many chronic obstructive pulmonary disease (COPD) patients below retirement age are outside the workforce. The existing knowledge about association between acute exacerbation of COPD (AECOPD) and disability retirement is limited.
Aim: The aim of this study is to explore disability retirement in COPD patients 3 years following first-ever AECOPD.
Methods: This retrospective registry-based follow-up cohort study design is based on nationwide Danish registry data. Patients admitted to the hospital for the first time between 1999 and 2017 with AECOPD and age between 35 and 59 years, active in the workforce, were included in the study. Socio-demographics, comorbidities and inhaled medication use were explored. COPD patients’ hazard ratio of disability retirement during 3-year follow-up was calculated. Cox regression was used to examine the effects of covariates on disability retirement.
Results: A total of 4032 patients were included in the study. During follow-up, 17.2% (692/4032) experienced disability retirement from the workforce. Factors associated with disability retirement were expressed as hazard ratio (95% confidence intervals): Higher age (ref. age 46– 50: Age 51– 55, 1.42, (1.12– 1.81); age 56– 59, 1.37 (1.08– 1.74)); living alone (1.34 (1.14– 1.56)); number of comorbidities for 1, 2, and 3 comorbidities (1.36 (1.14– 1.62), 1.57 (1.19– 2.07), 1.77 (1.20– 2.60)); emphysema (2.01 (1.44– 2.79)); depression (1.60 (1.12– 2.28)); cardiac comorbidity (1.38 (1.07– 1.78)); triple inhalation therapy (2.76 (2.20– 3.47)); ICS + LAMA or ICS + LABA treatment (1.82 (1.48– 2.23)); and ICS treatment (1.49 (1.17– 1.90)). Higher educational level was associated with a significantly reduced risk of disability retirement, medium, short higher and long higher educational level, relative to low education level (0.78 (0.67– 0.91), 0.63 (0.48– 0.83) and 0.27 (0.12– 0.60)).
Conclusion: Patients vulnerable to disability retirement are patients with markers of severe COPD, comorbidities, and social vulnerability.
Keywords: chronic obstructive pulmonary disease, return to work, early retirement, comorbidities
Introduction
Approximately 47–70% of the COPD patients below retirement age are not working.1–3 In addition to poor workforce connection, COPD patients also have poorer performance at work and more days off work, compared to healthy individuals.4 The poor workforce performance comes with high indirect socio-economic expenses, eg, lost tax revenue and increased public support.5,6 Early retirement/disability retirement benefit has previously been associated with increased readmission and mortality rates.7
Previous studies that explored factors associated with COPD patients being outside the workforce have found that older age, lower education level, more breathlessness, and high exposure to vapours, gasses, dust, and fumes, low exercise capacity as well as increased airflow obstruction were associated with being outside the workforce.1,3,4 Smoking has prospectively been associated with a higher likelihood of disability retirement.8–10 However, the knowledge on how AECOPD affects patients’ workforce connection and to which extent the acute exacerbation event leads to permanent detachment from the workforce is not well established in the literature. Understanding how AECOPD affects workforce connection and what precedes detachment will help identify vulnerable individuals in the COPD population.
The aim of this study is therefore to examine the characteristics of patients who during a 3-year follow-up period become disability retirement beneficiaries following first AECOPD.
Method
Study Setting
The Danish welfare system provides free health care for all citizens and provides social benefits to citizens who are incapacitated from participating in the workforce. These benefits, among others, include unemployment benefits, disability pension, sickness benefit, voluntary early retirement, and regular retirement pension for all citizens. Information on each Danish citizen is recorded by the Danish Civil Personal Registration number unique to each citizen.
Study Design
This study is a nationwide retrospective register-based cohort study from 1999 to 2017 with access to data on the entire Danish population. Employment data and Cause of Death Registry data were available until December 31, 2020.
Study Population
The study population consisted of first-time admissions to the hospital with AECOPD. Patients who were employed prior to admission and alive 30 days after hospital admission were included. Patients receiving sickness benefit 3 out of 4 weeks prior to admission were excluded since AECOPD would not likely be the source of detachment in this group.
Exclusion criteria were as follows: A previous diagnosis of asthma; age below 35 to limit misclassification of COPD in case of actual asthma; age above 59 were excluded to eliminate patients leaving the workforce due to regular retirement pension at age 65 and patients leaving the workforce due to voluntary early retirement, which during the observation period was possible in Denmark from the age of 60. Individuals with missing data on covariates were excluded.
Follow-up started 4 weeks after admission, as registration of public payment of sickness benefit starts with ≥4 weeks of sickness leave in the Danish public support system.
Data Sources
The Danish Civil Personal Registration number was used to identify patients across different Danish national registries containing information on all Danish citizens.11 Access to the Danish National Patient Registry was available which contains ICD-10 diagnosis codes for all contacts with Danish hospitals, both outpatient and admission.12 Furthermore, we obtained data on time of death through the Danish Cause of Death Registry;13 psychiatric diagnoses were obtained through the Danish Central Psychiatry Registry; age and sex were obtained through the Danish Civil Personal Registration System; employment status was obtained through the Danish National Labour Market Registry (the DREAM database) which records all public social support received on a weekly basis,14 and redeemed medication prescriptions were obtained through the Danish National Prescription Registry which records information on all redeemed prescriptions from Danish pharmacies.15 Highest achieved educational level and cohabitation status were extracted from registries administered by the Statistics of Denmark.
Variable Definitions
AECOPD
AECOPD was defined as an ICD-10 code COPD (DJ44), excluding DJ448B chronic asthmatic bronchitis as primary diagnosis, or a combination of respiratory failure (DJ96) or pneumonia (DJ13-18) with a COPD diagnosis (defined as above) as a secondary diagnosis within 30 days of admission.16 This definition of AECOPD has previously been confirmed with a positive predictive value of 92% in the Danish patient registry.16
Workforce Connection
Employment was defined as being self-supported or on certain types of public support related to being part of the workforce (eg, education support, see Table S1). The support classified as being part of the workforce was included due to their time-limited nature and an expectation of these patients becoming part of the workforce after the support ends.
Disability retirement included benefits only available to people with significant and lasting impaired ability to work (see Table S1).
The date of admission for AECOPD was used to calculate time to disability retirement from the workforce, using data form the DREAM database. If individuals did not receive disability retirement, they were recorded as no event and with 3-year follow-up.
Covariates
Covariates included patients’ age, sex, cohabitation status, income, educational level, and inhalation medication use (prescriptions redeemed 6 months prior to admission indicating actual medication used). Comorbidity count was created using comorbidities included in the Charlson comorbidity score, comorbidities mentioned in Global Initiative for Chronic Obstructive Pulmonary Disease (GOLD) guidelines, comorbidities included in the COPD-specific comorbidity test (COTE) index and depression (see Table S2).17–19 Comorbidities were recorded 5 years prior to admission from the Danish National Patient Registry. Both the Danish National Patient Registry and the Danish National Prescription Registry were used for identification of diabetes, anxiety and depression using the medication ATC codes “A10, Drugs used in diabetes”, “N05B, Anxiolytics”, and “N06A, Antidepressants”, respectively (see Table S2). Hypertension was defined as a redemption of two anti-hypertensive drug groups (eg, diuretic and anti-adrenergic) twice within 6 months from AECOPD admission, to exclude misclassification of other cardiovascular diseases (see Table S2).
Inhalation medication usage was recorded 6 months prior to admission. The 6 months recording of redeemed prescriptions were used to create exclusive inhalation medication groups where included individuals were only able to be in one group (No inhalation medication, ICS, “LAMA or LABA”, “LAMA + ICS or LABA + ICS”, “LAMA + LABA”, triple therapy or SABA only).
Educational level was divided in four educational levels (short, medium, short higher and long higher education) according to International Standard Classification of Education (ISCED): 0–2 (early childhood education level to lower secondary education level (short)), 3 (upper secondary education level (medium)), 5–6 (short-cycle tertiary education level to bachelor or equivalent level (short higher)), and 7–8 (masters/doctoral degree or equivalent (long higher)).20 ISCED level 4 is not included since it does not exist in the Danish education system. Age was for the purpose of analysis grouped in age intervals 35–45, 46–50, 51–55, 56–59 to avoid linearity problems in the Cox regression.
Statistical Analysis
Continuous variables were reported using means with standard deviations (SD), where data were normally distributed, and medians with 25th–75th percentile [IQR], when data deviated from the normal distribution. Categorical variables were presented using counts and percentages. Cox regression was used to explore 3-year hazard of disability retirement.
Patients dying during follow-up were treated as competing risks in the analyses due to individuals dying being unable to receive disability retirement. Early voluntary retirement was similarly treated as a competing risk, as it does not necessarily indicate a functional decline and a change to disability retirement is highly unlikely. The competing risk hazard ratios (HRs) for death from the Cox regression of disability retirement is reported separately.
One explorative Cox regression model was created including age group, sex, educational level, and cohabitation status, number of comorbidities, comorbidities mentioned in the GOLD guidelines with ischemic heart disease, atrial fibrillation/flutter, and heart failure combined to one cardiac comorbidity variable and inhalation medication use.17 Number of comorbidities and specific comorbidities were not included in the model at the same time.
Return to work, defined as the above-mentioned employment definition, following AECOPD was tracked for the purpose of identifying individuals not returning to work between their first admission with AECOPD and disability retirement.
SAS version 9.4 (SAS Institute Inc., Cary, NC, USA) and R version 3.4.1 were used for data management and statistical analysis.
Results
Patients
Inclusion and exclusion of patients is shown in Figure 1.
 |
Figure 1 Flowchart of patient inclusion. |
Characteristics
Baseline characteristics are shown in Table 1.
 |
Table 1 Baseline Data on Population |
Disability Retirement
The cumulative incidence of disability retirement is displayed in Figure 2. During the 3-year follow-up, 17.2% (693/4032) of patients experienced disability retirement from the workforce. In addition, 4.7% (190/4032) died during the follow-up without receiving disability retirement prior to the time of death. Among those that were granted disability retirement 29.1% (202/693) did not return to work between their admission and disability retirement benefit.
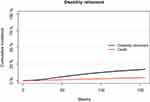 |
Figure 2 Cumulative incidence of disability retirement. |
Cox regression analysis of disability retirement is shown in Figure 3. Significant higher hazard ratios were observed with higher age, higher number of comorbidities, emphysema, depression, cardiac comorbidity, and more advanced inhalation medication treatment step. A somewhat dose response of number of comorbidity and inhalation medication treatment step is observed. Significantly lower hazard ratios are observed with lower age, and longer educational level with an indication of a lower hazard the longer the education.
The competing risk analysis of mortality is shown in Figure 4. Significant higher hazard ratios were observed with male sex, higher age, living alone, more comorbidity, emphysema, and cancer.
Discussion
In this nationwide study of 4032 first-time AECOPD 30-day survivors, between year 1999 and year 2017 in Denmark, disability retirement was seen for 17.2% with 4.7% dying without disability retirement during the three-year follow-up period. Increased risk of disability retirement was seen in patients with higher age, more comorbidities, living alone, more advanced treatment and shorter educational level.
Only 12% of the patients admitted with AECOPD between 1999 and 2017 were between 35 and 59 years old. The demographic distribution of the patients’ first time admission were relatively comparable to that seen in the study by Balcell et al who found a mean first admission age of 67.5 SD (8.5) which corresponds to 15.8% below 59 years of age.21 The differences seen may be explained by different inclusion/exclusion criteria between the studies.
It is noteworthy that 70% of the patients were outside the workforce at first AECOPD admission, similar to what was found by Fletcher et al.2 Other studies have found that 47–60%, of COPD patients are outside the workforce.1,3 We must suspect that the admitted patients are amongst the more vulnerable part of the population. It indicates that interventions targeting workforce connection in COPD patients should be implemented earlier than at the time of first admission with AECOPD.
More than one-fourth of the patients experiencing disability retirement during the three-year follow-up did not return to work after AECOPD. This may indicate that the event of first admission with AECOPD initiates some patients’ way towards disability retirement even though the cumulative incidence does not indicate a steep rise following first admission. An explanation of why the cumulative incidence does not increase steeply following AECOPD is most likely that the process of being awarded disability retirement is long, and includes testing of working abilities, in the Danish social system. However, the steady increase may also indicate that the event is of less importance than the chronic development in disease severity. As such, the main driver of the detachment still needs further exploration.
Not surprisingly, the HR of disability retirement was higher at higher age, as is seen with other medical conditions.22,23 Disability retirements correlation with age may be explained by increasing ages association with a higher likelihood of physical impairment.24
Higher educational level was associated with a favorable workforce connection. This supports the existing knowledge on the negative effect of short education levels on exacerbation rate and mortality in Denmark.25 The negative association between short educational level and workforce attachment may be difficulties carrying out manual labour, which is more prevalent in people with shorter education.26 Data on what type of work (manual vs desk work) individuals were employed in, were unfortunately not available. In addition, patients with shorter educational level often have low ability to cope with stress, especially in those with chronic somatic diseases.27 Earlier interventions towards shorter educated groups are therefore necessary to maintain their workforce connection.
Emphysema’s association with poor outcome may be a proxy of more severe disease. It may also be that this phenotype of COPD patients has a poorer workforce connection. Depression was also associated with increased disability retirement, but surprisingly, anxiety, well known to have negative impact on COPD patients’ health-related quality of life and mortality, was not negatively associated with disability retirement.28,29 Both the Psychiatric Registry and the Prescription Database only contained a low number of patients with anxiety and depression. This may therefore be very under-diagnosed in the Danish population, as seen in other studies.30 Anxiety may therefore still be a cause of workforce detachment in COPD and a pro-active approach in diagnostics and treatment has previously been suggested beneficial.31
Cardiac comorbidity’s association with an increased hazard of disability retirement is supported by the existing literature on cardiac diseases effect on disability retirement.32 Somewhat surprisingly, cancer is not significantly associated with disability retirement. This may be due to the age of the patients included in this analysis, as the prevalence of cancer increases with age, also in COPD patients.33 However, in the competing risk of death analysis it is also seen that cancer is associated with an increased mortality, which may explain the limited impact of cancer in COPD patients on disability retirement.
The significant competing risk of death estimates are as expected. Male sex and higher age are generally associated with mortality.34 More comorbidities and the specific comorbidities of cancer and cardiac comorbidity is also not surprisingly associated with increased mortality as they are well-known causes of death also in younger individuals.35,36
Inhaler therapy was associated with increased HR for workforce detachment. Inhaled medication use is most likely a proxy of disease severity and not an actual negative effect of the medicine on workforce attachment. During the observational period several different recommendations for treatment of COPD with inhaled medicine have existed.17,37–40 However, frequent AECOPD has always been an indication for ICS. It is therefore not surprising that it carries the strongest indication for workforce detachment, as AECOPDs in themselves are associated with morbidity and reduced health-related quality of life.41 Common to all treatment recommendations have been that the lower the lung function and the more symptomatic the patient is, the more inhaled therapies were added to the treatment. These effects are seen in the treatment combinations with ICS having the highest HR. The study furthermore identifies a need for better adherence and earlier initiation of treatment, with 41% of individual off treatment at first admission to the hospital. This frequency is high, however not improbable. Previous studies found 5% of the patients non-adherent to medication, 32% with poor adherence and 36% of the COPD patients admitted for the first time due to an acute exacerbation receive their diagnosis at admission.21,25
Strengths and Limitations
The study uses Nationwide Danish registries including patients over an 18-year period. This makes the study comprehensive in exploring disability retirement during a 3-year follow-up period and would be difficult to perform in a prospective study setting with the same number of patients included. The epidemiologic registry design leaves some desirable variables missing, eg, smoking, spirometry, home oxygen usage, non-invasive ventilation usage, dyspnea score, six-minute walk distance, and labour type.
The study only looked at AECOPD admissions and is therefore compiled of the most severe exacerbations. This makes the study less suitable to evaluate the magnitude of COPD patients outside the workforce in general.
The choice of excluding all patients with a previous diagnosis of asthma may have excluded some patients with COPD. As such, to secure that only COPD patients were included we may have reduced the size of our cohort. A proportion of patients in this study had received ICS-treatment only. Misclassification of asthmatic patients is of course also a possible explanation; however, these patients were primarily included before 2006, see Figure S1. The number of different types of inhaled medicine for COPD patients were limited before this and mono-therapy with ICS was still considered a possible treatment option.42 As the validity of the diagnosis used in the study is high16 and patients with a previous asthma diagnosis were excluded it is less likely that misclassification is the major driver of this observation.
SSRI was used to categorize patients as having depression in the current study, but we acknowledge the possibility of it being used for anxiety. Furthermore, benzodiazepines were used to characterize anxiety patients; however, in some, these may be used to treat insomnia. The total number of patients with anxiety and depression is still low, with prevalence estimates of 10–42% for depression and 10–19% for anxiety in the general COPD population, indicating a large undertreatment of mental comorbidities.43
The interpretation of the associations seen in the Cox regression models with comorbidity is limited by the quality of the National Patient Registry. Comorbidity such as cancer recording is likely complete due to the diagnosis primarily being established in a hospital setting. Comorbidity such as emphysema may be underreported since the emphysema mush have been severe enough to warrant the diagnosis established in a hospital setting. This ensures diagnosis relevance but may cause some under-recording.
In conclusion, disability retirement from the workforce occurred in 17% of the patients. Detachment happens steadily over time with increased hazard ratio in patients with higher age, comorbidities, more advanced inhalation medication treatment step, shorter educational level and in those living alone.
Data Sharing Statement
Data are available from the respective registries, and access is granted by the data responsible institute (The Capital Region of Denmark). For inquiries about the data extracted contact corresponding author Peter A. Jacobsen.
Ethics Approval and Informed Consent Statement
Ethical approval is not needed in Denmark for retrospective registry studies according to the Scientifical Ethical Committees Act §14 section 2. Access to data was granted by the data responsible institute (The Capital Region of Denmark, project id: P2019-402) where informed consent is not required in accordance with the Data Protection Act §10.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This research received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Disclosure
Dr Christian Torp-Pedersen reports grants from Bayer, grants from Novo Nordisk, during the conduct of the study. The authors report no other conflicts of interest in this work.
References
1. Rai KK, Jordan RE, Siebert WS., et al. Birmingham COPD Cohort: a cross-sectional analysis of the factors associated with the likelihood of being in paid employment among people with COPD. Int J COPD. 2017;12:233–242. doi:10.2147/COPD.S119467
2. Fletcher MJ, Upton J, Taylor-Fishwick J, et al. COPD uncovered: an international survey on the impact of chronic obstructive pulmonary disease [COPD] on a working age population. BMC Public Health. 2011;11(1):612. doi:10.1186/1471-2458-11-612
3. Jacobsen PA. Characteristics and treatable traits of patients with chronic obstructive pulmonary disease (COPD) with and without paid employment. Respir Res. 2021;22(1):147. doi:10.1186/s12931-021-01736-6
4. Rai KK, Adab P, Ayres JG, Jordan RE. Systematic review: chronic obstructive pulmonary disease and work-related outcomes. Occupational Med. 2018;68(2):99–108. doi:10.1093/occmed/kqy012
5. Patel JG, Nagar SP, Dalal AA. Indirect costs in chronic obstructive pulmonary disease: a review of the economic burden on employers and individuals in the United States. Int J COPD. 2014;9:289–300. doi:10.2147/COPD.S57157
6. Wacker ME, Jörres RA, Schulz H, et al. Direct and indirect costs of COPD and its comorbidities: results from the German COSYCONET study. Respir Med. 2016;111:39–46. doi:10.1016/j.rmed.2015.12.001
7. Jacobsen PA, Kragholm KH, Torp-Pedersen C, Janssen DJA, Spruit MA, Weinreich UM. Employment status, readmission and mortality after acute exacerbation of COPD. Int J Chron Obstruct Pulmon Dis. 2021;16:2257–2265. doi:10.2147/COPD.S319840
8. Koskenvuo K, Broms U, Korhonen T, et al. Smoking strongly predicts disability retirement due to COPD: the Finnish Twin Cohort Study. Eur Respir J. 2011;37(1):26–31. doi:10.1183/09031936.00008910
9. Husemoen LL, Osler M, Godtfredsen NS, Prescott E. Smoking and subsequent risk of early retirement due to permanent disability. Eur J Public Health. 2004;14(1):86–92. doi:10.1093/eurpub/14.1.86
10. Claessen H, Arndt V, Drath C, Brenner H. Smoking habits and occupational disability: a cohort study of 14,483 construction workers. Occup Environ Med. 2010;67(2):84–90. doi:10.1136/oem.2009.046318
11. Schmidt M, Pedersen L, Sorensen HT. The Danish Civil Registration System as a tool in epidemiology. Eur J Epidemiol. 2014;29(8):541–549. doi:10.1007/s10654-014-9930-3
12. Schmidt M, Schmidt SA, Sandegaard JL, Ehrenstein V, Pedersen L, Sorensen HT. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol. 2015;7:449–490. doi:10.2147/CLEP.S91125
13. Helweg-Larsen K. The Danish Register of Causes of Death. Scand J Public Health. 2011;39(7 Suppl):26–29. doi:10.1177/1403494811399958
14. Hjollund NH, Larsen FB, Andersen JH. Register-based follow-up of social benefits and other transfer payments: accuracy and degree of completeness in a Danish interdepartmental administrative database compared with a population-based survey. Scand J Public Health. 2007;35(5):497–502. doi:10.1080/14034940701271882
15. Kildemoes HW, Sorensen HT, Hallas J. The Danish National Prescription Registry. Scand J Public Health. 2011;39(7 Suppl):38–41. doi:10.1177/1403494810394717
16. Thomsen RW, Lange P, Hellquist B, et al. Validity and underrecording of diagnosis of COPD in the Danish National Patient Registry. Respir Med. 2011;105(7):1063–1068. doi:10.1016/j.rmed.2011.01.012
17. From the Global Strategy for the Diagnosis. Management and Prevention of COPD. Global Initiative for Chronic Obstructive Lung Disease (GOLD); 2019.
18. Charlson ME, Pompei P, Ales KL, Mackenzie CR, New A. Method of classifying prognostic co-morbidity in longitudinal-studies - development and validation. J Chronic Dis. 1987;40(5):373–383. doi:10.1016/0021-9681(87)90171-8
19. Divo M, Cote C, de Torres JP, et al. Comorbidities and risk of mortality in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 2012;186(2):155–161. doi:10.1164/rccm.201201-0034OC
20. UNESCO Institute for Statistics: International Standard Classification of Education ISCED 2011, Montréal, 2012.
21. Balcells E, Anto JM, Gea J, et al. Characteristics of patients admitted for the first time for COPD exacerbation. Respir Med. 2009;103(9):1293–1302. doi:10.1016/j.rmed.2009.04.001
22. Smedegaard L, Nume AK, Charlot M, Kragholm K, Gislason G, Hansen PR. Return to work and risk of subsequent detachment from employment after myocardial infarction: insights from Danish nationwide registries. J Am Heart Assoc. 2017;6:10. doi:10.1161/JAHA.117.006486
23. Hagen KB, Tambs K, Bjerkedal T, Prospective Cohort A. Study of risk factors for disability retirement because of back pain in the general working population. Spine. 2002;27(16):1790–1796. doi:10.1097/00007632-200208150-00019
24. Chiu C-J, Wray LA. Physical disability trajectories in older americans with and without diabetes: the role of age, gender, race or ethnicity, and education. Gerontologist. 2010;51(1):51–63. doi:10.1093/geront/gnq069
25. Tottenborg SS, Lange P, Johnsen SP, Nielsen H, Ingebrigtsen TS, Thomsen RW. Socioeconomic inequalities in adherence to inhaled maintenance medications and clinical prognosis of COPD. Respir Med. 2016;119:
26. Kontio T, Viikari-Juntura E, Solovieva S. To what extent do education and physical work load factors explain occupational differences in disability retirement due to knee OA? A nationwide register-based study in Finland. BMJ Open. 2019;8(11):e023057. doi:10.1136/bmjopen-2018-023057
27. Janowski K, Kurpas D, Kusz J, Mroczek B, Jedynak T. Emotional control, styles of coping with stress and acceptance of illness among patients suffering from chronic somatic diseases. Stress Health. 2014;30(1):34–42. doi:10.1002/smi.2493
28. Atlantis E, Fahey P, Cochrane B, Smith S. Bidirectional associations between clinically relevant depression or anxiety and COPD: a systematic review and meta-analysis. Chest. 2013;144(3):766–777. doi:10.1378/chest.12-1911
29. Omachi TA, Katz PP, Yelin EH, et al. Depression and health-related quality of life in chronic obstructive pulmonary disease. Am J Med. 2009;122(8):778 e9–15. doi:10.1016/j.amjmed.2009.01.036
30. Yohannes AM, Alexopoulos GS. Depression and anxiety in patients with COPD. Eur Respir Rev. 2014;23(133):345–349. doi:10.1183/09059180.00007813
31. Panagioti M, Scott C, Blakemore A, Coventry PA. Overview of the prevalence, impact, and management of depression and anxiety in chronic obstructive pulmonary disease. Int J Chron Obstruct Pulmon Dis. 2014;9:1289–1306. doi:10.2147/COPD.S72073
32. Lunde ED, Fonager K, Joensen AM, et al. Association between newly diagnosed atrial fibrillation and work disability (from a nationwide Danish cohort study). Am J Cardiol. 2022;169:64–70. doi:10.1016/j.amjcard.2021.12.039
33. van de Schans SA, Janssen-Heijnen ML, Biesma B, et al. COPD in cancer patients: higher prevalence in the elderly, a different treatment strategy in case of primary tumours above the diaphragm, and a worse overall survival in the elderly patient. Eur J Cancer. 2007;43(15):2194–2202. doi:10.1016/j.ejca.2007.08.011
34. Oksuzyan A, Juel K, Vaupel JW, Christensen K. Men: good health and high mortality. Sex differences in health and aging. Aging Clinical and Experimental Research. 2008;20(2):91–102. doi:10.1007/BF03324754
35. Christiansen MN, Kober L, Weeke P, et al. Age-specific trends in incidence, mortality, and comorbidities of heart failure in Denmark, 1995 to 2012. Circulation. 2017;135(13):1214–1223. doi:10.1161/CIRCULATIONAHA.116.025941
36. Flanders WD, Lally CA, Zhu B-P, Henley SJ, Thun MJ. Lung cancer mortality in relation to age, duration of smoking, and daily cigarette consumption: results from Cancer Prevention Study II. Cancer Res. 2003;63(19):6556–6562.
37. From the Global Strategy for the Diagnosis. Management and Prevention of COPD. Global Initiative for Chronic Obstructive Lung Disease (GOLD); 2006.
38. From the Global Strategy for the Diagnosis. Management and Prevention of COPD. Global Initiative for Chronic Obstructive Lung Disease (GOLD); 2011.
39. From the Global Strategy for the Diagnosis. Management and Prevention of COPD. Global Initiative for Chronic Obstructive Lung Disease (GOLD); 2001.
40. From the Global Strategy for the Diagnosis. Management and Prevention of COPD. Global Initiative for Chronic Obstructive Lung Disease (GOLD); 2017.
41. Anzueto A. Impact of exacerbations on COPD. Eur Respir Rev. 2010;19(116):113–118. doi:10.1183/09059180.00002610
42. Fitzgerald MF, Fox JC. Emerging trends in the therapy of COPD: bronchodilators as mono- and combination therapies. Drug Discov Today. 2007;12(11–12):472–478. doi:10.1016/j.drudis.2007.04.003
43. Maurer J, Rebbapragada V, Borson S, et al. Anxiety and depression in COPD: current understanding, unanswered questions, and research needs. Chest. 2008;134(4Suppl):43S–56S. doi:10.1378/chest.08-0342
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.


