Back to Journals » Clinical Interventions in Aging » Volume 18
Association Between Plasma Ceramides and One-Year Mortality in Patients with Acute Coronary Syndrome: Insight from the PEACP Study
Authors Li F, Li D , Yu J, Jia Y, Wen J, Li W, Tong Y , Wu J, Wan Z, Cao Y, Zhang Q , Zeng R
Received 22 December 2022
Accepted for publication 30 March 2023
Published 6 April 2023 Volume 2023:18 Pages 571—584
DOI https://doi.org/10.2147/CIA.S402253
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Prof. Dr. Nandu Goswami
Fanghui Li,1,2,* Dongze Li,1,* Jing Yu,1 Yu Jia,3 Jirui Wen,4 Wentao Li,2 Yao Tong,2 Jiang Wu,4 Zhi Wan,1 Yu Cao,1 Qing Zhang,2 Rui Zeng1,2
1Department of Emergency Medicine, Laboratory of Emergency Medicine, West China Hospital, Sichuan University, Chengdu, People’s Republic of China; 2Department of Cardiology, West China Hospital, Sichuan University, Chengdu, People’s Republic of China; 3Department of General Practice and National Clinical Research Center for Geriatrics, International Medical Center, West China Hospital, Sichuan University, Chengdu, People’s Republic of China; 4Deep Underground Space Medical Center, West China Hospital, Sichuan University, Chengdu, People’s Republic of China
*These authors contributed equally to this work
Correspondence: Rui Zeng; Qing Zhang, Department of Cardiology, West China Hospital, Sichuan University, 37 Guoxue Road, Chengdu, Sichuan, 610041, People’s Republic of China, Tel +86-28-85423248, Fax +86-28-85582944, Email [email protected]; [email protected]
Background: The plasma lipidome profile is likely to improve risk stratification in patients with acute coronary syndrome (ACS) and predict cardiovascular events for secondary disease prevention. Ceramides are involved in the initiation or acceleration of several key pathophysiological processes in atherosclerosis. This study evaluated whether plasma ceramide levels at admission was associated with one-year mortality in patients with ACS.
Methods: In total, 826 patients with ACS from a prospective multicenter study for early evaluation of acute chest pain were enrolled. High-performance liquid chromatography with tandem mass spectrometry (LC/MS) was used to measure the plasma levels of eleven ceramides (C16–C26). The primary outcome was all-cause mortality, and the secondary outcome was cardiac mortality during the one-year follow-up. The relationship between the ceramide levels and mortality was evaluated by Cox regression analysis. The receiver operating characteristic (ROC) curve was established to evaluate discrimination of ceramides.
Results: Eighty-eight (10.7%) patients died after a 12-month follow-up. Five ceramides (C16:0, C18:0, C20:0, C24:1 and C24:2) and their ratios to Cer(d18:1/24:0) were independently associated with the risk of all-cause death and cardiac death. Combining the Global Registry of Acute Coronary Events (GRACE) score with ceramides and their ratios to Cer(d18:1/24:0) had areas under ROC curves ranging from 0.778– 0.804 (P< 0.001) for all-cause mortality, which was greater than that of the GRACE score alone.
Conclusion: Measurements of long-chain ceramides and very-long-chain ceramides may help in identifying a high risk of mortality beyond traditional assessment tools in patients with ACS.
Trial Registration: clinicaltrials.gov, identifier: NCT04122573.
Keywords: ceramide, acute coronary syndrome, mortality, high-performance liquid chromatography with tandem mass spectrometry
Introduction
Acute coronary syndrome (ACS) is a life-threatening cardiovascular emergency with relatively high mortality and morbidity, which mainly results from coronary plaque rupture.1 Performing risk stratification for ACS patients facilitates treatment decisions and improves patients’ survival. Current guidelines regarding ACS management emphasize the importance of stratifying patients with high mortality risk.2 For those patients with high risk, intensive treatment should be given. In contrast, unnecessary medical treatment should be avoided in patients with favorable prognoses.3 A recent study reported that the plasma lipidome profile was likely to improve the risk stratification of patients and predict cardiovascular events for secondary disease prevention.4
Ceramides are complex sphingolipids belonging to the waxy lipid family and are one of the most bioactive membrane lipids crucial to sphingolipid synthesis and degradation metabolism.5 As second messengers of intracellular lipids, ceramides play crucial roles in cellular proliferation, differentiation, senescence, and immunity.6 Recent studies have suggested that ceramides are involved in initiating or accelerating several key pathophysiological processes of atherosclerosis, including apoptosis, inflammation, and lipoprotein uptake.7–10
Advanced lipidomic analysis techniques enable the rapid quantification of plasma ceramides, by which study on ceramides and cardiovascular adverse events has been made possible. Previous studies have demonstrated strong predictive values of plasma ceramides for cardiac mortality in patients with stable coronary artery disease.11–14
A recent study showed that an elevated plasma ceramide ratio [Cer(d18:1/16:0)/Cer(d18:1/24:0)] was significantly related to the risk of cardiac death in patients with ACS.13 However, to the best of our knowledge, few studies have been conducted to study the association of multiple ceramides with long-term all-cause mortality in patients with ACS. Besides, we suspect that the increased plasma ceramide concentration may provide additional prognostic information beyond traditional risk factors in patients with ACS. Therefore, we conducted this prospective multicenter study by measuring 11 types of ceramides to investigate the association of ceramides with one-year mortality in patients with ACS.
Materials and Methods
Study Design
This study was conducted using data from a prospective multicenter study for early evaluation of acute chest pain (PEACP) study to investigate if ceramides could predict death in patients with ACS. The PEACP study was a multicenter, prospective cohort study, conducted by seven tertiary hospitals in China and enrolling patients with acute chest pain admitted to the emergency department from November 2020 to April 2021 (clinicaltrials.gov, identifier: NCT04122573). This study was conducted in conformity to the Declaration of Helsinki. In addition, the research protocol was approved by the Human Ethical Committee of West China Hospital of Sichuan University, and all patients signed informed consent forms.
Study Population
In the present study, we investigated the prognostic value of ceramide for patients with ACS. According to our preliminary experiment, the incidence of death was approximately 10.5%. The area under the ROC curves (AUROC) of ceramides for mortality was assumed to be greater than 0.6. To achieve a difference of 80% power at 5% level of significance (for a two-tailed test), a sample size of 675 was required. MedCalc Statistic Software, version 19.0.2 (MedCalc Software, Belgium) was used to calculate sample size.
The inclusion criteria were as follows: age greater than 18 years, first-time diagnosis of ST-segment elevation myocardial infarction (STEMI), non-STEMI (NSTEMI), or unstable angina (UA) according to the diagnostic criteria in the American College of Cardiology/American Heart Association guidelines,15,16 and less than 24 h between the onset of symptoms and ED admission. Patients with missing data, unquantified data of ceramides, confirmed pregnancy status, and presence of a malignant tumor or end-stage hepatopathy were excluded.
Data Collection and Definition
The following patient data were recorded prospectively: vital signs, demographic data, medical history, laboratory examination, echocardiography, coronary angiography, imaging findings, and in-hospital treatment. In the PEACP study, full blood cell counts, blood biochemical parameters and cardiac markers were measured by hematology analysis system (LH750; Beckman Coulter, Brea, CA, USA), Architect c16000 analyzer (Abbott Diagnostics, Dallas, TX, USA), and immunology analyzer (Cobas E601, Roche Diagnostics), respectively.
As recommended in the current guidelines, the Global Registry of Acute Coronary Events (GRACE) score17 and Gensini score18 were used to assess the risk level of ACS patients. The GRACE score was calculated by age, heart rate, systolic blood pressure (SBP), creatinine, cardiac enzymes, ST-segment deviation, Killip class, and cardiac arrest (detailed calculation method is available at http://www.outcomesumassmed.org/grace). The Gensini score, a tool for evaluating the severity of coronary artery disease, was calculated according to importance of stenosis location and severity of coronary artery stenosis after the first coronary artery angiography.
In this study, hypertension was defined as blood pressure (BP) of greater than 140/90 mmHg on at least two occasions, BP of more than 130/80 mmHg in patients with diabetes or chronic kidney disease or those requiring antihypertensive treatment. Diabetes was defined as a history of diabetes or the need for antidiabetic agents. Smoking was classified as at least one cigarette per day for more than 6 months. Alcohol drinking was defined as drinking any type of alcoholic beverage at least once a week for at least 6 months.
Blood Sample Collection and Quantification of Ceramides
Blood samples (5 mL) were collected in EDTA tubes and then were centrifuged at 1500 rpm for 10 min at 4°C to separate plasma, which was stored at −80°C until further testing. Taking 2 µL plasma from each sample to a mixture one for quality control. Plasma (10 µL) was spiked with deuterated internal standards before extraction. Ceramide was extracted as previously described.19 Briefly, 150 µL sample was taken and deproteinated with 450 µL cold isopropanol, and then centrifuged at 12,000 g at 4°C for 5 min after 30s’ vortex. Thereafter, transfer 180 µL of supernatant to a new EP tube. High-performance LC/MS for ceramide testing was reported in detail in a previous study.20 The individual ceramides were quantified using a TSQ Quantiva Triple Quadrupole mass spectrometer, equipped with a Dionex Ultimate 3000 UHPLC system (Thermo Fisher, San Jose, CA, USA) and operated in multiple response monitoring mode. Calibration line samples constructed with known amounts of synthetic ceramides and the corresponding deuterated (D7) standards were used for ceramide quantification.
Calculate the peak area ratios of each ceramide to its corresponding deuterated form, draw the ceramide concentration curve, and then conduct linear regression analysis. Endogenous plasma ceramide concentrations were derived from the individual regression equations obtained by calculating the samples’ corresponding concentrations from the measured peak area ratios. The intra- and inter-precision (coefficient variance) and accuracy (relative error) were within 10%, which were also has been performed in detail.20 The final ceramide concentration in the plasma is presented in µmol/L.
Outcome and Follow-Up
In this study, the primary endpoint was all-cause mortality confirmed by hospital medical records and telephone interviews. The secondary outcome was cardiac death during follow-up, which was identified by hospital record reviews for identified hospitalizations and through phone interviews. The outcome assessment committee of the PEACP Study was responsible for the review and verification of each reported event.
Statistical Analysis
Parametric continuous variables were expressed as mean ± standard deviation (SD) and non-parametric continuous variables as medians with interquartile ranges. Categorical variables were expressed as frequencies and percentages.
One-way analysis was used to compare parametric patient characteristics and the Mann–Whitney U-test was used to compare non-parametric variables. Fisher’s exact test or the chi-square test was used to compare categorical variables. The correlation between all 11 ceramides and the common prognostic factors of ACS was analyzed by Spearman correlation analysis.
The ratios of ceramides to Cer(d18:1/24:0), which are reported to have better prognostic predictive ability for cardiovascular events, were calculated and analyzed.11,13 ROC curves were constructed to evaluate the prognostic value of the GRACE score, seven significant ceramides, and their plasma ratios to Cer(d18:1/24:0) for mortality, and to identify the additional prognostic value of ceramides beyond the GRACE score. Cox regression models were established to evaluate whether ceramides were associated with mortality after adjusting for confounding factors, including age, sex, admission SBP, smoking, drinking, body mass index (BMI), hypertension, diabetes, white blood cell count (WBC), total cholesterol, triglyceride, high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), creatinine kinase-myocardial band isoenzyme (CK-MB), blood urea nitrogen, treatment, GRACE score, and Gensini score. The hazard ratios (HRs) and 95% confidence intervals (CIs) were calculated. A two-tailed p value <0.05 was considered to be statistically significant. SPSS Statistics (version 20.0; SPSS, Chicago, IL, USA) and R for Windows (version 3.5.0; Vienna, Austria) were used for data analysis.
Results
Baseline Patient Characteristics
From November 2020 to April 2021, 3610 patients with an onset time of < 24 hours visited the acute chest pain center. According to the inclusion and exclusion criteria, 847 patients were included in this study initially. After a median follow-up time of 13.9 (10.4–15.7) months, 826 patients with definite outcomes were analyzed. A diagram demonstrating the patient selection process is shown in Figure 1.
 |
Figure 1 Research flow chart. Abbreviations: ED, emergency department; ACS, acute coronary syndrome. |
The average age of enrolled patients was 66.4±12.9 years and 609 patients (73.7%) were men. During follow-up, 88 (10.7%) patients died, 61 (7.4%) of whom died of cardiac causes. Patients who died were older and more likely to have smoked or drank; had a lower BMI, admission SBP, and left ventricular ejection fraction; and had higher heart rate, Killip class, WBC, neutrophil cell count, D-dimer, fibrinogen, blood glucose, N-terminal pro-brain natriuretic peptide (NT-proBNP), high sensitive cardiac troponin T (hs-CTnT), and GRACE scores (P< 0.05), compared with patients who survived (Table 1).
 |
Table 1 Relationships Between Baseline Clinical Characteristics and the Prognosis in Patients with Acute Coronary Syndrome |
Correlation of All Ceramides and Common Risk Factors of Outcomes for Acute Coronary Syndrome
Based on Pearson correlation analysis, all 11 ceramides were positively correlated with each other (P<0.0001, Figure 2A). The average mass fraction of these ceramides was calculated, among which Cer(d18:1/24:1) accounted for the largest (20%) and Cer(d18:1/24:0) accounted for the smallest (5%) mass fractions (Figure 2B). Moreover, there were significant positive correlations between all ceramides with triglycerides, total cholesterol, and low density lipoprotein cholesterol (LDL-C) (P<0.0001); and Cer(d18:1/18:0), Cer(d18:1/20:0), and Cer(d18:1/24:1) had a significant positive correlation with WBC count, cardiac markers (NT-proBNP, hs-CTnT, and CK-MB), and GRACE score (P<0.05; Figure 3).
Relationship Between All Ceramides and Clinical Outcome of Acute Coronary Syndrome
Table 2 shows the median and interquartile ranges of all ceramides in the patients who survived or died after a 12-month follow-up. The results showed that patients who died had significantly higher levels of Cer(d18:1/24:2), Cer (d18:1/24:1), Cer(d18:1/20:0), Cer(d18:1/18:0), Cer(d18:1/21:0), and Cer(d18:1/16:0), and significantly lower levels of Cer(d18:1/24:0) (P<0.05).
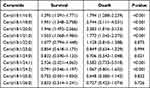 |
Table 2 The Level of Ceramides in Patients with Different Prognosis |
Predictive Value of Ceramides for Mortality
According to ROC curve analysis, seven ceramides and their plasma ratios to Cer(d18:1/24:0) independently related to mortality (Table 3). The GRACE score had an AUROC of 0.778 (95% CI: 0.721–0.834, P<0.001), and the seven ceramides and their plasma ratios to Cer(d18:1/24:0) had AUROCs ranging from 0.579 to 0.734 (P<0.05) for all-cause death. Among these ceramides and their plasma ratios to Cer(d18:1/24:0), the AUROCs for all-cause mortality of Cer(d18:1/18:0)/Cer(d18:1/24:0), Cer(d18:1/18:0), Cer(d18:1/24:2)/Cer(d18:1/24:0), and Cer(d18:1/16:0)/Cer(d18:1/24:0) were 0.734, 0.715, 0.715, and 0.712, respectively and were not significantly different from that of the GRACE score.
 |
Table 3 Predictive Value of Ceramides and GRACE Risk Score for All-Cause Death and Cardiac Death |
To further evaluate the incremental predicted value of ceramides for mortality beyond the GRACE score, each ceramide and its plasma ratio to Cer(d18:1/24:0) were combined with the GRACE score separately. All combinations had significant predictive value for all-cause death, with AUROC ranging from 0.778–0.804 (P<0.001). Moreover, all the combinations showed significantly greater AUROCs (ranging from 0.788–0.804) than that of GRACE score alone (P<0.05), except for Cer(d18:1/24:0) plus GRACE and Cer(d18:1/24:1)/Cer(d18:1/24:0) plus GRACE. Cer(d18:1/18:0) plus GRACE and Cer(d18:1/18:0)/Cer(d18:1/24:0) plus GRACE had the highest AUROC of 0.804 (95% CI: 0.752–0.855, P<0.001; 95% CI: 0.753–0.856, P<0.001). The same analyses were conducted for cardiac mortality and the detailed results are presented in Table 3.
The multivariate Cox regression analysis showed that after adjusting for all the confounders, Cer(d18:1/18:0), Cer(d18:1/24:1), Cer(d18:1/24:2), Cer(d18:1/16:0), Cer(d18:1/20:0), their plasma ratios to Cer(d18:1/24:0), and Cer(d18:1/24:2)/Cer(d18:1/24:0) were independently correlated to risk of all-cause death (Figure 4), while Cer(d18:1/24:1), Cer(d18:1/20:0), Cer(d18:1/18:0), Cer(d18:1/21:0), Cer(d18:1/24:2), Cer(d18:1/16:0) and their plasma ratios to Cer(d18:1/24:0) were independently predictors of cardiac death (P<0.05; Supplementary Figure S1).
Discussion
The present multicenter study prospectively detected 11 kinds of ceramides by targeted LC/MS, the carbochain, which ranged from 16 to 26, and investigated their relationship with one-year mortality in patients with ACS. The results of our study showed that patients with mortality had higher levels of long-chain ceramides (C16:0, C18:0, C20:0, and C21:0) and very long-chain ceramides (C24:1, and C24:2). Furthermore, these seven ceramides showed significant incremental predicted values of mortality beyond the GRACE score. In addition, Cox regression analysis showed that five ceramide subtypes (C16:0, C18:0, C20:0, C24:1 and C24:2), and their plasma ratios to Cer(d18:1/24:0) were independent predictors of one-year mortality. These five ceramide subtypes were main ceramide subtypes in plasma of ACS accounting for a large mass fraction of 62% and they had strong positive correlation with each other.
Previous studies measured the plasma levels of five kinds of ceramides in patients with ACS; it was concluded that Cer(d18:1/24:1), Cer(d18:1/20:0), Cer(d18:1/16:0) and their ratios to Cer(d18:1/24:0) were independent predictors of major adverse cardiac events in ACS patients.11,13 In this multicenter study, we prospectively detected 11 types of ceramides and reported the widest spectrum of ceramide measurements in ACS research. All of the eleven ceramide subtypes were positively correlated with each other, even though their association with mortality risk was not consistent, implying that the biosynthesis and metabolism of those ceramides may be similar; Moreover, even if a certain ceramide subtype [Cer(d18:1/24:0)] seems to be cardioprotective, the overall high level of ceramide is detrimental to cardiovascular health. In addition to results consistent with previous studies, we further demonstrated that Cer(d18:1/24:2), Cer(d18:1/18:0), and their ratios to Cer(d18:1/24:0) were also independent predictors for both cardiac death and all-cause death. Besides, we found that the combination of ceramides to the GRACE score reported increased predictive value for all-cause and cardiac mortality in patients with ACS. In addition, correlation analysis showed that Cer(d18:1/24:1), Cer(d18:1/20:0), and Cer(d18:1/18:0) were significantly positively related to inflammatory indicators, cardiac markers, and GRACE scores, which are traditional cardiovascular risk factors.
Ceramides and their metabolites are the intermediate link in cardiac metabolic diseases caused by insulin resistance and inflammation.21–23 Several studies have reported that ceramides are involved in initiating or accelerating several key pathophysiological processes of atherosclerosis, including apoptosis, inflammation, and lipoprotein uptake.24–26 Reportedly, myocardial cells may secrete ceramide when living with ischemia and reperfusion, activating mitochondrial autophagy and apoptosis.27,28 In addition, recent studies have reported that ceramides accumulate in coronary atherosclerotic plaques and may mediate inflammatory factors that affect the stability of atherosclerotic plaques, thus promoting the apoptosis of vascular endothelial cells, leading to acute attacks of coronary heart disease.24,29 In our results, five ceramide subtypes (C16:0, C18:0, C20:0, C24:1 and C24:2), which were independent predictors of mortality in patients with ACS, all have high relevant to inflammatory indicators. These findings shed light on the mechanism by which ceramides could stratify the risk in patients with ACS and further predict their prognosis.
Different types of disease appear to be associated with different subtypes of ceramide. Previous studies reported that Cer(d18:1/20:0) had a significant predictive value for the occurrence of type 2 diabetes in the healthy population.30,31 And interventions in Cer(d18:1/14:0) and Cer(d18:1/16:0) may improve the outcomes of patients with type 2 diabetes.32,33 It is revealed that very long chain ceramides (C24, C26, and C26:1) are associated with the development of kidney injury.34,35 In our study, among those five significant ceramides, Cer(d18:1/18:0) achieved the best performance for mortality prediction, and it was also the second most abundant ceramide (14%) in ACS plasma, suggesting that Cer(d18:1/18:0) may be a key bioactive substances for pathophysiology of ACS. And it is reported that Cer(d18:1/18:0) is positively correlated with body mass index and negatively correlated with insulin sensitivity in previous study, which may be a potential regulation mechanism of Cer(d18:1/18:0) on ACS.36
The GRACE score is an established, traditional risk stratification tool for patients with ACS.37 From these results, ceramides provide a significant additional predictive value for the GRACE score, which may be due to the involvement of other mechanisms of ACS. The combinations of ceramides and GRACE scores had favorable AUROCs of approximately 0.80. The most favorable aspect of ceramides as predictors of prognosis is their potential to provide guidance of effective interventions. Although there are no relevant randomized controlled trials of ceramide and patients with ACS yet, some previous studies have demonstrated that plasma ceramide concentrations can be significantly decreased by aerobic exercise and statin therapy.7,38 Moreover, physical exercise and lipid-lowering treatment can also decrease the occurrence of cardiovascular death, which suggests that suitable interventions, including efficient lifestyle counseling, increased doses of station, ezetimibe combinations, and some novel therapies, such as PCSK9 inhibitors, may be a promising way to improve the prognosis of patients with ACS.3,39–42
Ceramide measurements by high-throughput LC/MS are straightforward and cost-efficient. Isotope labeling standards allows accurate quantification and analytical stability. And automatic sample-processing systems and mass spectrometry equipment are equipped in most clinical laboratories of modern medical institutions. Hence, these advanced conditions enable rapid and accurate detection of plasma ceramide in clinical practice. However, as there are various types of ceramides with different biological activities in diseases, which may be involved in different regulation pathways, it is necessary to explore the interactions between these ceramides in molecular biology to gain a deeper understanding of ceramide subtypes.
Limitations
There are several limitations in this study. First, although it was a multicenter and prospective study, it had a relatively small sample size; thus, studies with larger populations are warranted to further verify the results of this study. Second, this study detected ceramide only once at admission and did not conduct dynamic monitoring. Third, metabolites of the ceramide synthetic pathway, such as sphingosine, and carriers of ceramide, such as lipoproteins, were not detected in this study. Fourth, major adverse cardiovascular events were not evaluated as an endpoint in this study due to data missing.
Conclusion
In conclusion, plasma concentrations of Cer(d18:1/18:0), Cer(d18:1/24:1), Cer(d18:1/24:2), Cer(d18:1/20:0), Cer(d18:1/16:0), and their ratios to Cer(d18:1/24:0) were independent predictors of one-year mortality in patients with ACS. These ceramides have an additional predictive value for mortality beyond traditional risk assessment tools. Ceramides may help to guide effective clinical prediction, prevention, and intervention. The function of the ceramide subtypes in patients with ACS should be further investigated.
Abbreviations
ACS, acute coronary syndrome; AUROC, area under the receiver operating characteristic curves; BMI, body mass index; CI, confidence interval; CK-MB, creatinine kinase-myocardial band isoenzyme; CRP, C-reactive protein; GRACE, Global Registry of Acute Coronary Events; HR, hazard ratio; HDL-C, high-density lipoprotein cholesterol; hs-cTnT, high sensitive cardiac troponin T; LC/MS, liquid chromatography with tandem mass spectrometry; LDL-C, low-density lipoprotein cholesterol; LVEF, left ventricular ejection fraction; NT-proBNP, N-terminal pro-brain natriuretic peptide; PEACP, prospective multicenter study for early evaluation of acute chest pain; PCI, percutaneous coronary intervention; ROC, receiver operating characteristic; SBP, systolic blood pressure; SD, standard deviation; WBC, white blood cell count.
Data Sharing Statement
The datasets used and analysed during the current study are available from the corresponding author on reasonable request.
Ethics Approval and Informed Consent
This study was conducted in conformity to the Declaration of Helsinki and was approved by the Human Ethical Committee of West China Hospital of Sichuan University.
Acknowledgments
We would like to thank Editage (www.editage.cn) for English language editing.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This work was supported financially by grants from National Key Research and Development Program of China (No. 2020AAA0105000, 2020AAA0105005), Sichuan Science and Technology Program (No. 2022YFS0279, 2021YFQ0062, 2022JDRC0148), Sichuan Provincial Health Commission (Chuanganyan ZH2022-101), Sichuan University West China Nursing Discipline Development Special Fund Project (HXHL20017, HXHL20046, HXHL21016).
Disclosure
The authors have no competing interests to disclose.
References
1. Wong GC, Welsford M, Ainsworth C, et al. Canadian Cardiovascular Society/Canadian Association of interventional cardiology guidelines on the acute management of ST-elevation myocardial infarction: focused update on regionalization and reperfusion. Can J Cardiol. 2019;35(2):107–132.
2. Ibanez B, James S, Agewall S, et al. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39(2):119–177.
3. Li F, Li D, Yu J, et al. Barthel Index as a predictor of mortality in patients with acute coronary syndrome: better activities of daily living, better prognosis. Clin Interv Aging. 2021;15:1951–1961.
4. Mundra PA, Barlow CK, Nestel PJ, et al. Large-scale plasma lipidomic profiling identifies lipids that predict cardiovascular events in secondary prevention. JCI Insight. 2018;3:17.
5. Gault CR, Obeid LM, Hannun YA. An overview of sphingolipid metabolism: from synthesis to breakdown. Adv Exp Med Biol. 2010;688:1–23.
6. Pan W, Yu J, Shi R, et al. Elevation of ceramide and activation of secretory acid sphingomyelinase in patients with acute coronary syndromes. Coron Artery Dis. 2014;25(3):230–235.
7. Tarasov K, Ekroos K, Suoniemi M, et al. Molecular lipids identify cardiovascular risk and are efficiently lowered by simvastatin and PCSK9 deficiency. J Clin Endocrinol Metab. 2014;99(1):E45–52.
8. Li PL, Zhang Y. Cross talk between ceramide and redox signaling: implications for endothelial dysfunction and renal disease. Handb Exp Pharmacol. 2013;216:171–197.
9. Basnakian AG, Ueda N, Hong X, Galitovsky VE, Yin X, Shah SV. Ceramide synthase is essential for endonuclease-mediated death of renal tubular epithelial cells induced by hypoxia-reoxygenation. Am J Physiol Renal Physiol. 2015;288(2):F308–314.
10. Ueda N. Ceramide-induced apoptosis in renal tubular cells: a role of mitochondria and sphingosine-1-phoshate. Int J Mol Sci. 2015;16(3):5076–5124.
11. Anroedh S, Hilvo M, Akkerhuis KM, et al. Plasma concentrations of molecular lipid species predict long-term clinical outcome in coronary artery disease patients. J Lipid Res. 2018;59(9):1729–1737.
12. Cheng JM, Suoniemi M, Kardys I, et al. Plasma concentrations of molecular lipid species in relation to coronary plaque characteristics and cardiovascular outcome: results of the ATHEROREMO-IVUS study. Atherosclerosis. 2015;243(2):560–566.
13. Laaksonen R, Ekroos K, Sysi-Aho M, et al. Plasma ceramides predict cardiovascular death in patients with stable coronary artery disease and acute coronary syndromes beyond LDL-cholesterol. Eur Heart J. 2016;37(25):1967–1976.
14. Tu C, Xie L, Wang Z, et al. Association between ceramides and coronary artery stenosis in patients with coronary artery disease. Lipids Health Dis. 2020;19(1):151.
15. Amsterdam EA, Wenger NK, Brindis RG, et al. 2014 AHA/ACC Guideline for the management of patients with non-ST-elevation acute coronary syndromes: a report of the American College of Cardiology/American Heart Association task force on practice guidelines. J Am Coll Cardiol. 2014;64(24):e139–e228.
16. O’Gara PT, Kushner FG, Ascheim DD, et al. 2013 ACCF/AHA guideline for the management of ST-elevation myocardial infarction: a report of the American College of Cardiology Foundation/American Heart Association task force on practice guidelines. J Am Coll Cardiol. 2013;61(4):e78–e140.
17. Granger CB, Goldberg RJ, Dabbous O, et al. Predictors of hospital mortality in the global registry of acute coronary events. Arch Intern Med. 2013;163(19):2345–2353.
18. Gensini GG. A more meaningful scoring system for determining the severity of coronary heart disease. Am J Cardiol. 1983;51(3):606.
19. Sarafian MH, Gaudin M, Lewis MR, et al. Objective set of criteria for optimization of sample preparation procedures for ultra-high throughput untargeted blood plasma lipid profiling by ultra performance liquid chromatography-mass spectrometry. Anal Chem. 2014;86(12):5766–5774.
20. Huang Q, Hao S, Yao X, et al. High-throughput quantitation of serological ceramides/dihydroceramides by LC/MS/MS: pregnancy baseline biomarkers and potential metabolic messengers. J Pharm Biomed Anal. 2021;192:113639.
21. Summers SA. Ceramides in insulin resistance and lipotoxicity. Prog Lipid Res. 2006;45(1):42–72.
22. Holland WL, Summers SA. Sphingolipids, insulin resistance, and metabolic disease: new insights from in vivo manipulation of sphingolipid metabolism. Endocr Rev. 2008;29(4):381–402.
23. Summers SA. The ART of lowering ceramides. Cell Metab. 2015;22(2):195–196.
24. Li H, Junk P, Huwiler A, et al. Dual effect of ceramide on human endothelial cells: induction of oxidative stress and transcriptional upregulation of endothelial nitric oxide synthase. Circulation. 2002;106(17):2250–2256.
25. Lawrence GD. Perspective: the saturated fat-unsaturated oil dilemma: relations of dietary fatty acids and serum cholesterol, atherosclerosis, inflammation, cancer, and all-cause mortality. Adv Nutr. 2021;12(3):647–656.
26. Mandal N, Grambergs R, Mondal K, Basu SK, Tahia F, Dagogo-Jack S. Role of ceramides in the pathogenesis of diabetes mellitus and its complications. J Diabetes Complications. 2021;35(2):107734.
27. Novgorodov SA, Gudz TI. Ceramide and mitochondria in ischemia/reperfusion. J Cardiovasc Pharmacol. 2009;53(3):198–208.
28. Bielawska AE, Shapiro JP, Jiang L, et al. Ceramide is involved in triggering of cardiomyocyte apoptosis induced by ischemia and reperfusion. Am J Pathol. 1997;151(5):1257–1263.
29. Uchida Y, Uchida Y, Kobayashi T, et al. Detection of ceramide, a risk factor for coronary artery disease, in human coronary plaques by fluorescent angioscopy. Circ J. 2017;81(12):1886–1893.
30. Fretts AM, Jensen PN, Hoofnagle A, et al. Plasma ceramide species are associated with diabetes risk in participants of the strong heart study. J Nutr. 2020;150(5):1214–1222.
31. Yang J, Wang M, Yang D, et al. Integrated lipids biomarker of the prediabetes and type 2 diabetes mellitus Chinese patients. Front Endocrinol. 2023;13:1065665.
32. Raichur S, Brunner B, Bielohuby M, et al. The role of C16:0 ceramide in the development of obesity and type 2 diabetes: cerS6 inhibition as a novel therapeutic approach. Mol Metab. 2019;21:36–50.
33. Kasumov T, Solomon TP, Hwang C, et al. Improved insulin sensitivity after exercise training is linked to reduced plasma C14:0 ceramide in obesity and type 2 diabetes. Obesity. 2015;23(7):1414–1421.
34. Klein RL, Hammad SM, Baker NL, et al.; DCCT/EDIC Research Group. Decreased plasma levels of select very long chain ceramide species are associated with the development of nephropathy in type 1 diabetes. Metabolism. 2014;63(10):1287–1295.
35. Nicholson RJ, Holland WL, Summers SA. Ceramides and acute kidney injury. Semin Nephrol. 2022;42(3):151281.
36. Ritter O, Jelenik T, Roden M. Lipid-mediated muscle insulin resistance: different fat, different pathways? J Mol Med. 2015;93(8):831–843.
37. Li F, Li D, Yu J, et al. Silent myocardial infarction and long-term risk of frailty: the atherosclerosis risk in communities study. Clin Interv Aging. 2021;16:1139–1149.
38. Bergman BC, Brozinick JT, Strauss A, et al. Serum sphingolipids: relationships to insulin sensitivity and changes with exercise in humans. Am J Physiol Endocrinol Metab. 2015;309(4):E398–408.
39. Dong Y, Hao G, Wang Z, Wang X, Chen Z, Zhang L. Ideal cardiovascular health status and risk of cardiovascular disease or all-cause mortality in Chinese middle-aged population. Angiology. 2019;70(6):523–529.
40. Kones R, Rumana U. Prevention of cardiovascular disease: updating the immensity of the challenge and the role of risk factors. Hosp Pract. 2014;42(1):92–100.
41. Kokkinos PF, Faselis C, Myers J, et al. Interactive effects of fitness and statin treatment on mortality risk in veterans with dyslipidaemia: a cohort study. Lancet. 2013;381(9864):394–399.
42. Okoro EU. TNFα-induced LDL cholesterol accumulation involve elevated LDLR cell surface levels and SR-B1 downregulation in human arterial endothelial cells. Int J Mol Sci. 2021;22:12.
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.



