Back to Journals » Journal of Inflammation Research » Volume 15
Association of Blood Glucose Variability with Sepsis-Related Disseminated Intravascular Coagulation Morbidity and Mortality
Authors Liu D, Fan Y , Zhuang Y, Peng H, Gao C , Chen Y
Received 27 July 2022
Accepted for publication 15 November 2022
Published 30 November 2022 Volume 2022:15 Pages 6505—6516
DOI https://doi.org/10.2147/JIR.S383053
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Dr Adam D Bachstetter
Dan Liu,1,* YiWen Fan,2,* YuGang Zhuang,1 Hu Peng,1 ChengJin Gao,3 YanQing Chen1
1Emergency Department, Shanghai Tenth People’s Hospital, Affiliated with Tongji University School of Medicine, Shanghai, People’s Republic of China; 2Department of Pathology and Medical Biology, Groningen Research Institute for Asthma and COPD (GRIAC), University of Groningen, University Medical Center Groningen, Groningen, the Netherlands; 3Emergency Department, Xinhua Hospital, affiliated with the Shanghai Jiao Tong University School of Medicine, Shanghai, People’s Republic of China
*These authors contributed equally to this work
Correspondence: ChengJin Gao, Emergency Department, Xinhua Hospital, Affiliated to the Shanghai Jiao Tong University School of Medicine, No. 1665, Kongjiang Road, Yangpu District, Shanghai, People’s Republic of China, Tel +86 25076045, Email [email protected] YanQing Chen, Emergency Department, Shanghai Tenth People’s Hospital, affiliated with Tongji University School of Medicine, No. 301, Yanchang Middle Road, Jingan District, Shanghai, People’s Republic of China, Tel +86 18917683768, Email [email protected]
Purpose: Sepsis-related disseminated intravascular coagulation (DIC) is closely associated with poor prognosis and high mortality. Higher blood glucose (BG) variability indicates an increased risk of mortality in sepsis; however, its relationship with sepsis-related DIC has not been investigated. This study aimed to determine the association between glucose variability and sepsis-related DIC.
Patients and Methods: Patients with sepsis admitted to the intensive care unit were enrolled between October 2017 and January 2021. Baseline data and BG records from the first 72 h were collected. We calculated the glucose liability index (GLI), largest amplitude of glucose excursion, BG standard deviation, and coefficient of variation on days 1 and 3. The relationship between GLI and morbidity of sepsis-related DIC was explored using a competing risk model. In subgroup analysis, we divided patients with and without diabetes into three groups according to the BG range.
Results: Of the 238 patients enrolled, 28.2% developed DIC during hospitalization (n=67). GLI on day 3 was found to have the closest relationship with DIC incidence as it has the largest area under the ROC curve and the highest associated odds ratio of death per unit change (GLI3-day: AUC=0.891 OR=1.84), also independently increased the occurrence of DIC after adjusting for the competing risk of death (sub-distribution hazard ratios=1.866, p< 0.01). In subgroup analysis, patients with diabetes had worse outcomes under hypoglycemia than under hyperglycemia. Patients without diabetes having stable BG had the best outcomes.
Conclusion: Our study suggested that a higher GLI in patients with sepsis at 72 h was independently associated with an increased risk of sepsis-related DIC, which was not associated with pre-existing diabetes.
Keywords: blood disorder, glycemic variability, hypoglycemia, sepsis
Introduction
Sepsis is a life-threatening organ dysfunction caused by a dysregulated host response to infection.1 This encompasses exaggerated inflammatory, immunosuppressive, vascular leaking, and coagulative processes.2 Although the activation of coagulation in patients with sepsis is considered the fundamental host response against infection,3 over-activation can be harmful.4 Severe consumptive coagulopathy, termed disseminated intravascular coagulation (DIC), is associated with organ dysfunction and hemorrhage and directly increases the mortality rate of patients with sepsis.5
Sepsis-related DIC is a fatal complication of sepsis and is closely associated with organ dysfunction and hemorrhage. A large, multicenter, prospective validation study showed that the mortality of patients with sepsis having DIC was 38.4%, which was almost twofold higher than that of those without DIC.6 Moreover, subgroup analyses of large studies showed a higher incidence of DIC and increased mortality rate in patients with severe sepsis when they did not receive timely activated protein C or antithrombin treatments.7,8 Therefore, earlier diagnosis and appropriate treatment are crucial in the management of patients with sepsis.
Stress hyperglycemia with insulin resistance is common in critically ill patients,9,10 and controlling blood glucose (BG) is critical in the intensive care unit (ICU) treatment of patients with sepsis.11–14 However, as several large multicenter studies on intensive insulin therapy failed to demonstrate higher survival rates from strictly controlling BG levels,15–19 especially large amount of evidence suggests that BG variability gets more strong association with worse prognosis than simple BG measurements in the critically ill patient population,20 so the BG variability is gaining more attention nowadays.21–25
The metrics of BG variability (GV), including HbA1c,25 standard deviation (SD),26,27 mean amplitude of glucose excursions (MAGE),27–30 and glycemic lability index (GLI)31,32 are associated with an increased risk of mortality in critically ill patients.26,30,33,34 Moreover, a retrospective cohort study reported that low variability had a protective effect, even in cases of hyperglycemia.34
Furthermore, GV has been thought to be closely associated with endothelial dysfunction in vivo.35 In vitro studies have shown that acute fluctuations in glucose can induce endothelial cell damage. Epitheliopathy plays a critical role in the pathogenesis of sepsis,36 including the aberrant activation of intravascular coagulation, which may lead to sepsis-related DIC.
Although the association between GV and sepsis has been broadly studied, the relationship between GV and sepsis-related DIC has not yet been identified. This study aimed to explore the internal relevance of GV and sepsis-related DIC in the ICU setting.
Materials and Methods
Study Design and Data Collection
We recorded data on comorbidities, prothrombin time, activated partial thromboplastin time (APTT), D-dimer, fibrinogen level, and platelet count and then calculated the points according to the Chinese Society of Thrombosis and Haemostasis Scoring System for DIC (CDSS).37,38 Subsequently, the patients were divided into “survivor” or “non-survivor” groups based on whether they were alive at 28 days after admission.
We collected all recorded BG values and recorded the time points within the first 72 h. We then performed calculations for later analysis (see BG measures).
Patient Enrolment in the ICU Setting
This was a retrospective, exploratory study based on a review of the medical records of adult intensive care patients at two highly complex, public, tertiary hospitals (Xinhua Hospital, affiliated with the Shanghai Jiao Tong University School of Medicine, and the Shanghai Tenth People’s Hospital, affiliated with Tongji University School of Medicine, Shanghai, China). These ICUs have capacities of 13 and 23 critical care beds, respectively. Patients admitted to the ICUs were treated per the glucose regulation protocol, in which insulin is commonly used for glucose control to maintain targets of 80–180 mg/dL (4.4–10 mmol/L).39 In the event of hypoglycemia, 40 mL of 50% glucose solution (GS) was injected, followed by a 10% GS intravenous drip, and the BG was re-tested after 1 h.
Adult patients diagnosed with sepsis and/or septic shock, admitted to the ICU between October, 2017, and January, 2021, were screened for eligibility according to the following criteria: (1) age ≥18 years; (2) sequential organ failure assessment (SOFA) score ≥ 2 points within 24 h of admission; (3) hospital stay ≥3 days; and (4) routine BG monitoring every 2–6 h in the ICU.
Patients with the following criteria were excluded: (1) discharged or died within 3 days of admission; (2) fewer than four records of BG per day within a 72-h period; and (3) concurrent tumors, pregnancy, blood diseases, active bleeding, or anemia.
BG Measures
In both ICUs, routine BG measures applied every 2–6 h depending on patients’ condition. It was assured that patients all got > 4 times measures in recording days.
We screened all patients and collected the values and time points of glucose records within 72 h of admission.
Glucose Liability Index (GLI)
The GLI was one of the most significant indexes for assessing glucose variability in this study. It is calculated as the squared difference between consecutive glucose measurements per unit of actual time (Δh) between those records: GLI = Σ[{Δglucose (mmol/L)}2·Δh −1]·(per se).40–43
Largest Amplitude of Glucose Excursion (LAGE)
This index stands for the glucose excursion for a certain duration, calculated as LAGE = Glumax-Glumin. We calculated LAGEday1 and LAGE3-days separately.
Additionally, we calculated the mean glucose values.
All indexes were calculated separately for day 1 and 3-day (“3-day” means 3 days’ data together), which either gives the earliest information about patients’ disease baseline or offers the clinicians the patients’ blood glucose change pattern under certain treatment in early period in ICU.
Definitions
Diabetes
Diabetes was diagnosed based on the standards of the American Diabetes Association.40–43
Sepsis and Septic Shock
Sepsis is defined as a life-threatening organ dysfunction caused by a dysregulated host response to infection. Organ dysfunction was defined by an increase in the SOFA score by ≥2 points. Septic shock is a type of sepsis characterized by profound circulatory, cellular, and metabolic abnormalities associated with a greater risk of mortality than sepsis alone.
Sepsis Related DIC
We defined sepsis related DIC based on the criteria of CDSS previously described elsewhere (details given in Supplementary Material Table 1).38
In summary, CDSS score was counted by clinicians or trained nurses, including underlying disease, clinical manifestation, and laboratory examination. The score has been counted twice a day separately in morning and night shift in enrolled sepsis patients, and If the score was >7 points, the septic patient would be defined as having sepsis related DIC.
Statistical Analyses
We used mean ± SD or median and interquartile range to describe continuous variables with the variable distribution. Counts and percentages are used to describe categorical variables. In comparison between the two groups, the Student’s t-test or Wilcoxon rank-sum test and χ2 test or Fisher’s exact test were used for continuous and categorical variables, respectively. For comparisons among three or more subgroups, we performed a one-way analysis of variance or Kruskal–Wallis (H-test) depending on variable distribution.
The receiver operating characteristic (ROC) curve was plotted as sensitivity versus 1-specificity values. The area under the curve (AUC) was calculated from the ROC curve. AUC has been used in the research as one of the references to select a better “predictor” with higher association with sepsis related DIC occurrence from multiple GVs.
Sepsis-related DIC occurrence and 90-day mortality were set as the primary and secondary endpoints, respectively. We considered death before DIC diagnosis as a competing risk factor for DIC morbidity. We used the competing risk model (Fine and Gray model) that assessed the factors influencing DIC morbidity independently after adjusting for competing risk. Combined with clinical reality, univariate logistic regression results, together with the results of the Student’s t-test and χ2 test, were used to determine the factors included in the competing risk model. We reported the sub-distribution hazard ratios(sHRs) of the competing risk regression covariates with corresponding 95% confidence intervals.
Furthermore, in subgroup analysis, we explored the differences in sepsis-related DIC occurrence rates within groups that achieved the moderate target glucose range of 70–180 mg/dL (4–10 mmol/L)19 to determine if moderate control will benefit patients with sepsis having DIC. We divided patients with and without diabetes into three groups according to their BG range within 72 h as the low BG group (low blood glucose [LBG], minimum BG ≤ 72 mg/dL [4 mmol/L], n=11), moderate BG group (MBG, minimum BG ³ 72 mg/dL [4 mmol/L], ≤180 mg/dL [10 mmol/L], n=64), and high BG group (HBG, maximum BG³ 180 mg/dL [10 mmol/L], n=163). Moreover, we divided patients within LBG into two subgroups, in which diabetic patients were included in group 1 (LBG1), and non-diabetic patients were enrolled in group 2 (LBG2).
Analyses were performed using IBM SPSS Statistics for Windows, Version 24.0 (IBM Corp., Armonk, NY, USA). Sample size calculation was performed using G*power (version 3.1.9.7 for Windows 10, Franz Faul, University of Kiel, Kiel, Germany). Competing risk analysis was performed in R software (version 3.6.3, R Foundation for Statistical Computing, Vienna, Austria) using the “cmprsk” package38 by following the steps mentioned on the website and the document downloaded from the official website.44 Statistical significance was defined as a two-sided p-value of <0.05.
The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) guideline has been used to construct our methodological design.45
Results
Baseline of Enrolled Patients
Between October 2017, and January 2021, 881 patients were screened for this study. Finally, a total of 238 patients (143 men [60.1%]) were enrolled (Figure 1). The average age was 69.9 years and the average SOFA score at admission was 5.0 with an Acute Physiology and Chronic Health Evaluation II (APACHE II) score of 17.1. Respiratory tract infection was the main cause of sepsis in most patients (n=96, 40.3%), followed by abdominal infection, urinary tract infection, and soft tissue infection. Within the group, 67 patients (28.2%) developed DIC (CDSS) during hospitalization and 80 (33.6%) were identified as having MODS during admission, whereas 88 (37%) died within 90 days after admission. Detailed baseline characteristics are shown in Table 1.
 |
Table 1 Patient Characteristics |
 |
Figure 1 Enrollment strategy of the study. |
GV
As mentioned previously, we calculated several GV variables. Based on previous research,46 we explored the relationship between different expressions of GV and DIC occurrence using the univariate logistic regression model and receiver operating characteristic (ROC) curve (Table 2). We found that the GLI3-day had the largest area under the ROC curve (AUC) and the highest associated odds ratio (OR) of death per unit change (GLI3-day: AUC=0.891 OR=1.84), suggesting that GLI3-day is the most ideal variable for use in subsequent analyses.
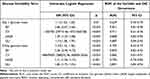 |
Table 2 Determination of Glucose Variability |
Fine and Gray Model Related to DIC Morbidity
We considered death before DIC diagnosis as a competing risk for DIC morbidity.
Univariate logistic regression results are shown in Table 3. We took the results of the logistic regression and cox risk model (not given in the manuscript), together with clinical reality and the comparison between groups previously performed in another study,38 those relevant risk factors in the risk competition model has been decided (Table 3).
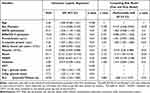 |
Table 3 The Results of Univariate Results and Multivariable Competing Risk Model |
After adjusting for sex (female), SOFA on admission, APACHE II on admission, procalcitonin (PCT), C-reactive protein (CRP), platelet count, shock, multiple-organ dysfunction syndrome (MODS), diabetes, and GLI3-day, we found that male sex (sHR=2.39, p<0.05), CRP (sHR=1.005, p<0.01), shock (sHR=2.140, p<0.05), platelet count (sHR=0.973, p<0.01), and GLI3-day (sHR=1.866, p<0.01) were the factors which strongly and independently influenced DIC occurrence in patients with sepsis.
Different Outcomes of Patients With and Without Diabetes
In subgroup analysis, we found that the MBG group (n=64) had the most stable BG and a significantly lower DIC occurrence rate (3.1%, p<0.01) (Supplemental Material 1). The MBG group had the best outcomes among the three groups, indicating that achieving a moderate BG target (72–180 mg/dL) may be advantageous to patients with sepsis.
Patients with diabetes were more likely to have abnormal BG (Supplemental Material 1), as only 12.5% of patients with diabetes had MBG; however, 54.5% had LBG and 43.6% had HBG (p<0.01). We then divided the patients into groups based on whether they had diabetes or not for further analysis (Table 4).
 |
Table 4 The Outcomes Comparison Among Different Blood Glucose Level Groups in Diabetic Patients and Non-Diabetic Patients |
There were 85 patients with diabetes, 6 with LBG1, 8 with MBG1, and 71 with HBG1. LBG1 had higher scores when discharged, including SOFA and APACHE II (p<0.05), suggesting that the occurrence of hypoglycemia leads to worse outcomes in patients with sepsis having diabetes. Strikingly, all patients in the LBG1 group died within 28 days, 83.3% in the LBG1 group developed DIC (n=5), and DIC occurrence and mortality were significantly higher in the LBG1 group than in the other groups (p<0.05). In contrast, the MBG1 group had the lowest DIC occurrence (n=0, 0%) and mortality rates (n=2, 25%) and achieved the most stable BG during the first 72 h (p<0.05).
Although the HBG group had the highest BG variability, they did not appear to have the highest mortality and DIC occurrence or a higher SOFA score when discharged.
For the group without diabetes, the MBG2 group had a significantly lower incidence of MODS (14.3%) and shock (23.2%) than the HBG2 group (48.9% versus 59.8%). Moreover, the MBG2 group had the fewest patient deaths within the 90-day period and the number of patients who developed DIC during hospitalization. However, both LBG2 and HBG2 groups had high MODS and shock morbidities and higher mortality and DIC occurrence rates than MBG; however, no significant differences were observed between the groups.
Discussion
This study explored the association between GV and sepsis-related DIC in patients in the ICU. We noted that GLI3-day was the most sensitive predictor of sepsis-related DIC and independently influenced DIC morbidity. Further, we found that hypoglycemic episodes in patients with diabetes having sepsis were associated with a higher DIC occurrence rate and 90-day mortality. Patients who maintained moderate BG for 72 h achieved better outcomes, including significantly lower DIC morbidity and 90-day mortality. We observed that patients with the lowest glycemic variability had the lowest DIC occurrence. Our study indicated that the GLI of patients with sepsis potentially predicts sepsis-related DIC, notably BG at the 72nd hour.
Here, 238 patients were enrolled, and 72-h BG records of 3195 were included in our final analysis. In our cohort, after applying the CDSS scoring system to define DIC, DIC incidence and total 90-day mortality rate were 28.2% and 37.0%, respectively, which is similar to previous rates.7,47
Several GVs were calculated based on our data set, including glucose mean, GLI, and LAGE (see BG measures). We demonstrated that GLI3-day was the most sensitive predictor of the incidence of sepsis-related DIC and independently influenced DIC morbidity after adjusting for sex, SOFA on admission, APACHE II on admission, PCT, CRP, platelet count, shock, diabetes, and MODS.
Although DIC is considered a late complication of sepsis, coagulation dysfunction occurs throughout the pathological process of sepsis, as confirmed by various studies.47–49 Therefore, timely monitoring of various indicators of DIC is of great significance for its prompt treatment and management and may help to improve the prognosis and survival of patients.50,51
The GLI is an index based on the change of glucose level over time, more so for prolonged periods.43,52 Frequent testing may result in a slightly higher GLI without immensely skewing the values. Researchers may obtain a relatively high MAGE after testing for several days. Additionally, GLI takes advantage of the inclusion of time and rate of change in its calculation, which may lead to a better association with DIC occurrence than CV, SD, and LAGE. Moreover, GLI was developed to describe the variability in patients with diabetes who underwent over four examinations per day,43 analogous to an actual ICU setting.
Recent decades have demonstrated a difference in the relationship between diabetes and sepsis outcomes. Some studies have shown that diabetes is associated with increased mortality in patients with sepsis,53,54 whereas others have suggested a neutral or even decreased risk.54–57
Here, diabetes was not associated with DIC occurrence and 90-day mortality; however, we found that patients with diabetes were more likely to develop dysglycemia within 72 h.
Further subgroup analysis showed that clinicians should focus on hypoglycemic episodes in patients with diabetes having sepsis since it was associated with a higher DIC occurrence rate and 90-day mortality. Hypoglycemia was reported as a predictor of poor outcomes in patients with sepsis and is closely associated with ICU and hospital mortality.58–61 This may be exaggerated in patients with diabetes having sepsis. However, hyperglycemia was not associated with more complications and worse outcomes in patients with diabetes having sepsis, which may be the result of high mean BG tolerance in the diabetes group.62,63
In contrast, in the group with sepsis not having diabetes, no differences were observed between the outcomes of the HBG2 and LBG2 groups. Notably, patients who maintained moderate BG for 72 h achieved better outcomes, including significantly lower DIC morbidity and 90-day mortality. Regardless of the presence of diabetes, the MBG group had significantly better outcomes. In particular, the MBG group had the lowest GLI, indicating the potential of low GLI as a predictor of favorable outcomes.
High BG variation is associated with an increased risk of mortality in critically ill patients. A novel finding of our study is that variable BG increased the morbidity of sepsis-related DIC even after adjusting for the competing risk of death. This may be due to the endothelial dysfunction because of high glycemic variability. Dysglycemia and high glucose variability are related to compromised endothelial function and injured endothelial cells in patients with type I and II diabetes, as well as in patients with coronary artery disease.64–66 Endothelial cells play a key role in maintaining intravascular patency;67 thus, disrupted endothelial homeostasis in septic conditions may play a fundamental role in the pathogenesis of sepsis-related DIC (36) and contribute to the high glycemic variability. Similarly, we observed that patients with the lowest glycemic variability had the lowest DIC occurrence.
Our study indicated that the GLI of patients with sepsis may have the potential to predict sepsis-related DIC. Therefore, patients with unstable BG during hospitalization should be closely monitored for DIC. However, this study had some limitations. First, as an observational study, we lack a unified BG management protocol with a strict BG target for all patients, so there might rise a problem on detection bias. However, ICUs involved in our research followed certain routine measure for BG so>90% enrolled patients got 4–6 records/day, which gave a less possibility for the bias among patients. An estimated range of BG levels for the patients with sepsis was recommended; however, the target BG was dependent on the patient’s clinical status. The administration of insulin injections was the mainstay of controlling BG levels when BG was >180 mg/dL, similar to the recommendations of the surviving sepsis campaign.68 However, we were not able to follow a detailed management protocol for every patient. Second, we were unable to address the underlying mechanism of this disease. Moreover, limited by the facility and setting, we were not able to apply continuous glucose monitoring for our patients; therefore, some information may have been missed during our research period. These limitations should be considered in future studies.
Conclusion
Our study indicated that a higher 72-h GLI in patients with sepsis was independently associated with an increased risk of sepsis-related DIC that was not associated with pre-existing diabetes. Therefore, healthcare workers who manage patients with sepsis could pay more attention to closely monitor BG levels, especially during the 72nd hour, which might give extra information about the septic patients’ condition changes.
Abbreviations
AF, atrial fibrillation; APACHE, Acute Physiology and Chronic Health Evaluation; APTT, activated partial thromboplastin time; AUC, area under the ROC curve; BG, blood glucose; CDSS, clinical decision support system; COPD, chronic obstructive pulmonary disease; CV, coefficient of variation; DIC, disseminated intravascular coagulation; DVT, deep vein thrombosis; GLI, glucose liability index; GS, glucose solution; GV, glycemic variability; HBG, high blood glucose; HF, heart failure; HR, hazard ratios; ICU, intensive care unit; LAGE, largest amplitude of glucose excursion; LBG, low blood glucose; MAGE, mean amplitude of glucose excursions; MBG, mean blood glucose; MBG, moderate BG Group; MODS, multiple organ dysfunction syndrome; OR, odds ratio; ROC, receiver operating characteristic; SD, standard deviation; sHRs, sub-distribution hazard ratios; SOFA, sequential organ failure assessment.
Data Sharing Statement
Data of the manuscript are not sharing online. Please contact correspondence authors to obtain data if necessary.
Ethics Approval and Consent to Participate
This study was approved by the Shanghai Tenth People’s Hospital, which is affiliated with the Tongji University School of Medicine (SHSY-IEC-5.0/22K84/P01) and the Xinhua Hospital, which is affiliated with the Shanghai Jiao Tong University School of Medicine (No. XHEC-D-2022-032). The requirement for informed consent was waived owing to the retrospective nature of the study design.
Consent for Publication
The study was conducted from October 2017 to January 2021. All patients enrolled in this study have signed the written informed consent, which permits the researchers to engage in research use of identifiable biospecimens and identifiable data during the peri-operative period and future follow-up without the requirement to obtain additional consent for the future storage, maintenance, or research use, so long as the future activities are within the scope of the broad consent. Patients’ data used in the manuscript are maintained with confidentiality. The work described has been carried out in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans.
Acknowledgments
We would like to thank Editage for English language editing.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work. Dan Liu and YiWen Fan contributed the same to the manuscript.
Funding
This work was supported by the National Natural Science Foundation of China (No. 82272184).
Disclosure
The authors report no conflicts of interest in this work.
References
1. Singer M, Deutschman CS, Seymour CW, et al. The third international consensus definitions for sepsis and septic shock (Sepsis-3). JAMA. 2016;315:801–810. doi:10.1001/jama.2016.0287
2. van der Poll T, van de Veerdonk FL, Scicluna BP, Netea MG. The immunopathology of sepsis and potential therapeutic targets. Nat Rev Immunol. 2017;17:407–420. doi:10.1038/nri.2017.36
3. Jackson SP, Darbousset R, Schoenwaelder SM. Thromboinflammation: challenges of therapeutically targeting coagulation and other host defense mechanisms. Blood. 2019;133:906–918. doi:10.1182/blood-2018-11-882993
4. van der Poll T, Herwald H. The coagulation system and its function in early immune defense. Thromb Haemost. 2014;112:640–648. doi:10.1160/TH14-01-0053
5. Giustozzi M, Ehrlinder H, Bongiovanni D, et al. Coagulopathy and sepsis: pathophysiology, clinical manifestations and treatment. Blood Rev. 2021;50:100864. doi:10.1016/j.blre.2021.100864
6. Gando S, Saitoh D, Ogura H, et al. A multicenter, prospective validation study of the Japanese Association for Acute Medicine disseminated intravascular coagulation scoring system in patients with severe sepsis. Crit Care. 2013;17:R111. doi:10.1186/cc12783
7. Dhainaut JF, Yan SB, Joyce DE, et al. Treatment effects of drotrecogin alfa (activated) in patients with severe sepsis with or without overt disseminated intravascular coagulation. J Thromb Haemost. 2004;2:1924–1933. doi:10.1111/j.1538-7836.2004.00955.x
8. Kienast J, Juers M, Wiedermann CJ, et al. Treatment effects of high-dose antithrombin without concomitant heparin in patients with severe sepsis with or without disseminated intravascular coagulation. J Thromb Haemost. 2006;4:90–97. doi:10.1111/j.1538-7836.2005.01697.x
9. Wolfe RR, Allsop JR, Burke JF. Glucose metabolism in man: responses to intravenous glucose infusion. Metabolism. 1979;28:210–220. doi:10.1016/0026-0495(79)90066-0
10. Shangraw RE, Jahoor F, Miyoshi H, et al. Differentiation between septic and postburn insulin resistance. Metabolism. 1989;38:983–989. doi:10.1016/0026-0495(89)
11. Robinson LE, van Soeren MH. Insulin resistance and hyperglycemia in critical illness: role of insulin in glycemic control. AACN Clin Issues. 2004;15:45–62. doi:10.1097/00044067-200401000-00004
12. Coursin DB, Connery LE, Ketzler JT. Perioperative diabetic and hyperglycemic management issues. Crit Care Med. 2004;32:S116–25. doi:10.1097/01.ccm.0000115623.52021.c0
13. Malmberg K, Rydén L, Efendic S, et al. Randomized trial of insulin-glucose infusion followed by subcutaneous insulin treatment in diabetic patients with acute myocardial infarction (DIGAMI study): effects on mortality at 1 year. J Am Coll Cardiol. 1995;26:57–65. doi:10.1016/0735-1097(95)00126-k
14. Malmberg K; DIGAMI (diabetes mellitus, insulin glucose infusion in acute myocardial infarction) Study Group. Prospective randomised study of intensive insulin treatment on long term survival after acute myocardial infarction in patients with diabetes mellitus. BMJ. 1997;314:1512–1515. doi:10.1136/bmj.314.7093.1512
15. Brunkhorst FM, Engel C, Bloos F, et al. Intensive insulin therapy and pentastarch resuscitation in severe sepsis. N Engl J Med. 2008;358:125–139. doi:10.1056/NEJMoa070716
16. Devos P. Impact of tight glucose control by intensive insulin therapy on ICU mortality and the rate of hypoglycaemia: final results of the Glu Control study. Intensive Care Med. 2007;33:S189.
17. Agus MS, Steil GM, Wypij D, et al. Tight glycemic control versus standard care after pediatric cardiac surgery. N Engl J Med. 2012;367:1208–1219. doi:10.1056/NEJMoa1206044
18. Schultz MJ, Spronk PE, van Braam Houckgeest F. Glucontrol, no control, or out of control? Intensive Care Med. 2010;36:173–4;author reply 175. doi:10.1007/s00134-009-1666-2
19. Finfer S, Chittock DR, Su SY, et al.; NICE-SUGAR Study Investigators. Intensive versus conventional glucose control in critically ill patients. N Engl J Med. 2009;360:1283–1297. doi:10.1056/NEJMoa0810625
20. Kauffmann RM, Hayes RM, Buske BD, et al. Increasing blood glucose variability heralds hypoglycemia in the critically ill. J Surg Res. 2011;170(2):257–264. doi:10.1016/j.jss.2011.03.008
21. Hirsch IB, Brownlee M. Should minimal blood glucose variability become the gold standard of glycemic control? J Diabetes Complications. 2005;19:178–181. doi:10.1016/j.jdiacomp.2004.10.001
22. Brownlee M, Hirsch IB. Glycemic variability: a hemoglobin A1c-independent risk factor for diabetic complications. JAMA. 2006;295:1707–1708. doi:10.1001/jama.295.14.1707
23. Hirsch IB. Glycemic variability and diabetes complications: does it matter? Of course it does! Diabetes Care. 2015;38:1610–1614. doi:10.2337/dc14-2898
24. DeVries JH. Glucose variability: where it is important and how to measure it. Diabetes. 2013;62:1405–1408. doi:10.2337/db12-1610
25. Siegelaar SE, Holleman F, Hoekstra JB, DeVries JH. Glucose variability; does it matter? Endocr Rev. 2010;31:171–182. doi:10.1210/er.2009-0021
26. Krinsley JS. Glycemic variability: a strong independent predictor of mortality in critically ill patients. Crit Care Med. 2008;36:3008–3013. doi:10.1097/CCM.0b013e31818b38d2
27. Zhou J, Li H, Ran XY, et al. Establishment of normal reference ranges for glycemic variability in Chinese subjects using continuous glucose monitoring. Med Sci Monit. 2011;17:CR9–C13. doi:10.12659/msm.881318
28. Klimontov VV, Saik OV, Korbut AI. Glucose variability: how does it work? Int J Mol Sci. 2021;22:7783. doi:10.3390/ijms22157783
29. Kovatchev B, Cobelli C. Glucose variability: timing, risk analysis, and relationship to hypoglycemia in diabetes. Diabetes Care. 2016;39:502–510. doi:10.2337/dc15-2035
30. Hermanides J, Vriesendorp TM, Bosman RJ, Zandstra DF, Hoekstra JB, Devries JH. Glucose variability is associated with intensive care unit mortality. Crit Care Med. 2010;38:838–842. doi:10.1097/CCM.0b013e3181cc4be9
31. Preechasuk L, Suwansaksri N, Ipichart N, Vannasaeng S, Permpikul C, Sriwijitkamol A. Hyperglycemia and glycemic variability are associated with the severity of sepsis in nondiabetic subjects. J Crit Care. 2017;38:319–323. doi:10.1016/j.jcrc.2016.12.005
32. Silveira LM, Basile-Filho A, Nicolini EA, Dessotte CAM, Aguiar GCS, Stabile AM. Glycaemic variability in patients with severe sepsis or septic shock admitted to an Intensive Care Unit. Intensive Crit Care Nurs. 2017;41:98–103. doi:10.1016/j.iccn.2017.01.004
33. Pitrowsky M, Shinotsuka CR, Soares M, Salluh JI. Glucose control in critically ill patients in 2009: no alarms and no surprises. Rev Bras Ter Intensiva. 2009;21:310–314.
34. Waeschle RM, Moerer O, Hilgers R, Herrmann P, Neumann P, Quintel M. The impact of the severity of sepsis on the risk of hypoglycaemia and glycaemic variability. Crit Care. 2008;12:R129. doi:10.1186/cc7097
35. Kanamori T, Takeshita Y, Isobe Y, et al. Mealtime dosing of a rapid-acting insulin analog reduces glucose variability and suppresses daytime cardiac sympathetic activity: a randomized controlled study in hospitalized patients with type 2 diabetes. BMJ Open Diabetes Res Care. 2018;6:e000588. doi:10.1136/bmjdrc-2018-000588
36. Higgins SJ, De Ceunynck K, Kellum JA, et al. Tie2 protects the vasculature against thrombus formation in systemic inflammation. J Clin Invest. 2018;128:1471–1484. doi:10.1172/JCI97488
37. Wang M, Kou H, Deng J, et al. Retrospective evaluation of new Chinese diagnostic scoring system for disseminated intravascular coagulation. PLoS One. 2015;10:e0129170. doi:10.1371/journal.pone.0129170
38. Fan YW, Liu D, Chen JM, Li WJ, Gao CJ. Fluctuation in red cell distribution width predicts disseminated intravascular coagulation morbidity and mortality in sepsis: a retrospective single-center study. Minerva Anestesiol. 2021;87:52–64. doi:10.23736/S0375-9393.20.14420-1
39. American Diabetes Association. 15. Diabetes care in the hospital: standards of medical care in Diabetes-2021. Diabetes Care. 2021;44:S211–20. doi:10.2337/dc21-S015
40. Rodbard D. Glucose variability: a review of clinical applications and research developments. Diabetes Technol Ther. 2018;20:S25–S215. doi:10.1089/dia.2018.0092
41. Mesejo A, Montejo-González JC, Vaquerizo-Alonso C, et al. Diabetes-specific enteral nutrition formula in hyperglycemic, mechanically ventilated, critically ill patients: a prospective, open-label, blind-randomized, multicenter study. Crit Care. 2015;19:390. doi:10.1186/s13054-015-1108-1
42. Zuo YY, Kang Y, Yin WH, Wang B, Chen Y. The association of mean glucose level and glucose variability with intensive care unit mortality in patients with severe acute pancreatitis. J Crit Care. 2012;27:146–152. doi:10.1016/j.jcrc.2011.12.004
43. Ryan EA, Shandro T, Green K, et al. Assessment of the severity of hypoglycemia and glycemic lability in type 1 diabetic subjects undergoing islet transplantation. Diabetes. 2004;53:955–962. doi:10.2337/diabetes.53.4.955
44. Berry SD, Ngo L, Samelson EJ, Kiel DP. Competing risk of death: an important consideration in studies of older adults. J Am Geriatr Soc. 2010;58:783–787. doi:10.1111/j.1532-5415.2010.02767.x
45. Vandenbroucke JP, von Elm E, Altman DG, et al. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. PLOS Med. 2007;4:e297. doi:10.1371/journal.pmed.0040297
46. Ali NA, O’Brien JM, Dungan K, et al. Glucose variability and mortality in patients with sepsis. Crit Care Med. 2008;36:2316–2321. doi:10.1097/CCM.0b013e3181810378
47. Bateman RM, Sharpe MD, Jagger JE, et al. 36th International Symposium on intensive care and emergency medicine: Brussels, Belgium. Crit Care. 2016;20;(Suppl 2):94.
48. Gando S, Levi M, Toh CH. Disseminated intravascular coagulation. Nat Rev Dis Primers. 2016;2:16037. doi:10.1038/nrdp.2016.37
49. Levi M, van der Poll T. Inflammation and coagulation. Crit Care Med. 2010;38:S26–S34. doi:10.1097/CCM.0b013e3181c98d21
50. Caliezi C, Wuillemin WA, Zeerleder S, Redondo M, Eisele B, Hack CE. C1-esterase inhibitor: an anti-inflammatory agent and its potential use in the treatment of diseases other than hereditary angioedema. Pharmacol Rev. 2000;52:91–112.
51. Bone RC. Toward a theory regarding the pathogenesis of the systemic inflammatory response syndrome: what we do and do not know about cytokine regulation. Crit Care Med. 1996;24:163–172. doi:10.1097/00003246-199601000-00026
52. Fico G, Hernández L, Cancela J, et al. Exploring the frequency domain of continuous glucose monitoring signals to improve characterization of glucose variability and of diabetic profiles. J Diabetes Sci Technol. 2017;11:773–779. doi:10.1177/1932296816685717
53. Thomsen RW, Hundborg HH, Lervang HH, Johnsen SP, Schønheyder HC, Sørensen HT. Diabetes mellitus as a risk and prognostic factor for community-acquired bacteremia due to enterobacteria: a 10-year, population-based study among adults. Clin Infect Dis. 2005;40:628–631. doi:10.1086/427699
54. Stegenga ME, Vincent JL, Vail GM, et al. Diabetes does not alter mortality or hemostatic and inflammatory responses in patients with severe sepsis. Crit Care Med. 2010;38:539–545. doi:10.1097/CCM.0b013e3181c02726
55. Esper AM, Moss M, Martin GS. The effect of diabetes mellitus on organ dysfunction with sepsis: an epidemiological study. Crit Care. 2009;13:R18. doi:10.1186/cc7717
56. Graham BB, Keniston A, Gajic O, Trillo Alvarez CA, Medvedev S, Douglas IS. Diabetes mellitus does not adversely affect outcomes from a critical illness. Crit Care Med. 2010;38:16–24. doi:10.1097/CCM.0b013e3181b9eaa5
57. Schuetz P, Jones AE, Howell MD, et al. Diabetes is not associated with increased mortality in emergency department patients with sepsis. Ann Emerg Med. 2011;58:438–444. doi:10.1016/j.annemergmed.2011.03.052
58. Bellomo R, Egi M. Hypoglycemia in sepsis: biomarker, mediator, or both? Crit Care Med. 2011;39:2367–2369. doi:10.1097/CCM.0b013e31822a5be5
59. Ssekitoleko R, Jacob ST, Banura P, et al. Hypoglycemia at admission is associated with inhospital mortality in Ugandan patients with severe sepsis. Crit Care Med. 2011;39:2271–2276. doi:10.1097/CCM.0b013e3182227bd2
60. Finfer S, Liu B, Chittock DR, et al.; NICE-SUGAR Study Investigators. Hypoglycemia and risk of death in critically ill patients. N Engl J Med. 2012;367:1108–1118. doi:10.1056/NEJMoa1204942
61. D’Ancona G, Bertuzzi F, Sacchi L, et al. Iatrogenic hypoglycemia secondary to tight glucose control is an independent determinant for mortality and cardiac morbidity. Eur J Cardiothorac Surg. 2011;40:360–366. doi:10.1016/j.ejcts.2010.11.065
62. Umpierrez G, Cardona S, Pasquel F, et al. Randomized controlled trial of intensive versus conservative glucose control in patients undergoing coronary artery bypass graft surgery: GLUCO-CABG trial. Diabetes Care. 2015;38:1665–1672. doi:10.2337/dc15-0303
63. See KC. Glycemic targets in critically ill adults: a mini-review. World J Diabetes. 2021;12:1719–1730. doi:10.4239/wjd.v12.i10.1719
64. Tateishi K, Saito Y, Kitahara H, Kobayashi Y. Impact of glycemic variability on coronary and peripheral endothelial dysfunction in patients with coronary artery disease. J Cardiol. 2022;79:65–70. doi:10.1016/j.jjcc.2021.08.009
65. Farabi SS, Quinn L, Phillips S, et al. Endothelial dysfunction is related to glycemic variability and quality and duration of sleep in adults with Type 1 diabetes. J Cardiovasc Nurs. 2018;33:E21–5–e5. doi:10.1097/JCN.0000000000000485
66. Cosenso-Martin LN, Takaoka LY, Vilela-Martin JF. Randomized study comparing vildagliptin vs glibenclamide on glucose variability and endothelial function in patients with type 2 diabetes mellitus and hypertension. Diabetes Metab Syndr Obes. 2020;13:3221–3229. doi:10.2147/DMSO.S257096
67. Ito T, Kakuuchi M, Maruyama I. Endotheliopathy in septic conditions: mechanistic insight into intravascular coagulation. Crit Care. 2021;25:95. doi:10.1186/s13054-021-03524-6
68. Evans L, Rhodes A, Alhazzani W, et al. Surviving sepsis campaign: international guidelines for management of sepsis and septic shock 2021. Intensive Care Med. 2021;47:1181–1247. doi:10.1007/s00134-021-06506-y
 © 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2022 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
