Back to Journals » International Journal of Women's Health » Volume 15
Validating the Edinburgh Postnatal Depression Scale Against the Diagnostic and Statistical Manual of Mental Disorders, 5th Edition for Use in Uganda
Authors Atuhaire C, Brennaman L, Nambozi G, Taseera K, Atukunda EC , Ngonzi J, Atwine D, Matthews LT, Rukundo GZ
Received 3 August 2023
Accepted for publication 8 November 2023
Published 21 November 2023 Volume 2023:15 Pages 1821—1832
DOI https://doi.org/10.2147/IJWH.S427752
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 3
Editor who approved publication: Professor Elie Al-Chaer
Catherine Atuhaire,1 Laura Brennaman,1 Grace Nambozi,1 Kabanda Taseera,2 Esther C Atukunda,3 Joseph Ngonzi,4 Daniel Atwine,5 Lynn T Matthews,6,7 Godfrey Zari Rukundo8
1Department of Nursing, Mbarara University of Science and Technology, Mbarara, Uganda; 2Department of Microbiology, Mbarara University of Science and Technology, Mbarara, Uganda; 3Department of Pharmacy, Mbarara University of Science and Technology, Mbarara, Uganda; 4Department of Obstetrics & Gynaecology, Mbarara University of Science and Technology, Mbarara, Uganda; 5SOAR Research Foundation, Mbarara, Uganda; 6Division of Infectious Diseases and Center for Global Health Massachusetts General Hospital, Boston, MA, USA; 7Division of Infectious Disease, University of Alabama at Birmingham, Birmingham, AL, USA; 8Department of Psychiatry, Mbarara University of Science and Technology, Mbarara, Uganda
Correspondence: Catherine Atuhaire, Email [email protected]
Background: The Edinburgh Postnatal Depression Scale (EPDS) is a widely acknowledged screening tool for postpartum depression (PPD) globally, but its validation in Uganda has been lacking. This study aimed to assess the EPDS’s accuracy as a PPD screening tool in Uganda compared to the Mini-International Neuropsychiatric Interview (MINI 7.0.2) based on the DSM-5.
Methods: This was a descriptive cross-sectional study conducted at a referral hospital and two peri-urban primary care postpartum clinics in rural southwestern Uganda. We enrolled 287 mothers aged 18 to 49 at their six-week postpartum visit. The EPDS was used for initial screening, and the MINI 7.0.2 was employed for clinical diagnosis. The study used the Runyankore-Rukiga language version of the EPDS and collected data from November 11, 2019, to June 10, 2020, with the MINI 7.0.2 as the reference standard.
Results: The overall PPD prevalence was 29.5%, as opposed to 26.5% with EPDS and MINI 7.0.2 DSM-5 criteria (p = 0.239). The EPDS demonstrated a sensitivity of 86.8%, specificity of 92.1%, positive predictive value of 80.5%, and negative predictive value of 94.9%. A cutoff score of ≥ 10 was found to be the most effective acceptable point after drawing the AUC of ROC and determining the most appropriate point using Youden’s index. The area under the ROC curve, indicating the scale’s overall performance against MINI 7.0.2, was 0.89 for Bwizibwera HCIV, 0.97 for Kinoni HCIV, and 0.84 for MRRH. In conclusion, the EPDS can effectively screen for postpartum depression in southwestern Uganda using a cutoff score of ≥ 10. It exhibits strong diagnostic performance in correctly identifying PPD in postpartum mothers.
Keywords: validation, EPDS, DSM-5, MINI, postpartum depression
Background
Postpartum depression (PPD) is a type of mood disorder that can affect women following child birth. It is characterized by a persistent and often severe form of depression. PPD can have significant emotional, physical, and social impacts on the affected individuals. The short- and long-term impact of postpartum depression on the mother, her marital relationship, the children and community make it an important condition to screen, diagnose, treat and prevent.1 Routine use of screening scales for the purpose of identifying PPD symptoms is an effective, simple and economical way to identify women at risk for the disorder.2 Validating these screening scales provides standard clinical scales to compare symptoms and treatment efficacy across different populations of diverse cultural, emotional and economic backgrounds. There are several screening instruments for PPD and the most commonly used scale is the Edinburgh Postnatal Depression Scale (EPDS).3,4 The EPDS was originally developed in Edinburgh by Scottish Health Centers in 1987.5 It can be self-administered in literate communities and researcher administered for mothers who cannot read and write.3 The health worker administering this scale may not have specialized training in psychiatric disorders but should be familiar with mental health problems.6 The EPDS is used to assess emotional experiences over the previous 7 days using 10 Likert-scale items by assessing for sadness and fearfulness, loss of interest, anxiety and worry, sleep deficit, self-blame, sense of being overwhelmed, and suicidal ideation in postpartum women.7 It is simple, quick to score and has shown high acceptability levels by patients as well as being readily available without purchase expenses.8 Due to the limited number of psychiatrists in Uganda, it is anticipated that the EPDS will be utilized in the clinical practice by nurses and midwives to identify mothers suffering from PPD on postnatal clinics.
During validation of the EPDS among Scottish women in Edinburgh, the scale demonstrated a sensitivity of 86%, specificity of 78% yielding a positive predictive value of 73% at a cut-off of 10 or more out of 30 as set by Cox.3 In a primary health care setting the scale is recommended for its ability to detect change in the severity of depression over time.6,9 The few studies that were conducted in African settings reported the EPDS as a valid scale for assessing PPD. For example, Khalifa and others10 validated the EPDS against the Mini-International Neuropsychiatric Interview among postpartum women in South Sudan and the sensitivity and specificity were 89% and 82%, respectively. A related validation of the EPDS in Shona language against the DSM-IV criteria for major depression in Zimbabwe recorded sensitivity of 78% and specificity of 89%11 whereas in the Amharic language in Ethiopia researchers validated the EPDS against the Comprehensive Psychopathological Rating Scale (CPRS) and reported 78.9% sensitivity and 75.3% specificity.12
Although this scale has been validated in several countries, 60 languages and populations, it has been validated in very few African settings and most of these validations were for specific postpartum populations like postpartum mothers who are living with HIV or antenatal women.2,5,13 As far as we know, the EPDS has not been validated to establish the psychometrics in the Ugandan local context, yet a preliminary cross-sectional study revealed a high PPD prevalence of 27.1% using the clinical diagnostic criteria,14 hence there is a need to validate a reliable screening tool in this setting. The few studies on validation of the EPDS could be attributed to the fact that PPD was largely considered to be a Western phenomenon, with infrequent documentation in low-resource settings.9,15,16 However, currently PPD is increasingly recognized as a public health threat in low-resource settings such as Uganda and it requires a method of measuring depressive symptoms that is both valid and practical to administer. Such studies require careful consideration of the impact that culture and language may have upon the validity of the measures used. Whereas in general, PPD is characterized by loss of interest in usual events, sleep challenges, feelings of sadness, fatigability, problems of appetite, and difficulty in coping with daily activities,6 literature suggests that the presentation of PPD is different for African mothers as compared to mothers in higher income countries like Scotland. A study carried out by Cox et al revealed that Ugandan women were more likely to describe somatic symptoms like backaches, headaches during their routine postpartum health visits and less likely to express emotional feelings as compared to the Scottish mothers6,17 yet PPD manifests as a psychological clinical profile. This disparity in symptoms compromises accurate screening of mothers suffering from PPD, hence increasing the risk of consequences from this condition. The EPDS was developed to be used among the Scottish postpartum women. Consensus has emerged that such a scale can be used in other settings but that there must be a careful process of translation and validation by establishing its sensitivity, specificity and predictive values before usage to ensure cross-cultural equivalence.6,18,19 Moreover, researchers stress that a screening instrument must go through a formal validation in a particular population before it is implemented into practice.20 Therefore, this study validated the EPDS against the DSM-5 diagnostic criteria using the MINI 7.0.2 to determine its appropriateness in detecting PPD among mothers in southwestern Uganda.
Methods
Study Design and Setting
This descriptive, cross-sectional study was conducted at one regional referral hospital (Mbarara Regional Referral Hospital-MRRH) and two peri-urban primary care postpartum clinics (Bwizibwera Health Centre IV-BHC IV and Kinoni Health Centre IV-KHC IV) that serve rural communities with lower incomes and lower rates of formal education in Mbarara and Rwampara districts, south western region of Uganda. BHC IV and KHC IV are within a 26.3 km and 39.9 km radius, respectively, from MRRH located in the centre of Mbarara city. Services are provided free at all the clinics and the staffs at both clinics are employed by the government of Uganda. The most widely spoken language is Runyankore-Rukiga. This was part of a larger research project that determined the prevalence and associated factors of PPD in Mbarara and Rwampara districts, south western Uganda.14
Study Population and Eligibility Criteria
This study enrolled 18 to 49 years old mothers during their 6 weeks’ postpartum visit to the clinic for their routine 6 weeks’ postpartum check-up. The data were obtained from 11th November 2019 to 10th June 2020. The eligibility criteria included women able to speak and understand Runyankore-Rukiga, had delivered a live baby and were willing to participate in the study. Mothers who had lost their babies or those who were sick with severe medical illness, personal and family history of mood disorder were excluded as physical symptoms (insomnia, anorexia, decreased concentration and pain, etc.) and trauma of their loss could mimic those of depression and may bias the sample.
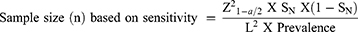
Sample Size Calculation
The sample size estimation for anticipated sensitivity and specificity was determined by the Burderer’s formula.21 Because the prevalence of PPD in Uganda was unknown at the time this study commenced but was later determined in a separate part of the current study, an arbitrary value of 50% had been assumed.
Where n = required sample size,
SN = anticipated sensitivity of EPDS as compared to MINI 7.0.2 = 82%. This was calculated as an average of the sensitivities of 89%, 78.9% and 78% that had been reported in Sudan, Ethiopia, and Zimbabwe, respectively.11,22,23
SP = anticipated specificity of EPDS as compared to MINI 7.0.2 = 82.1%. This was calculated as an average of the specificity of 82%, 75.3% and 89% that had been reported in Ethiopia, Zimbabwe and South Africa, respectively.11,22,23
α = size of the critical region = 0.1
z1-α/2 =1.96
L = absolute precision desired on either side of sensitivity or specificity = 0.09
After additional 10% to cater for non-response, a sensitivity-based sample size of 287 postpartum mothers were enrolled into the study.
Data Collection Tools
The Edinburgh Postnatal Depression Scale3 is a 10-item Likert scale (range 0–30). It is designed to screen for PPD by assessing for sadness and fearfulness, loss of interest, anxiety and worry, sleep deficit, self-blame, sense of being overwhelmed, and suicidal ideation.3 The original authors recommended that the cutoff point of this scale should be set at ≥10 out of a total score of 30.3 They further noted that this scale does not rely on somatic symptoms, which is common in postpartum women irrespective of depression.
The MINI 7.0.2 according to the DSM-524 was used to diagnose mothers suffering from postpartum depression. This is a semi-structured interview that assesses 17 most common disorders in mental health according to the DSM-5 but for this study we focused on symptoms of major depression.
Translation and Back Translation of the EPDS Before Data Collection
After obtaining permission from the original authors, the English version of the EPDS was translated into Runyankore-Rukiga by trained, bilingual professional translators (psychiatrist, graduate nurse and a midwife) who were on the study team. The team met to discuss the translations and ensure a version almost identical to the original one. The translated copies were then back translated to English for consistency and accuracy by two independent bilingual Runyankore-Rukiga speaking Ugandans, neither of whom are mental health experts. The translated and back translated content received no modification as this version was identical with the original English EPDS and this was in accordance with the principles for translation of the EPDS described in the EPDS manual.6 To evaluate if the initial translation was accurately performed, we piloted this tool with five women in Municipal Health Centre IV which is out of the study area. The Runyankore-Rukiga version of the EPDS is provided as Additional Files 1.
Participant Recruitment and Data Collection Process
Before study initiation, staff at the three postpartum clinic sites attended a 3-day training session conducted by investigators, in which the study procedures were explained in detail, including data collection and interview techniques with a focus on how to administer the different scales in different rooms. To evaluate criterion validity of the EPDS, we validated it against the MINI 7.0.2. The MINI 7.0.2 is designed to be administered by trained mental health workers. After obtaining consent from the eligible mothers and enrolling them into the study at each site, they were screened with the EPDS. The consenting, recruitment and screening process was implemented by trained nurses or midwives in one of the private rooms at each study site. Shortly afterwards, a clinical diagnosis was made for each participant in another private room by a psychiatric medical doctor or clinician using a MINI 7.0.2 for DSM-5 (See the flow of participants in Figure 1). The MINI 7.0.2 was considered the gold standard. Total scores of the EPDS were calculated and scored by the first author at the end of each data collection day as a quality control. The clinicians conducting the MINI 7.0.2 diagnostic evaluations were blinded to the initial screening results of the EPDS. Recruitment of study participants was carried out until the sample size was achieved. All participants were subjected to the EPDS and a clinical evaluation using the MINI 7.0.2.
 |
Figure 1 Flow chart of the participants. |
Data Management
The EPDS data set was reviewed against the MINI 7.0.2 data set. To determine psychometric properties of the EPDS, data set of the EPDS was retrieved, reviewed, analyzed and compared against the data set obtained using the MINI 7.0.2. Among the cases with PPD, the true positives (positive on both scales) and false negatives (positive on the MINI 7.0.2 and negative on the EPDS) were identified. This process was also repeated for the controls without PPD where the true negatives and false positives were identified.
The sensitivity was calculated by dividing the number of participants who are true positive against the total number of cases identified using the MINI 7.0.2 and multiplied by 100%. For the specificity of the EPDS, the participants who tested negative on both scales were divided by the total number of controls as identified by the MINI 7.0.2 and multiplied by 100%.
The non-parametric Youden index ROC analysis method was used to generate the sensitivity, specificity and the predictive values for each cutoff point based on the EPDS score. It defines the optimal cutoff point which is the difference between true positive rate and false positive rate over all possible cutoff point values.
Statistical Analysis
Data from the EPDS and structured clinical interview were analyzed regarding their sensitivity, specificity, positive predictive (PPV) and negative predictive values (NPV) using the software package EPI-INFO software version 7.2. Confidence intervals were computed by embedding the calculations in a logistic regression. To estimate the ability of the EPDS to discriminate a group of women with postpartum depression from the group without postpartum depression, the average scores of both groups were calculated and compared. The sensitivity, specificity, positive predictive value and negative predictive value of the translated version of EPDS were obtained to determine the psychometric properties of EPDS.
Results
Socio-Demographic Characteristics of the Study Population
The sample comprised 287 postpartum women who were enrolled into the study between November 2019 and June 2020, with 149 enrolled from Mbarara Regional Referral Hospital, 92 from Bwizibwera Health Centre-IV and 46 from Kinoni Health Centre-IV. Of 287 women, the group with the largest proportion were between 25 and 34 years (45.6%), were married (95.5%), identified as Banyankore by tribe (76.7%), had attained at least secondary school education (36.9%), were residing in urban areas (66.2%), were protestants by religion (49.8%), business women (39.7%) and were dwelling in permanent houses (79.1%) See Table 1.
 |
Table 1 Socio-Demographic Characteristics of the Participants |
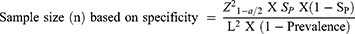
EPDS Cutoff Point
Cutoff points are used to assess the threshold above which the tests are most accurate to identify the presence of PPD in a given setting. For this, the corresponding measures of determining the validity indices of different cutoffs of the EPDS for screening for PPD were computed against the clinical diagnosis as guided by the MINI 7.0.2 according to the DSM-5. The levels of sensitivity (proportion of mothers suffering from PPD according to MINI 7.0.2 that were correctly identified by EPDS), specificity (proportion of mothers not suffering from PPD correctly identified as such by EPDS), positive predictive value (proportion of true positives among all positives identified by EPDS) and negative predictive value (proportion of true negatives among all negative identification by EPDS) were computed. The best cutoff point of the EPDS was found at 10 (Table 2).
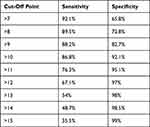 |
Table 2 EPDS Cutoffs Point |
The Level of Accuracy of the EPDS Compared to the MINI 7.0.2 in Determining the Prevalence of PPD Among Women in South Western Uganda
Following the validation results, the EPDS was used to determine the overall postpartum depression prevalence at a cutoff point of ≥10 and this test yielded 29.5% based on the EPDS as compared to 26.5% with the MINI 7.0.2. The overall PPD prevalence of the two tests was not statistically significant (p = 0.239). This resulted in 66 women as levels of true positives/TP and 16 as levels of false positives/FP (Table 3). The level of accuracy of the EPDS versus the MINI 7.0.2 is 90.6%.
 |
Table 3 Comparing the Level of Accuracy of the EPDS Against the MINI 7.0.2 |
= ((TN + TP)/Total) * 100
= ((186+66)/278) * 100.
This high level of concordance between the diagnostic MINI 7.0.2 and the EPDS implies that there is no statistical difference between the two tests in detecting PPD among women in the Ugandan context.
Psychometric Properties of the EPDS at ≥10 Cut Off Point in Screening for PPD
The psychometric properties of the EPDS using a cutoff point of ≥10 were calculated with the actual PPD status of the participants according to the MINI 7.0.2. The test characteristics overall revealed a sensitivity of 86.8% and specificity of 92.1%. The likelihood ratio (LR) for PPD when the test is positive (LR+ve) is 10.96, and the LR of a negative test (LR−ve) is 0.14. There is a strong positive relationship between EPDS and the MINI 7.0.2 illustrated by an odds ratio of 76.72. The positive predictive value (PPV) and negative predictive value (NPV) were both calculated, resulting in 80.5% and 94.9%, respectively, as described below:
The psychometric properties were also stratified by health facility and age category in order to establish any variations between the study sites; no statistically significant variations were noted, see Table 4.
 |
Table 4 Psychometric Properties of the EPDS at ≥10 Cut Off Point in Screening for PPD |
Area Under the Receiver Operating Characteristic (ROC) for EPDS versus the MINI 7.0.2 in Screening for PPD Across Different Health Facilities
The nonparametric analysis of the Receiver Operating Characteristic (ROC) yielded an area under the curve of 0.89 for Bwizibwera HCIV, 0.97 for Kinoni HCIV and 0.84 for MRRH (overall 95% confidence interval 0.85–0.93). This indicates that the test can significantly and accurately distinguish between postpartum mothers who are truly depressed and those mothers who are not depressed at the cutoff point of ≥10.
Discussion
The EPDS is a simple, valid and effective screening scale for detection of postpartum depression among postpartum mothers in an urban and peri-urban primary care setting serving the rural community with high postpartum depression prevalence. We found an overall PPD prevalence of 29.5% using the Edinburgh Postnatal Depression scale (EPDS) at a cutoff point of ≥10 and this was comparable with a prevalence of 26.5% as determined by the MINI 7.0.2. The PPD prevalence rate falls within the same range with recent studies in other African countries such as South Africa (31.7%),25 Zimbabwe (33%),11 and Nigeria (22.9%).26 Some studies in Africa have reported a much lower prevalence rate of 12% in Tanzania,27 9.2% in Sudan22 and 13% in Kenya.28 Although all these studies used EPDS scale, it is difficult to compare results of the current study with the above studies because of the variations in the PPD prevalence potentially due to the different categories of postpartum women, sample sizes used, cutoff points, reference scales and timeframe of assessment with regard to their risk of PPD. Having excluded women with the most important risk factors for postpartum depression from this research, could also reach prevalence values higher than 26.5% as determined by the MINI 7.0.2. These results therefore imply that if the general Ugandan population of postpartum women is subjected to the EPDS, more numbers may be found to be suffering from PPD.
A cut-off point for a local setting like Uganda is essential for accurate detection and PPD burden estimation. As such, the present study confirmed that a cutoff point of ≥10 as the suitable cutoff point for the EPDS. These findings are also in the same range with cutoff points reported by other validation studies in African countries such as Ghana ≥10,29 Zimbabwe ≥10.11 However, the cutoff point established by this study was higher than related studies carried out in Nigeria ≥8),30 and Ethiopia ≥5.31 The variation between the present study and other validation studies in Africa is attributed to diversity in economic circumstances, socio-cultural norms and the heterogeneous nature of study populations. It is particularly important to choose accurate psychometric property findings in a low-income setting as they may not place a burden on the health service through an overly high false-positive rate.
The sensitivity, specificity, positive predictive value and negative predictive value of the EPDS were established by this study to be 86.8%, 92.1%, 80.5% and 94.9%, respectively. The sensitivity between 80% and 90% is considered to have good diagnostic performance, meaning that the EPDS can correctly identify women who are suffering from postpartum depression, hence in this population the EPDS provides good sensitivity. Similarly, specificity of 92.1% is also considered quite good to correctly identify women who do not have postpartum depression. In addition, the study stratified mothers according to the health facility and age category to compare the psychometric properties of the EPDS across variables and to also ensure generalizability of the findings. The level of accuracy of this scale is comparable and within this sample no statistically significant variations occurred even when stratified. Therefore, the EPDS is identified as a valid scale in measuring postpartum depression in the Ugandan context in this study sample. These study findings are consistent with data from other validation studies in low resource settings where EPDS has been validated in local languages in similar demographically representative settings. For example, systematic reviews reported strong reliability and validity of EPDS for detecting perinatal common disorders among women in low and lower-middle income countries.11,12,22 The high sensitivity test reveals that the index scale can establish that there are few false-negative results, and thus fewer cases of disease are missed. This also applies to the high specificity revealed as this is important for ruling in disease or mothers with PPD.32 In low-resource settings like Uganda, the strength of the EPDS lies in its high NPV, meaning that with negative results there is high level of confidence that women are free from PPD. The acceptable sensitivity and specificity findings will help in the identification of Ugandan postpartum women at risk of depression.
In the current research, a nonparametric analysis of the ROC was conducted, resulting in an area under the curve of 0.89 for Bwizibwera HCIV, 0.97 for Kinoni HCIV, and 0.84 for MRRH, implying that the EPDS can effectively distinguish between postpartum mothers who are truly depressed and those women who are not depressed at the cutoff point of ≥10.
Strengths and Limitations
The strength of our study is that it was conducted in an urban and peri-urban setting that serves the rural population. Although some studies had utilized this scale in screening for PPD without validation to the Ugandan population,33 this is the first study that translated and established the accuracy of the EPDS in screening mothers with PPD in Uganda. In addition, validating the EPDS will improve consistency between the tools by clearly defining the cutoff point. Consistency in defining these cutoff points across different tools ensures that similar criteria are used for screening, improving overall consistency. An important limitation of this study was not including women receiving postpartum services from the private clinics and the general population of postpartum women; therefore, it may not be generalized to this population as it is likely to be higher than the current findings. In addition, this study only focused on the current episode of major depression without assessing for the past episodes of depression as the EPDS only considers the current depression. Not including past episodes of depression does not inform us whether the mothers had depression before the postpartum period but this limitation could be overcome in future studies. In addition, by recruiting women attending health facilities, we may have missed women who do not utilize these services. They could be more prone to PPD. Women who do not attend postpartum services in a health facility setting are more likely to have postpartum check-ups with midwives in their neighborhoods. Village midwives could be a great asset in locating these types of women in future studies. The authors also used a wide precision gap of 0.09 which is the upper limit in order to target a smaller recruitment given the unpredictable timing of the covid-19 pandemic during data collection.
Implications and Recommendations
Screening for postpartum depression should be integrated into routine postpartum care in areas with high PPD prevalence. By routinely using the EPDS to screen mothers with PPD, the awareness of health care providers can improve early detection of postpartum depression. In turn, this can lead to positive health outcomes for both mothers, babies and their families, which is an important goal of health care provision and promotion. In addition, incorporating PPD screening in the nursing-midwifery education curricular may be impactful.
This scale may also be validated in postpartum women living with HIV and antepartum mothers suffering from antepartum depression as this may increase the chances of identifying PPD at an early phase. Midwives, nurses, traditional birth attendants, family health practitioners and other primary health care workers can easily apply this screening scale and be encouraged to refer women suspected to have PPD to health facilities for further evaluation. This will ensure that most cases of PPD do not go undetected and untreated.
There is an urgent need for a better understanding of a feasibility study and acceptability study or survey of routine screening of postpartum women utilizing the validated EPDS in south western Uganda to provide appropriate support most especially during this pandemic period when depression is at a high rise.
Conclusion
From our study findings, overall, it can be concluded that the EPDS is a satisfactory instrument for screening for PPD and can be successfully used to screen postpartum depression at a cutoff score of ≥10 among southwestern Ugandan women attending routine postpartum check-up. This cutoff point will help health workers to classify mothers with and without PPD. Future researchers may contribute to the ongoing refinement and application of the EPDS by obtaining cutoff points that are accurate, relevant, and adaptable to larger sample sizes, diverse communities and changing clinical and demographic contexts. They can also conduct longitudinal studies to assess how the EPDS performs over time and compares with other screening tools.
Abbreviations
AUC, Area under the curve; BHC-IV, Bwizibwera Health Centre IV; DSM-5, Diagnostic and Statistical Manual of Mental Disorders; 5th Edition; EPDS, Edinburgh Postnatal Depression Scale; HIV, Human Immunodeficiency Virus; KHC-IV, Kinoni Health Centre IV; MRRH, Mbarara Regional Referral Hospital; NPV, Negative Predictive Value; PPV, Positive Predictive Value; PPD, Postpartum Depression; ROC, Receiver Operating Characteristics; SN, Sensitivity; SP, Specificity.
Data Sharing Statement
The data that support the findings of this study are available from the first and corresponding author, Catherine Atuhaire but restrictions apply under license for the current study.
Ethical Approval and Consent Statement
Ethical approval was obtained from the Mbarara University of Science and Technology Institutional Ethics Review Committee and the Uganda National Council for Science and Technology, Kampala, Uganda. After obtaining ethical approval, permission was obtained from the hospital Director, Mbarara Regional Referral Hospital and the District Health Officers of the community health centres. The study was conducted in accordance with the Declaration of Helsinki. Written informed consent for data collection and publication of the study findings was obtained from all the participants before they were enrolled into the study.
Acknowledgments
We are grateful to all mothers who participated in this research and to ADB-HEST for the support towards implementation of this study. In addition, we acknowledge HBNU for funding the statistical analysis of these data through National Institute of Mental Health (NIMH).
Author Contributions
All authors made a significant contribution to the work reported, that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
This study received funding from African Development Bank.
Disclosure
The authors declare no competing interest in this work.
References
1. Letourneau NL, Dennis C-L, Benzies K, et al. Postpartum depression is a family affair: addressing the impact on mothers, fathers, and children. Issues Ment Health Nurs. 2012;33(7):445–457. doi:10.3109/01612840.2012.673054
2. Cox JL, Chapman G, Murray D, Jones P. Validation of the Edinburgh Postnatal Depression Scale (EPDS) in non-postnatal women. J Affect Disord. 1996;39(3):185–189. doi:10.1016/0165-0327(96)00008-0
3. Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: development of the 10-item Edinburgh Postnatal Depression Scale. Br J Psychiatry. 1987;150(6):782–786. doi:10.1192/bjp.150.6.782
4. Hewitt C, Gilbody S, Brealey S, et al. Methods to identify postnatal depression in primary care: an integrated evidence synthesis and value of information analysis. Health Technol Assess. 2009;13(36). doi:10.3310/hta13360
5. Cox J. Thirty years with the Edinburgh Postnatal Depression Scale: voices from the past and recommendations for the future. Br J Psychiatry. 2019;214(3):127–129. doi:10.1192/bjp.2018.245
6. Cox J, Holden J, Henshaw C. Perinatal Mental Health: The Edinburgh Postnatal Depression Scale (EPDS) Manual.
7. Beck CT, Gable RK. Further validation of the postpartum depression screening scale. Nur Res. 2001;50(3):155–164. doi:10.1097/00006199-200105000-00005
8. Buist A, Condon J, Brooks J, et al. Acceptability of routine screening for perinatal depression. J Affect Disord. 2006;93(1–3):233–237. doi:10.1016/j.jad.2006.02.019
9. Gibson J, McKenzie‐McHarg K, Shakespeare J, Price J, Gray R. A systematic review of studies validating the Edinburgh Postnatal Depression Scale in antepartum and postpartum women. Acta Psychiatr Scand. 2009;119(5):350–364. doi:10.1111/j.1600-0447.2009.01363.x
10. Khalifa DS, Glavin K, Bjertness E, Lien L. Determinants of postnatal depression in Sudanese women at 3 months postpartum: a cross-sectional study. BMJ Open. 2016;6(3):e009443. doi:10.1136/bmjopen-2015-009443
11. Chibanda D, Mangezi W, Tshimanga M, et al. Validation of the Edinburgh Postnatal Depression Scale among women in a high HIV prevalence area in urban Zimbabwe. Arch Womens Mental Health. 2010;13(3):201–206. doi:10.1007/s00737-009-0073-6
12. Shrestha SD, Pradhan R, Tran TD, Gualano RC, Fisher JR. Reliability and validity of the Edinburgh Postnatal Depression Scale (EPDS) for detecting perinatal common mental disorders (PCMDs) among women in low-and lower-middle-income countries: a systematic review. BMC Pregnancy Childbirth. 2016;16(1):1–19. doi:10.1186/s12884-016-0859-2
13. Atuhaire C, Brennaman L, Cumber SN, Rukundo GZ, Nambozi G. The magnitude of postpartum depression among mothers in Africa: a literature review. Pan Afr Med J. 2020;37.
14. Atuhaire C, Rukundo GZ, Nambozi G, et al. Prevalence of postpartum depression and associated factors among women in Mbarara and Rwampara districts of south-western Uganda. BMC Pregnancy Childbirth. 2021;21(1). doi:10.1186/s12884-021-03967-3
15. Chorwe-Sungani G, Chipps J. A systematic review of screening instruments for depression for use in antenatal services in low resource settings. BMC Psychiatry. 2017;17(1):1–10. doi:10.1186/s12888-017-1273-7
16. e Couto TC, Brancaglion MYM, Alvim-Soares A, et al. Postpartum depression: a systematic review of the genetics involved. World J Psychiatry. 2015;5(1):103. doi:10.5498/wjp.v5.i1.103
17. Benvenuti P, Ferrara M, Niccolai C, Valoriani V, Cox JL. The Edinburgh postnatal depression scale: validation for an Italian sample. J Affect Disord. 1999;53(2):137–141. doi:10.1016/S0165-0327(98)00102-5
18. Rahman A, Iqbal Z, Harrington R. Life events, social support and depression in childbirth: perspectives from a rural community in the developing world. Psychol Med. 2003;33(7):1161. doi:10.1017/S0033291703008286
19. Cox J. Use and misuse of the Edinburgh Postnatal Depression Scale (EPDS): a ten point ‘survival analysis’. Springer; 2017.
20. Kozinszky Z, Dudas RB. Validation studies of the Edinburgh Postnatal Depression Scale for the antenatal period. J Affect Disord. 2015;176:95–105. doi:10.1016/j.jad.2015.01.044
21. Buderer NMF. Statistical methodology: i. Incorporating the prevalence of disease into the sample size calculation for sensitivity and specificity. Acad Emerg Med. 1996;3(9):895–900. doi:10.1111/j.1553-2712.1996.tb03538.x
22. Khalifa DS, Glavin K, Bjertness E, Lien L. Postnatal depression among Sudanese women: prevalence and validation of the Edinburgh Postnatal Depression Scale at 3 months postpartum. Int J Women’s Health. 2015;7:677. doi:10.2147/IJWH.S81401
23. Tesfaye M, Hanlon C, Wondimagegn D, Alem A. Detecting postnatal common mental disorders in Addis Ababa, Ethiopia: validation of the Edinburgh postnatal depression scale and Kessler scales. J Affect Disord. 2010;122(1–2):102–108. doi:10.1016/j.jad.2009.06.020
24. First M, Williams J, Karg R, Spitzer R. Structured clinical interview for DSM-5—Research version (SCID-5 for DSM-5, research version; SCID-5-RV). Arlington, VA: American Psychiatric Association; 2015:1–94.
25. Hung KJ, Tomlinson M, le Roux IM, et al. Community-based prenatal screening for postpartum depression in a South African township. Int J Gynaecol Obstet. 2014;126(1):74–77. doi:10.1016/j.ijgo.2014.01.011
26. Chinawa JM, Odetunde OI, Ndu IK, et al. Postpartum depression among mothers as seen in hospitals in Enugu, South-East Nigeria: an undocumented issue. Pan Afr Med J. 2016;23(1). doi:10.11604/pamj.2016.23.180.8244
27. Rogathi JJ, Manongi R, Mushi D, et al. Postpartum depression among women who have experienced intimate partner violence: a prospective cohort study at Moshi, Tanzania. J Affect Disord. 2017;218:238–245. doi:10.1016/j.jad.2017.04.063
28. Madeghe BA, Kimani VN, Vander Stoep A, Nicodimos S, Kumar M. Postpartum depression and infant feeding practices in a low income urban settlement in Nairobi-Kenya. BMC Res Notes. 2016;9(1):506. doi:10.1186/s13104-016-2307-9
29. Weobong B, Akpalu B, Doku V, et al. The comparative validity of screening scales for postnatal common mental disorder in Kintampo, Ghana. J Affect Disord. 2009;113(1–2):109–117. doi:10.1016/j.jad.2008.05.009
30. Uwakwe R. Affective (depressive) morbidity in puerperal Nigerian women: validation of the Edinburgh Postnatal Depression Scale. Acta Psychiatr Scand. 2003;107(4):251–259. doi:10.1034/j.1600-0447.2003.02477.x
31. Hanlon C, Medhin G, Alem A, et al. Detecting perinatal common mental disorders in Ethiopia: validation of the self-reporting questionnaire and Edinburgh Postnatal Depression Scale. J Affect Disord. 2008;108(3):251–262. doi:10.1016/j.jad.2007.10.023
32. Levis B, Negeri Z, Sun Y, Benedetti A, Thombs BD. Accuracy of the Edinburgh Postnatal Depression Scale (EPDS) for screening to detect major depression among pregnant and postpartum women: systematic review and meta-analysis of individual participant data. BMJ. 2020;371.
33. Kakyo TA, Muliira JK, Mbalinda SN, Kizza IB, Muliira RS. Factors associated with depressive symptoms among postpartum mothers in a rural district in Uganda. Midwifery. 2012;28(3):374–379. doi:10.1016/j.midw.2011.05.001
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.