Back to Journals » ClinicoEconomics and Outcomes Research » Volume 15
Weight and BMI Changes Following Initiation of Emtricitabine/Tenofovir Alafenamide Co-Formulated with Darunavir or Co-Administered with Dolutegravir in Overweight or Obese, ART-Naïve People Living with HIV-1
Authors Donga P, Emond B , Rossi C, Bookhart BK, Lee J, Caron-Lapointe G, Wei F, Lafeuille MH
Received 6 April 2023
Accepted for publication 7 July 2023
Published 24 July 2023 Volume 2023:15 Pages 579—591
DOI https://doi.org/10.2147/CEOR.S413800
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Giorgio Colombo
Prina Donga,1 Bruno Emond,2 Carmine Rossi,2 Brahim K Bookhart,1 Johnnie Lee,1 Gabrielle Caron-Lapointe,2 Fangzhou Wei,3 Marie-Hélène Lafeuille2
1Janssen Scientific Affairs, LLC, Titusville, NJ, USA; 2Analysis Group, Inc, Montréal, QC, Canada; 3Analysis Group, Inc, Menlo Park, CA, USA
Correspondence: Carmine Rossi, Analysis Group, Inc, 1190 Avenue des Canadiens-de-Montréal, Tour Deloitte, Suite 1500, Montréal, QC, H3B 0G7, Canada, Tel +1 514-871-4233, Email [email protected]
Introduction: Integrase strand transfer inhibitor-based regimens (eg, containing dolutegravir [DTG]) are associated with weight/body mass index (BMI) increases among people living with HIV-1 (PLWH). Assessing antiretroviral therapy (ART)-related weight/BMI changes is challenging, as PLWH may experience return-to-health weight gain as a result of viral suppression. This retrospective, longitudinal real-world study compared weight/BMI outcomes among overweight/obese (BMI ≥ 25 kg/m2; thus excluding return-to-health weight/BMI changes), treatment-naïve PLWH who initiated darunavir (DRV)/cobicistat (c)/emtricitabine (FTC)/tenofovir alafenamide (TAF) or DTG + FTC/TAF.
Methods: Treatment-naïve PLWH with BMI ≥ 25 kg/m2 who initiated DRV/c/FTC/TAF or DTG + FTC/TAF (index date) had ≥ 12 months of baseline observation and ≥ 1 weight/BMI measurement in baseline and post-index periods in the Symphony Health IDV® database (07/17/2017– 12/31/2021) were included. Inverse probability of treatment weighting (IPTW) was used to balance differences in baseline characteristics between cohorts. On-treatment time-to-weight/BMI increases ≥ 5% were compared between cohorts using weighted adjusted Cox models.
Results: Post-IPTW, 76 overweight/obese DRV/c/FTC/TAF-treated (mean age = 51.2 years, 30.7% female, 35.6% Black, mean baseline BMI = 33.2 kg/m2) and 88 overweight/obese DTG + FTC/TAF-treated PLWH (mean age = 51.5 years, 31.4% female, 31.4% Black, mean baseline BMI = 32.7 kg/m2) were included. The median [interquartile range] time from ART initiation to weight/BMI increase ≥ 5% was shorter for the DTG + FTC/TAF cohort (21.8 [9.9, 32.3] months) than the DRV/c/FTC/TAF cohort (median and interquartile times not reached; Kaplan–Meier rate at 21.8 months = 20.8%). Over the entire follow-up, overweight/obese PLWH initiating DTG + FTC/TAF had a more than twofold greater risk of experiencing weight/BMI increase ≥ 5% compared to those initiating DRV/c/FTC/TAF (hazard ratio [95% confidence interval]=2.43 [1.02; 7.04]; p = 0.036).
Conclusion: Overweight/obese PLWH who initiated DTG + FTC/TAF had significantly greater risk of weight/BMI increase ≥ 5% compared to similar PLWH who initiated DRV/c/FTC/TAF and had shorter time-to-weight/BMI increase ≥ 5%, suggesting a need for additional monitoring to assess the risk of weight gain-related cardiometabolic disease.
Keywords: human immunodeficiency virus, weight gain, BMI, darunavir, dolutegravir, observational study
Introduction
The emergence of antiretroviral therapy (ART) to treat people living with HIV-1 (PLWH) has resulted in marked improvements in life expectancy, clinical outcomes, and quality of life.1–4 However, the longer life expectancy reported among PLWH in United States (US)5 has also led to an increase in the prevalence of chronic cardiometabolic disease and other aging-related comorbidities for PLWH treated with ART.6,7 As the prevalence of obesity has also increased among ART initiators (from 9% in 1998 to 18% in 2010),8 weight gain has emerged as an important clinical consideration among PLWH and a risk factor for cardiometabolic disease for those treated with ART.9
The US Department of Health and Human Services (DHHS) guidelines generally recommend ART regimens containing either dolutegravir (DTG) or bictegravir (BIC), both integrase strand transfer inhibitors (INSTIs), for the majority of newly diagnosed PLWH initiating treatment who do not have a history of using long-acting injectable pre-exposure prophylaxis.10 Pharmacokinetic-enhanced protease inhibitors (PIs), including darunavir (DRV), are also specifically recommended among PLWH who have yet to receive baseline laboratory and resistance testing results but need to initiate treatment rapidly or among those who are at risk of non-adherence.10 Of note, despite INSTIs being recommended for most PLWH, the US DHHS guidelines also highlight the greater risk of weight gain for INSTI-based regimens relative to other approved ART regimens. INSTI-related weight gain has been further confirmed in a recent systematic literature review of previously published real-world studies that showed that PLWH treated with an agent from the INSTI class experienced greater weight gain or body mass index (BMI) increase than with agents from other ART classes.11
Specifically, when compared to PIs, INSTI-based ART has been associated with greater weight and BMI increase after initiation in both treatment-naïve and treatment-experienced PLWH.12,13 DTG, in particular, has been noted in multiple settings to lead to a greater weight increase in treatment-naïve PLWH relative to other INSTIs and other ART classes.14–16 Furthermore, beyond INSTIs, and potentially compounding the effect on weight outcomes, tenofovir alafenamide (TAF), a backbone agent used in many ART regimens, has been associated with greater weight increases than other backbone agents (eg, tenofovir disoproxil fumarate or abacavir/lamivudine).17–22 Assessing the impact of ART on weight or BMI change among PLWH in the real-world has been challenging, given that many PLWH who initially lost weight after HIV infection may experience a return-to-health following treatment initiation and achieving viral suppression.23,24 One strategy to capture weight or BMI changes beyond the return-to-health phenomenon would be to evaluate ART-related weight/BMI changes among PLWH who are overweight or obese. The Centers for Disease Control and Prevention considers adults with a BMI ≥25 and <30 kg/m2 as overweight, whereas those with a BMI ≥30 kg/m2 are considered obese; it further subdivides obesity into the following categories: Class 1 (BMI of 30 to <35 kg/m2), Class 2 (BMI of 35 to <40 kg/m2), and 3 (BMI ≥40 kg/m2).25 However, there are limited data on weight/BMI changes among treatment-naïve PLWH who are overweight or obese, who may be at a greater risk of experiencing longer-term cardiovascular or metabolic outcomes, after initiating ART.26 To help separate the impact of treatment on ART-related weight gain relative to return-to-health weight gain, the objective of this study was to describe and compare real-world weight and BMI changes in treatment-naïve PLWH who are overweight or obese (ie, BMI ≥25 kg/m2; thus excluding weight/BMI changes occurring due to return-to-health phenomenon) and who initiated either DRV/cobicistat (c)/emtricitabine (FTC)/TAF or DTG + FTC/TAF in the US.
Materials and Methods
Data Source
To identify the study population and conduct the analysis, this study used nationwide US electronic medical records (EMR) data from the Symphony Health, an ICON plc company, IDV® database from 07/17/2017 to 12/31/2021. Historical clinical information such as clinical diagnoses, weight and BMI measurements, medications prescribed and administered, vitals, and lab results are included as part of this provider-based EMR database. The data contains de-identified information and is compliant with the patient requirements of the Health Insurance Portability and Accountability Act (HIPAA).
Study Design
This study used a retrospective longitudinal cohort study design. Adult (≥18 years old), PLWH with BMI ≥25 kg/m2 initiated on DRV/c/FTC/TAF or DTG + FTC/TAF between 07/17/2018 and 08/31/2021 were included. The same backbone agents (ie, FTC/TAF) were required for all PLWH, to isolate the effect that the third agent (ie, DRV/c or DTG) has on weight/BMI changes. Mutually exclusive DRV/c/FTC/TAF or DTG + FTC/TAF cohorts were created based on the first observed prescription for DRV/c/FTC/TAF or DTG (index date), with no previous ART prescriptions observed in the 12-month period prior to the index date, to ascertain that these were treatment-naïve cohorts. PLWH were considered for inclusion in the DTG + FTC/TAF cohort if FTC/TAF was received within 14 days before or after the first DTG prescription date.
The baseline period, during which patients were required to have a weight or BMI measurement, was defined as the 12-month period before the index date. For PLWH without a weight/BMI measurement during the baseline period, weight/BMI was further assessed up until 30 days post-index, given weight/BMI changes during this period are likely unrelated to the index ART.8 An on-treatment approach was used to define the follow-up period, which spanned from 30 days after the index date until the earliest of initiation of a new ART regimen, end of continuous clinical activity, or end of data availability (ie, 12/31/2021).
Study Population
Adult PLWH were included in this study if they initiated DRV/c/FTC/TAF or DTG + FTC/TAF between 07/17/2018 and 08/31/2021 (to allow sufficient potential follow-up before the end of data to observe ≥1 weight or BMI measurement starting 30 days post-index), had ≥1 diagnosis code for HIV-1 on or prior to the index date (International Classification of Disease, Ninth Revision, Clinical Modification [ICD-9-CM]: 042, 795.71 and V08; International Classification of Disease, Tenth Revision, Clinical Modification [ICD-10-CM] codes: B20, R75, and Z21), had ≥12 months of clinical activity prior to the index date (ie, baseline period), were ≥18 years old on the index date, had ≥1 weight measurement in both the baseline (including the first 30 days after baseline) and follow-up periods or ≥1 BMI measurement in both the baseline (including the first 30 days after baseline) and follow-up periods, and had their most recent baseline BMI measurement ≥25 kg/m2.
PLWH were excluded if they had ≥1 prescription for ART during the baseline period (excluding prescriptions for FTC/TAF in the 14 days preceding the index date for the DTG + FTC/TAF cohort); had ≥1 diagnosis code for HIV-2 during the baseline period, had ≥1 diagnosis code for cirrhosis or hepatitis during the baseline period; had ≥1 diagnosis code for stage V chronic kidney disease or end-stage renal disease, or creatine clearance <15 mL/min during the baseline period; had ≥1 diagnosis code for pregnancy during the baseline period or on the index date; had ≥1 diagnosis code for cancer, except for resected non-invasive cutaneous squamous carcinoma, basal cell carcinoma, or cutaneous Kaposi’s sarcoma during the baseline period; or had a prescription for both DRV/c/FTC/TAF and DTG on the index date.
Study Measures
A description of the demographic and clinical characteristics during the baseline period was performed for the DRV/c/FTC/TAF or DTG + FTC/TAF cohorts. The baseline weight/BMI measurement was the measurement closest to the index date in the baseline period, or within 30 days post-index if no baseline measurements were available.
Time to weight or BMI increase of ≥5% or ≥10% above the baseline weight/BMI measurement was evaluated over the entire follow-up period and compared between the DRV/c/FTC/TAF and DTG + FTC/TAF cohorts. Change in BMI categories between the baseline and follow-up (ie, on-treatment measurement furthest from the index date) periods was described for the two cohorts separately. In addition, mean differences, as well as percentage increases (ie, >0% increase, ≥5% increase, and ≥10% increase) in weight and BMI between the baseline and follow-up periods were explored at 3-, 6-, 9-, and 12-month time points during the follow-up period and described in the DRV/c/FTC/TAF and DTG + FTC/TAF cohorts. Mean follow-up weight/BMI measurements for each time point were based on all weight/BMI measurements observed during the specific 3-month interval of interest.
Statistical Analysis
Baseline characteristics were balanced between PLWH in the DRV/c/FTC/TAF and DTG + FTC/TAF cohorts using inverse probability treatment weighting (IPTW). Weights were calculated based on propensity scores (PSs) obtained from a logistic regression model that included the following independent variables: age, sex at birth, race, geographic region, insurance plan type, year of the index date, Quan-Charlson Comorbidity index (Quan-CCI) excluding HIV-1 symptoms, hypertension, baseline BMI, use of medications associated with weight gain, and use of antihypertensives. For each individual, the IPTW-derived weight was calculated as 1/PS for PLWH in the DRV/c/FTC/TAF cohort and 1/(1-PS) for PLWH in the DTG + FTC/TAF cohort. In addition, IPTW-derived weights were normalized by the mean treatment weight. In the resulting IPTW-weighted sample, each individual’s contribution was based on their reweighted representation, and the IPTW-weighted sample size for each cohort was calculated as the sum of the IPTW-derived weight for each individual in that cohort. Therefore, even though the same individuals were included in the analysis before and after weighting, the IPTW-weighted sample size was different from the sample size before applying IPTW.27 Based on the calculations above, the average treatment effect was obtained from the comparison of weight/BMI changes between the IPTW-weighted DRV/c/FTC/TAF and DTG + FTC/TAF cohorts.
Comparison of baseline characteristics after applying IPTW was made using standardized differences, with differences of <10% being considered balanced.28 The time to weight or BMI increase ≥5% or ≥10% was described for the DRV/c/FTC/TAF and DTG + FTC/TAF cohorts using weighted Kaplan–Meier (KM) analysis. In addition, hazard ratios (HRs) estimated based on weighted Cox proportional hazard models were used to compare the time to weight or BMI increase of ≥5% or ≥10% between cohorts. Mean differences estimated based on weighted ordinary least squares regression models were used to compare the mean change in weight/BMI from the baseline period to each follow-up time point between the DRV/c/FTC/TAF and DTG + FTC/TAF cohorts. The proportion of PLWH with >0% increase, ≥5% increase, or ≥10% increase in weight or BMI between the baseline and each follow-up time point was also described between cohorts. Remaining imbalances in baseline characteristics (after applying IPTW) were adjusted for in all IPTW-weighted regression models to obtain doubly robust estimates. The following baseline variables were adjusted for: race, geographic region, insurance plan type, and dyslipidemia/hyperlipidemia during baseline. All 95% confidence intervals (CIs) and p-values were calculated using non-parametric bootstrap procedures with 500 iterations.
Results
Patient Characteristics
A total of 164 PLWH who were overweight or obese were eligible for analysis, of which 51 were included in the DRV/c/FTC/TAF cohort and 113 were included in the DTG + FTC/TAF cohort (Figure 1). After IPTW, the weighted sample size yielded 76 PLWH in the DRV/c/FTC/TAF cohort (mean age: 51.2 years, 30.7% female, 35.6% Black, 71.1% resided in the South) and 88 PLWH in the DTG + FTC/TAF cohort (mean age: 51.5 years, 31.4% female, 31.4% Black, 63.9% resided in the South; Table 1). The mean (standard deviation [SD]) baseline BMI was 33.2 (6.5) kg/m2 in the DRV/c/FTC/TAF cohort and 32.7 (6.0) kg/m2 in the DTG + FTC/TAF cohort. The mean (SD) baseline weight was 99.4 (20.6) kg [219.1 lbs] in the DRV/c/FTC/TAF cohort and 98.0 (18.7) kg [216.1 lbs] in the DTG + FTC/TAF cohort, and the mean (SD) follow-up period was 16.6 (9.7) months in the DRV/c/FTC/TAF cohort and 15.5 (9.7) months in the DTG + FTC/TAF cohort.
 |
Table 1 Baseline Demographics and Clinical Characteristics |
Time to Weight or BMI Increase ≥5% or ≥10%
The DTG + FTC/TAF cohort had a shorter median [interquartile range (IQR)] time from ART initiation to weight gain ≥5% (21.8 [9.9, 32.3] months) than the DRV/c/FTC/TAF cohort (median and interquartile times not reached; Figure 2a). At 24 months, descriptively higher rates of weight increase ≥5% based on KM analyses were observed among PLWH in the DTG + FTC/TAF cohort (KM rate [95% CI] = 50.6% [34.6%; 69.0%]; n = 6 remaining at risk, ie, PLWH who did not have weight increase ≥5%, but who are still observable at 24 months) than PLWH in the DRV/c/FTC/TAF cohort (KM rate [95% CI] = 20.8% [9.1%; 43.6%]; n = 14 remaining at risk). Similarly, at 24 months, PLWH in the DTG + FTC/TAF (n = 10 remaining at risk) cohort had descriptively higher rates of weight increase ≥10% (KM rate [95% CI] = 21.7% [12.4%; 36.4%]; median [IQR] time not reached [25.0 months, not reached]) than PLWH in the DRV/c/FTC/TAF cohort (KM rate [95% CI] = 5.3% [0.7%; 33.4%]; n = 17 remaining at risk; median and interquartile times not reached; Figure 2b).
Figure 2 Continued.
Similar trends were observed for BMI increases ≥5% and ≥10% (Figures 2c and d). Over the entire follow-up period, PLWH who were overweight or obese and initiated DTG + FTC/TAF had a more than twofold greater risk of experiencing a weight or BMI increase ≥5% as compared to PLWH who were overweight or obese and initiated DRV/c/FTC/TAF (HR [95% CI] = 2.43 [1.02; 7.04]; p = 0.036; Figure 3). The comparative analysis for weight/BMI increase ≥10% did not converge, given the small number of events. Nevertheless, over the entire follow-up, the proportion of patients with weight/BMI increase ≥10% was descriptively higher for the DTG + FTC/TAF (14.9%) than for the DRV/c/FTC/TAF cohort (6.9%).
Change Between Baseline and Latest Follow-Up BMI Category
During follow-up, 26.3% (20/76) of PLWH in the DRV/c/FTC/TAF cohort and 31.8% (28/88) of PLWH in the DTG + FTC/TAF cohort experienced a change in BMI category between the baseline and follow-up periods (Table 2). More specifically, 17.0% (15/88) of DTG + FTC/TAF initiators increased one BMI category relative to 14.4% (11/76) of DRV/c/FTC/TAF initiators. A descriptively higher proportion of Class 3 obese DRV/c/FTC/TAF PLWH moved to Class 2 obesity (26.4%) than Class 3 obesity (10.1%). A descriptively higher proportion of Class 1 obese DTG + FTC/TAF PLWH progressed to Class 2 obesity (15.7%) than Class 1 obesity (0.0%).
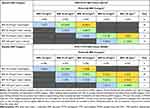 |
Table 2 Baseline BMI Category and Proportion of PLWH with BMI Category Shiftsa During Follow-Up |
Comparison of Weight and BMI Change at Specific Time Points
PLWH in the DTG + FTC/TAF cohort experienced descriptively greater absolute weight or BMI increases than PLWH in the DRV/c/FTC/TAF cohort, with results reaching statistical significance at 12 months (Supplementary Figure 1). Weighted doubly robust mean differences in weight ranged from 1.36 kg [3.00 lbs] at 3 months (increase for DTG + FTC/TAF cohort: Δ3 months= +0.49 kg [+1.08 lbs]; decrease for DRV/c/FTC/TAF cohort: Δ3 months= −0.67 kg [−1.48 lbs]; p = 0.18) to 4.08 kg [8.99 lbs] at 12 months (increase for DTG + FTC/TAF cohort: Δ12 months= +0.49 kg [+1.08 lbs]; decrease for DRV/c/FTC/TAF cohort: Δ12 months= −2.14 kg [−4.72 lbs]; p = 0.024). At each time point, PLWH in the DRV/c/FTC/TAF cohort experienced an overall mean decrease in weight post-index, while PLWH in the DTG + FTC/TAF cohort experienced an overall mean increase in weight post-index. Results were consistent for the comparison of mean BMI differences between the DRV/c/FTC/TAF and DTG + FTC/TAF cohorts, with results reaching statistical significance at 12 months (Supplementary Figure 1). The proportion of PLWH who were overweight or obese that experienced ≥5% or ≥10% weight/BMI increase was numerically higher in the DTG + FTC/TAF cohort compared to the DRV/c/FTC/TAF cohort at each time point (Supplementary Table 1).
Discussion
To the authors’ knowledge, this real-world study is the first to compare changes in weight or BMI between PLWH who were overweight or obese and initiated a DRV/c-based regimen compared with PLWH who initiated a DTG-based regimen that included the same FTC/TAF nucleoside reverse transcriptase inhibitor backbone. In PLWH, it can be difficult to separate the effect of individual medications in an ART regimen on weight gain from the return-to-health phenomenon observed when PLWH begin ART.24 Furthermore, the most recent US DHHS HIV treatment guidelines specifically call out the concern for excess weight gain associated with INSTI-based regimens that include DTG or bictegravir compared to non-nucleoside reverse transcriptase inhibitor (NNRTI)- or PI-based regimens.10 Thus, addressing the question of the impact of different ART regimens on weight change among PLWH who were initially overweight or obese is important as there has already been an observed increase in the prevalence of obesity among PLWH initiating ART.8 Hence, the current study focused on an understudied population, ie, PLWH who were already overweight or obese (BMI ≥25 kg/m2) at baseline prior to ART initiation, in an effort to exclude PLWH experiencing the return-to-health phenomenon and better ascertain the effect of specific ART regimens on weight gain.
Based on this study design, it was found that PLWH treated with DTG + FTC/TAF experienced a more than twofold (HR = 2.43) greater risk of weight/BMI increase ≥5% while on treatment compared to DRV/c/FTC/TAF. The DTG + FTC/TAF cohort also had a shorter median time to weight gain related to the DRV/c/FTC/TAF cohort, such that 51% of the overweight or obese DTG + FTC/TAF cohort (vs 21% in DRV/c/FTC/TAF cohort) experienced the ≥5% weight/BMI outcome within 2 years of starting treatment, with differences between the two cohorts starting to appear as early as after 3 months of follow-up. In addition, PLWH treated with DTG + FTC/TAF experienced an increase in mean weight gain/BMI increase at each time point up to 12 months post-treatment initiation, whereas PLWH who initiated DRV/c/FTC/TAF experienced a decrease in mean weight gain/BMI at each time point over the same period.
Findings of the current study are consistent with several previous real-world analyses, which have demonstrated increased weight gain associated with initiating therapy with an INSTI-based regimen relative to other types of regimens, such as those that are PI-based.12,29,30 In a large retrospective real-world study of 20,367 PLWH in the US, those who initiated a new PI were 39% less likely to experience ≥5% weight gain (p = 0.014) and 49% less likely to experience a ≥5% BMI gain (p < 0.001) than PLWH who initiated a new INSTI.12 Similar associations have been observed for INSTI-based regimens compared to NNRTI-based regimens.16,31,32 A retrospective longitudinal study of 22,972 PLWH from the North American AIDS Cohort Collaboration on Research and Design found that after 5 years of ART, PLWH who initiated an INSTI-based regimen experienced mean weight gain of 5.9 kg [13.0 lbs], compared to 3.7 kg [8.2 lbs] for NNRTI-based regimens.16
Within the INSTI class of ART, DTG has been linked to a higher risk of weight gain and an increase in BMI, relative to other INSTI drugs or NNRTI-based regimens.15,33,34 In one study of 1152 treatment-naive PLWH from the Vanderbilt Comprehensive Care Clinic cohort, the adjusted average weight gains for PLWH treated with DTG at 18 months were significantly higher compared to gains for NNRTIs or elvitegravir (6.0 kg [13.2 lbs] vs 2.6 kg [5.7 lbs] and 0.5 kg [1.1 lbs], respectively; both p < 0.05).15 These findings are also supported by a recent systematic literature review and network meta-analysis of 73 studies spanning approximately 10 years (2011 to September 13, 2021), which found that DTG-based regimens can result in significantly higher average weight gains relative to other ART regimens, including NNRTIs and elvitegravir/c.34
Weight change in PLWH remains an important topic in patients initiating an ART regimen, as there are potential implications on downstream clinical outcomes. For instance, various studies have shown an increase in the risk of type II diabetes mellitus among obese PLWH.9,24,35–38 In a study that analyzed data of 9193 PLWH from the Data Collection on Adverse Events of Anti-HIV Drugs (D:A:D) study, adjusted models reported an incidence rate ratio for the risk of diabetes mellitus of 1.12 (95% CI: 1.04, 1.22; p = 0.005) for every unit gain in BMI after 1 year of ART therapy.35 A separate retrospective longitudinal real-world study of treatment-naïve adult female, Black, or Hispanic PLWH who initiated ART found that PLWH who experienced a ≥ 5% weight/BMI gain (n = 620) after initiating ART were significantly more likely (HR = 2.19; p = 0.044) to be diagnosed with type 2 diabetes mellitus during a mean 2-year follow-up period.9 While additional research is warranted, these findings suggest that ART regimens may play a role in the increased risk of additional comorbidities among PLWH. For PLWH, who are already overweight or obese, ART-associated weight gain may further compound the risk of chronic cardiometabolic disease and other aging-related comorbidities. Future studies are warranted to evaluate consequences of ART-related weight gain in PLWH.
Limitations
Some limitations apply to the data used and analyses conducted as part of the current study. First, EMR data may contain inaccuracies or omissions in diagnoses, medication use, and other variables. Second, it was assumed that the prescribed ART medication was taken as indicated. Third, the provider-based data source used in this study does not capture the services PLWH may have received from providers outside of the network. Fourth, since this study population included treatment-naïve PLWH, results may not be generalizable to treatment-experienced PLWH. Similarly, given that only PLWH who are overweight/obese were included in the present study, findings may not be generalizable to the population of PLWH who are not overweight or obese. Fifth, despite using IPTW and adjusting for many variables available in the data, unmeasured confounders associated with weight/BMI changes (eg, lifestyle changes, diet, physical activity, contraceptive methods) may remain; however, it is not possible to determine what impact these unmeasured confounders may have on the results, as these are not observable in the data. Sixth, variables such as waist circumference and laboratory results (eg, HIV viral load and CD4+ cell count), which may be associated with weight change, could not be included in the PS model for balancing, as they were unavailable for the majority of PLWH in the sample. In addition, use of pre-exposure prophylaxis was not measured in the period prior to the 12-month baseline period; however, there is no reason to indicate that this would differ between the two cohorts, so it is thus likely not a confounder for this study. Finally, while results consistently showed greater weight/BMI increases for DTG + FTC/TAF relative to DRV/c/FTC/TAF, the ability to detect statistically significant results for the comparison of weight and BMI change at specific time points was limited by small sample size.
Conclusions
Treatment-naïve PLWH who were overweight or obese and initiated ART with DTG + FTC/TAF were at significantly greater risk of experiencing weight or BMI increase ≥5% compared to PLWH who were overweight or obese and initiated DRV/c/FTC/TAF. Based on these findings, it may be important for PLWH who are at greater risk of developing cardiovascular and metabolic conditions associated with obesity to carefully select their initial ART regimen. Future studies with larger sample sizes and additional follow-up are needed to confirm these findings, particularly among PLWH using newer ART formulations of DTG (ie, DTG/lamivudine).
Data Sharing Statement
The data that support the findings of this study are available from Symphony Health, an ICON plc Company. Restrictions apply to the availability of these data, which were used under license for this study.
Ethics Statement
Data were de-identified and comply with the patient requirements of the Health Insurance Portability and Accountability Act (HIPAA) of 1996; therefore, no review by an institutional review board was required per Title 45 of CFR, Part 46.101(b)(4) (https://www.hhs.gov/ohrp/regulations-and-policy/regulations/45-cfr-46/#46.101).
Acknowledgments
Medical writing support was provided by Cody Patton, BSc, an independent consultant working on behalf of Analysis Group, Inc., a consulting company that has provided paid consulting services to Janssen Scientific Affairs, LLC, which funded the development and conduct of this study and manuscript.
Author Contributions
All authors have made substantial contributions to the conception or design of the study, or the acquisition, analysis, or interpretation of data, drafting the manuscript and revising it critically for important intellectual content, and have provided final approval of this version to be published and agree to be accountable for all aspects of the work. All authors reviewed and approved the final content of this manuscript and agreed to submit the manuscript to ClinicoEconomics and Outcomes Research.
Funding
This study was funded by Janssen Scientific Affairs, LLC. The study sponsor was involved in several aspects of the research, including the study design, interpretation of data, and writing of the manuscript.
Disclosure
Prina Donga, Brahim K. Bookhart, and Johnnie Lee are employees of Janssen Scientific Affairs, LLC and are stockholders of Johnson & Johnson. Bruno Emond, Carmine Rossi, Gabrielle Caron-Lapointe, Fangzhou Wei, and Marie-Hélène Lafeuille are employees of Analysis Group, Inc., a consulting company that provided paid consulting services to Janssen Scientific Affairs, LLC. The authors report no other conflicts of interest in this work.
References
1. Bavinton BR, Pinto AN, Phanuphak N, et al. Viral suppression and HIV transmission in serodiscordant male couples: an international, prospective, observational, cohort study. Lancet HIV. 2018;5(8):e438–e447. doi:10.1016/S2352-3018(18)30132-2
2. Palella FJ Jr, Delaney KM, Moorman AC, et al. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. HIV Outpatient Study Investigators. N Engl J Med. 1998;338(13):853–860. doi:10.1056/nejm199803263381301
3. Sterne JA, Hernán MA, Ledergerber B, et al. Long-term effectiveness of potent antiretroviral therapy in preventing AIDS and death: a prospective cohort study. Lancet. 2005;366(9483):378–384. doi:10.1016/s0140-6736(05)67022-5
4. Farnham PG, Gopalappa C, Sansom SL, et al. Updates of lifetime costs of care and quality-of-life estimates for HIV-infected persons in the United States: late versus early diagnosis and entry into care. J Acquir Immune Defic Syndr. 2013;64(2):183–189. doi:10.1097/QAI.0b013e3182973966
5. Marcus JL, Leyden WA, Alexeeff SE, et al. Comparison of overall and comorbidity-free life expectancy between insured adults with and without HIV infection, 2000-2016. JAMA Netw Open. 2020;3(6):e207954. doi:10.1001/jamanetworkopen.2020.7954
6. Losina E, Hyle EP, Borre ED, et al. Projecting 10-year, 20-year, and lifetime risks of cardiovascular disease in persons living with human immunodeficiency virus in the United States. Clin Infect Dis. 2017;65(8):1266–1271. doi:10.1093/cid/cix547
7. Siddiqi KA, Ostermann J, Zhang J, Khan MM, Olatosi B. Ageing with HIV in the United States: changing trends in inpatient hospital stays and comorbidities, 2003-2015. HIV Med. 2023;24(1):93–103. doi:10.1111/hiv.13325
8. Koethe JR, Jenkins CA, Lau B, et al. Rising obesity prevalence and weight gain among adults starting antiretroviral therapy in the United States and Canada. AIDS Res Hum Retroviruses. 2016;32(1):50–58. doi:10.1089/aid.2015.0147
9. McComsey GA, Emond B, Shah A, et al. Association between weight gain and the incidence of cardiometabolic conditions among people living with HIV-1 at high risk of weight gain initiated on antiretroviral therapy. Infect Dis Ther. 2022;11(5):1883–1899. doi:10.1007/s40121-022-00673-1
10. U.S. Department of Health and Human Services. Guidelines for the Use of Antiretroviral Agents in Adults and Adolescents Living with HIV. Available from: https://clinicalinfo.hiv.gov/sites/default/files/guidelines/documents/adult-adolescent-arv/guidelines-adult-adolescent-arv.pdf.
11. Hester EK, Greenlee S, Durham SH. Weight changes with integrase strand transfer inhibitor therapy in the management of HIV infection: a systematic review. Ann Pharmacother. 2022;10600280211073321. doi:10.1177/10600280211073321
12. Chow W, Donga P, Côté-Sergent A, et al. An assessment of weight change associated with the initiation of a protease or integrase strand transfer inhibitor in patients with human immunodeficiency virus. Curr Med Res Opin. 2020;36(8):1313–1323. doi:10.1080/03007995.2020.1775074
13. Emond B, Rossi C, Cote-Sergent A, et al. Body mass index increase and weight gain among people living with HIV-1 initiated on single-tablet darunavir/cobicistat/emtricitabine/tenofovir alafenamide or bictegravir/emtricitabine/tenofovir alafenamide in the United States. Curr Med Res Opin. 2022;38(2):287–298. doi:10.1080/03007995.2021.2007006
14. Bourgi K, Ofner S, Musick B, et al. Weight gain among treatment-naive persons with HIV receiving dolutegravir in Kenya. J Acquir Immune Defic Syndr. 2022;91(5):490–496. doi:10.1097/QAI.0000000000003087
15. Bourgi K, Rebeiro PF, Turner M, et al. Greater weight gain in treatment-naive persons starting dolutegravir-based antiretroviral therapy. Clin Infect Dis. 2020;70(7):1267–1274. doi:10.1093/cid/ciz407
16. Bourgi K, Jenkins CA, Rebeiro PF, et al. Weight gain among treatment-naïve persons with HIV starting integrase inhibitors compared to non-nucleoside reverse transcriptase inhibitors or protease inhibitors in a large observational cohort in the United States and Canada. J Int AIDS Soc. 2020;23(4):e25484. doi:10.1002/jia2.25484
17. Emond B, Rossi C, Rogers R, Lefebvre P, Lafeuille MH, Donga P. Real-world analysis of weight gain and body mass index increase among patients with HIV-1 using antiretroviral regimen containing tenofovir alafenamide, tenofovir disoproxil fumarate, or neither in the United States. J Health Econ Outcomes Res. 2022;9(1):39–49. doi:10.36469/jheor.2022.31825
18. Gomez M, Seybold U, Roider J, Harter G, Bogner JR. A retrospective analysis of weight changes in HIV-positive patients switching from a tenofovir disoproxil fumarate (TDF)- to a tenofovir alafenamide fumarate (TAF)-containing treatment regimen in one German University Hospital in 2015-2017. Infection. 2019;47(1):95–102. doi:10.1007/s15010-018-1227-0
19. Sax PE, Erlandson KM, Lake JE, et al. Weight gain following initiation of antiretroviral therapy: risk factors in randomized comparative clinical trials. Clin Infect Dis. 2020;71(6):1379–1389. doi:10.1093/cid/ciz999
20. Schafer JJ, Sassa KN, O’Connor JR, Shimada A, Keith SW, DeSimone JA. Changes in body mass index and atherosclerotic disease risk score after switching from tenofovir disoproxil fumarate to tenofovir alafenamide. Open Forum Infect Dis. 2019;6(10):ofz414. doi:10.1093/ofid/ofz414
21. Taramasso L, Berruti M, Briano F, Di Biagio A. The switch from tenofovir disoproxil fumarate to tenofovir alafenamide determines weight gain in patients on rilpivirine-based regimen. AIDS. 2020;34(6):877–881. doi:10.1097/QAD.0000000000002496
22. Venter WDF, Moorhouse M, Sokhela S, et al. Dolutegravir plus two different prodrugs of tenofovir to treat HIV. N Engl J Med. 2019;381(9):803–815. doi:10.1056/NEJMoa1902824
23. Yuh B, Tate J, Butt AA, et al. Weight change after antiretroviral therapy and mortality. Clin Infect Dis. 2015;60(12):1852–1859. doi:10.1093/cid/civ192
24. Kumar S, Samaras K. The impact of weight gain during HIV treatment on risk of pre-diabetes, diabetes mellitus, cardiovascular disease, and mortality. Front Endocrinol (Lausanne). 2018;9:705. doi:10.3389/fendo.2018.00705
25. Centers for Disease Control and Prevention. Defining Adult Overweight & Obesity. Available from: https://www.cdc.gov/obesity/basics/adult-defining.html.
26. Achhra AC, Sabin C, Ryom L, et al. Body mass index and the risk of serious non-AIDS events and all-cause mortality in treated HIV-positive individuals: d: a: d cohort analysis. J Acquir Immune Defic Syndr. 2018;78(5):579–588. doi:10.1097/QAI.0000000000001722
27. Austin PC, Stuart EA. Moving towards best practice when using inverse probability of treatment weighting (IPTW) using the propensity score to estimate causal treatment effects in observational studies. Stat Med. 2015;34(28):3661–3679. doi:10.1002/sim.6607
28. Austin PC. Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Commun Stat Simul Comput. 2009;38(6):1228–1234.
29. Chen YW, Anderson D, Pericone CD, Donga P. Real-world assessment of weight change in African American females and Hispanics with HIV-1 after initiating integrase strand-transfer inhibitors or protease inhibitors. J Health Econ Outcomes Res. 2022;9(1):1–10. doi:10.36469/001c.30184
30. Chen YW, Hardy H, Pericone CD, Chow W. Real-world assessment of weight change in people with HIV-1 after initiating integrase strand transfer inhibitors or protease inhibitors. J Health Econ Outcomes Res. 2020;7(2):102–110. doi:10.36469/jheor.2020.13457
31. Kline MDA, Daniels C, Xu X, et al. Antiretroviral therapy anchor-based trends in body mass index following treatment initiation among military personnel with HIV. Mil Med. 2021;186(3–4):279–285. doi:10.1093/milmed/usaa416
32. Kerchberger AM, Sheth AN, Angert CD, et al. Weight gain associated with integrase strand transfer inhibitor use in women. Clin Infect Dis. 2020;71(3):593–600. doi:10.1093/cid/ciz853
33. Grabar S, Potard V, Piroth L, et al. Striking differences in weight gain after cART initiation depending on early or advanced presentation: results from the ANRS CO4 FHDH cohort. J Antimicrob Chemother. 1093;1:67.
34. Kanters S, Renaud F, Rangaraj A, et al. Evidence synthesis evaluating body weight gain among people treating HIV with antiretroviral therapy - a systematic literature review and network meta-analysis. EClinicalMedicine. 2022;48:101412. doi:10.1016/j.eclinm.2022.101412
35. Achhra AC, Mocroft A, Reiss P, et al. Short-term weight gain after antiretroviral therapy initiation and subsequent risk of cardiovascular disease and diabetes: the D:A:D study. HIV Med. 2016;17(4):255–268. doi:10.1111/hiv.12294
36. Bannister WP, Mast TC, de Wit S, et al. Changes in body mass index and clinical outcomes after initiation of contemporary antiretroviral regimens. AIDS. 2022;36(15):2107–2119. doi:10.1097/QAD.0000000000003332
37. McCann K, Shah S, Hindley L, et al. Implications of weight gain with newer anti-retrovirals: 10-year predictions of cardiovascular disease and diabetes. AIDS. 2021;35(10):1657–1665. doi:10.1097/qad.0000000000002930
38. Petoumenos K, Kuwanda L, Ryom L, et al. Effect of Changes in Body Mass Index on the Risk of Cardiovascular Disease and Diabetes Mellitus in HIV-Positive Individuals: results From the D:A:D Study. J Acquir Immune Defic Syndr. 2021;86(5):579–586. doi:10.1097/qai.0000000000002603
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.