Back to Journals » Clinical Epidemiology » Volume 15
Use of Linked Nordic Registries for Population Studies in Hematologic Cancers: The Case of Multiple Myeloma
Authors Abildgaard N, Freilich J, Anttila P, Bent-Ennakhil N, Ma Y, Lassenius M, Ørstavik S, Toppila I, Waage A, Turesson I, Hansson M
Received 4 May 2023
Accepted for publication 29 August 2023
Published 18 September 2023 Volume 2023:15 Pages 987—999
DOI https://doi.org/10.2147/CLEP.S413587
Checked for plagiarism Yes
Review by Single anonymous peer review
Peer reviewer comments 2
Editor who approved publication: Professor Henrik Sørensen
Niels Abildgaard,1,2 Jonatan Freilich,3,4 Pekka Anttila,5 Nawal Bent-Ennakhil,6 Yuanjun Ma,3 Mariann Lassenius,7 Sigurd Ørstavik,8 Iiro Toppila,7 Anders Waage,9 Ingemar Turesson,10 Markus Hansson11
1Hematology Research Unit, Department of Hematology, Odense University Hospital, Odense, Denmark; 2Department of Clinical Research, University of Southern Denmark, Odense, Denmark; 3Department of Access Consulting, PAREXEL International, Stockholm, Sweden; 4Department of Public Health and Clinical Medicine, Dermatology, Umeå University, Umeå, Sweden; 5Comprehensive Cancer Center, Department of Hematology, University of Helsinki, and Helsinki University Hospital, Helsinki, Finland; 6Takeda Pharmaceuticals International AG, Zurich, Switzerland; 7Medaffcon, Espoo, Finland; 8Takeda Pharmaceuticals International AG, Oslo, Norway; 9Department of Hematology, St Olav’s University Hospital, Trondheim, Norway; 10Lund University Cancer Centre, University of Lund, Skåne University Hospital, Lund, Sweden; 11Sahlgrenska Academy and Sahlgrenska University Hospital, Göteborg, Sweden
Correspondence: Niels Abildgaard, Department of Hematology, Odense University Hospital, Kloevervaenget 10, Floor 12, 5000 Odense C, Denmark, Tel +45 6541 1155, Email [email protected]
Purpose: Linked health-care registries and high coverage in Nordic countries lend themselves well to epidemiologic research. Given its relatively high incidence in Western Europe, complexity in diagnosis, and challenges in registration, multiple myeloma (MM) was selected to compare registries in Denmark, Finland, and Sweden.
Patients and Methods: Data were obtained from four archetypal registries in each country (spanning January 2005–October 2018): National Patient Registry (NPR), Prescribed Drug Registry (PDR), Cancer Registry (CR), and Cause of Death Registry. Patients newly diagnosed with MM who received MM-specific treatment were included. PDR/NPR treatment records were used to assess incident NPR cases. The registration quality of MM-specific drugs in the PDR of each country was also evaluated.
Results: In Denmark, only 6% of patients in the NPR were not registered in the CR; in Sweden, it was 16.9%. No systematic differences were identified that could explain this discrepancy. In Denmark, lenalidomide and bortezomib were registered in the NPR with high coverage, but less expensive drugs typically given in combination with bortezomib were not covered in any of the registries. In Finland and Sweden, bortezomib records were not identified in the PDR, but some were in the NPR; other drugs had good coverage in the PDR.
Conclusions: The registries evaluated in this study can be used to identify the MM population; however, given the gaps in MM registration in the Finnish and Swedish CRs, Danish registries provide the most comprehensive datasets for research on treatment patterns for MM.
Plain Language Summary: National patient registries collect observational data on populations of patients and are often used for research. In this study, we investigated how complete the national patient registries were for Denmark, Finland and Sweden when recording the number of patients with multiple myeloma (MM; a type of bone marrow cancer) between 2005 and 2018. We also investigated the completeness in registration of given treatments during the study period in the national registries. Overall, the Danish national patient registries had the most comprehensive information on patients with MM. Registry data from Denmark could therefore be useful for conducting further research into the characteristics, treatment patterns, and outcomes of patients with MM.
Keywords: incidence, prevalence, real-world evidence
Introduction
National registries are important sources of clinical information1,2 that can help to estimate incidence, prevalence, and patient survival for a disease, identify and quantify risk factors, and evaluate treatment patterns and outcomes.1–4 Nordic countries have a long history of collecting registry data covering births, deaths, diseases, migration, and various social issues for administrative purposes.5–7 Denmark, Finland, Iceland, Norway, and Sweden all have registries covering almost their entire population, and these have been reviewed previously.8,9
The key to unlocking the use of large administrative databases for research purposes is the availability of unique personal identifiers, which allows linkage of registries.2,5,9–11 It is possible, therefore, to retrieve linked data for each individual, ranging from sociodemographic characteristics, medical diagnoses, and surgical procedures, to dispensing of prescriptions.8,12,13
Registry coverage of hematologic cancers is challenging. Notably, in the absence of a solid tissue diagnosis, registration of a hematologic cancer requires data on blood, bone marrow, flow cytometry, molecular and cytogenetic tests from various laboratories, in addition to histopathology and clinical records.13 In a study conducted in Finland, over 50% of hematologic cases identified in the National Patient Registry (NPR) were not included in the Cancer Registry (CR).14 In multiple myeloma (MM), a B-cell malignancy that accounts for 15–20% of all hematologic cancers,15 diagnosis is further complicated by the need for biochemical data and imaging findings.16,17
The objective of this report is to provide an overview of the different Nordic registries, and their suitability for research on MM in terms of patient identification, estimation of disease incidence/prevalence, and ascertainment of drug regimens. The study was part of the Health outcomes and Understanding of Myeloma: A multi-National (HUMAN) study, which was conducted to gain further insight into the treatment patterns and outcomes of patients with newly diagnosed MM (NDMM) in Nordic countries. Full results of the HUMAN study, including real-world treatment outcomes and healthcare resource use, will be presented in a separate article.
Materials and Methods
The HUMAN study was observational, using secondary data from a variety of national health registers. Patient consent was not required for this was registry-based study. Use of data was approved by the data holders of each registry, the ethics committee in Sweden (DNR 2017/2355-31), the Danish Data inspection board (Syddanmark 2012-58-0018), and the Finnish Institute for Health and Welfare (THL/415/5.05.00/2018). Requests for access to data in Norway were also submitted; however, approval was not granted in time for analysis and inclusion in the study. All data accessed complied with relevant data protection and privacy regulations.
Patient Identification
Data were obtained from three national health-care registries in each country, from January 1, 2005, to October 31, 2018 (Figure 1). To identify the MM population diagnosed in 2010 or later (International Classification of Diseases 10th Revision [ICD-10] code C90.0), a 5-year period from 2005 to 2009 was included as wash-out period to ensure that patients registered in 2010 were not diagnosed before 2010. In Denmark, first MM diagnoses up to 2016 were identified in the NPR and in the CR. In Finland and Sweden, only the NPR was used for patient identification; in Finland, first MM diagnoses up to 2016 were identified; in Sweden, it was up to 2017 (CR was checked if the diagnosis date was missing from the NPR).
In addition, patients in the NPR who had been prescribed MM-specific treatment in the Prescribed Drug Registry (PDR), and had a diagnosis registered in the Cause of Death Registry (CDR) in Denmark and Sweden (from 2010 to 2018), and in Finland (from 2010 to 2016) were also included. MM-specific treatment could be autologous stem cell transplantation (ASCT), prescription drugs identified in the PDR, or hospital-administrated drugs in the NPR. These drugs included bortezomib (Anatomical Therapeutic Chemical [ATC] code L01XX32), carfilzomib (L01XX45), daratumumab (L01XC24), elotuzumab (L01XC23), ixazomib (L01XC23), melphalan (L01AA03), panobinostat (L01XX42), lenalidomide (L04AX04), thalidomide (L04AX02), and pomalidomide (L04AX06).
To create a more homogenous analytical dataset, and to prevent potentially confounding outcomes, patients diagnosed with any other type of cancer were excluded.
Registries Evaluated in the Study
The characteristics of the four registry archetypes (NPR, CR, CDR, and PDR) are summarized in Tables 1–3. An additional subanalysis was performed of patient records from three hospitals in Southern Sweden to validate the findings of the exploratory analysis regarding the inclusion and exclusion criteria for the Swedish CR.
 |
Table 1 Comparison of the National Patient Registries for Denmark, Finland, and Sweden |
 |
Table 2 Comparison of the Prescription Drug Registries for Denmark, Finland, and Sweden |
 |
Table 3 Comparison of the Cancer Registries for Denmark, Finland, and Sweden |
Determining Population Size
To assess the true population of patients with MM in each respective country, different criteria were used to assess range (ie, upper and lower boundary of the population estimation), as well as assessing whether CRs should be used for ascertaining diagnosis of MM. Since all patients should receive MM-specific treatment, prescriptions were also used to further identify patients with a diagnosis of MM. In the most conservative estimate, patients were required to have an MM diagnosis in NPR and CR, and a record of MM-specific treatment in the PDR. At the very minimum, to be considered as having MM, patients were required to have at least an NPR diagnosis and a record of MM-specific treatment.
Prevalence of MM was then estimated as the cumulative number of patients with MM identified as per criteria in each respective country during a 12-month calendar year, divided by the average population size (identified from available national population statistics data from the respective countries) during that calendar year. Prevalence was calculated for each calendar year during the study follow-up. Incidence of MM was estimated by recording only patients with NDMM in the year of first diagnosis registration at the start of each calendar year (average population size and subtracting prevalent patients). Incidence and prevalence were reported per 100,000 individuals. A best estimate of incidence and prevalence is also provided, which was calculated by adding the number of treated and untreated patients in both the NPR and CR (NPR+/CR+) to the number of treated patients in the NPR who are not found in the CR (NPR+/CR–).
Statistical Analysis
Continuous variables were summarized using descriptive statistics, and categorical variables were presented as frequencies and percentages (%) by category. Analyses were performed using SAS® 9.3 or higher (SAS Institute, Cary, NC, USA), Stata v11 or higher (StataCorp, College Station, TX, USA) and R v3.1.0 (R Core Team, R Foundation for Statistical Computing, Vienna, Austria), or higher.
Results
The MM population for each country is presented in Figure 2.
Evaluation of Cancer Registries
Treated patients registered in the NPR, but not in the CR (NPR+/CR−), were compared with treated patients registered in both (NPR+/CR+) to assess any systematic reasons for lack of CR registration. A small proportion of patients (<1%) who were recorded in the CR were not found in the NPR (NPR–/CR+); no further analyses were conducted on patients who fell into this category.
In Denmark, 3680 patients met inclusion criteria for NPR+/CR+, and 233 for NPR+/CR−; therefore, only 6% of patients in the NPR were not registered in the CR. There was no difference between NPR+/CR+ and NPR+/CR− patients in terms of whether the diagnosis was established at a hematology or other clinic (96% and 95% of patients, respectively, were diagnosed in a hematology clinic). Given the small proportion of NPR+/CR− patients, no further analyses were conducted.
In Sweden, 3254 patients formed the MM cohort; 16.9% of those registered in the NPR were not registered in the CR (Figure 3). Various analyses revealed no systematic difference that could explain the discrepancy between patients registered in the CR (NPR+/CR+) and those who were not (NPR+/CR−). In terms of treatment, the proportion of patients receiving ASCT after the first MM diagnosis was similar in both groups: 22% in the NPR+/CR+ group; 19% in the NPR+/CR− group. There were no differences between the two patient groups in terms of the clinical departments where they were treated (eg, hematology, oncology, or internal medicine clinic; data not shown), or where they were diagnosed (eg, in the in- or outpatient setting) (Table 4). Further analyses, to determine whether CR− patients received drugs indicative of not having MM, revealed no differences in the drugs used to treat the two patient groups (Table 4).
In Finland, 3759 patients were NPR+/CR+, whereas 2820 were NPR+/CR– (Figure 3). It can therefore be assumed that only 57% of patients with MM are represented in the Finnish NPR and CR. Underrepresentation of hematologic cancers in the Finnish CR has been described previously.14 Based on this, a decision was made to cease any further analyses on the registration quality of MM in the Finnish CR.
Validation of the MM Population in the Swedish CR
A subanalysis was carried out to validate the findings of the HUMANS study with regard to the MM patients included in the Swedish CR. To do this, patient records from three hospitals in Skåne, Sweden (Kristianstad sjukhus, Helsingborgs lasarett, and Skånes universitetssjukhus Lund) were analyzed. Of 317 individuals who had a registered C90.0 ICD-10 code in the NPR and a record of MM-specific treatment from these hospitals, 257 patients (81%) had a registered diagnosis in the Swedish CR (NPR+CR+) while 60 (19%) were not reported to the CR (NPR+CR–). Medical records were available for 55/60 CR– patients and analyzed by a clinical investigator, who extracted detailed information about patients’ clinical characteristics, treatment, and outcomes from electronic medical records (EMR) (Supplementary Data Box 1).
The EMR review determined that 38/55 patients (69%) with a diagnosis of MM were not reported to the Swedish CR while the remaining 17/55 (31%) did not have MM, despite having been assigned a C90.0 ICD-10 code and prescribed medications used in MM. Thus, the rate of reporting to the CR for these three hospitals during this period was 87% (257/295).
Registration of MM Drugs in PDR
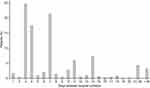
In Denmark, hospital-administered drugs such as bortezomib are not prescribed through the pharmacy and are therefore not captured in the e-pharmacy IT system. Instead, these drugs must be registered manually in the NPR as part of the patient visit to the clinic. Thus, bortezomib use was determined by the length in days between bortezomib registrations from the NPR (Figure 4). However, it is unknown whether bortezomib was registered with a similar frequency across all sites.
Less expensive drugs that are typically given in combination with bortezomib (ie, thalidomide and melphalan) were not well registered (Table 5). Only 39% of patients on bortezomib had registered combination treatment (defined as registration within 30 days of first bortezomib registration). Lenalidomide was also found to be well registered with prescriptions 30 days apart.
 |
Table 5 Registration of Drugs Commonly Prescribed with Bortezomib in Denmark |
In Finland, medication data are not usually included in the NPR (HILMO National Care Registry for Health Care Institutions [HILMO]) based on the ATC code (Table 6); however, it was revealed that hematologists used the medical procedure code to register bortezomib based on the last letters of the ATC code (1XX32) in a subset of the population. Although the PDR contains information on drugs for MM that are purchased on a national level from pharmacies (ie, melphalan, thalidomide, and lenalidomide), it does not include bortezomib, which is prescribed and administered within hospitals.
 |
Table 6 MM-Specific Drug Registrations in Finnish Registries |
Results of the analysis in Sweden showed that melphalan, thalidomide, and lenalidomide registrations were available in the PDR. As expected, bortezomib had poor representation. While the NPR had very few bortezomib registrations, the numbers remained insufficient for studying persistence of bortezomib or bortezomib, melphalan, and prednisone combination therapy. In Sweden, as in Finland, bortezomib therefore was studied by weekly or twice-weekly visits as proxies. In this time period bortezomib was the only drug given with this frequency.
Incidence and Prevalence of MM
In Denmark, MM incidence and prevalence calculations were based on the number of treated or untreated patients registered in the NPR and CR (NPR+/CR+) given that the CR was considered to have high coverage of the population. In Sweden and Finland, as the CR was considered to have full coverage, the population size was calculated based on the number of patients registered in the NPR and CR (treated or untreated) plus the number of treated patients in the NPR not found in the CR; ie, NPR+/CR+ (treated and untreated) and NPR+/CR− (treated) (Table 7 and Table 8). As bortezomib is underreported in these two countries, the NPR+/CR− (treated) group would be dominated by patients treated with other drugs. A summary of the incidence and prevalence of NDMM in the three countries, based on calculation of best estimate, is presented in Table 9.
 |
Table 9 Best Estimate of Incidence and Prevalence of NDMM in Denmark, Finland, and Sweden from 2010 to 2016 per 100,000 Individuals |
In Denmark, an increase was observed in both the incidence and prevalence of MM from 2010 to 2016. In Finland, the prevalence of MM increased steadily, while the incidence showed a downward trend, from a high of 7.9/100,000 in 2010, to a low of 6.2/100,000 in 2015, and subsequently 6.4/100,000 in 2016. In Sweden, a steady increase in the prevalence of MM was also observed, while the incidence remained relatively stable (ranging from 7.2 to 7.8/100,000).
Discussion
The results of this study indicate that, for research on MM, Danish registries provide the most comprehensive data, especially in terms of treatment patterns, and highlight the limitations of the Swedish and Finnish CRs in the registration of MM, and more broadly, hematologic cancers.
The Danish CR was found to have good coverage of MM, due to better integration of the CR with the EMR system; therefore, the CR was used to identify the patient population. In Denmark, the CR is automatically connected to the NPR, which means that physicians must register whether a diagnosis is confirmed and reported to the CR when the first NPR ICD-10 code registration of a cancer diagnosis is generated. Coverage of MM in the Swedish CR was not as complete as in the Danish CR, and 16.9% of patients with NDMM in Sweden who were identified in the NPR were not registered in the CR. Our further analyses revealed that in that the CR had 87% coverage for the three Skåne sites; however, if using MM registration in NPR and MM prescribed drug in PDR could overestimate the population with 5%. Thus, depending on the research question, epidemiology studies should consider whether to use CR+ for MM case inclusion.
In Finland, completeness of registration for nonsolid tumors has been shown to be lower than that of all solid tumors (86% versus 96%), with underreporting most prominent for tumors that are not typically histologically verified, such as hematologic malignancies and nonmalignant central nervous system tumors.28 While the CR in Finland provides overall accurate and close to complete national cancer data for solid malignant tumors, registration of tumors with no histology is still compromised.28 Given this known limitation, inclusion in the Finnish CR was not used in this study other than for estimating incidence/prevalence. In a personal communication, the head of the Finnish CR noted that “Shortcomings have been noted in the cancer registry regarding the coverage of hematological malignancies. Multiple myeloma is one of the difficult entities, especially since information on the start of the disease may be lacking, and the time of diagnosis can be incorrect”.
In Denmark, bortezomib was found to be well registered, even though hospital-administrated drugs are not prescribed through the pharmacy and therefore not captured in the e-pharmacy’s IT system. Lenalidomide was also found to be well registered, while less expensive drugs that are typically given in combination with bortezomib were not (ie, melphalan, or melphalan in combination with thalidomide). Danish national MM guidelines during 2010–2018 stipulate that, at least in the late study period, bortezomib is co-prescribed with other drugs, mainly melphalan in the elderly patients and cyclophosphamide in younger patients. However, our study found that only 39% of patients receiving bortezomib had a co-medication registered.
In Finland, some medication data were available in the HILMO registry. While melphalan, thalidomide, and lenalidomide prescriptions had good coverage in the PDR (as expected, since bortezomib is not prescribed, but administered by the physician in the clinic), bortezomib was not covered. Therefore, proxies or other data sources are required for any analysis on bortezomib use. In Sweden, use of melphalan, thalidomide, lenalidomide, but not bortezomib, was registered in the PDR. Furthermore, very few bortezomib registrations were identified in the NPR, since bortezomib is typically administered during nurse visits, and the NPR only contains data on physician visits, not nurse visits. Therefore, neither the PDR nor the NPR can be used for studying persistence of bortezomib or bortezomib-based combination therapy.
Registries in the Nordic countries offer numerous benefits for epidemiologic research, including: large sample sizes allowing for the study of rare exposure and outcome measures, complete, prospective, and independent data collection, and limited or no selection and attrition bias.2 Important outcomes such as OS can be assessed from Cause of Death registers, drug outcomes from the PDRs and treatments such as stem cell transplantation can be derived from the NPRs. However, certain limitations must be considered. First, since the data have not been collected primarily for the purposes of addressing a given research question, their quality for the intended research purpose is unknown and the variables are limited to those used in the registry.2,29 Furthermore, coded diagnoses might not always be relevant, and there can be variation in coding practice between departments or institutions or over time (such as when new coding systems are introduced) or incomplete coding for seriously ill patients.2 Another important limitation is the process for obtaining data from the registries, which can be complex and time consuming due to the requirement for numerous applications and approvals from data owners.30 Indeed, although Norway was included in the study protocol, data were not available for this analysis owing to a delay in approvals.
The current study explored combined use of the NPR, CR, PDR, and CDR in the Nordic countries. However, other registries are available as data sources, namely the specific national MM registries in Denmark31 and Sweden.32 The Danish National Multiple Myeloma Registry (DMMR) was established in 2005, aiming primarily to collect clinical data including complications, prognostic staging, and first and second lines of therapy in all newly diagnosed patients with symptomatic and smoldering MM, and to support research. Data are validated and completeness is above 98%.31 Similarly, in 2008, the Swedish Myeloma Registry was established, which records data in newly diagnosed patients with myeloma.32 The Individual Patient Overview (IPÖ), which was developed in Sweden, collects data from patients with cancer and creates individual patient-visual summaries. The data are accessible and developed on the same technical platform used for all national quality registers in the field; data can be transferred from the IPÖ to a quality register, which improves data in the national research catalog.33
Evidence suggests that the incidence and prevalence of MM are increasing globally, not just in Scandinavia.17,34 In a global burden-of-disease study, published in 2016, the incidence of MM was shown to have increased 126% between 1990 and 2016.17 In this study, an increase in both the incidence and prevalence of MM, from 2010 up to 2016, was noted in Denmark. In Finland and Sweden, the prevalence showed a steady increase; however, while the incidence remained relatively stable in Sweden (ranging from 7.2 to 7.8/100,000), it showed a downward trend in Finland. The 2016 incidence was 7.3, 6.4, and 7.6/100,000 in Denmark, Finland, and Sweden, respectively. This aligns closely with the 2020 age-adjusted incidence provided by the European Cancer Information System (https://ecis.jrc.ec.europa.eu/), which showed incidence of 8.8, 7.0, and 7.8 in Denmark, Finland, and Sweden, respectively. In other recent reports, the incidence was 6.8/100,000 in Sweden based on the MM registry data32 and 6.09/100,000 in Finland.35
The observation that prevalence is increasing while incidence is unchanged in Sweden or maybe even decreasing in Finland suggests improved MM survival. Improved MM survival, including among more elderly patients (aged over 80 years) and generally for those treated with options other than ASCT, has been described recently in studies conducted in Denmark,36 Norway, and Sweden.37,38 However, it is also important to note that diagnoses were evaluated from 2005 to 2016, while medications were evaluated from 2010 to 2016, potentially introducing a selection bias with more patients in the earlier years. Furthermore, differences in the trends in the three countries could be due to the differences in the quality of MM registration in the cancer registries and in the registration of MM-specific drugs.
Conclusion
National registries are a rich resource for researchers aiming to examine the epidemiology, treatment patterns, health-care utilization, and treatment outcomes for specific diseases. The registries evaluated in this study allowed identification of the MM population across the three Nordic countries, although gaps were identified in the Swedish and Finnish CRs. The main drugs used for the treatment of patients with MM within the study period, lenalidomide, and bortezomib, had good coverage in Danish registries but not in Finnish or Swedish registries, indicating that, for studying treatment patterns in MM based on use of NPRs and PDRs, researchers are best served by Danish registries. Future research into the MM population using data from these registries will enable in-depth epidemiologic analyses, such as those relating to the patient characteristics, overall survival, and healthcare resource utilization for these patients.
Abbreviations
ASCT, autologous stem cell transplantation; ATC, Anatomical Therapeutic Chemical; AvoHILMO, National Care Registry for Primary Healthcare Institutions; CDR, Cause of Death Registry; CR, Cancer Registry; DAGS, Danish Outpatient Grouping System; DMMR, Danish National Multiple Myeloma Registry; DRG, Diagnosis Related Groups; EMR, electronic medical record; HILMO, National Care Registry for Health Care Institutions; HUMAN, Health outcomes and Understanding of Myeloma: A multi-National study; ICD-10, International Classification of Diseases 10th Revision; ICPC-2, International Classification of Primary Care 2nd Edition; IPÖ, Individual Patient Overview; KVÅ, Koder ur Klassifikation av vårdåtgärder (classification of care measures); MM, multiple myeloma; NCSP, Nordic Classification of Surgical Procedures; NDMM, newly diagnosed multiple myeloma; NPR, National Patient Registry; OTC, over the counter; PDR, Prescribed Drug Registry; THL, Terveyden ja hyvinvoinnin laitos.
Data Sharing Statement
The datasets generated during and/or analyzed during the study are not publicly available but are available from the corresponding author on reasonable request.
Acknowledgments
The authors gratefully acknowledge the contribution of Anders Green, MD, DrMedSci, Institute of Applied Economics and Health Research and Odense University Hospital, Odense, Denmark, in providing scientific support and advice on access to, and management of data from, the Danish registries. Writing support was provided by Kate Bradford at Parexel, funded by Takeda Pharmaceuticals International AG.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis, and interpretation, or in all areas; took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Funding
Study funded by Takeda Pharmaceuticals International AG.
Disclosure
N Abildgaard has received research grants from Amgen, Bristol Myers Squibb, Celgene, Janssen, and Takeda; consulting fees from Bristol Myers Squibb, Celgene, Janssen, Novartis, and Takeda. J Freilich and Y Ma are employees of Parexel and received funding from Takeda for conducting study analyses. N Bent-Ennakhil and S Ørstavik are employees of Takeda. P Anttila has received consulting fees from Amgen, Bristol Myers Squibb, Celgene, GlaxoSmithKline, Janssen, Novartis, Sanofi, and Takeda; travel grants from AbbVie, Amgen, Bristol Myers Squibb, Celgene, Janssen, Mundipharma, Novartis, Roche, Sanofi Genzyme, and Teva. A Waage has received consulting fees from Janssen and Takeda. M Lassenius and I Toppila are employees of Medaffcon; Medaffcon received funding from Parexel for conducting study analyses. I Turesson has received consulting fees from Janssen and Takeda. M Hansson has received consulting fees from Janssen, Pfizer, Takeda, and Bristol Myers Squibb. The authors report no other conflicts of interest in this work.
References
1. Frank L. Epidemiology when an entire country is a cohort. Science. 2000;287(5462):2398–2399. doi:10.1126/science.287.5462.2398
2. Thygesen LC, Ersbøll AK. When the entire population is the sample: strengths and limitations in register-based epidemiology. Eur J Epidemiol. 2014;29(8):551–558. doi:10.1007/s10654-013-9873-0
3. Forsea AM. Cancer registries in Europe-going forward is the only option. Ecancermedicalscience. 2016;10:641. doi:10.3332/ecancer.2016.641
4. Zanetti R, Sacchetto L, Coebergh JW, Rosso S. To accelerate cancer prevention in Europe: challenges for cancer registries. Eur J Cancer. 2018;104:151–159. doi:10.1016/j.ejca.2018.09.001
5. Furu K, Wettermark B, Andersen M, Martikainen JE, Almarsdottir AB, Sørensen HT. The Nordic countries as a cohort for pharmacoepidemiological research. Basic Clin Pharmacol Toxicol. 2010;106(2):86–94. doi:10.1111/j.1742-7843.2009.00494.x
6. Thygesen LC, Daasnes C, Thaulow I, Brønnum-Hansen H. Introduction to Danish (nationwide) registers on health and social issues: structure, access, legislation, and archiving. Scand J Public Health. 2011;39(7 Suppl):12–16. doi:10.1177/1403494811399956
7. Van Der Wel KA, Östergren O, Lundberg O, et al. A gold mine, but still no Klondike: Nordic register data in health inequalities research. Scand J Public Health. 2019;47(6):618–630. doi:10.1177/1403494819858046
8. Maret-Ouda J, Tao W, Wahlin K, Lagergren J. Nordic registry-based cohort studies: possibilities and pitfalls when combining Nordic registry data. Scand J Public Health. 2017;45(17_suppl):14–19. doi:10.1177/1403494817702336
9. Laugesen K, Ludvigsson JF, Schmidt M, et al. Nordic health registry-based research: a review of health care systems and key registries. Clin Epidemiol. 2021;13:533–554. doi:10.2147/CLEP.S314959
10. Nilbert M, Thomsen LA, Winther Jensen J, et al. The power of empirical data; lessons from the clinical registry initiatives in Scandinavian cancer care. Acta Oncol. 2020;59(11):1343–1356. doi:10.1080/0284186x.2020.1820573
11. Pukkala E, Engholm G, Højsgaard Schmidt LK, et al. Nordic cancer registries - an overview of their procedures and data comparability. Acta Oncol. 2018;57(4):440–455. doi:10.1080/0284186x.2017.1407039
12. Wettermark B, Zoëga H, Furu K, et al. The Nordic prescription databases as a resource for pharmacoepidemiological research--a literature review. Pharmacoepidemiol Drug Saf. 2013;22(7):691–699. doi:10.1002/pds.3457
13. Gavin A, Rous B, Marcos-Gragera R, et al. Towards optimal clinical and epidemiological registration of haematological malignancies: guidelines for recording progressions, transformations and multiple diagnoses. Eur J Cancer. 2015;51(9):1109–1122. doi:10.1016/j.ejca.2014.02.008
14. Leinonen MK, Rantanen M, Pitkäniemi J, Malila N. Coverage and accuracy of myeloproliferative and myelodysplastic neoplasms in the Finnish Cancer Registry. Acta Oncol. 2016;55(6):782–786. doi:10.3109/0284186x.2015.1127416
15. Castella M, Fernández de Larrea C, Martín-Antonio B. Immunotherapy: a novel era of promising treatments for multiple myeloma. Int J Mol Sci. 2018;19(11):3613. doi:10.3390/ijms19113613
16. Rajkumar SV, Dimopoulos MA, Palumbo A, et al. International Myeloma Working Group updated criteria for the diagnosis of multiple myeloma. Lancet Oncol. 2014;15(12):e538–548. doi:10.1016/s1470-2045(14)70442-5
17. Cowan AJ, Allen C, Barac A, et al. Global burden of multiple myeloma: a systematic analysis for the global burden of disease study 2016. JAMA Oncol. 2018;4(9):1221–1227. doi:10.1001/jamaoncol.2018.2128
18. Danish Health Data Authority. National patient register. Available from: https://sundhedsdatastyrelsen.dk/da/registre-og-services/om-de-nationale-sundhedsregistre/sygdomme-laegemidler-og-behandlinger/landspatientregisteret.
19. Finnish Institute for Health and Welfare (THL). Finnish national care register for healthcare institutions (HILMO). Available from: https://thl.fi/en/web/thlfi-en/statistics-and-data/data-and-services/register-descriptions/care-register-for-health-care.
20. Finnish Institute for Health and Welfare (THL). Primary health care outpatient care notification (AvoHILMO). Available from: https://thl.fi/fi/tilastot-ja-data/ohjeet-tietojen-toimittamiseen/perusterveydenhuollon-avohoidon-hoitoilmoitus-avohilmo.
21. The National Board of Health and Welfare, Sweden. National patient register. Available from: https://www.socialstyrelsen.se/en/statistics-and-data/registers/national-patient-register/.
22. Danish Health Data Authority. Medicines statistics register. Available from: https://sundhedsdatastyrelsen.dk/da/registre-og-services/om-de-nationale-sundhedsregistre/sygdomme-laegemidler-og-behandlinger/laegemiddelstatistikregisteret.
23. Kela. Deliveries of medicines reimbursed by health insurance. Available from: https://www.stat.fi/tilasto/resep.
24. The National Board of Health and Welfare, Sweden. National prescribed drug register. Available from: https://www.socialstyrelsen.se/en/statistics-and-data/registers/national-prescribed-drug-register/.
25. Danish Health Data Authority. Cancer registry. Available from: https://sundhedsdatastyrelsen.dk/da/registre-og-services/om-de-nationale-sundhedsregistre/sygdomme-laegemidler-og-behandlinger/cancerregisteret.
26. Cancer Society of Finland. Finnish cancer registry. Available from: https://syoparekisteri.fi/.
27. The National Board of Health and Welfare, Sweden. National cancer register. Available from: https://www.socialstyrelsen.se/en/statistics-and-data/registers/national-cancer-register/.
28. Leinonen MK, Miettinen J, Heikkinen S, Pitkäniemi J, Malila N. Quality measures of the population-based Finnish cancer registry indicate sound data quality for solid malignant tumours. Eur J Cancer. 2017;77:31–39. doi:10.1016/j.ejca.2017.02.017
29. Sund R. Quality of the Finnish Hospital Discharge Register: a systematic review. Scand J Public Health. 2012;40(6):505–515. doi:10.1177/1403494812456637
30. Ludvigsson JF, Håberg SE, Knudsen GP, et al. Ethical aspects of registry-based research in the Nordic countries. Clin Epidemiol. 2015;7:491–508. doi:10.2147/clep.S90589
31. Gimsing P, Holmström MO, Klausen TW, et al. The Danish National Multiple Myeloma Registry. Clin Epidemiol. 2016;8:583–587. doi:10.2147/clep.S99463
32. Blimark CH, Turesson I, Genell A, et al. Outcome and survival of myeloma patients diagnosed 2008–2015. Real-world data on 4904 patients from the Swedish Myeloma Registry. Haematologica. 2018;103(3):506–513. doi:10.3324/haematol.2017.178103
33. Regional Cancer Centres Samverkan. Individuell patientöversikt (IPÖ) i cancervården [Individual patient overview (IPÖ) in cancer care]. Swedish. Available from: https://cancercentrum.se/samverkan/vara-uppdrag/kunskapsstyrning/patientoversikter/.
34. Vélez R, Turesson I, Landgren O, Kristinsson SY, Cuzick J. Incidence of multiple myeloma in Great Britain, Sweden, and Malmö, Sweden: the impact of differences in case ascertainment on observed incidence trends. BMJ Open. 2016;6(1):e009584. doi:10.1136/bmjopen-2015-009584
35. Pitkäniemi J, Malila N, Tanskanen T, et al. Cancer in Finland 2018. Cancer Soc Finland Pub. 2018;2018:98.
36. Hannig LH, Nielsen LK, Ibsen R, Arnheim-Dahlstrom L, Kjellberg J, Abildgaard N. The impact of changed treatment patterns in multiple myeloma on health-care utilisation and costs, myeloma complications, and survival: a population-based comparison between two time periods in Denmark. Eur J Haematol. 2021;107(1):63–73. doi:10.1111/ejh.13615
37. Borgsten F, Gatopoulou X, Pisini M, et al. Healthcare resource utilisation and sickness absence in newly diagnosed multiple myeloma patients who did not undergo autologous stem cell transplantation: trends in Sweden with the changing treatment landscape. Eur J Haematol. 2021;107(1):92–103. doi:10.1111/ejh.13623
38. Langseth ØO, Myklebust T, Johannesen TB, Hjertner Ø, Waage A. Incidence and survival of multiple myeloma: a population-based study of 10 524 patients diagnosed 1982–2017. Br J Haematol. 2020;191(3):418–425. doi:10.1111/bjh.16674
 © 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.
© 2023 The Author(s). This work is published and licensed by Dove Medical Press Limited. The full terms of this license are available at https://www.dovepress.com/terms.php and incorporate the Creative Commons Attribution - Non Commercial (unported, v3.0) License.
By accessing the work you hereby accept the Terms. Non-commercial uses of the work are permitted without any further permission from Dove Medical Press Limited, provided the work is properly attributed. For permission for commercial use of this work, please see paragraphs 4.2 and 5 of our Terms.