Back to Journals » Psychology Research and Behavior Management » Volume 15
Development of the Nurse Occupational Stigma Scale
Authors Yang L , Zhang S, Leng J, Fan Z , Luo Y
Received 24 March 2022
Accepted for publication 28 June 2022
Published 2 July 2022 Volume 2022:15 Pages 1627—1636
DOI https://doi.org/10.2147/PRBM.S362709
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Igor Elman
Lu Yang,1 Shuangxin Zhang,1 Jiaqi Leng,2 Zhiguang Fan,2 Yi Luo1
1Department of Nursing, Changchun University of Chinese Medicine, Changchun City, Jilin Province, People’s Republic of China; 2Department of Education, Jilin International Studies University, Changchun City, Jilin Province, People’s Republic of China
Correspondence: Zhiguang Fan, Department of Education, Jilin International Studies University, Jingyue Street 3658, Changchun City, Jilin Province, People’s Republic of China, Tel +86 1 594-831-4623, Fax +86 431-84924101, Email [email protected]
Introduction: Occupational stigma toward nurses exerts a negative impact on the physical and mental health and work performance of nurses. However, hitherto, there has been no quantitative instrument designed to assess occupational stigma toward nurses.
Objective: The present study aimed to develop the Nurse Occupational Stigma Scale (NOSS) and test its reliability and validity in the Chinese context.
Methods: The items of the scale were formed through the open-ended interview and literature review. A questionnaire survey was administered among 765 patients using NOSS and the Caring Behaviors Inventory (CBI-24).
Results: In the initial questionnaire, a total of 21 items were developed, and 5 items were dropped for cross-loadings. The formal scale consists of 16 items divided into three dimensions of negative label, nurse-patient relationship, and devaluation and discrimination. The results of confirmatory factor analysis (CFA) indicated that the three-factor model fitted well (χ2/df=2.635, RMSEA=0.064, RFI=0.926, CFI=0.962, NFI=0.941, IFI=0.953). The total scores of the NOSS and the scores of all dimensions were significantly negatively correlated with the scores of the CBI-24. The internal consistency coefficients of the scale and all dimensions were between 0.827– 0.920, and the split-half reliability coefficients were between 0.826– 0.942. The NOSS had the measurement invariance across gender.
Conclusion: With its good reliability and validity, the NOSS can be an appropriate instrument for researchers to conduct studies about nurse occupational stigma.
Keywords: nurse, occupational stigma, reliability, validity
Introduction
As the important component of healthcare system, nurses play a pivotal role in improving medical care and maintaining people’s health.1 It was found in previous studies that nurses not only help alleviate patients’ pain,2 but also help cultivate patients’ positive attitude and improve their life quality.3 However, influenced by the content, nature, environment and cultural concept of nursing,4,5 nurses may suffer the effects of stigma.
During the Protestant Reformation, nursing was undertaken by untrained and inexperienced people. During this period, people usually associated nurses with the negative label of “humble servant” and “vulgarity”.6 Nursing was also considered a humble occupation.7 Until the Crimean War, Florence Nightingale effectively ameliorated the healthcare work of military hospitals with her professionalism and dedication.8 In addition, she put forward scientific nursing theory and nursing education, created modern nursing, reversed people’s negative evaluation of nursing, and improved the occupational status of nurses.9
However, the stigmatizing remarks against nurses still exist to date. Occupational stigma toward nurses refers to the negative label and negative evaluation attached by the public to the occupational behavior, characteristics, and social status of nurses, and nurse-patient relationship.10,11 For individuals, stigma is composed of three basic components: cognition, emotion, and behavior. Cognition reflects public negative opinions and evaluation of nurses. Negative emotional and behavioral responses can be elicited by negative beliefs about nurses. For example, if nurses’ attitude toward patients is regarded as indifferent, patients may have an aversion to the nurses, thus inducing verbal abuse and irrational violence.
Early studies on occupational stigma paid more attention to “dirty work” such as funeral and mortuary operators,12 tour guides and construction workers.13,14 These occupations are stigmatized mainly due to their physical, social, and moral stains.7 The work of any occupation can be tainted to a certain extent, consequently causing the practitioners to suffer stigma.15 Nurses may also encounter stigmatization, although they are regarded as highly prestigious, respectable, and trustworthy by the public.16 By contrast, the nurses who are on night shift, in contact with strangers and in “dirty” work suffer more stigma. For example, the nurses in emergency departments often need to be exposed to death, dress a wound and deal with vomit, which may lead to people’s avoidance of them.
Occupational stigma can shape and influence public opinions on and attitude toward nurses. Nurses internalizing public stigma as a part of self-evaluation can lead to self-stigma,17 with the manifestation of self-depreciation and self-blame in cognition, and negative label driven actions in behavior. In general, the negative results of occupational stigma can be divided into three aspects: the impact on nurses’ mental health, occupational development, and nurse-patient relationship. First, occupational stigma is positively correlated with nurses’ perceived discrimination and exclusion, which can trigger anxiety, depression, and psychological problems.18 Second, occupational stigma weakens nurses’ occupational wellness and identification,19 and strengthens their burnout and retention unwillingness.20,21 Third, stigma also affects nursing majors’ cognition of nursing, thus causing them to give up the nursing profession in the future.22
At present, qualitative studies on the impact of occupational stigma on the physical and mental health and well-being of nurses have been conducted by most researchers.23,24 Only a few studies have adopted quantitative studies, and the lack of scientific instruments for assessment is one of the obstacles. So far, only part of the contents of several scales have involved occupational stigma toward nurses. For instance, the Job-Esteem Scale for Korean Nurses is comprised of six dimensions of professional self-awareness,25 professional competence, role and expertise of care, social trust and respect, respect and recognition of the organization and professional authority and future value. Only some items assess nurses’ attitude toward and evaluation of the occupation, reflecting part of self-stigma. For instance, “Nurses are respected by other professionals in the institution” and “My profession will be one of the highly regarded professions in the future”. The Nurse Caring Behaviors Inventory (CBI-24) assess patients’ perception of nurses’ caring behavior from assurance, knowledge and skill, respectful and connectedness, reflecting part of public stigma.26 However, the attitude toward stigma and the connotation of stigma are not identical, and the scale does not involve the negative results of social isolation and status loss caused by stigma.
In the process of stigmatization, people put negative labels on the whole nurse group based on several nurses’ misconduct or their accidental misconduct.27 Once nurses are labelled, the patient would have expectations of them, then monitor and analyze their behavior and speech.28 Stigmatized labels can affect patients’ evaluation of nurses and perception of nurse-patient relationship.29 Therefore, patients with high stigma toward nurses have lower perception of nurses’ care for them. The present study used the CBI-24 to measure the criterion validity of the NOSS.
In summary, the research on occupational stigma is still in the early stage, let alone the investigations into occupational stigma toward nurses. Therefore, based on literature analysis and the open-ended interview, the present study, strictly following the principles of psychometrics, developed an instrument applicable for assessing nurses’ occupational stigma, and paved the way for the relevant empirical research.
Participants and Methods
Research Design
The present study followed the basic principles of scale development.30 First, based on literature review and the open-ended interview, the initial items were developed. With subject matter experts (SMEs), some items were modified or deleted to form the initial questionnaire. Second, the survey with the initial questionnaire was administered among patients. After item analysis and exploratory factor analysis (EFA), some items were deleted, and the formal questionnaire was developed. Third, the survey with the formal questionnaire was conducted again among patients to test its validity, reliability, and measurement invariance across gender.
Participants
Participants were selected according to convenience sampling to test the scale’s reliability and validity. Participants (patients) in three hospitals in Jilin Province and Jiangsu Province were investigated in two phases.
The investigation of the first phase was from August to September 2021, and the investigation of the second phase was from October to November 2021. Influenced by COVID-19, Chinese hospitals have adopted strict prevention and control policies, so the questionnaire survey only could be conducted in specific departments. Therefore, two nursing interns were systematically trained by the researchers and jointly completed the survey.
The inclusion criteria for participants: (1) Age≧18. (2) Participants were able to understand and communicate. (3) Participants had no mental illness or consciousness disorder. (4) Participants volunteered for the study and signed the informed consent. Participants’ self-report was used to judge whether they had mental illness. In terms of sociodemographic information, two questions were included: “Have you ever suffered from mental illness in the last 3 months?” and “Have you taken any psychotropic drugs in the last 3 months?”. If the participant replied “yes”, then he would be stopped to complete the questionnaire.
The present study was conducted anonymously. Before the survey, participants were informed of the purpose, procedure, confidentiality, and anonymity of the survey. With participants’ permission, the link for the survey was sent to them. Participants were required to complete the questionnaire independently. After the survey, the researchers checked all the data, and deleted the invalid questionnaires. The criteria for deletion: (1) The response time was too short (less than 120 seconds). (2) Both positive and negative items were responded the same. The present study was approved by the Ethics Committee of Jilin International Studies University (Project Number: JY20210511).
Development and Administration of Scale
Theoretical Framework
Link and Phelan define stigma as labeling, stereotype, separation, status loss and discrimination.31 Their conceptual model for stigma posits that stigma exists when the following interrelated components converge. First, people are labeled differences. Second, labeled people are associated with negative attributes. Third, labeled people encounter social separation. Fourth, labeled people experience status loss and discrimination. Therefore, we proposed that occupational stigma toward nurses should comprise three dimensions: negative label, nurse-patient relationship, and devaluation and discrimination. Among them, negative label refers to labeling differences and associating negative attributes with nurses, which reflects negative stereotypes; Nurse-patient relationship refers to labeled nurses placed in distinct categories, which leads to the separation of “us” and “them”. Devaluation and discrimination refer to labeled nurses experiencing unequal status loss and discrimination.
Source of Initial Items
Based on the open-ended interview, the initial items of the NOSS were developed. First, an open-ended interview was conducted among 251 students from one college. Research questions comprised: “What negative labels can you associate with nurses?” “What negative emotional reactions of patients can nurses’ negative labels induce?” “ What negative behavioral reactions of patients can nurses’ negative labels induce?”
After the survey, five graduate students in psychology sorted out and analyzed the collected data independently. The phrases not in line with the theme, semantically unclear and ambiguous were deleted. Finally, a total of 638 valid phrases were retained. After that, these valid phrases were merged and simplified. Among them, the highly quoted phrases were extracted such as “impatience”, “apathy”, “servant”, “low social status”, “inferior educational background”, “privacy leakage” and so forth. According to these highly quoted phrases, 37 initial items were developed subsumed into three dimensions of stereotype, nurse-patient relationship and devaluation and discrimination.
Delphi Method
One professor in psychology and two associate professors in nursing were invited to evaluate and discuss the items, and the unclear, ambiguous, similar, and repeated items were dropped, merged, or modified. Finally, 21 items were retained, and the initial NOSS was developed.
Instruments
Nurse Occupational Stigma Scale (NOSS)
The initial NOSS consists of 21 items. The formal one is composed of 16 items divided into negative label, nurse-patient relationship and social status. Item examples for negative label are “Nurses are less educated” and “Nurses act as a servant to people”; item examples for nurse-patient relationship are “Nurses are impatient with patients” and “Nurses are not sympathetic to patients”; item examples for devaluation and discrimination are “Nurses have a low social status” and “Nurses have low incomes”. Each item is rated on a Likert scale from 1 (strongly disagree) to 5 (strongly agree). Participants are required to score according to how well the statement describes them. The sum of all item scores is the total scores with higher scores indicating higher occupational stigma toward nurses.
Caring Behaviors Inventory (CBI-24)
The CBI-24 was used to examine the criterion validity of the NOSS.32 It is comprised of 24 items divided into 4 dimensions of assurance, knowledge and skill, respectful and connectedness. Item examples for assurance are “Returning to the patient voluntarily” and “Talking with the patient”. Item examples for knowledge and skill are “Demonstrating professional knowledge and skill” and “Managing equipment skillfully”. Item examples for respectful are “Demonstrating professional knowledge and skill” and “Managing equipment skillfully. Item examples for connectedness are “Giving instructions or teaching the patient” and “Spending time with the patient”. The CBI-24 is a 6-point Likert scale. Patients are required to score from 1 (never) to 6 (always) according to the frequency of specific behaviors of nurses. The sum of all item scores is the total scores with higher scores showing better caring behaviors of nurses. In the present study, the Cronbach’s alpha coefficient of the scale was 0.984.
Statistical Analyses
Drawing on SPSS 25.0, item analysis was performed on the data from Sample 1. The independent samples t-test on the high- and low-scored groups (27%) and the item-total correction were used to analyze the discrimination. If the significance of critical ratio value (C.R.) in the independent sample t-test was lower than 0.05, it indicated that the item had good discrimination. Pearson correlation analysis was used to calculate the correlation between each item and the total score of each dimension, and the items with correlation coefficient lower than 0.4 were deleted. The value of Kaiser–Meyer–Olkin (KMO) higher than 0.7 and the p value of Bartlett’s test of sphericity lower than 0.05 were set to the criteria to check whether the data was suitable for EFA. Factors were extracted using principal component analysis (PCA), and oblique rotation was done using equamax. The criteria for removing poorly performed items: (1) Factor loadings are lower than 0.4.33 (2) The loading difference between two factors was lower than 0.2. (3) Communalities are lower than 0.3.34
The data from Sample 2 was used for CFA, reliability, validity, and cross-gender invariance testing. In terms of CFA, χ2/df lower than 3, RMSEA lower than 0.08, RFI, CFI, NFI and IFI higher than 0.90, PNFI and PCFI higher than 0.50 were set as the criteria for a good fitting model.35 The scale’s criterion validity, internal consistency reliability and split-half reliability were tested using SPSS 25.0. The reliability coefficient higher than 0.70 was set as the indicator of a reliable scale.36 Measurement invariance across gender was tested using AMOS 24.0. The configural (M1), weak (M2), strong (M3) and strict (M4) invariance models were constructed in order. M1 was constructed by setting equal factor dimensions. Under the premise that M1 held, M2 was constructed by setting equal factor loadings. Under the prerequisite that M1 held, M3 was constructed by setting equal intercepts. Under the condition that M3 held, M4 was constructed by setting equal residual variances. ΔCFI lower than 0.01 was set as the criteria for the acceptable invariance.37
Results
Demographic Statistics
765 valid questionnaires were collected from two phases. 362 valid questionnaires were collected from the first phase (Sample 1). Among them, 141 were males, and 219 were females. The average age was 32.80 (SD=11.33, range=18–65). In terms of marriage, 166 were unmarried (45.86%);188 were married (51.93%); 8 were divorced or widowed (2.20%).
403 valid questionnaires were collected from the second phase (Sample 2). Among them, 163 were males (40.44%) and 240 were females (59.55%). The average age was 38.09 (SD=13.41, range=18–65); In terms of marriage, 121 were unmarried (30.02%); 276 were married (68.49%); 6 were divorced or widowed (1.49%).
Pre-Testing
Item Analysis
The results of item analysis indicated that the critical ratio (C.R.) of each item was between 9.35 and 30.63 and p value was lower than 0.001, suggesting that significant differences existed in the scores of all items between high- and low-scored groups (Table 1).The correlation between all items and the total scores of the NOSS was between 0.52 (>0.4), and the p value was lower than 0.01 (Table 1). No item was dropped in this phase.
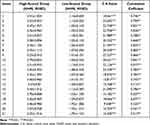 |
Table 1 Correlation Coefficients Between Items and Total Score (N=362) |
Exploratory Factor Analysis
Data were suitable for EFA as the value of KMO was 0.933; the value of Bartlett’s test of sphericity was 4720.806; degree of freedom was 120; and the p value was lower than 0.001. According to the results of factor extraction, three factors yielded eigenvalues higher than 1.0 with total of 71.473% of the variance (Table 2). Item 6, 14, 13, 4 and 10 were dropped for cross-loadings. After CFA was performed, the reliability and the total variance were tested to compare with the initial theoretical conceptualization. A clear factor-structure was obtained by considering both statistical indices and conceptual meanings.
 |
Table 2 Item and Factor Loadings for the NOSS (N=362) |
Factors were extracted again from the retained 16 items, and three factors with eigenvalues higher than 1.0 were extracted. The results are presented in Table 2. Among 16 items, the lowest loading was 0.660; the highest was 0.872; communalities of all items were between 0.607 and 0.878. Every factor was made up of 5 to 6 items, and the total variance of the three factors was 73.037%. According to our theoretical conceptualization and the items contained in the dimensions, factor 1 was named negative label; factor 2 was named nurse-patient relationship; and factor 3 was named devaluation and discrimination.
Construct Validity
Confirmatory Factor Analysis
CFA was performed on the data from Sample 2 to test to test the fit of three-factor structured NOSS. The fit indices of the model were χ2/df=2.635, RMSEA=0.064, RFI=0.926 and CFI=0.962, suggesting the three-factor model fitted well.
Criterion Validity Testing
With the CBI-24 as the criterion, the criterion validity of the NOSS was tested. The results (Table 3) showed that the total scores of the NOSS and its dimensions were significantly negatively correlated with the scores of the CBI-24 (p<0.01).
 |
Table 3 Correlation Analysis of the NOSS with Other Scales (N=403) |
Reliability Testing
The results of reliability testing are presented in Table 4. The Cronbach’s alpha coefficients of the NOSS and its dimensions were between 0.827 and 0.920, and the split-half reliability coefficients were between 0.826 and 0.942.
 |
Table 4 Table of Confidence Coefficients for NOSS (N=403) |
Cross-Gender Invariance Testing
The measurement invariance of the NOSS was tested using the data from Sample 2 (N=403). As the premise of testing other invariance, configural invariance is generally as the baseline model for testing. In other words, any further testing for invariance is through constructing nested models by limiting the corresponding parameters on the basis of configural invariance. The results showed that the configural (M1), weak (M2), strong (M3) and strict (M4) invariance models had good fit indices (Table 5). When comparing M2 to M1, and M3 to M2, ∆CFI were 0.002 and 0.006 respectively, suggesting that M1, M2, M3 and M4 were all established. When comparing M4 to M3, ∆CFI was equal to 0.013, suggesting that M4 was not established. In general, the requirements for testing strict invariance are too strict to be used to for testing measurement invariance across groups.38 Therefore, the NOSS could be considered with cross-gender invariance, as M3 was established.
 |
Table 5 Measurement Invariance Across Gender of the NOSS (N=403) |
Discussion
Occupational stigma exerts a profound impact on the work attitude, performance, and well-being of practitioners, and even the development of relevant industries.39 To data, there have been few studies on stigma toward nurses, since most studies on occupational stigma have centered on dirty work. According to the analysis of the existing literature, the NOSS developed in the present study is the first occupational stigma scale for nurses, which showed novelty and enriched the research on occupational stigma. In order to ensure the NOSS meeting the psychometric requirements, the present study strictly followed the steps of questionnaire development. Firstly, we took the conceptual model of stigma as the theoretical framework to determine the three-factor structured NOSS. Secondly, we formed the initial items of the scale according to the results of open-ended interview survey and the suggestions of experts. Thirdly, we developed the formal scale by means of item analysis, EFA, CFA, criterion validity and reliability analyses. With its good reliability and validity, the NOSS can be a scientific instrument for accurately assessing public stigma toward nurses and the effectiveness of interventions in stigma.
Based on literature review and the open-ended interview, the structure of the NOSS was initially formed. With EFA and CFA, the three-factor structural NOSS was developed, comprising negative label, nurse-patient relationship, and devaluation and discrimination. Composed of 5 items, negative label refers that patients distinguish and label the differences between nursing and other occupations, then associate the differences with negative attributes. Patients place all nurses in the same category for oversimplification, and then connect negative social identity or attributes to nurses. Individuals with higher scores in negative label have more negative stereotypes about nurses. Comprised of 6 items, nurse-patient relationship reflect social separation—patients separate “us” from nurses “them”. Individuals with higher scores in scores tend to exaggerate the differences between nurses and patients, and even set them against each other, thus undermining nurse-patient relationship. Constituted by 5 items, devaluation and discrimination indicate patients’ exclusion and discrimination against nurses. Individuals with higher scores are inclined to hold a pejorative attitude toward nurses. The corollary of negative label and stereotype is status loss.31
Currently, no consensus has been reached on the dimensions and structure of nurse occupational stigma. Developed by Mak and Cheung,40 the Self-Stigma Scale-Short Form (SSS–S) can be used to assess individuals’ perception of stigma toward their occupations, such as “My occupation is a burden to me”, “My occupation taints my life”. This one-factor scale mainly refers to what about self-stigma is perceived. Based on the SSS–S, Ji et al developed the Family Implicated Stigma Scale by changing the subjects in original items from employees themselves to employees’ family for assessing the negative impact of family implicated stigma.32 The NOSS is used to assess patents’ stigma toward nurses, mainly involving public stigma. The three scales are distinct in terms of dimensions and target population.
As regards reliability and validity, the internal consistency coefficients of the total NOSS and its dimensions were between 0.827 and 0.920, and the split-half reliability coefficients were between 0.826 and 0.942, which met the requirements of psychometrics. The results of EFA and CFA indicated that the three-factor model had good model fit. The results of criterion validity analysis showed that the total NOSS and its dimensions were significantly negatively correlated with nurse caring behaviors (p<0.01), suggesting that the NOSS had good criterion validity. In measurement invariance testing, the configural, weak and strong invariances were all acceptable except the strict invariance. The possible impact of unequal residuals should be taken into account when interpreting potential gender differences, although the NOSS can be considered to have cross-gender invariance for meeting the strong invariance model. Although the NOSS could be assumed to be invariant across gender by fulfilling the strong invariance model, any possible effect of residual inequality ought to be taken into account when explaining potential gender differences.
The present study still has several limitations. First, the individual differences of occupational stigma toward nurses were not further discussed according to the departments and types of participants. In future research, targeted scale items can be developed based on the characteristics of patients in different departments to extend the applicability of our scale. Second, in terms of reliability testing, the study did not analyze the test-retest reliability. Considering the adoption of an anonymous survey and the participants from different departments of three hospitals, we did not analyze the test-retest reliability, which may also affect the stability of our scale. Third, the content of NOSS conforms to the Chinese cultural context, but its applicability in cross-cultural contexts needs to be further explored. Fourth, we did not examine the parallel form reliability of the NOSS, in the light of the difficulty of developing a parallel form equivalent to the scale, and the possible reduced enthusiasm for competing two similar questionnaires. A more comprehensive test for the reliability of NOSS needs to be carried out in future research.
Conculsion
Based on the conceptual model for stigma, the 16-item NOSS was developed. The NOSS consists of three dimensions of negative label, nurse-patient relationship, and devaluation and discrimination. The results of CFA demonstrated the reasonability of this three-factor model. The results of reliability and validity analyses indicated that the NOSS exhibited satisfactory psychometric properties. The present study offers a theoretical basis for conducting quantitative studies on nurse occupational stigma. In addition, the present study also provides an effective instrument for evaluating the effectiveness of interventions in stigma.
Ethical Approval
The study protocol was approved by the Ethics Committee of Jilin International Studies University (project number: JY20220104). The investigation process adhered to the principle of confidentiality, with the questionnaires completed anonymously, and the research data were used only in this research.
Acknowledgment
We thank Jilin Provincial Department of Education for funding this study. (Project No. JJKH20211016JY).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Tschannen D, Alexander C, Taylor S, et al. Quality improvement engagement and competence: a comparison between frontline nurses and nurse leaders. Nurs Outlook. 2021;69(5):836–847. doi:10.1016/j.outlook.2021.02.008
2. Liu Y, Zhang Z, Gong Q, et al. Analysis of primary nursing intervention for elderly patients with cancer pain on the improvement of potential risk and pain degree. Am J Transl Res. 2021;13(10):11890–11898.
3. Zhang S, Liu Y, Song S, Peng S, Xiong MJ. The psychological nursing interventions based on Pygmalion effect could alleviate negative emotions of patients with suspected COVID-19 patients: a retrospective analysis. Int J Gen Med. 2022;15:513–522. doi:10.2147/ijgm.S347439
4. Hadley MB, Blum LS, Mujaddid S, et al. Why Bangladeshi nurses avoid ‘nursing’: social and structural factors on hospital wards in Bangladesh. Soc Sci Med. 2007;64(6):1166–1177. doi:10.1016/j.socscimed.2006.06.030
5. Longhurst C. Evidence of discrimination against BME nurses revealed. Nurs Manage. 2017;24(2):8. doi:10.7748/nm.24.2.8.s8
6. Oliveira A. History of nursing - the period of decline of nursing in the centuries that followed the Medieval Age. Escola Anna Nery. 2009;13:463–465.
7. Ashforth BE, Kreiner GE. “How can you do it?”: dirty work and the challenge of constructing a positive identity. Acad Manag Rev. 1999;24(3):413–434. doi:10.2307/259134
8. Glasper AJ. Recognising Florence Nightingale’s contribution to nursing. 2020;29(14):832–833. doi:10.12968/bjon.2020.29.14.832
9. Silva R, Ferreira MJ. Nursing and society: evolution of Nursing and of capitalism in the 200 years of Florence Nightingale. Revista Latino-Americana de Enfermagem. 2021;29:e3425. doi:10.1590/1518-8345.4482.3425
10. Dos Santos LM. Male nursing practitioners and nursing educators: the relationship between childhood experience, social stigma, and social bias. Int J Environ Res Public Health. 2020;17(14):4959. doi:10.3390/ijerph17144959
11. Wesołowska K, Elovainio M, Komulainen K, Hietapakka L, Heponiemi TJ. Nativity status and workplace discrimination in registered nurses: testing the mediating role of psychosocial work characteristics. J Adv Nurs. 2020;76(7):1594–1602. doi:10.1111/jan.14361
12. Guidetti G, Grandi A, Converso D, et al. Funeral and mortuary operators: the role of stigma, incivility, work meaningfulness and work–family relation to explain occupational burnout. Int J Environ Res Public Health. 2021;18(13):6691. doi:10.3390/ijerph18136691
13. Li Y, Song Y, Wang M, Huan T-CT. The influence of tour guides’ service quality on tourists’ tour guide stigma judgment: an asian perspective. J Hosp Tour Manag. 2021;48:551–560. doi:10.1016/j.jhtm.2021.08.011
14. Eyllon M, Vallas SP, Dennerlein JT, et al. Mental health stigma and wellbeing among commercial construction workers: a mixed methods study. J Occup Environ Med. 2020;62(8):e423–e430. doi:10.1097/JOM.0000000000001929
15. Huang B, Ma L, Huang LJ. My work is meaningless: the consequences of perceived occupational stigma for employees in high-prestige occupations. Front Psychol. 2022;13:715188. doi:10.3389/fpsyg.2022.715188
16. Ashforth E, Kreiner G, Clark A, Fugate M. Normalizing dirty work: managerial tactics for countering occupational taint. Acad Manag J. 2007;50(1):149–174. doi:10.5465/amj.2007.2416209
17. Clough BA, Ireland MJ, March S. Development of the SOSS-D: a scale to measure stigma of occupational stress and burnout in medical doctors. J Ment Health. 2019;28(1):26–33. doi:10.1080/09638237.2017.1370642
18. Xie N, Qin Y, Wang T, Zeng Y, Deng X, Guan L. Prevalence of depressive symptoms among nurses in China: a systematic review and meta-analysis. PLoS One. 2020;15(7):e0235448. doi:10.1371/journal.pone.0235448
19. Sturm BA, Dellert JC. Exploring nurses’ personal dignity, global self-esteem and work satisfaction. Nurs Ethics. 2016;23(4):384–400. doi:10.1177/0969733014567024
20. Johnson J, Cameron L, Mitchinson L, et al. An investigation into the relationships between bullying, discrimination, burnout and patient safety in nurses and midwives: is burnout a mediator? J Res Nurs. 2019;24(8):604–619. doi:10.1177/1744987119880329
21. Witton N, Goldsworthy S, Phillips LA. Moral distress does this impact on intent to stay among adult critical care nurses? Nurs Crit Care. 2022. doi:10.1111/nicc.12767
22. Wu C, Palmer MH, Sha K. Professional identity and its influencing factors of first-year post-associate degree baccalaureate nursing students: a cross-sectional study. Nurse Educ Today. 2020;84:104227. doi:10.1016/j.nedt.2019.104227
23. Mitake T, Iwasaki S, Deguchi Y, et al. Relationship between burnout and mental-illness-related stigma among nonprofessional occupational mental health staff. Biomed Res Int. 2019;2019:1–6. doi:10.1155/2019/5921703
24. Ostaszkiewicz J, O’Connell B, Dunning T. ‘We just do the dirty work’: dealing with incontinence, courtesy stigma and the low occupational status of carework in long‐term aged care facilities. J Clin Nurs. 2016;25(17–18):2528–2541. doi:10.1111/jocn.13292
25. Choi HJ, Jung KI. Development of job-esteem scale for Korean nurses. J Korean Acad Nurs. 2020;50(3):444–458. doi:10.4040/jkan.19209
26. Levin S, Van Laar C. Stigma and Group Inequality: Social Psychological Perspectives. Psychology Press; 2006.
27. Xu T, Tang L, Lin X. The effect of perceived discrimination on future dangerousness of probationers in China: an empirical test of crime labeling theory. Int J Law Crime Justice. 2021;65:100470. doi:10.1016/j.ijlcj.2021.100470
28. Jacoby A, Snape D, Baker GA. Epilepsy and social identity: the stigma of a chronic neurological disorder. Lancet Neurol. 2005;4(3):171–178. doi:10.1016/S1474-4422(05)70020-X
29. Ashford RD, Brown AM, McDaniel J, Curtis B. Biased labels: an experimental study of language and stigma among individuals in recovery and health professionals. Subst Use Misuse. 2019;54(8):1376–1384. doi:10.1080/10826084.2019.1581221
30. Flora DB, Flake JK. The purpose and practice of exploratory and confirmatory factor analysis in psychological research: decisions for scale development and validation. Can J Behav Sci. 2017;49(2):78. doi:10.1037/cbs0000069
31. Link BG, Phelan JC. Conceptualizing stigma. Annu Rev Sociol. 2001;27(1):363–385. doi:10.1146/annurev.soc.27.1.363
32. Wu Y, Larrabee JH, Putman HP. Caring behaviors inventory: a reduction of the 42-item instrument. Nurs Res. 2006;55(1):18–25. doi:10.1097/00006199-200601000-00003
33. Stemler SE, Tsai J. Best practices in interrater reliability: three common approaches. Best Pract Quantitative Methods. 2008;2008:29–49.
34. Long W. Questionnaire Statistical Analysis Practice: SPSS Operation and Application. Chongqing: Chongqing University Press; 2010.
35. Bentler PM, Bonett DG. Significance tests and goodness of fit in the analysis of covariance structures. Psychol Bull. 1980;88(3):588. doi:10.1037/0033-2909.88.3.588
36. George D. SPSS for Windows Step by Step: A Simple Study Guide and Reference, 17.0 Update, 10/e. Pearson Education India; 2011.
37. Cheung GW, Rensvold RB. Evaluating goodness-of-fit indexes for testing measurement invariance. Struct Equation Model. 2002;9(2):233–255. doi:10.1207/S15328007SEM0902_5
38. Widaman KF, Reise SP. Exploring the measurement invariance of psychological instruments: applications in the substance use domain. 1997.
39. Ji H, Yan J, Guo W. How and when does occupational stigma promote intent to leave? The mediation effect of family implicated stigma and the moderating effect of family involvement. Acta Psychologica Sinica. 2022;54(2):182. doi:10.3724/SP.J.1041.2022.00182
40. Mak WW, Cheung RY. Self-stigma among concealable minorities in Hong Kong: conceptualization and unified measurement. Am J Orthopsychiatr. 2010;80(2):267. doi:10.1111/j.1939-0025.2010.01030.x
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
