Back to Journals » ClinicoEconomics and Outcomes Research » Volume 15
CELESTIA: Cost-Effectiveness Analysis of Empagliflozin Versus Sitagliptin in Patients with Type 2 Diabetes in Greece
Authors Ghetti G , Pradelli L , Papageorgiou G, Karpouzos G, Arikan Y
Received 6 December 2022
Accepted for publication 3 February 2023
Published 17 February 2023 Volume 2023:15 Pages 97—109
DOI https://doi.org/10.2147/CEOR.S400522
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Dean Smith
Gianni Ghetti,1 Lorenzo Pradelli,1 Giannis Papageorgiou,2 George Karpouzos,2 Yelda Arikan3
1AdRes Health Economics and Outcome Research, Turin, Italy; 2Boehringer Ingelheim Hellas, Athens, Greece; 3Boehringer Ingelheim, Amsterdam, the Netherlands
Correspondence: Gianni Ghetti, AdRes Health Economics and Outcome Research, Via Vittorio Alfieri, 17, Turin, 10121, Italy, Email [email protected]
Purpose: Globally, the prevalence of diabetes is on the rise, with the number of affected individuals predicted to cross 700 million by 2045. In Greece, in 2015, almost 700,000 people received prescribed medication for type 2 diabetes. The CELESTIA study aims to assess the cost-effectiveness of empagliflozin compared to branded sitagliptin in type 2 diabetes patients both with and without established cardiovascular disease in Greece from a third payer perspective.
Methods: The IQVIA Core Diabetes Model was used and analyses were conducted from the Greek healthcare payer perspective. Patients received either empagliflozin or sitagliptin until HbA1c threshold of 8.5% (69 mmol/mol) was exceeded. Subsequently, patients were assumed to intensify to insulin therapy. Baseline cohort characteristics and treatment effects were derived from clinical trial data. Literature data were used for input (utilities, treatment costs and costs of diabetes-related complications costs). A lifetime time horizon (50 years) was applied, and costs and benefits were discounted at an annual rate of 3.5%.
Results: Over a lifetime horizon, for empagliflozin, the estimated ICER was of € 6,587 and € 966 per quality-adjusted life years gained versus sitagliptin, in patients without established cardiovascular disease and in patients with established cardiovascular disease, respectively. Probabilistic sensitivity analysis confirmed the robustness of the analysis.
Conclusion: The analysis demonstrated that for type 2 diabetes patients, empagliflozin is a cost-effective treatment option versus branded sitagliptin in Greece.
Keywords: cost-effectiveness, empagliflozin, Greece, IQVIA core diabetes model, sitagliptin, type 2 diabetes
Introduction
Diabetes and its complications are a significant cause of mortality and disability worldwide. In 2017, an estimated 6.28% (462 million) people worldwide were reported to be suffering from the disease. Diabetes is one of the top 10 leading causes of mortality, with more than 1 million deaths per year that can be attributed to the disease alone.1 Globally, the number of affected individuals is predicted to cross 700 million by 2045.2
In 2015, in Greece, an estimated 6.8% of the population (almost 700,000 people) received prescribed medication for type 2 diabetes.3 The annual economic burden associated with diabetes patients was estimated to be around €7,000 in a 2014 study. In this study, it emerged that the economic burden was significantly higher in patients with poor glycemic control (glycosylated hemoglobin >7%). Furthermore, most of the economic burden was due to diabetes-related complications and comorbidities.4
Many landmark studies have shown that maintaining good glycemic control can reduce the incidence of diabetes-related complications over the long term5–9 and thus improving glycemic control remains one more focus of care in combination with the reduction of cardio-renal risk for patients with type 2 diabetes. Based on this, treatment intensification is recommended when glycated hemoglobin (HbA1c) exceeds the 7.5% (58 mmol/mol).10 In addition to this, also multifactorial care, targeting not only glycemic control but also blood pressure, serum lipids, body weight and hypoglycemia risk, is associated with a reduced risk of complications.11–14 Indeed, the latest consensus report by the European Association for the Study of Diabetes and the American Diabetes Association recommends a more holistic approach to diabetes treatment, with additional focus on the treatment effects on cardiovascular disease, body weight and hypoglycemia risk, rather than a sole focus on glycemic control.15
The aim of the Cost-Effectiveness anaLysis of Empagliflozin versus Sitagliptin in patients with Type 2 dIAbetes (CELESTIA) study was to assess the cost-effectiveness of empagliflozin 10 mg, a sodium-glucose cotransporter-2 (SGLT-2) inhibitor, compared to branded sitagliptin 100 mg, a dipeptidyl peptidase-4 (DPP-4) inhibitor, in Greece. The analysis considered both type 2 diabetes patients without established cardiovascular disease (CVD) and type 2 diabetes patients with established CVD.
Materials and Methods
Modelling Approach
The IQVIA CORE Diabetes Model (CDM) was used to perform the analyses. IQVIA CDM is an online simulation tool that estimates both clinical and economic results for cohorts of patients with diabetes. In particular, it performs real-time simulations, of patient receiving intensive or conventional insulin therapy, oral antidiabetic drugs, screening and treatment strategies for microvascular complications, treatment strategies for end-stage complications and multifactorial interventions. Disease progression is based on a series of inter-dependent Markov sub-models that simulate progression of disease-related complications and other cause mortality. Each sub-model uses time-state- and diabetes type-dependent probabilities derived from published sources, utilizing tracker variables to overcome the memoryless properties of standard Markov models. The model facilitates interconnectivity and interaction between the modelled complications, representing the complex and varied sequelae of the disease. Clinical and economic outcomes are calculated within the model using a non-parametric bootstrapping approach. The reliability of simulated outcomes has been tested, with results validated against those reported by clinical trials and epidemiological studies. The interested reader should refer to previously published articles describing this tool16–18 and to the information that are available online (http://www.core-diabetes.com/).
The outputs of the model include amongst other outcomes: life years (LY), quality-adjusted life-years (QALY), direct healthcare costs and incidence of complications. A lifetime horizon was considered in the analyses (50 years), as recommended in American Diabetes Association guidelines.19 Both costs and benefits were discounted by an annual 3.5% rate, in line with previous cost-effectiveness studies in type 2 diabetes in Greece.20,21
Clinical Data: Patients without Established CVD
The IQVIA CDM version 9.5 was used to estimate the long-term cost-effectiveness of empagliflozin versus branded sitagliptin in adult patients without established CVD whose HbA1c level is inadequately controlled on metformin alone in Greece.
EMPA-REG MET trial data22 were used for baseline cohort characteristics. Baseline values required by the IQVIA CDM that were not reported in the publication were based on cohort data from another study that enrolled a similar patient population and other published data. Table S1 summarizes patients baseline characteristics used in the analysis.
The treatment benefits on physiological parameters and adverse event rates were sourced from a network-meta-analysis (NMA) [data on file] and from the publication of Häring et al22 (Table 1).
 |
Table 1 Treatment Effects and Adverse Event Rates Applied in the Analyses for Patients without Established CVD |
Clinical Data: Patients with Established CVD
The IQVIA CDM version 9.0 was used to estimate the long-term cost-effectiveness of empagliflozin versus branded sitagliptin in adult patients with established CVD in Greece.
The model was calibrated to align the three-year event rates predicted by the IQVIA CDM with the results of the EMPA-REG OUTCOME trial for empagliflozin.23 For sitagliptin efficacy was estimated using the results from an indirect treatment comparison (ITC) of empagliflozin to sitagliptin24 (Table 2). Table S2 summarizes the assumptions considered to match the endpoints in the EMPA-REG OUTCOME trial and those reported by the ITC with the IQVIA CDM endpoints. The calibration process, with all the conducted steps, have been already described in previous published analysis.25–27
 |
Table 2 Comparison of Expected vs Projected 3-Year Cumulative Incidence (%) Outcomes for Empagliflozin and Sitagliptin Post CDM Outcome Calibration |
EMPA-REG OUTCOME trial data23 were used for baseline cohort characteristics. Baseline values required by the IQVIA CDM that were not reported in the publication were taken from clinical study report data and other published articles. Table S3 summarizes patients baseline characteristics used in the analysis.
The treatment benefit on physiological parameters and adverse event rates in the first year were aligned with each trial23,28,29 (Table 3). For second and third years, the treatment effect followed the progression over time available in each trial. From the fourth year onwards, the two treatments were assumed equally effective and, thus, HbA1c progression from the EMPA-REG OUTCOME trial was applied to both.
 |
Table 3 Treatment Effects and Adverse Event Rates Applied in the Analyses for Patients with Established CVD |
Treatment Intensification and Long-Term Disease Progression: Patients without Established CVD
The patient cohort was assumed to receive a first-line treatment of empagliflozin or sitagliptin, plus metformin as background therapy. An HbA1c threshold of 8.5% (69 mmol/mol) was defined which triggered the patients to receive an escalation therapy. Patients were switched to basal insulin therapy, as assumed in other recent analyses.30,31 In particular, an escalation therapy of insulin glargine 42 units per day with metformin as background therapy was considered in the analysis. Both treatment effect and adverse event rates of insulin glargine were derived from published literature data32 (Table 4). The United Kingdom Prospective Diabetes Study (UKPDS) 82 risk equation33 was used to model HbA1c after the first year for the remainder of the analysis. Similarly, also the evolution of blood pressure and serum lipids were predicted by applying the progression factors available in the IQVIA CDM (UKPDS 82 and Framingham). Regarding body mass index (BMI), as long as patients stayed on empagliflozin or sitagliptin, the impact on BMI was maintained.
 |
Table 4 Treatment Effects and Adverse Event Rates Applied in the Analyses for Patients without Established CVD (Second-Line Treatment) |
Treatment Intensification and Long-Term Disease Progression: Patients with Established CVD
The patient cohort was assumed to receive a first-line treatment of empagliflozin or sitagliptin. An HbA1c threshold of 8.5% (69 mmol/mol) was defined which triggered the patients to receive an escalation therapy. Patients were switched to basal-bolus insulin therapy, as assumed in other recent analyses.25–27 In particular, a basal insulin dose of 94 units per day and bolus insulin of 59 units per day were considered, as reported by Riddle et al.34 Based on a Greek cross-sectional disease registry, basal insulin regimens were prescribed for 80% of the patients.35 Both treatment effect and adverse event rates of basal-bolus insulin were taken from published data34 (Table 5). In the analysis, CVO outcomes were extended until treatment escalation. Therefore, before treatment switch, HbA1c progression, mortality, and cardiovascular and renal outcomes followed CVO trials results. After treatment switch, the UKPDS 82 risk equations33 were applied to predict all outcomes.
 |
Table 5 Treatment Effects and Adverse Event Rates Applied in the Analyses for Patients with Established CVD (Second-Line Treatment) |
Patient Management
Input data regarding the clinical management of patients were derived from published literature. These data included the proportion of patients on preventive medications, undergoing routine screening for diabetic complications, and the sensitivity and specificity of the screening tests performed.
Utility Data
Table S4 summarizes the data used in the analysis and the related sources. In the analysis, a minimum approach was applied to estimation of utilities, so that in the case of multiple events, the lower utility was applied. For BMI, in line with published results,36 a disutility of – 0.0061 per unit gain in BMI for over 25 kg/m2 was considered in the analysis.
Costs
The analysis was conducted from a third-party payer perspective (National Organization for Healthcare Services Provision [EOPYY]) and, therefore, only direct healthcare costs were included. The analysis aimed at comparing the lifetime costs and effects of empagliflozin versus branded sitagliptin. All prices used were euros (€).
Treatment costs considered in the analysis included drug cost, and needle and the costs associated with self-monitoring of blood glucose for patients receiving insulin (Table S5). Unit costs were sourced from the most recent price bulletin issued by the Greek Ministry of Health.37 For patients with established CVD, aside the main therapy (either empagliflozin or sitagliptin), also insulin as concomitant therapy was considered. The proportion of patients receiving insulin at baseline was considered in the calculation of first-year cost (48% for empagliflozin and 24% for sitagliptin). To estimate the cost of the following-up years, the proportion of patients receiving insulin at the end of trial was used (51% for empagliflozin and 33% for sitagliptin).
Other captured direct healthcare costs were diabetes-related complications (cardiovascular disease, renal, acute events, eye disease, neuropathy, foot ulcer and amputation), costs and patient management costs. Annual costs were obtained from published literature,20,38 and all costs were inflated to 2021 using the National Statistical Service.39 Table S6 summarized all the input costs used in the analysis.
Results
Base Case Analysis
Over a lifetime horizon, empagliflozin provided additional life years (+0.026 LY and +0.492 LY) and quality-adjusted life years (+0.132 QALY and +0.333 QALY) at an additional cost of €868 and €321 compared to sitagliptin, respectively, in patients without established CVD and in patients with established CVD. The ICER estimated for empagliflozin compared to sitagliptin was €6,587/QALY gained and €966/QALY gained, respectively (Table 6).
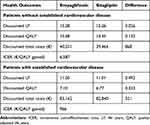 |
Table 6 Long-Term Cost-Effectiveness Outcomes in the Base Case Analyses |
Compared to sitagliptin, the use of empagliflozin implies an increase in the treatment cost of 11.2% and 19.0%, respectively, for patients without established CVD and patients with established CVD (Table 7). This increase is partially offset by a saving of resources in other cost categories. Overall, the increase in total costs with empagliflozin is estimated in 2.2% and 0.4%, respectively, for patients without established CVD and patients with established CVD (Table 7).
 |
Table 7 Breakdown of Costs |
Regarding clinical results, empagliflozin was associated with a lower cumulative incidence of events per 1,000 patient-years for almost every event considered in the analysis in both patients without and with established CVD (Table 8).
 |
Table 8 Cumulative Incidence of Events per 1,000 Patient-Years |
Probabilistic Sensitivity Analysis
Results of the probabilistic sensitivity analysis were presented on an incremental cost-effectiveness plane and as a cost-effectiveness acceptability curve.
For patients without established CVD, most of the simulations (75.4%) lie in the south-east and north-east quadrants (Figure 1A). Empagliflozin was dominant (less costly and more effective) in 23.1% of the simulations, and the probability of being cost-effective compared with sitagliptin for a WTP threshold of €30,000/QALY gained was 72.2% (Figure 1B).
For patients with established CVD, in almost all simulations (98.8%) empagliflozin was more effective (Figure 1C). Empagliflozin was dominant in 40.4% of the simulations, and the probability of being cost-effective compared with sitagliptin for a WTP threshold of €30,000/QALY gained was 98.4% (Figure 1D).
Discussion
The CELESTIA study was conducted from a payer perspective to estimate the long-term cost-effectiveness of empagliflozin 10 mg versus branded sitagliptin 100 mg in both type 2 diabetes patients without established CVD and type 2 diabetes patients with established CVD in Greece.
Sitagliptin was chosen as a comparator in the analysis because it was the first DPP-4 inhibitor that received the marketing authorization and the first launched into the Greek market. Therefore, healthcare professionals clinical experience with this drug could be considered longer in time.
Empagliflozin resulted as a cost-effective treatment option versus sitagliptin for type 2 diabetes, and it was also associated with less diabetes-related complications. This implied cost savings that partially offset the higher treatment costs versus branded sitagliptin. The estimated ICER for empagliflozin versus branded sitagliptin was €6,587 and €966/QALY gained, respectively, in patients without established CVD and in patients with established CVD. The results suggested that empagliflozin was cost-effective as the ICER was well below the median willingness to pay (WTP) threshold of €34,000/QALY gained identified for non-oncology studies in Greece.40 The probabilistic sensitivity analysis confirmed the robustness of base case results.
According to the results of a Greek cross-sectional study,41 the prevalence of heart disease in patients with diabetes mellitus is 24.0%. Thus, we obtained that, on average, treatment with empagliflozin resulted in both additional LYs (+0.138) and additional QALYs (+0.180) compared to sitagliptin. In terms of direct healthcare costs, empagliflozin was associated on average with a direct healthcare cost of €50,610 versus €49,874 for branded sitagliptin. These results led to an ICER of €4,092/QALY gained for empagliflozin compared to branded sitagliptin.
This study reports novel cost-effectiveness results of empagliflozin versus sitagliptin, taking into account both type 2 diabetes patients without established CVD and type 2 diabetes patients with established CVD. Previous cost-effectiveness analyses for empagliflozin versus sitagliptin, using the IQVIA CDM, in type 2 diabetes patients have been reported, although only patients with established CVD were modelled.25,27 Similar trends were observed in both studies, as empagliflozin was found to be cost-effective compared with sitagliptin. In another study, the objective was to estimate the long-term cost-effectiveness of sequential therapy of empagliflozin versus sitagliptin for treatment in patients with type 2 diabetes with or without CVD from the perspective of the US payer.42 Although different treatment pathways were considered, the results of this analysis are consistent with our findings. Indeed, the analysis showed that for US payers, second-line empagliflozin followed by addition of sitagliptin is a highly cost-effective treatment compared with second-line sitagliptin then empagliflozin in patients with or without CVD on metformin monotherapy.
Limitations to this study should be considered. Regarding input data, it was assumed that published utility data were applicable to the Greek patients and healthcare setting. In the absence of local data, this choice was deemed appropriate. Literature data were used to estimate diabetes-related complications costs, and these inputs were validated by expert opinion. Regarding methodology, in our analysis we considered only intensification to insulin therapy and discontinuation of initial therapy when HbA1c threshold of 8.5% (69 mmol/mol) was exceeded. We used UKPDS 82 risk equations to estimate physiological parameters progression. Even if based on old data, these have been extensively used in the literature and their use permit detailed and reliable lifetime simulations of key health outcomes in people with type 2 diabetes. As a lifetime simulation, our analysis relies on extrapolation of short-term outcomes over a lifetime horizon. To minimize the risk connected to this approach, we used the IQVIA CDM, that has been widely published and validated as simulation model for type 2 diabetes analysis.
Another item of discussion can arise looking at the results of the EMPagliflozin compaRative effectIveness and SafEty (EMPRISE) study. The EMPA-REG OUTCOME study showed that empagliflozin has an impact on the number of hospitalizations due to heart failure as well as on cardiovascular and non-cardiovascular mortality in type 2 diabetes patients with established CVD. However, these beneficial effects were not evaluated in patients without clinical evidence of CVD. The EMPRISE study aimed to assess comparative effectiveness, safety, and health care utilization of empagliflozin in type 2 diabetes patients, using real-world data from three databases in the US. An interim analysis from the EMPRISE study, based on data from August 2014 through September 2017, was recently published.43 The aim of this analysis was to evaluate the association between empagliflozin and several cardiovascular and safety outcomes compared to DPP-4 inhibitor. After propensity-score matching, the use of empagliflozin resulted in a 37–52% decreased risk of hospitalization for heart failure (HHF) compared with DPP-4 inhibitor and a similar risk of myocardial infarction or stroke. In our analysis, we did not consider any beneficial effect of empagliflozin on heart failure for patients without established cardiovascular disease, therefore the results for these patients can be considered conservative.
Conclusion
The CELESTIA study highlights that, in Greece, empagliflozin can be considered a cost-effective treatment option for both type 2 diabetes patients without established CVD and type 2 diabetes patients with established CVD in Greece.
Data Sharing Statement
All data generated or analyzed during this study are included in this published article/as Supplementary Information Files.
Ethics Approval
This article is based on the IQVIA CDM, which was used to simulate the long-term clinical and economic results of empagliflozin and sitagliptin based on existing literature findings and completed clinical trials. Moreover, it does not involve any studies on human participants and animals directly performed by any of the authors.
Code Availability
Access to the IQVIA CDM is available upon payment. For more information visit http://www.core-diabetes.com/.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This analysis and manuscript were sponsored and funded by Boehringer Ingelheim that sponsored also the open access fee. Employees were involved in the study design and data analysis, and in the writing of this manuscript.
Disclosure
Ghetti G and Pradelli L are employees of AdRes, which has received project funding by Boehringer Ingelheim. Ghetti G reports grants from Amgen, AstraZeneca, Biogen, Fresenius Kabi, Janssen-Cilag, Novartis Gene Therapies, and Roche, outside the submitted work. Pradelli L reports grants from Amgen S.r.l, AstraZeneca S.p.A., Brahms GmbH, Biogen Italia S.R.L., Gilead Sciences S.R.L., Ipsen S.p.A., Janssen-Cilag S.p.A., Novartis Farma S.p.A., Novartis Gene Therapy EU Limited, Roche S.p.A., Sanofi S.R.L., and UCB Pharma S.p.A.; grants and personal fees from Fresenius Kabi GmbH, outside the submitted work. Papageorgiou G and Karpouzos G are employees of Boehringer Ingelheim Hellas, Athens, Greece. Arikan Y is an employee of Boehringer Ingelheim, Amsterdam, The Netherlands. The authors report no other conflicts of interest in this work.
References
1. Khan MAB, Hashim MJ, King JK, Govender RD, Mustafa H, Al Kaabi J. Epidemiology of type 2 diabetes – global burden of disease and forecasted trends. J Epidemiol Glob Health. 2020;10(1):107–111. doi:10.2991/jegh.k.191028.001
2. Saeedi P, Petersohn I, Salpea P, et al; IDF Diabetes Atlas Committee. Global and regional diabetes prevalence estimates for 2019 and projections for 2030 and 2045: results from the international diabetes federation diabetes atlas, 9th edition. Diabetes Res Clin Pract. 2019;157:107843. doi:10.1016/j.diabres.2019.107843
3. Liatis S, Dafoulas GE, Kani C, et al. The prevalence and treatment patterns of diabetes in the Greek population based on real-world data from the nation-wide prescription database. Diabetes Res Clin Pract. 2016;118:162–167. doi:10.1016/j.diabres.2016.06.018
4. Migdalis I, Rombopoulos G, Hatzikou M, Manes C, Kypraios N, Tentolouris N. The cost of managing type 2 diabetes mellitus in Greece: a retrospective analysis of 10-year patient level data “The HERCULES study”. Int J Endocrinol. 2015;2015:520759. doi:10.1155/2015/520759
5. Patel A, MacMahon S, Chalmers J, et al; ADVANCE Collaborative Group. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008;358(24):2560–2572. doi:10.1056/NEJMoa0802987
6. Holman RR, Paul SK, Bethel MA, Matthews DR, Neil HA. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008;359(15):1577–1589. doi:10.1056/NEJMoa0806470
7. Ismail-Beigi F, Craven T, Banerji MA, et al; ACCORD trial group. Effect of intensive treatment of hyperglycaemia on microvascular outcomes in type 2 diabetes: an analysis of the ACCORD randomised trial. Lancet. 2010;376(9739):419–430. doi:10.1016/S0140-6736(10)60576-4
8. Stettler C, Allemann S, Jüni P, et al. Glycemic control and macrovascular disease in types 1 and 2 diabetes mellitus: meta-analysis of randomized trials. Am Heart J. 2006;152(1):27–38. doi:10.1016/j.ahj.2005.09.015
9. UK Prospective Diabetes Study Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998;352(9131):837–853.
10. National Institute for Health and Care Excellence. NICE guideline [NG28]: type 2 diabetes in adults: management; 2021.
11. Kearney PM, Blackwell L, Collins R, et al; Cholesterol Treatment Trialists’ (CTT) Collaborators. Efficacy of cholesterol-lowering therapy in 18,686 people with diabetes in 14 randomised trials of statins: a meta-analysis. Lancet. 2008;371(9607):117–125. doi:10.1016/S0140-6736(08)60104-X
12. Gaede P, Lund-Andersen H, Parving HH, Pedersen O. Effect of a multifactorial intervention on mortality in type 2 diabetes. N Engl J Med. 2008;358(6):580–591. doi:10.1056/NEJMoa0706245
13. Griffin SJ, Borch-Johnsen K, Davies MJ, et al. Effect of early intensive multifactorial therapy on 5-year cardiovascular outcomes in individuals with type 2 diabetes detected by screening (ADDITION-Europe): a cluster-randomised trial. Lancet. 2011;378(9786):156–167. doi:10.1016/S0140-6736(11)60698-3
14. UK Prospective Diabetes Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ. 1998;317(7160):703–713.
15. Buse JB, Wexler DJ, Tsapas A, et al. 2019 update to: management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD). Diabetes Care. 2020;43(2):487–493. doi:10.2337/dci19-0066
16. Palmer AJ, Roze S, Valentine WJ, et al. The CORE diabetes model: projecting long-term clinical outcomes, costs and cost-effectiveness of interventions in diabetes mellitus (types 1 and 2) to support clinical and reimbursement decision-making. Curr Med Res Opin. 2004;20(Suppl 1):S5–S26. doi:10.1185/030079904X1980
17. Palmer AJ, Roze S, Valentine WJ, et al. Validation of the CORE diabetes model against epidemiological and clinical studies. Curr Med Res Opin. 2004;20(Suppl 1):S27–S40. PMID: 15324514. doi:10.1185/030079904X2006
18. McEwan P, Foos V, Palmer JL, Lamotte M, Lloyd A, Grant D. Validation of the IMS CORE diabetes model. Value Health. 2014;17(6):714–724. doi:10.1016/j.jval.2014.07.007
19. American Diabetes Association Consensus Panel. Guidelines for computer modeling of diabetes and its complications. Diabetes Care. 2004;27(9):2262–2265. doi:10.2337/diacare.27.9.2262
20. Tzanetakos C, Melidonis A, Verras C, Kourlaba G, Maniadakis N. Cost-effectiveness analysis of liraglutide versus sitagliptin or exenatide in patients with inadequately controlled type 2 diabetes on oral antidiabetic drugs in Greece. BMC Health Serv Res. 2014;14:419. doi:10.1186/1472-6963-14-419
21. Gourzoulidis G, Tzanetakos C, Ioannidis I, et al. Cost-effectiveness of empagliflozin for the treatment of patients with type 2 diabetes mellitus at increased cardiovascular risk in Greece. Clin Drug Investig. 2018;38(5):417–426. doi:10.1007/s40261-018-0620-x
22. Häring HU, Merker L, Seewaldt-Becker E, et al; EMPA-REG MET Trial Investigators. Empagliflozin as add-on to metformin in patients with type 2 diabetes: a 24-week, randomized, double-blind, placebo-controlled trial. Diabetes Care. 2014;37(6):1650–1659. doi:10.2337/dc13-2105
23. Zinman B, Inzucchi SE, Lachin JM, et al. Rationale, design, and baseline characteristics of a randomized, placebo-controlled cardiovascular outcome trial of empagliflozin (EMPA-REG OUTCOME™). Cardiovasc Diabetol. 2014;13:102. doi:10.1186/1475-2840-13-102
24. Balijepalli C, Shirali R, Kandaswamy P, et al. Cardiovascular safety of empagliflozin versus dipeptidyl peptidase-4 (DPP-4) inhibitors in type 2 diabetes: systematic literature review and indirect comparisons. Diabetes Ther. 2018;9(4):1491–1500. doi:10.1007/s13300-018-0456-7
25. Ramos M, Foos V, Ustyugova A, Hau N, Gandhi P, Lamotte M. Cost-effectiveness analysis of empagliflozin in comparison to sitagliptin and saxagliptin based on cardiovascular outcome trials in patients with type 2 diabetes and established cardiovascular disease. Diabetes Ther. 2019;10(6):2153–2167. doi:10.1007/s13300-019-00701-3
26. Ramos M, Ustyugova A, Hau N, Lamotte M. Cost-effectiveness of empagliflozin compared with liraglutide based on cardiovascular outcome trials in type II diabetes. J Comp Eff Res. 2020;9(11):781–794. doi:10.2217/cer-2020-0071
27. Ramos M, Men P, Wang X, Ustyugova A, Lamotte M. Cost-effectiveness of empagliflozin in patients with type 2 diabetes and established cardiovascular disease in China. Cost Eff Resour Alloc. 2021;19(1):46. doi:10.1186/s12962-021-00299-z
28. Wanner C, Inzucchi SE, Lachin JM, et al; EMPA-REG OUTCOME Investigators. Empagliflozin and progression of kidney disease in type 2 diabetes. N Engl J Med. 2016;375(4):323–334. doi:10.1056/NEJMoa1515920
29. Green JB, Bethel MA, Armstrong PW, et al; TECOS Study Group. Effect of sitagliptin on cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2015;373(3):232–242. doi:10.1056/NEJMoa1501352
30. Hayes AJ, Leal J, Gray AM, Holman RR, Clarke PM. UKPDS outcomes model 2: a new version of a model to simulate lifetime health outcomes of patients with type 2 diabetes mellitus using data from the 30 year United Kingdom prospective diabetes study: UKPDS 82. Diabetologia. 2013;56(9):1925–1933. doi:10.1007/s00125-013-2940-y
31. Bain SC, Hansen BB, Malkin SJP, et al. Oral semaglutide versus empagliflozin, sitagliptin and liraglutide in the UK: long-term cost-effectiveness analyses based on the PIONEER clinical trial programme. Diabetes Ther. 2020;11(1):259–277. doi:10.1007/s13300-019-00736-6
32. Malkin SJP, Hunt B, Huisman EL, Grand TS, Chubb B. The long-term cost-effectiveness of oral semaglutide in the Netherlands based on the PIONEER 2, 3 and 4 randomized controlled trials. Diabetes Res Clin Pract. 2021;175:108759. doi:10.1016/j.diabres.2021.108759
33. Fonseca V, Gill J, Zhou R, Leahy J. An analysis of early insulin glargine added to metformin with or without sulfonylurea: impact on glycaemic control and hypoglycemia. Diabetes Obes Metab. 2011;13(9):814–822. doi:10.1111/j.1463-1326.2011.01412.x
34. Riddle MC, Bolli GB, Ziemen M, et al; EDITION 1 Study Investigators. New insulin glargine 300 units/mL versus glargine 100 units/mL in people with type 2 diabetes using basal and mealtime insulin: glucose control and hypoglycemia in a 6-month randomized controlled trial (EDITION 1). Diabetes Care. 2014;37(10):2755–2762. doi:10.2337/dc14-0991
35. Liatis S, Iraklianou S, Kazakos K, et al; AGREEMENT Investigators. A Greek registry of current type 2 diabetes management, aiming to determine core clinical approaches, patterns and strategies. BMC Endocr Disord. 2019;19(1):39. doi:10.1186/s12902-019-0364-5
36. Bagust A, Beale S. Modelling EuroQol health-related utility values for diabetic complications from CODE-2 data. Health Econ. 2005;14(3):217–230. PMID: 15386666. doi:10.1002/hec.910
37. Greek Ministry of Health. Drug price bulletin; 2021. Available from: https://www.moh.gov.gr/articles/times-farmakwn/deltia-timwn/9022-laquo-epikairopoihsh-deltioy-timwn-farmakwn-anthrwpinhs-xrhshs-me-enswmatwsh-dioikhtikwn-metabolwn-raquo.
38. Tzanetakos C, Tentolouris N, Kourlaba G, Maniadakis N. Cost-effectiveness of dapagliflozin as add-on to metformin for the treatment of type 2 diabetes mellitus in Greece. Clin Drug Investig. 2016;36(8):649–659. doi:10.1007/s40261-016-0410-2
39. Hellenic Statistical Authority. Inflation rates. Available from: https://www.statistics.gr/en/home/.
40. Tzanetakos C, Stefanou G, Gourzoulidis G. PNS61 does a standard willingness-to-pay threshold exist in Greece? Value Health. 2019;22:S772–S773.
41. Tentolouris A, Eleftheriadou I, Athanasakis K, et al. Prevalence of diabetes mellitus as well as cardiac and other main comorbidities in a representative sample of the adult Greek population in comparison with the general population. Hellenic J Cardiol. 2020;61(1):15–22. doi:10.1016/j.hjc.2018.04.008
42. Reifsnider O, Kansal A, Pimple P, Aponte-Ribero V, Brand S, Shetty S. Cost-effectiveness analysis of empagliflozin versus sitagliptin as second-line therapy for treatment in patients with type 2 diabetes in the United States. Diabetes Obes Metab. 2021;23(3):791–799. doi:10.1111/dom.14268
43. Patorno E, Pawar A, Wexler DJ, et al. Effectiveness and safety of empagliflozin in routine care patients: results from the EMPagliflozin comparative effectIveness and SafEty (EMPRISE) study. Diabetes Obes Metab. 2022;24(3):442–454. doi:10.1111/dom.14593
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.

